The Potential of Use Basil and Rosemary Essential Oils as Effective Antibacterial Agents
Abstract
:1. Introduction
2. Results
2.1. Chemical Composition of the Basil and Rosemary Essential Oils
| Number of compounds | Compound | % | RI | ||
|---|---|---|---|---|---|
| 1 | α-Pinene | 0.4 | 929 | ||
| 2 | Camphene | 0.1 | 942 | ||
| 3 | Sabinene | 0.2 | 965 | ||
| 4 | β-Pinene | 0.6 | 969 | ||
| 5 | 2,3-Dehydro-1.8-cineole | Tr | 979 | ||
| 6 | Myrcene | 0.2 | 983 | ||
| 7 | p-Cymene | 0.1 | 1013 | ||
| 8 | 1,8-Cineole | 4.9 | 1020 | ||
| 9 | Limonene | 0.4 | 1021 | ||
| 10 | (E)-β-Ocimene | 0.6 | 1038 | ||
| 11 | trans-Linalool oxide (f) | Tr | 1058 | ||
| 12 | Fenchone | 0.2 | 1067 | ||
| 13 | cis-Linalool oxide (f) | Tr | 1073 | ||
| 14 | Linalool | 1.2 | 1085 | ||
| 15 | endo-Fenchol | 0.2 | 1098 | ||
| 16 | Camphor | 0.7 | 1119 | ||
| 17 | Menthone | 0.1 | 1134 | ||
| 18 | Isomenthone | Tr | 1143 | ||
| 19 | Borneol | 0.2 | 1149 | ||
| 20 | Menthol | 0.3 | 1159 | ||
| 21 | Terpinen-4-ol | 0.1 | 1163 | ||
| 22 | Estragole | 86.4 | 1188 | ||
| 23 | Fenchyl acetate | 0.3 | 1209 | ||
| 24 | Bornyl acetate | 0.3 | 1269 | ||
| 25 | 2-Hydroxycineol acetate | Tr | 1321 | ||
| 26 | Eugenol methyl ether | 0.5 | 1373 | ||
| 27 | β-Bourbonene | Tr | 1385 | ||
| 28 | β-Elemene | 0.3 | 1389 | ||
| 29 | cis-α-Bergamotene | Tr | 1412 | ||
| 30 | β-Caryophyllene | 0.1 | 1419 | ||
| 31 | trans-α-Bergamotene | 3.0 | 1435 | ||
| 32 | β-Sesquifenchene | 0.2 | 1437 | ||
| 33 | (Z)-β-Farnesene | tr | 1447 | ||
| 34 | α-Humulene | tr | 1452 | ||
| 35 | Cadina-1(6),4-diene | tr | 1459 | ||
| 36 | trans-β-Bergamotene | 0.2 | 1479 | ||
| 37 | α-Bulnesene | 0.1 | 1499 | ||
| 38 | γ-Cdinene | 0.5 | 1506 | ||
| 39 | Calamenene | tr | 1510 | ||
| 40 | β-Sesquiphellandrene | 0.1 | 1514 | ||
| 41 | p-Methoxycinnamaldehyde | 0.5 | 1525 | ||
| 42 | p-Methoxycinnamyl alcohol | 0.4 | 1532 | ||
| 43 | Spathulenol | 0.1 | 1565 | ||
| 44 | Caryophyllene oxide | 0.1 | 1571 | ||
| 45 | Humulene epoxide II | 0.1 | 1595 | ||
| 46 | 1- epi-Cubenol | 0.1 | 1603 | ||
| 47 | T-Cadinol | 0.7 | 1627 | ||
| 48 | α-Cadinol | tr | 1639 | ||
| Number of compounds | Compound | % | RI |
|---|---|---|---|
| 1 | Tricyclene | 0.2 | 919 |
| 2 | α-Thujene | 0.1 | 923 |
| 3 | α-Pinene | 11.0 | 932 |
| 4 | Camphene | 5.2 | 944 |
| 5 | Sabinene | 0.1 | 966 |
| 6 | β-Pinene | 9.2 | 971 |
| 7 | Myrcene | 1.2 | 983 |
| 8 | α-Phellandrene | 0.2 | 997 |
| 9 | Car-3-ene | 0.1 | 1005 |
| 10 | α-Terpinolene | 0.1 | 1010 |
| 11 | p-Cymene | 1.3 | 1017 |
| 12 | 1,8-Cineole | 46.4 | 1027 |
| 13 | Limonene | 1.0 | 1027 |
| 14 | γ-Terpinene | 1.0 | 1050 |
| 15 | trans-Sabinene | tr | 1054 |
| 16 | Terpinolene | 0.2 | 1079 |
| 17 | Linalool | 0.5 | 1087 |
| 18 | α-Campholenol | tr | 1096 |
| 19 | endo-Fenchol | tr | 1102 |
| 20 | Camphor | 11.4 | 1124 |
| 21 | Borneol | 3.1 | 1152 |
| 22 | Terpinen-4-ol | 0.4 | 1163 |
| 23 | α-Terpineol | 1.8 | 1175 |
| 24 | Bornyl acetate | 1.0 | 1269 |
| 25 | α-Cubebene | tr | 1349 |
| 26 | α-Ylangene | tr | 1372 |
| 27 | α-Copaene | 0.1 | 1377 |
| 28 | Longifolene | 0.1 | 1407 |
| 29 | β-Caryophyllene | 3.5 | 1421 |
| 30 | α-Humulene | 0.4 | 1452 |
| 31 | γ-Muurolene | 0.1 | 1471 |
| 32 | α-Selinene | tr | 1492 |
| 33 | α-Muurolene | tr | 1494 |
| 34 | γ-Cadinene | tr | 1506 |
| 35 | trans-Calamenene | tr | 1511 |
| 36 | δ-Cadinene | 0.1 | 1514 |
| 37 | β-Caryophyllene oxide | 0.1 | 1571 |
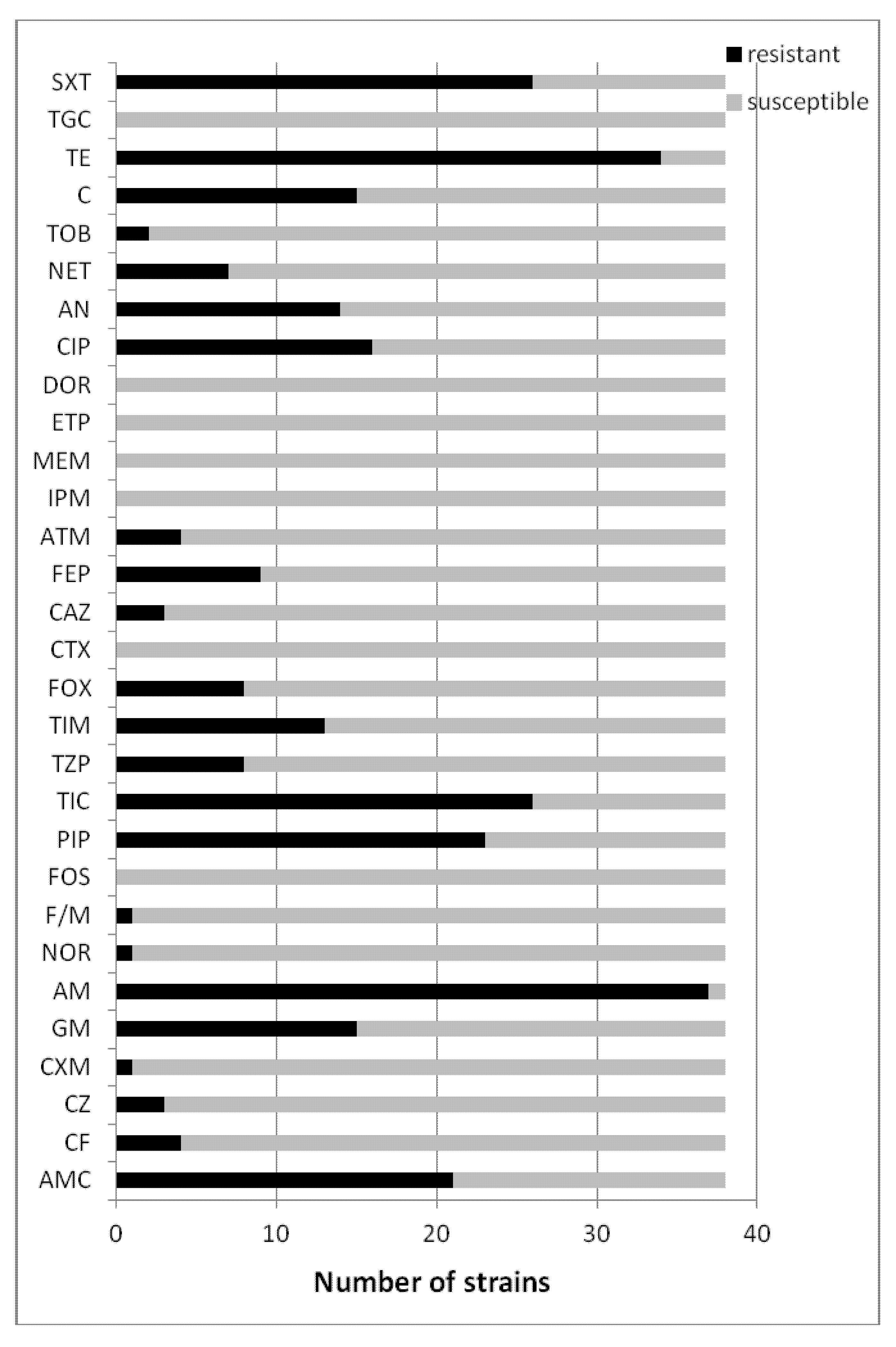
2.2. Susceptibility Testing of Clinical Escherichia coli Strains
2.2.1. Susceptibility Testing of Clinical Escherichia coli (ESBL+) Strains
2.2.2. Susceptibility Testing of Clinical Escherichia coli (ESBL−) Strains

2.3. The Susceptibility Escherichia coli Bacterial Strains to Basil Oil
2.3.1. The Susceptibility Escherichia coli (ESBL+) Strains to Basil Oil
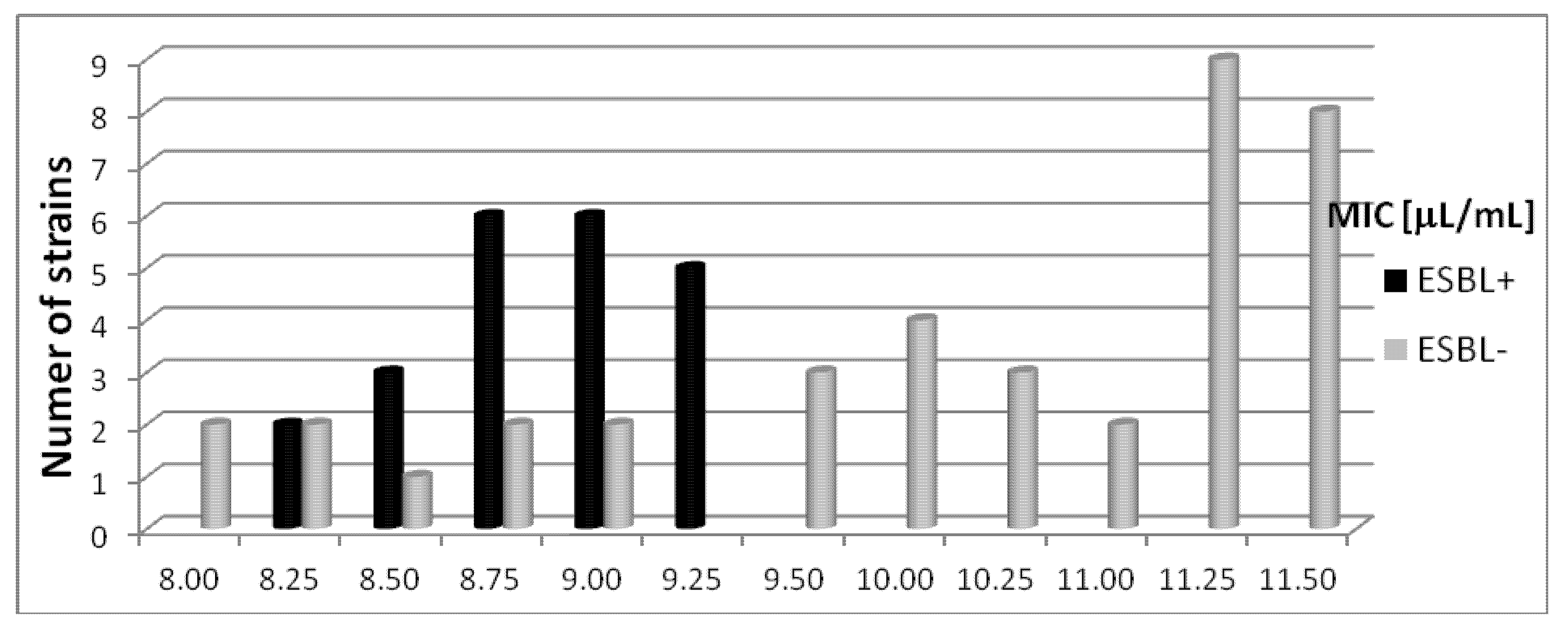
2.3.2. The Susceptibility Escherichia coli (ESBL−) Strains to Basil Oil
2.4. The Susceptibility Escherichia coli Bacterial Strains to Rosemary Oil
2.4.1. The Susceptibility of Escherichia coli (ESBL+) Strains to Rosemary Oil
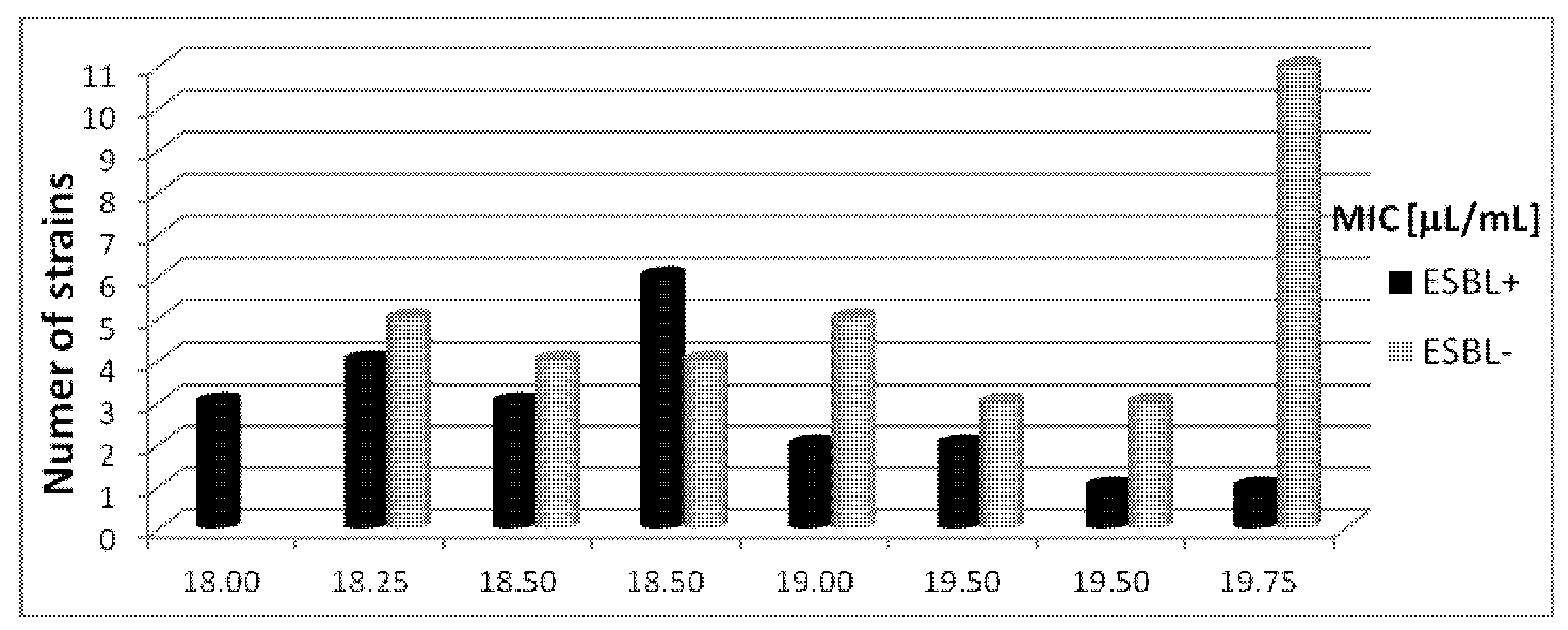
2.4.2. The Susceptibility of Escherichia coli (ESBL−) Strains to Rosemary Oil
3. Discussion
4. Experimental
4.1. Bacterial Strains
4.2. Bacterial Strain Identification
4.3. Essential Oil Analysis
4.4. Antibacterial Tests
4.5. Susceptibility Testing
5. Conclusions
- (1)
- The results of these experiments indicate the potential use of basil and rosemary essential oils against resistant Escherichia coli clinical strains, and also against extended-spectrum β-lactamase positive bacteria.
- (2)
- The tested basil oil was more active against all Escherichia coli clinical strains.
- (3)
- The action of essential oils against bacteria exhibiting different mechanisms ofresistance may beuseful, not only in treating but alsopreventingthe spreadof resistantstrains.
Acknowledgments
Conflicts of Interest
References
- Canton, R.; Novais, A.; Valverde, A.; Machado, E.; Peixe, L.; Baquero, F.; Coque, T.M. Prevalence and spread of extended-spectrum β-lactamase-producing Enterobacteriaceae in Europe. Clin. Microbiol. Infect. 2008, 14, 144–153. [Google Scholar] [CrossRef]
- Cornaglia, G.; Akova, M.; Amicosante, G.; Cantón, R.; Cauda, R.; Docquier, J.D.; Edelstein, M.; Frère, J.M.; Fuzi, M.; Galleni, M.; et al. ESCMID Study Group for Antimicrobial Resistance Surveillance (ESGARS). Metallo-β-lactamases as emerging resistance determinants in Gram-negative pathogens. Int. J. Antimicrob. Agents 2007, 29, 380–388. [Google Scholar] [CrossRef]
- Cornaglia, G.; Garau, J.; Livermore, D.M. Living with ESBLs. Clin. Microbiol. Infect. 2008, 14, 1–2. [Google Scholar] [CrossRef]
- Empel, J.; Baraniak, A.; Literacka, E.; Mrówka, A.; Fiett, J.; Sadowy, E.; Hryniewicz, W.; Gniadkowski, M. Molecular survey of β-lactamases conferring resistance to newer β-lactams in Enterobacteriaceae isolates from Polish hospitals. Antimicrob. Agents Chemother 2008, 52, 2449–2454. [Google Scholar] [CrossRef]
- Pitout, J.D.D.; Nordmann, P.; Laupland, K.B.; Nordmann, P. Emergence of Enterobcteriaceae producing extended-spectrum β-lactamases (ESBLs) in the community. J. Antimicrob. Chemother. 2005, 56, 52–59. [Google Scholar] [CrossRef]
- Nicolas-Chanoine, M.H.; Blanco, J.; Leflon-Guibout, V.; Demarty, R.; Alonso, M.P.; Caniça, M.M.; Park, Y.J.; Lavigne, J.P.; Pitout, J.; Johnson, J.R. Intercontinental emergence of Escherichia coli clone O25:H4-ST131 producing CTX-M-15. J. Antimicrob. Chemother. 2008, 61, 273–281. [Google Scholar]
- Woodford, N.; Reddy, S.; Fagan, E.J.; Hill, R. L.; Hopkins, K.L.; Kaufmann, M.E.; Kistler, J.; Palepou, M.F.; Pike, R.; Ward, M.E.; et al. Wide geographic spread of diverse acquired AmpC beta-lactamases among Escherichia coli and Klebsiella spp. in the UK and Ireland. J. Antimicrob. Chemother. 2007, 59, 102–105. [Google Scholar]
- Kang, H.Y.; Jeong, Y.S.; Oh, J.Y.; Jeong, J.H.; Seol, S.Y.; Cho, D.T.; Kim, J.; Lee, Y.C. Characterization of antimicrobial resistance and class 1 integrons found in Escherichia coli isolates from humans and animals in Korea. J. Antimicrob. Chemother. 2005, 55, 639–644. [Google Scholar] [CrossRef]
- Tenover, C.; Raney, P.M.; Williams, P.P.; Rasheed, J.K.; Biddle, J.W.; Oliver, A.; Fridkin, S.K.; Jevitt, L.; McGowan, J.E., Jr. Evaluation of the NCCLS extended-spectrum β-lactamase confirmation methods for Escherichia coli with isolates collected during Project ICARE. J. Clin Microbiol. 2003, 41, 3142–3146. [Google Scholar] [CrossRef]
- Pereira, R.S.; Sumita, T.C.; Furlan, M.R.; Jorge, A.O.; Ueno, M. Antibacterial activity of essential oils on microorganisms isolated from urinary tract infection. Rev. Saude Publica 2004, 38, 326–328. [Google Scholar] [CrossRef]
- Drieux, L.; Brossier, F.; Sougakoff, W.; Jarlier, V. Phenotypic detection of extended-spectrum beta-lactamase production in Enterobacteriaceae: Review and bench guide. Clin. Microbiol. Infect. 2008, 14, 90–103. [Google Scholar] [CrossRef]
- Canton, R.; Coque, T.M. The CTX-M beta-lactamase pandemic. Curr. Opin. Microbiol. 2006, 9, 466–475. [Google Scholar] [CrossRef]
- Silva, N.C.C.; Fernandes, A., Jr. Biological properties of medicinal plants: A review of their antimicrobial activity. J. Venom. Anim. Toxins Trop. Dis. 2010, 16, 402–413. [Google Scholar] [CrossRef]
- Rios, J.L.; Recio, M.C. Medicinal plants and antimicrobial activity. J. Ethnopharm. 2005, 100, 80–84. [Google Scholar] [CrossRef]
- Sparg, S.G.; Light, M.E.; van Staden, J. Biological activities and distribution of plant saponins. J. Ethnopharm. 2004, 94, 219–243. [Google Scholar] [CrossRef]
- Tajkarimi, M.M.; Ibrahim, S.A.; Cliver, D.O. Antimicrobial herb and spice compounds in food. Food Control 2010, 21, 1199–1218. [Google Scholar] [CrossRef]
- Burt, S. Essential oils: Their antibacterial properties and potential applications in foods—A review. Int. J. Food Microb. 2004, 94, 223–253. [Google Scholar] [CrossRef]
- De Rapper, S.; Kamatou, G.; Viljoen, A.; van Vuuren, S. The in vitro antimicrobial activity of Lavandula angustifolia essential oil in combination with other aroma-therapeutic oils. Evid. BasedComplement. Alternat. Med. 2013, 2013, 852049. [Google Scholar]
- Fernandes, T.G.; Carneiro de Mesquita, A.R.; Randau, K.P.; Franchitti, A.A.; Ximenes, E.A. In Vitro Synergistic Effect of Psidium guineense (Swartz) in Combination with Antimicrobial Agents against Methicillin-Resistant Staphylococcus aureus Strains. Scient. World J. 2012, 2012, 158237. [Google Scholar]
- Fankam, A.G.; Kuete, V.; Voukeng, I.K.; Kuiate, J.R.; Pages, J.-M. Antibacterial activities of selected Cameroonian spices and their synergistic effects with antibiotics against multidrug-resistant phenotypes. BMC Complement. Altern. Med. 2011, 11, 104. [Google Scholar] [CrossRef]
- Nweze, E.I.; Eze, E.E. Justification for the use of Ocimum gratissimum L. in herbal medicine and its interaction with disc antibiotics. BMC Complement. Altern. Med. 2009, 9, 37. [Google Scholar] [CrossRef]
- Sung, W.S.; Lee, D.G. The combination effect of Korean red ginseng saponins with kanamycin and cefotaxime against methicillinresistant Staphylococcus aureus. Biol. Pharm. Bull. 2008, 31, 1614–1617. [Google Scholar] [CrossRef]
- Zhao, J.; Lou, J.; Mou, Y.; Li, P.; Wu, J.; Zhou, L. Diterpenoid tanshinones and phenolic acids from cultured hairy roots of Salvia miltiorrhiza Bunge and their antimicrobial activities. Molecules 2011, 16, 2259–2267. [Google Scholar] [CrossRef]
- Lee, S.J.; Umano, K.; Shibamota, T.; Lee, K.G. Identification of volatile components in basil (Ocimum basilicum L.) and thyme leaves (Thymus vulgaris L.) and their antioxidant properties. Food Chem. 2005, 91, 131–137. [Google Scholar] [CrossRef]
- Wannissorn, B.; Jarikasem, S.; Siriwangchai, T.; Thubthimthed, S. Antibacterial properties of essential oils from Thai medicinal plants. Fitoterapia 2005, 76, 233–236. [Google Scholar] [CrossRef]
- Opalchenova, G.; Obreshkova, D. Comparative studies on the activity of basilan essential oil from Ocimum basilicum L. against multidrug resistant clinical isolates of the genera Staphylococcus, Enterococcus and Pseudomonas by using different test methods. J. Microbiol. Methods 2003, 54, 105–110. [Google Scholar] [CrossRef]
- Prabuseenivasan, S.; Jayakumar, M.; Ignacimuthu, S. In vitro antibacterial activity of some plant essential oils. BMC Complement. Altern. Med. 2006, 6, 39. [Google Scholar] [CrossRef]
- Bozin, B.; Mimica-Dukic, N.; Samojlik, J.; Jovin, E. Antimicrobial and antioxidant properties of rosemary and sage Rosmarinus officinalis L. and Salvia officinalis L., Lamiaceae essential oils. J. Agric. Food Chem. 2007, 55, 7879–7885. [Google Scholar] [CrossRef]
- Orhan, I.E.; Ozcelik, B.; Kan, Y.; Kartal, M. Inhibitory effects of various essential oils and individual components against extended-spectrum beta-lactamase (ESBL) produced by Klebsiella pneumoniae and their chemical compositions. J. Food Sci. 2011, 76, 538–546. [Google Scholar] [CrossRef]
- European Pharmacopoeia, 6th ed.; Council of Europe: Strasbourg, France, 2008.
- Polish Pharmacopeia VIII, 8th ed.; Polish Pharmaceutical Society: Warsaw, Poland, 2008.
- Kalemba, D.; Kunicka, A. Antibacterial and antifungal properties of essential oils. Curr. Med. Chem. 2003, 10, 813–829. [Google Scholar] [CrossRef]
- Mihajilov-Kristev, T.; Radnovic, D.; Kitic, D.; Stajnovic-Radic, Z.; Zlatkovic, B. Antimicrobial activity of Satureja hortensis L. essential oil against pathogenic microbial strains. Bioterchnol. Biotechnol. Equip. 2009, 23, 1492–1496. [Google Scholar] [CrossRef]
- Wan, J.; Wilcock, A.; Coventry, M.J. The effect of essential oil basil on the growth of Aeromonas hydrophila and Pseudomonas fluorescens. J. Appl. Microbiol. 1998, 84, 152–158. [Google Scholar] [CrossRef]
- Soković, M.; Glamočlija, J.; Marin, P.D.; Brkić, D.; van Griensven, L.J.L.D. Antibacterial effects of the essential oils of commonly consumed medicinal herbs using an in vitro model. Molecules 2010, 15, 7532–7546. [Google Scholar] [CrossRef]
- Sartoratto, A.; Machado, A.L.M.; Delarmelina, C.; Figueira, G.M.; Duarte, M.C.T.; Rehder, V.L.G. Composition and antimicrobial activity of essential oils from aromatic plants used in Brazil. Braz. J. Microbiol. 2004, 35, 275–280. [Google Scholar] [CrossRef]
- Nakamura, C.V.; Ueda-Nakamura, T.; Bando, E.; Melo, A.F.; Cortez, D.A.; Dias Filho, B.P. Antibacterial activity of Ocimum gratissimum L. essential oil. Mem. Inst. Oswaldo Cruz 1999, 94, 675–678. [Google Scholar] [CrossRef]
- Hammer, K.A.; Carson, C.F.; Riley, T.V. Antimicrobial activity of essential oils and other plant extracts. J. Appl. Microbiol. 1999, 86, 985–990. [Google Scholar] [CrossRef]
- Lopez, P.; Sanchez, C.; Battle, R.; Nerin, C. Soilid- and vapour-phase antimicrobial activities of six essential oils: Susceptibility of selected foodborne bacterial and fungal strains. Agric. Food Chem. 2005, 53, 6939–6946. [Google Scholar] [CrossRef]
- Fabio, A.; Cermelli, C.; Fabio, G.; Nicoletti, P.; Quaglio, P. Screening of the antibacterial effects of a variety of essential oils on microorganisms responsible for respiratory infections. Phytother. Res. 2007, 21, 374–377. [Google Scholar] [CrossRef]
- Jiang, Y.; Wu, N.; Fu, Y-J.; Wang, W.; Luo, M.; Zhao, C.J.; Zu, Y.G.; Liu, X.L. Chemical composition and antimicrobial activity of the essential oil of Rosemary. Environ. Toxicol. Pharmacol. 2011, 32, 63–68. [Google Scholar] [CrossRef]
- Bendeddouche, M.S.; Benhassaini, H.; Hazem, Z.; Romane, A. Essential oil analysis and antibacterial activity of Rosmarinus tournefortii from Algeria. Nat. Prod. Commun. 2011, 6, 1511–1514. [Google Scholar]
- Edris, A.E. Pharmaceutical and therapeutic potentials of essential oils and their individual volatile constituents: A review. Phytother. Res. 2007, 21, 308–323. [Google Scholar] [CrossRef]
- Bakkali, F.; Averbeck, S.; Averbeck, D.; Idaomar, M. Biological effect of essential oils-A review. Food Chem. Toxicol. 2008, 46, 446–475. [Google Scholar] [CrossRef]
- Reichling, J.; Schnitzler, P.; Suschke, U.; Saller, R. Essential oils of aromatic plants with antibacterial, antifungal, antiviral and cytotoxic properties—An overview. In Forsch Komplementmed; 2009; Volume 16, pp. 79–90. [Google Scholar]
- Sienkiewicz, M.; Kowalczyk, E.; Wasiela, M. Recent patents regarding essential oils and the significance of their constituents in human health and treatment. Recent Pat. Anti Infect. Drug Discov. 2012, 7, 133–140. [Google Scholar] [CrossRef]
- Adams, R.P. Identification of Essential Oil Components by Gas Chromatography/Mass Spectroscopy, 4th ed.; Allured Publishing Corporation: Carol Stream, IL, USA, 2007. [Google Scholar]
- Joulain, D.; Konig, W.A. The Atlas of Spectral Data of Sesquiterpene Hydrocarbons; E.B.-Verlag: Hamburg, Germany, 1998. [Google Scholar]
- Maino, M.; Bersani, C.; Comi, G. Impedance measurements to study the antimicrobial activity of essential oils from Lamiaceae and Compositae. Int. J. Food Microbiol. 2001, 67, 187–195. [Google Scholar] [CrossRef]
- Sivropoulou, A.; Nikolaou, C.; Papanikolaou, E.; Kokkini, S.; Lanaras, T.; Arsenakis, M. ntimicrobial, cytotoxic and antiviral activities of Salvia fructicosa essential oil. J. Agric. Food Chem. 1997, 45, 3197–3201. [Google Scholar]
- Vander Berghe, D.A.; Vietinck, A.J. Screening Methods for Antibacterial and Antiviral Agents from High er Plants. In Methods In Plant Biochemistry; Dey, P.M., Harborne, J.B., Eds.; Academic Press: London, UK, 1991. [Google Scholar]
- European Committee on Antimicrobial Susceptibility Testing (EUCAST). Breakpoint Tables for Interpretation of MICs and Zone Diameters, Version 2.0; valid from 1 January; 2012. Available online: http://www.eucast.org/ (accessed on 16 August 2012).
- Jarlier, V.; Nicolas, M.; Fournier, G.; Philippon, A. Extended broad-spectrum β-lactamases conferring transferable resistance to newer β-lactam agents in Enterobacteriaceae: Hospital prevalence and susceptibility patterns. Rev. Infect. Dis. 1988, 10, 867–878. [Google Scholar] [CrossRef]
- Sample Availability: Samples of the basil and rosemary essential oils (POLLENA-AROMA Poland) are available from the authors.
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Sienkiewicz, M.; Łysakowska, M.; Pastuszka, M.; Bienias, W.; Kowalczyk, E. The Potential of Use Basil and Rosemary Essential Oils as Effective Antibacterial Agents. Molecules 2013, 18, 9334-9351. https://doi.org/10.3390/molecules18089334
Sienkiewicz M, Łysakowska M, Pastuszka M, Bienias W, Kowalczyk E. The Potential of Use Basil and Rosemary Essential Oils as Effective Antibacterial Agents. Molecules. 2013; 18(8):9334-9351. https://doi.org/10.3390/molecules18089334
Chicago/Turabian StyleSienkiewicz, Monika, Monika Łysakowska, Marta Pastuszka, Wojciech Bienias, and Edward Kowalczyk. 2013. "The Potential of Use Basil and Rosemary Essential Oils as Effective Antibacterial Agents" Molecules 18, no. 8: 9334-9351. https://doi.org/10.3390/molecules18089334
APA StyleSienkiewicz, M., Łysakowska, M., Pastuszka, M., Bienias, W., & Kowalczyk, E. (2013). The Potential of Use Basil and Rosemary Essential Oils as Effective Antibacterial Agents. Molecules, 18(8), 9334-9351. https://doi.org/10.3390/molecules18089334





