Exploring Impact of Marijuana (Cannabis) Abuse on Adults Using Machine Learning
Abstract
1. Introduction
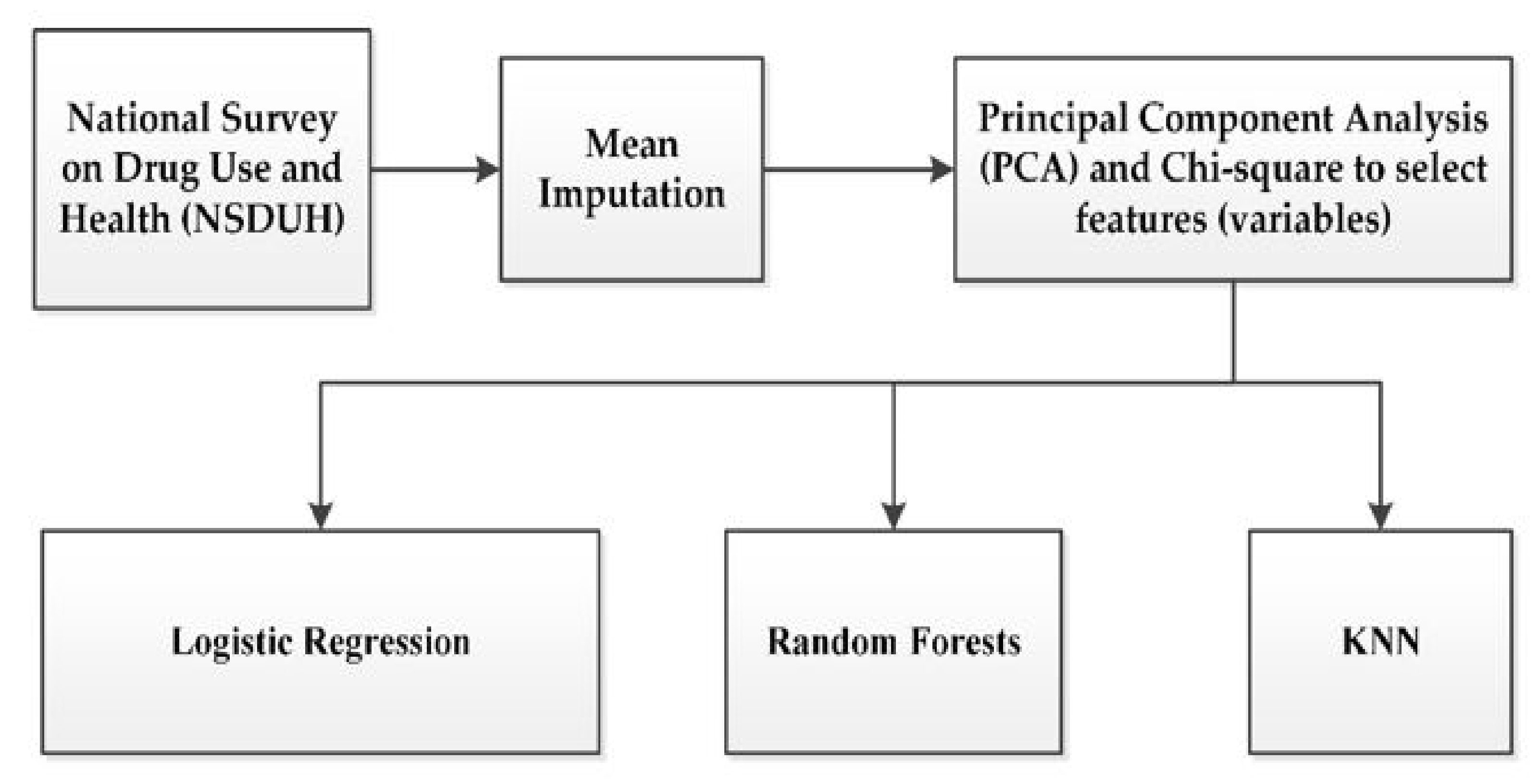
2. Materials and Methods
2.1. Research Design
2.2. Data Source
2.3. Data Collection
2.4. Data Preprocessing and Defining Labels
2.4.1. Feature (Variable) Selection
2.4.2. Imputation for Missing Data
2.4.3. Labeling of Risk for Depression
2.4.4. Labeling of Suicide Risk
2.5. Machine Learning Algorithms
2.5.1. Logistic Regression
2.5.2. Random Forest (RF)
2.5.3. K-Nearest Neighbor (KNN)
2.6. Measurement of Prediction Model Performances
3. Results
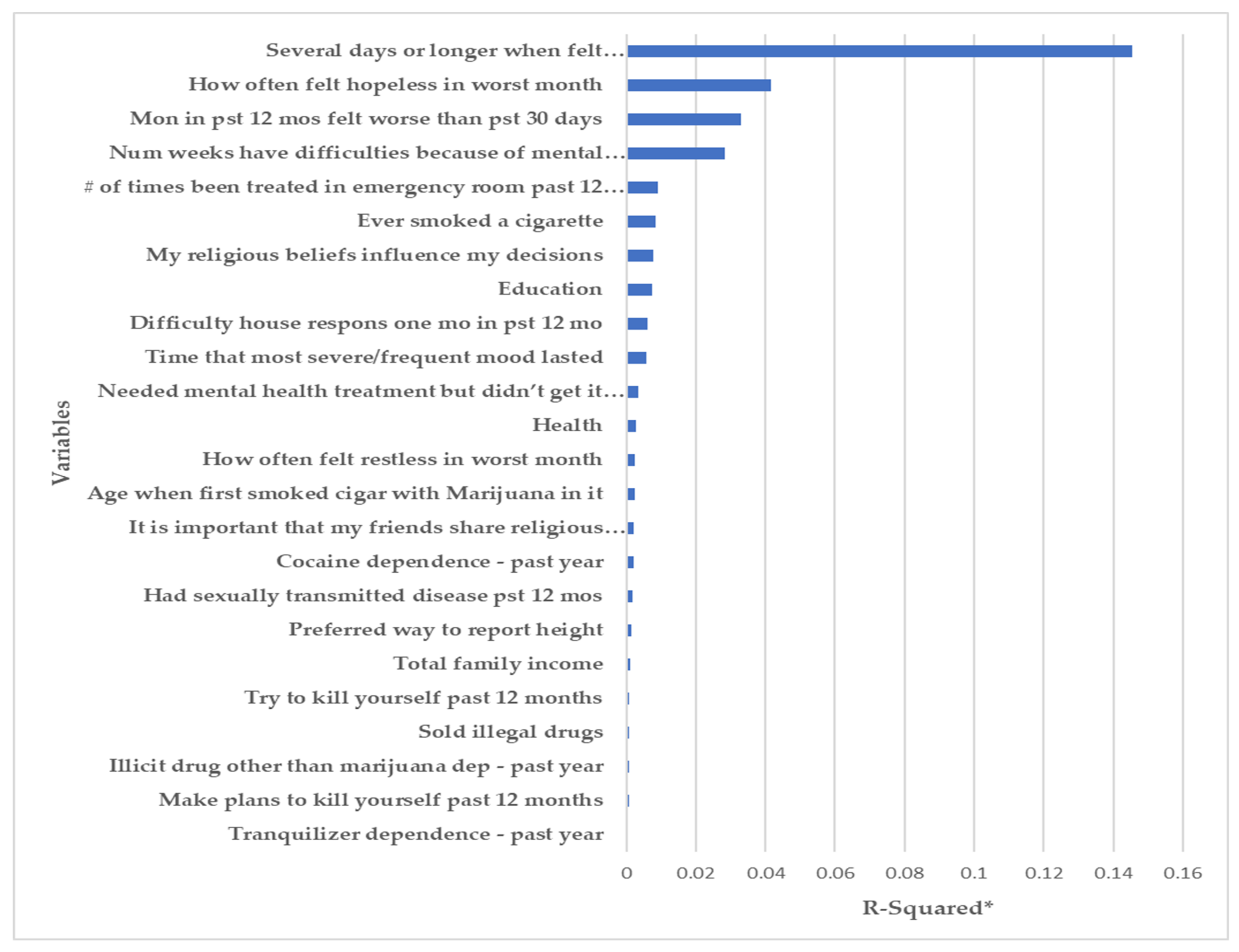
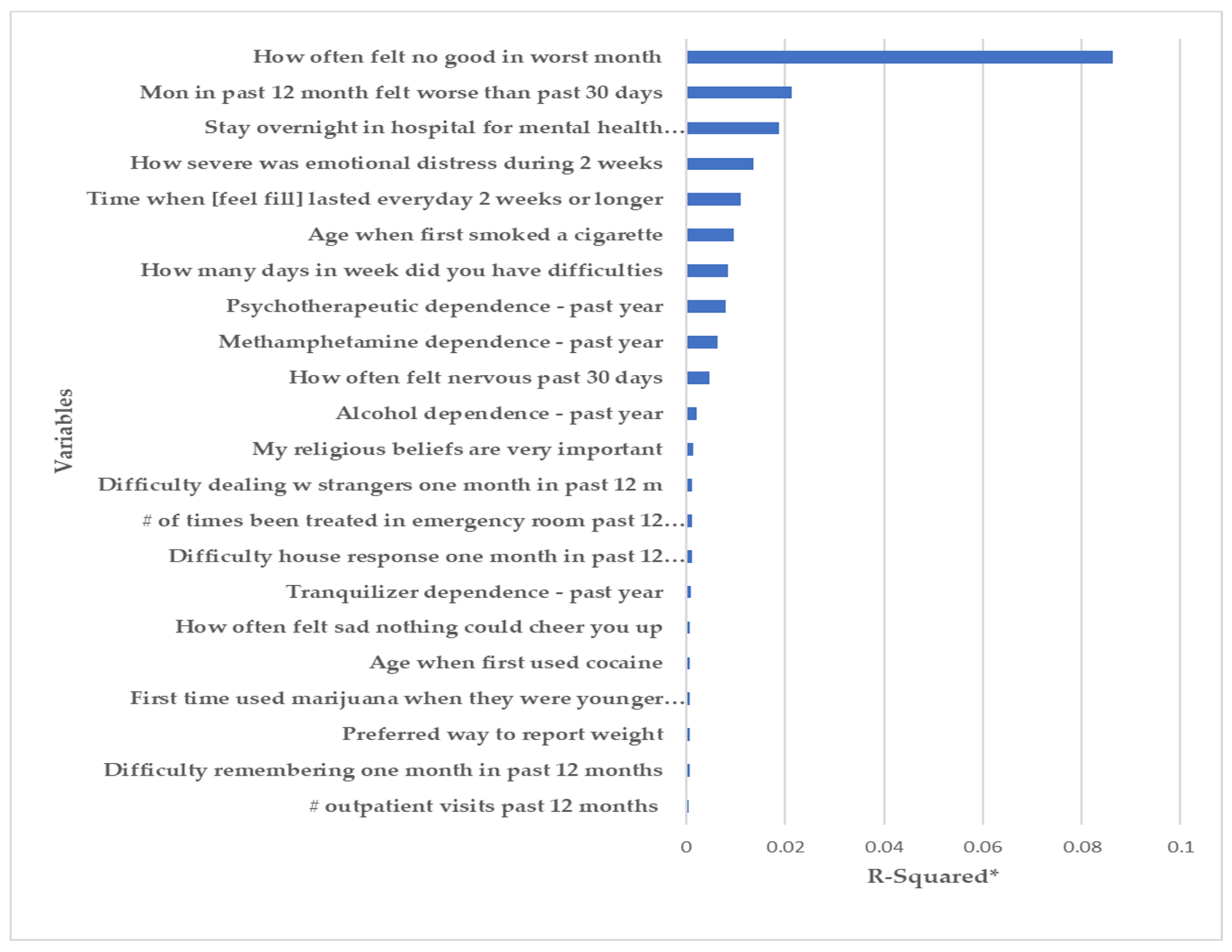
3.1. Features (Variables) Identified
3.1.1. Depression
3.1.2. Suicide Risk
3.2. Measurement of Prediction Model Performances
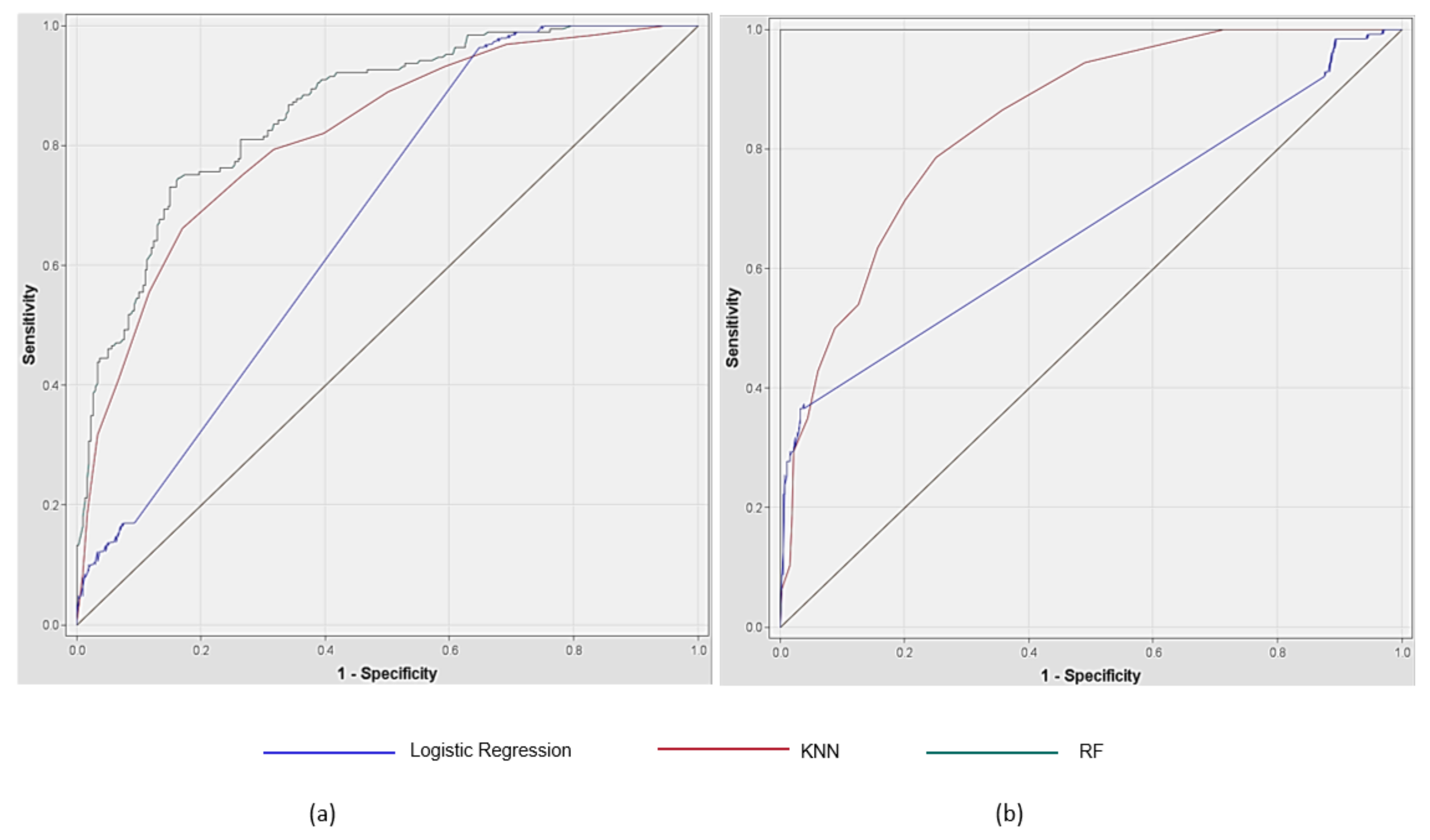
3.2.1. Depression
3.2.2. Suicide Risk
3.2.3. Summary of the ROC Curves
4. Discussion
4.1. Impact on Mental Condition
4.2. Implication for Practice
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ethan, X.; Logan, A.; Liam, M.; Leonard, J. Impact of Marijuana (Cannabis) on Health, Safety and Economy. Int. Digit. Organ. Sci. Res. 2020, 5, 43–52. [Google Scholar]
- Lee, J.; Petlakh, K. Progression to drug use from adolescent initiation of marijuana among South Korean inmates: A propensity score matching technique. Int. J. Comp. Appl. Crim. Justice 2019, 44, 221–230. [Google Scholar] [CrossRef]
- Mametja, M.; Ross, E. Decriminalized, Not Legalized: A Pilot Study of South African University Students’ Views on the Use, Impact, Legalization and Decriminalization of Marijuana. J. Drug Issues 2020, 50, 490–506. [Google Scholar] [CrossRef]
- Reis, J.P.; Auer, R.; Bancks, M.P.; Goff, D.C.; Lewis, C.E.; Pletcher, M.J.; Rana, J.S.; Shikany, J.M.; Sidney, S. Cumulative Lifetime Marijuana Use and Incident Cardiovascular Disease in Middle Age: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am. J. Public Health 2017, 107, 601–606. [Google Scholar] [CrossRef] [PubMed]
- Zibokere, E.; Ekiye, E. Theatre as an Agent of Change: Mobilising Against Marijuana Addiction in Tombia Ekpetiama Community in Bayelsa State. East Afr. J. Interdiscip. Stud. 2020, 2, 1–11. [Google Scholar] [CrossRef]
- National Institute on Drug Abuse. What Is the Scope of Marijuana Use in the United States? Available online: https://www.drugabuse.gov/publications/research-reports/marijuana/what-scope-marijuana-use-in-united-states (accessed on 16 June 2021).
- Substance Abuse Center for Behavioral Health Statistics and Quality. The 2018 National Survey on Drug Use and Health: Detailed Tables. Available online: https://www.samhsa.gov/data/report/2018-nsduh-detailed-tables (accessed on 23 June 2021).
- National Institute on Drug Abuse. Marijuana Research Report 2020. Available online: https://www.drugabuse.gov/publications/research-reports/marijuana/what-marijuana (accessed on 22 June 2021).
- Krauss, M.J.; Rajbhandari, B.; Sowles, S.J.; Spitznagel, E.L.; Cavazos-Rehg, P. A latent class analysis of poly-marijuana use among young adults. Addict. Behav. 2017, 75, 159–165. [Google Scholar] [CrossRef]
- Pearson, M.R.; Liese, B.S.; Dvorak, R.D. College student marijuana involvement: Perceptions, use, and consequences across 11 college campuses. Addict. Behav. 2016, 66, 83–89. [Google Scholar] [CrossRef]
- Miller, N.S.; Oberbarnscheidt, T.; Gold, M.S. Marijuana Addictive Disorders and DSM-5 Substance-Related Disorders. J. Addict. Res. Ther. 2017, 8, 11. [Google Scholar] [CrossRef]
- Popova, L.; McDonald, E.A.; Sidhu, S.; Barry, R.; Maruyama, T.A.R.; Sheon, N.M.; Ling, P.M. Perceived harms and benefits of tobacco, marijuana, and electronic vaporizers among young adults in Colorado: Implications for health education and research. Addiction 2017, 112, 1821–1829. [Google Scholar] [CrossRef]
- Wong, K.V. Using Marijuana to Cure Marijuana Addiction. Clin. Exp. Psychol. 2017, 3, 2. [Google Scholar] [CrossRef]
- Cascardo, D. Medical Marijuana: To Prescribe or Not to Prescribe? That Is the Question. Med. Pract. Manag. 2020, 14, 201–204. [Google Scholar]
- Di Forti, M.; Quattrone, D.; Freeman, T.; Tripoli, G.; Gayer-Anderson, C.; Quigley, H.; Rodriguez, V.; Jongsma, H.E.; Ferraro, L.; La Cascia, C.; et al. The contribution of cannabis use to variation in the incidence of psychotic disorder across Europe (EU-GEI): A multicentre case-control study. Lancet Psychiatry 2019, 6, 427–436. [Google Scholar] [CrossRef]
- National Institute on Drug Abuse. Marijuana DrugFacts 2019. Available online: https://www.drugabuse.gov/publications/drugfacts/marijuana (accessed on 16 June 2021).
- Berenson, A. Tell Your Children: The Truth About Marijuana, Mental Illness, and Violence; Free Press: New York, NY, USA, 2019. [Google Scholar]
- Zehra, A.; Burns, J.; Liu, C.K.; Manza, P.; Wiers, C.E.; Volkow, N.D.; Wang, G.-J. Cannabis Addiction and the Brain: A Review. J. Neuroimmune Pharmacol. 2018, 13, 438–452. [Google Scholar] [CrossRef]
- Zizlavsky, S.; Alia, D.; Suwento, R.; Siste, K.; Bardosono, S. P300 auditory wave image and its relation to cognitive function in subjects with marijuana addiction: A cross-sectional study in Cipinang and Pondok Bambu Penitentiary, Jakarta. J. Phys. Conf. Ser. 2018, 1073, 042039. [Google Scholar] [CrossRef]
- National Institute on Drug Abuse. Sex and Gender Differences in Substance Use—Substance Use in Women Research Report; National Institute on Drug Abuse: Baltimore, MD, USA, 2020.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion. Obstet. Gynecol. 2017, 130, e205–e209. [Google Scholar]
- Gobbi, G.; Atkin, T.; Zytynski, T.; Wang, S.; Askari, S.; Boruff, J.; Ware, M.; Marmorstein, N.; Cipriani, A.; Dendukuri, N.; et al. Association of Cannabis Use in Adolescence and Risk of Depression, Anxiety, and Suicidality in Young Adulthood. JAMA Psychiatry 2019, 76, 426–434. [Google Scholar] [CrossRef] [PubMed]
- Hasin, D.S.; Saha, T.D.; Kerridge, B.T.; Goldstein, R.; Chou, S.P.; Zhang, H.; Jung, J.; Pickering, R.P.; Ruan, W.J.; Smith, S.M.; et al. Prevalence of Marijuana Use Disorders in the United States Between 2001–2002 and 2012–2013. JAMA Psychiatry 2015, 72, 1235–1242. [Google Scholar] [CrossRef]
- Onaemo, V.N.; Fawehinmi, T.O.; D’Arcy, C. Comorbid Cannabis Use Disorder with Major Depression and Generalized Anxiety Disorder: A Systematic Review with Meta-analysis of Nationally Representative Epidemiological Surveys. J. Affect. Disord. 2020, 281, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Gold, M. Medicinal Marijuana, Stress, Anxiety, and Depression: Primum non nocere. Mo. Med. 2020, 117, 406–411. [Google Scholar] [PubMed]
- Britton, P.C.; Conner, K.R. Suicide Attempts within 12 Months of Treatment for Substance Use Disorders. Suicide Life Threat. Behav. 2010, 40, 14–21. [Google Scholar] [CrossRef]
- Culbreth, R.; Swahn, M.H.; Osborne, M.; Brandenberger, K.; Kota, K. Substance use and deaths by suicide: A latent class analysis of the National Violent Death Reporting System. Prev. Med. 2021, 150, 106682. [Google Scholar] [CrossRef]
- Tetteh, J.; Ekem-Ferguson, G.; Swaray, S.M.; Kugbey, N.; Quarshie, E.N.-B.; Yawson, A.E. Marijuana use and repeated attempted suicide among senior high school students in Ghana: Evidence from the WHO Global School-Based Student Health Survey, 2012. Gen. Psychiatry 2020, 33, e100311. [Google Scholar] [CrossRef]
- Holland, K. CBD vs. THC: What’s the Difference?—2020. Available online: https://www.healthline.com/health/cbd-vs-thc (accessed on 22 June 2021).
- Bridgeman, M.; Abazia, D.T. Medicinal Cannabis: History, Pharmacology, And Implications for the Acute Care Setting. P T Peer Rev. J. Formul. Manag. 2017, 42, 180–188. [Google Scholar]
- Encyclopaedia Britannica. Medical Cannabis. Available online: https://www.britannica.com/science/medical-cannabis (accessed on 30 June 2021).
- Zagorski, N. Be Prepared to Discuss CBD Products With Patients. Psychiatr. News 2020, 55. [Google Scholar] [CrossRef]
- Mudan, A.; DeRoos, F.; Perrone, J. Medical Marijuana Miscalculation. N. Engl. J. Med. 2019, 381, 1086–1087. [Google Scholar] [CrossRef]
- Hazekamp, A. The Trouble with CBD Oil. Med. Cannabis Cannabinoids 2018, 1, 65–72. [Google Scholar] [CrossRef]
- Stuyt, E. The Problem with the Current High Potency THC Marijuana from the Perspective of an Addiction Psychiatrist. Mo. Med. 2018, 115, 482–486. [Google Scholar]
- Center for Behavioral Health Statistics and Quality. 2019 National Survey on Drug Use and Health Public Use File Codebook; Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2020.
- Research Triangle Institute International. 2019 National Survey on Drug Use and Health: Field Interviewer Manual—Field Interviewer Computer Manual; Research Triangle Institute International: Rockville, MD, USA, 2018. [Google Scholar]
- Alshalabi, H.; Tiun, S.; Omar, N.; Albared, M. Experiments on the Use of Feature Selection and Machine Learning Methods in Automatic Malay Text Categorization. Procedia Technol. 2013, 11, 748–754. [Google Scholar] [CrossRef][Green Version]
- Mahmoudi, M.R.; Heydari, M.H.; Qasem, S.N.; Mosavi, A.; Band, S.S. Principal component analysis to study the relations between the spread rates of COVID-19 in high risks countries. Alex. Eng. J. 2021, 60, 457–464. [Google Scholar] [CrossRef]
- Song, F.; Guo, Z.; Mei, D. Feature Selection Using Principal Component Analysis. In 2010 International Conference on System Science, Engineering Design and Manufacturing Informatization; Hubei, Y., Ed.; IEEE Computer Society: Los Angeles, CA, USA, 2010. [Google Scholar]
- Advantages and Disadvantages of Principal Component Analysis in Machine Learning. Available online: http://theprofessionalspoint.blogspot.com/2019/03/advantages-and-disadvantages-of_4.html (accessed on 1 July 2021).
- Nijman, S.W.J.; Hoogland, J.; Groenhof, T.K.J.; Brandjes, M.; Jacobs, J.J.L.; Bots, M.L.; Asselbergs, F.W.; Moons, K.G.M.; Debray, T.P.A. Real-time imputation of missing predictor values in clinical practice. Eur. Heart J. Digit. Health 2020, 2, 154–164. [Google Scholar] [CrossRef]
- Spiess, M.; Kleinke, K.; Reinecke, J. Proper Multiple Imputation of Clustered or Panel Data. In Advances in Longitudinal Survey Methodology; Wiley: Hoboken, NJ, USA, 2021. [Google Scholar]
- James, G.; Witten, D.; Hastie, T.; Tibshirani, R. An Introduction to Statistical Learning; Springer: New York, NY, USA, 2013. [Google Scholar]
- Levy, J.J.; O’Malley, A.J. Don’t dismiss logistic regression: The case for sensible extraction of interactions in the era of machine learning. BMC Med. Res. Methodol. 2020, 20, 171. [Google Scholar] [CrossRef]
- Chen, W.; Xie, X.; Wang, J.; Pradhan, B.; Hong, H.; Bui, D.T.; Duan, Z.; Ma, J. A comparative study of logistic model tree, random forest, and classification and regression tree models for spatial prediction of landslide susceptibility. Catena 2017, 151, 147–160. [Google Scholar] [CrossRef]
- Kesler, S.R.; Rao, A.; Blayney, D.W.; Oakley-Girvan, I.A.; Karuturi, M.; Palesh, O. Predicting Long-Term Cognitive Outcome Following Breast Cancer with Pre-Treatment Resting State fMRI and Random Forest Machine Learning. Front. Hum. Neurosci. 2017, 11, 555. [Google Scholar] [CrossRef]
- Tibaduiza, D.; Torres-Arredondo, M.; Vitola, J.; Anaya, M.; Pozo, F. A Damage Classification Approach for Structural Health Monitoring Using Machine Learning. Complexity 2018, 2018, 5081283. [Google Scholar] [CrossRef]
- Xing, W.; Bei, Y. Medical Health Big Data Classification Based on KNN Classification Algorithm. IEEE Access 2020, 8, 28808–28819. [Google Scholar] [CrossRef]
- Abdel-Rahman, O. Cannabis use among Canadian adults with cancer (2007–2016): Results from a national survey. Expert Rev. Pharm. Outcomes Res. 2020, 1025–1029. [Google Scholar] [CrossRef]
- Anim, E. Investigating the Relationship between Marital Status, Marijuana Use and State Marijuana Laws in the USA; Northern Arizona University: Flagpole, AZ, USA, 2020. [Google Scholar]
- Resident Population of the United States by Sex and Age as of July 1, 2019 (in Million). Available online: https://www.statista.com/statistics/241488/population-of-the-us-by-sex-and-age/ (accessed on 1 July 2021).
- Stanton, R.; To, Q.G.; Khalesi, S.; Williams, S.L.; Alley, S.J.; Thwaite, T.L.; Fenning, A.S.; Vandelanotte, C. Depression, Anxiety and Stress during COVID-19: Associations with Changes in Physical Activity, Sleep, Tobacco and Alcohol Use in Australian Adults. Int. J. Environ. Res. Public Health 2020, 17, 4065. [Google Scholar] [CrossRef]
- Amiri, S.; Behnezhad, S. Alcohol use and risk of suicide: A systematic review and Meta-analysis. J. Addict. Dis. 2020, 38, 200–213. [Google Scholar] [CrossRef] [PubMed]
- Desai, R.; Thakkar, S.; Patel, H.P.; Tan, B.E.-X.; Damarlapally, N.; Haque, F.A.; Farheen, N.; DeWitt, N.; Savani, S.; Parisha, F.J.; et al. Higher odds and rising trends in arrhythmia among young cannabis users with comorbid depression. Eur. J. Intern. Med. 2020, 80, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Mochrie, K.D.; Whited, M.C.; Cellucci, T.; Freeman, T.; Corson, A.T. ADHD, depression, and substance abuse risk among beginning college students. J. Am. Coll. Health 2018, 68, 6–10. [Google Scholar] [CrossRef] [PubMed]
- National Institute on Drug Abuse. Rising Stimulant Deaths Show That We Face More than Just an Opioid Crisis; NIH: Bethesda, MD, USA, 2020.
| Characteristics | n (n = 698) | % | |
|---|---|---|---|
| Gender | Female | 277 | 39.68 |
| Male | 421 | 60.32 | |
| Age | 20–29 | 548 | 78.51 |
| 30–34 | 70 | 10.03 | |
| 35–49 | 80 | 11.46 | |
| Race | NonHispanic White | 364 | 52.15 |
| NonHispanic Black or African American | 100 | 14.33 | |
| NonHispanic | 19 | 2.72 | |
| Native American/Alaska Native | |||
| NonHispanic | 3 | 0.43 | |
| Native HawaiianI/Other Pacific Islander | |||
| NonHispanic Asian | 25 | 3.58 | |
| NonHispanic more than one race | 48 | 6.88 | |
| Hispanic | 139 | 19.91 | |
| Education | 5th–12th grade completed, no diploma | 59 | 8.45 |
| High school diploma/GED | 204 | 29.23 | |
| Some college credit, but no degree | 249 | 35.67 | |
| Associate degree | 64 | 9.17 | |
| College graduate or higher | 122 | 17.48 | |
| Family income | Less than $10,000 | 90 | 12.89 |
| $10,000–$19,999 | 94 | 13.47 | |
| $20,000–$29,999 | 71 | 10.17 | |
| $30,000–$39,999 | 76 | 10.89 | |
| $40,000–$49,999 | 88 | 12.61 | |
| $50,000–$74,999 | 104 | 14.90 | |
| $75,000 or more | 175 | 25.07 | |
| Marital status | Married | 83 | 11.89 |
| Widowed | 2 | 0.29 | |
| Divorced or Separated | 40 | 5.73 | |
| Never Been Married | 573 | 82.09 | |
| Employment | Employed | 487 | 69.77 |
| Unemployed | 100 | 14.33 | |
| No response | 111 | 15.90 | |
| Health Insurance | Covered by any Health Insurance | 560 | 80.23 |
| Not covered | 131 | 18.77 | |
| No response | 7 | 1.00 | |
| Model | Sensitivity | Specificity | Accuracy | 95% CI for Accuracy | AUC | Precision | F1 Score |
|---|---|---|---|---|---|---|---|
| Logistic Regression | 0.690 | 0.632 | 0.635 | 0.593–0.678 | 0.675 | 0.106 | 0.184 |
| RF | 0.771 | 0.773 | 0.773 | 0.753–0.810 | 0.857 | 0.587 | 0.667 |
| KNN | 0.751 | 0.732 | 0.740 | 0.701–0.779 | 0.816 | 0.640 | 0.691 |
| Model | Sensitivity | Specificity | Accuracy | 95% CI for Accuracy | AUC | Precision | F1 Score |
|---|---|---|---|---|---|---|---|
| Logistic Regression | 0.771 | 0.815 | 0.810 | 0.775–0.845 | 0.674 | 0.373 | 0.503 |
| RF | 1.0 | 0.997 | 0.998 | 0.993–1.002 | 1.0 | 0.992 | 0.996 |
| KNN | 0.711 | 0.826 | 0.808 | 0.773–0.843 | 0.845 | 0.429 | 0.535 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, J.; Chung, J.; Choi, J. Exploring Impact of Marijuana (Cannabis) Abuse on Adults Using Machine Learning. Int. J. Environ. Res. Public Health 2021, 18, 10357. https://doi.org/10.3390/ijerph181910357
Choi J, Chung J, Choi J. Exploring Impact of Marijuana (Cannabis) Abuse on Adults Using Machine Learning. International Journal of Environmental Research and Public Health. 2021; 18(19):10357. https://doi.org/10.3390/ijerph181910357
Chicago/Turabian StyleChoi, Jeeyae, Joohyun Chung, and Jeungok Choi. 2021. "Exploring Impact of Marijuana (Cannabis) Abuse on Adults Using Machine Learning" International Journal of Environmental Research and Public Health 18, no. 19: 10357. https://doi.org/10.3390/ijerph181910357
APA StyleChoi, J., Chung, J., & Choi, J. (2021). Exploring Impact of Marijuana (Cannabis) Abuse on Adults Using Machine Learning. International Journal of Environmental Research and Public Health, 18(19), 10357. https://doi.org/10.3390/ijerph181910357







