Burnout Impact of COVID-19 Pandemic on Health-Care Professionals at Assiut University Hospitals, 2020
Abstract
:1. Introduction
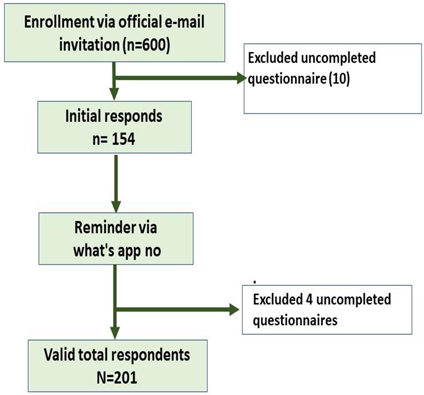
2. Materials and Methods
2.1. Ethical Consideration
2.2. Data Collection Tools
- (a)
- Socio-demographic data of the studied population, such as age, residence, marital status, smoking history, and history of chronic diseases.
- (b)
- Work-related characteristics, such as job title, enrolled department, working system, working hours per day, working days per week, and history of dealing with COVID-19 patients.
- (c)
- Maslach Burnout Inventory (MBI) which is universally accepted as the gold-standard self-reported measure due to its high reliability and validity. As the Cronbach’s α value for the main MBI scale was 0.829, the emotional exhaustion subscale was 0.887, the depersonalization subscale was 0.768, and the diminished personal accomplishment subscale was 0.891 [31]. It was designed to assess the three components of the BOS: emotional exhaustion (EE), depersonalization (DP), and reduced personal accomplishment (PA). It is a 22-item questionnaire on a seven-point Likert-scale (ranging from 0 = never to 6 = every day). Scores for each section were obtained by adding the numeric responses of the items which corresponded to each scale. High scores for the first two dimensions (EE and DP) and low scores for the third dimension (PA) indicated BOS [6]. MBI scores were further used to classify participants as having low (≤17 points), moderate (18–29 points), and high (≥30 points) levels of EE, low (< 6 points), moderate (6–11 points), and high (≥12 points) levels of DP and For PA low (≥40 points), moderate (39–34 points), and high (≤33 points) levels burnout dimensions.
2.3. Procedure
3. Results
3.1. Sociodemographic Characteristics of Enrolled Doctors
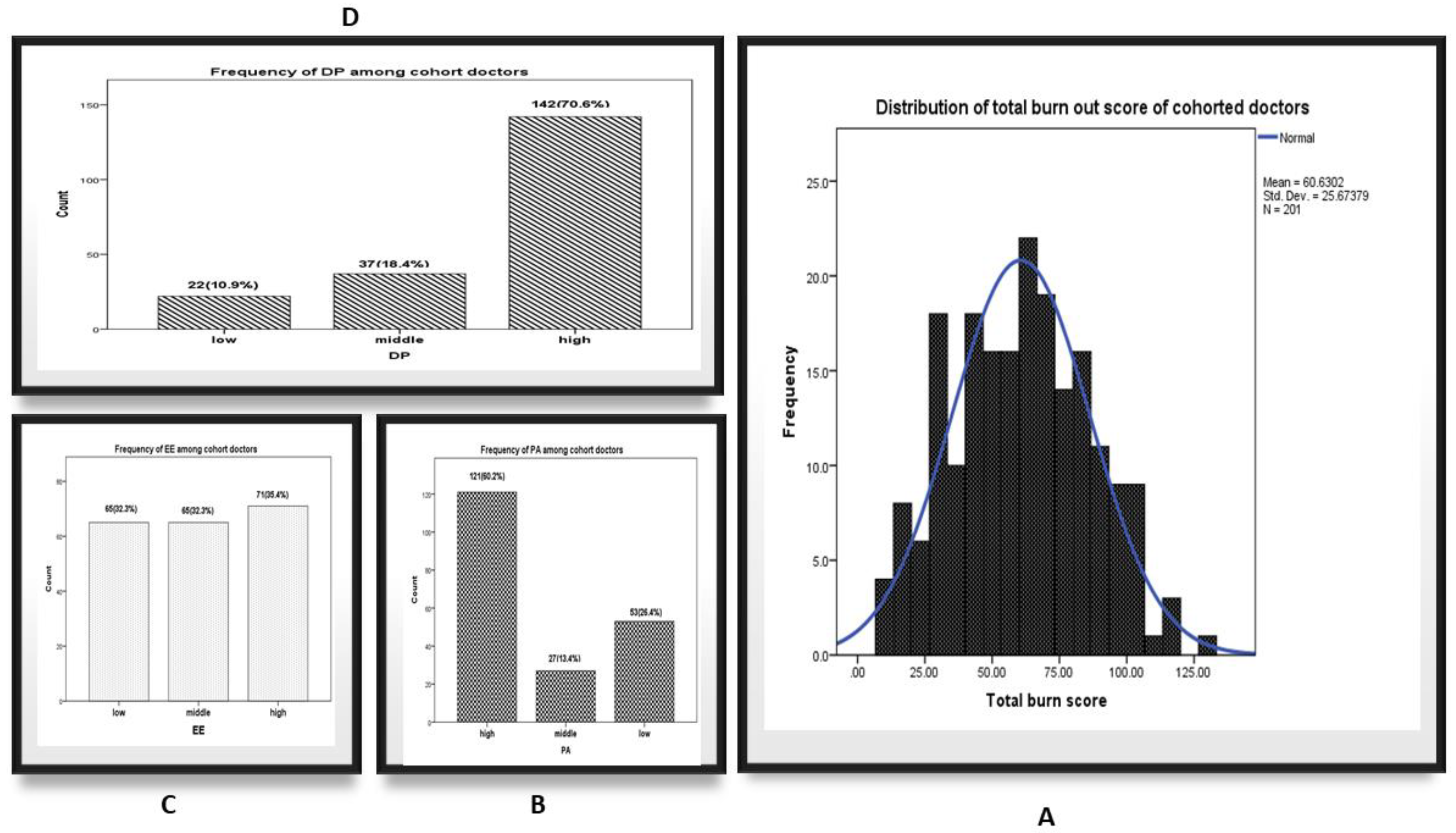
3.2. Figure 1: The Distribution of the Studied Cohort According to Maslach Burnout Inventory (MBI) Categories
3.3. Table 2: The Association between MBI Sub-Scores and Sociodemographic Characters of Cohort Doctors
3.4. Table 3: The Association between MBI Sub Scores with Their Workplace Characteristics and History of COVID-19 Cases Exposure
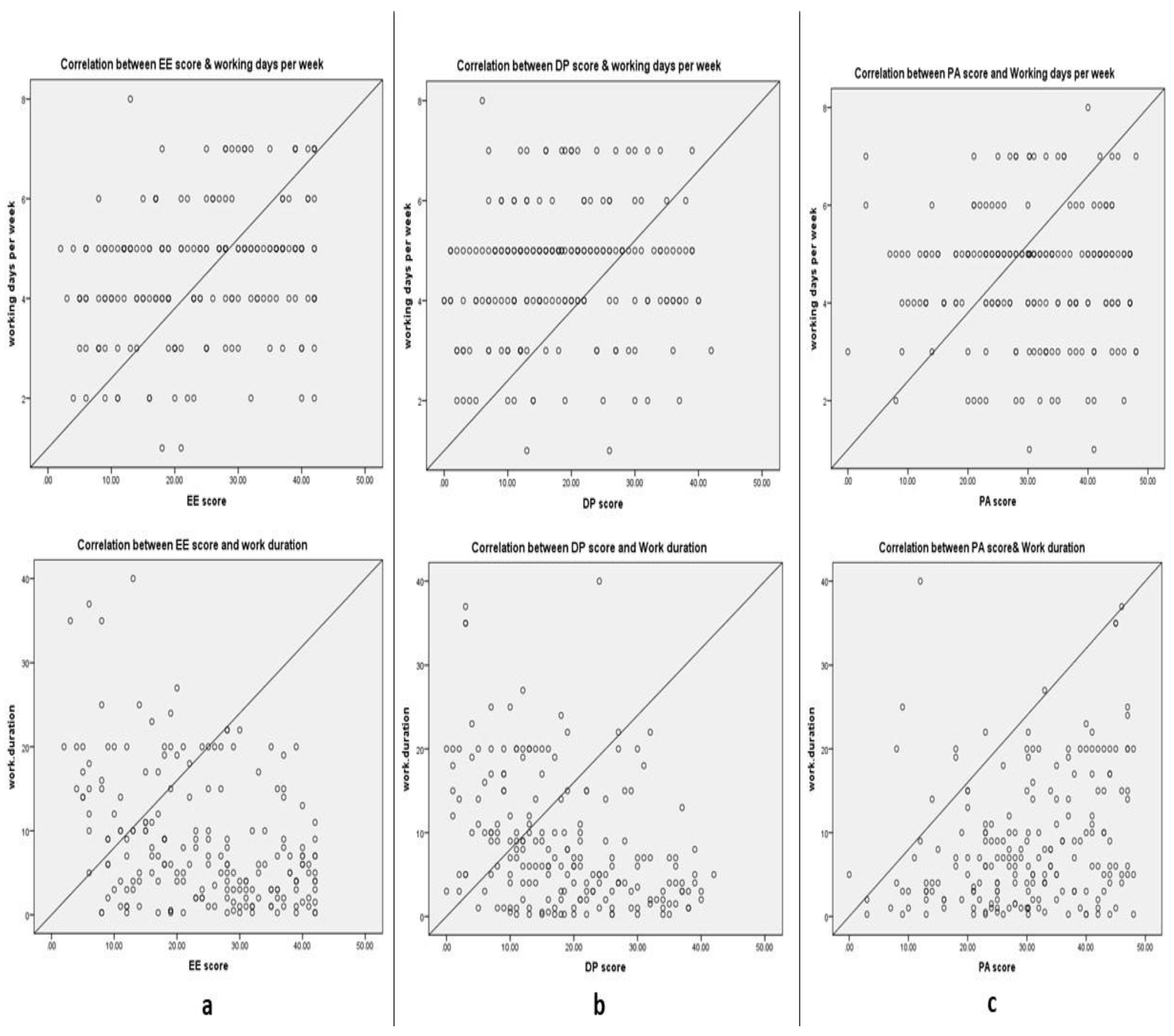
3.5. Figure 2 Correlations between Working Duration and Working Days per Week with Maslach Burnout Inventory Subfield Scores
4. Discussion
5. Conclusions
6. Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Al-Haddad, A.; Al-Omar, F.; Al-Khaleel, A.; Al-Khalaf, A. Prevalence of burnout syndrome and its related risk factors among physicians working in primary health care centers of the Ministry of Health, Al Ahsa region, Saudi Arabia, 2018-2019. J. Fam. Med. Prim. Care 2020, 9, 571–579. [Google Scholar] [CrossRef] [PubMed]
- Embriaco, N.; Papazian, L.; Kentish-Barnes, N.; Pochard, F.; Azoulay, E. Burnout syndrome among critical care healthcare workers. Curr. Opin. Crit. Care 2007, 13, 482–488. [Google Scholar] [CrossRef]
- Almutairi, A.F.; Adlan, A.A.; Balkhy, H.H.; Abbas, O.A.; Clark, A.M. “It feels like I’m the dirtiest person in the world”: Exploring the experiences of healthcare providers who survived MERS-CoV in Saudi Arabia. J. Infect. Public Health 2018, 11, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Talaee, N.; Varahram, M.; Jamaati, H.; Salimi, A.; Attarchi, M.; Dizaji, M.K.; Sadr, M.; Hassani, S.; Farzanegan, B.; Monjazebi, F.; et al. Stress and burnout in health care workers during COVID-19 pandemic: Validation of a questionnaire. J. Public Health 2020, 1–6. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Burn-Out an “Occupational Phenomenon”: International Classification of Diseases. Available online: https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases (accessed on 10 February 2021).
- Maslach, C.; Jackson, S.E.; Leiter, M.P.; Schaufeli, W.B.; Schwab, R.L. Maslach Burnout Inventory Manual, 3rd ed.; Mountain View; Consulting Psychologists Press: Palo Alto, CA, USA, 1996. [Google Scholar]
- Finney, C.; Stergiopoulos, E.; Hensel, J.; Bonato, S.; Dewa, C.S. Organizational stressors associated with job stress and burnout in correctional officers: A systematic review. BMC Public Health 2013, 13, 82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Mol, M.; Kompanje, E.; Benoit, D.; Bakker, J.; Nijkamp, M.D. The Prevalence of Compassion Fatigue and Burnout among Healthcare Professionals in Intensive Care Units: A Systematic Review. PLoS ONE 2015, 10, e0136955. [Google Scholar] [CrossRef]
- Bakker, A.B.; Le Blanc, P.M.; Schaufeli, W.B. Burnout contagion among intensive care nurses. J. Adv. Nurs. 2005, 51, 276–287. [Google Scholar] [CrossRef]
- Moss, M.; Good, V.S.; Gozal, D.; Kleinpell, R.; Sessler, C.N. A Critical Care Societies Collaborative Statement: Burnout Syndrome in Critical Care Health-care Professionals. A Call for Action. Am. J. Respir. Crit. Care Med. 2016, 194, 106–113. [Google Scholar] [CrossRef] [Green Version]
- Doulougeri, K.; Georganta, K.; Montgomery, A. “Diagnosing” burnout among healthcare professionals: Can we find consensus? Cogent Med. 2016, 3, 1237605. [Google Scholar] [CrossRef]
- Abdulrahman, M.; Farooq, M.M.; Al Kharmiri, A.; Al Marzooqi, F.; Carrick, F.R. Burnout and depression among medical residents in the United Arab Emirates: A Multicenter study. J. Fam. Med. Prim. Care 2018, 7, 435–441. [Google Scholar] [CrossRef]
- El-Menyar, A.; Ibrahim, W.H.; El Ansari, W.; Gomaa, M.; Sathian, B.; Hssain, A.A.; Wahlen, B.; Nabir, S.; Al-Thani, H. Characteristics and predictors of burnout among healthcare professionals: A cross-sectional study in two tertiary hospitals. Postgrad. Med. J. 2020. [Google Scholar] [CrossRef] [PubMed]
- Hamed, R.A.; Elaziz, S.Y.A.; Ahmed, A.S. Prevalence and predictors of burnout syndrome, post-traumatic stress disorder, depression, and anxiety in nursing staff in various departments. Middle East Curr. Psychiatry 2020, 27, 1–8. [Google Scholar] [CrossRef]
- Abd-Allah, A.; El-Hawy, L. Burnout and Health Related Quality of Life among Resident Physicians in Zagazig University Hospitals. Egypt. J. Occup. Med. 2019, 43, 189–204. [Google Scholar]
- Dewa, C.S.; Loong, D.; Bonato, S.; Trojanowski, L. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: A systematic review. BMJ Open 2017, 7, e015141. [Google Scholar] [CrossRef]
- Chauhan, S. Comprehensive review of coronavirus disease 2019 (COVID-19). Biomed. J. 2020, 43, 334–340. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. 2020. Available online: https://covid19.who.int/ (accessed on 3 March 2021).
- Wilson, W.; Raj, J.P.; Rao, S.; Ghiya, M.; Nedungalaparambil, N.M.; Mundra, H.; Mathew, R. Prevalence and Predictors of Stress, anxiety, and Depression among Healthcare Workers Managing COVID-19 Pandemic in India: A Nationwide Observational Study. Indian J. Psychol. Med. 2020, 42, 353–358. [Google Scholar] [CrossRef]
- World Health Organization (WHO). What’s Needed Now to Protect Health Workers: WHO COVID-19 Briefing. Available online: https://www.weforum.org/agenda/2020/04/10-april-who-briefing-health-workers-covid-19-ppe-training/ (accessed on 24 December 2020).
- Guo, J.; Lianming, L.; Baoguo, W.; Xiaoqiang, L.; Lianrui, G.; Zhu, T.; Qinghua, G.; Mingyue, Z.; Yingfeng, W.; Jian, Z.; et al. Psychological Effects of COVID-19 on Hospital Staff: A National Cross-Sectional Survey of China Mainland. Soc. Sci. Electron. Publ. 2020, 4, 6–11. [Google Scholar] [CrossRef]
- Montemurro, N. Intracranial hemorrhage and COVID-19, but please do not forget “old diseases” and elective surgery. Brain, Behav. Immun. 2021, 92, 207–208. [Google Scholar] [CrossRef]
- Cucu, A.I.; Turliuc, M.D.; Ciurea, A.V. The COVID-19 emergency does not rule out the diagnostic arsenal in intracerebral hemorrhage: Do not forget the old enemies. Brain Behav. Immun. 2021, 91, 792–793. [Google Scholar] [CrossRef]
- Li, S.; Wang, Y.; Xue, J.; Zhao, N.; Zhu, T. The Impact of COVID-19 Epidemic Declaration on Psychological Consequences: A Study on Active Weibo Users. Int. J. Environ. Res. Public Health 2020, 17, 2032. [Google Scholar] [CrossRef] [Green Version]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef] [PubMed]
- Mukhtar, S. Mental Health and Psychosocial Aspects of Coronavirus Outbreak in Pakistan: Psychological Intervention for Public Mental Health Crisis. Asian J. Psychiatry 2020, 51, 102069. [Google Scholar] [CrossRef] [PubMed]
- SurveyMonkey. Available online: https://www.surveymonkey.com/ (accessed on 14 March 2020).
- CDC Epi Info™. Available online: https://www.cdc.gov/epiinfo/index.html (accessed on 24 December 2020).
- Wu, Y.; Wang, J.; Luo, C.; Hu, S.; Lin, X.; Anderson, A.E.; Bruera, E.; Yang, X.; Wei, S.; Qian, Y. A Comparison of Burnout Frequency among Oncology Physicians and Nurses Working on the Frontline and Usual Wards During the COVID-19 Epidemic in Wuhan, China. J. Pain Symptom Manag. 2020, 60, e60–e65. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull. WHO 2001, 79, 373–374. [Google Scholar]
- Osman, D.; Abdlrheem, S. Burnout and Job Satisfaction among Healthcare Providers in Aswan University Hospital, Upper Egypt. J. High Inst. Public Health 2019, 49, 64–72. [Google Scholar] [CrossRef] [Green Version]
- Batra, K.; Singh, T.P.; Sharma, M.; Batra, R.; Schvaneveldt, N. Investigating the Psychological Impact of COVID-19 among Healthcare Workers: A Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 9096. [Google Scholar] [CrossRef]
- Luceño-Moreno, L.; Talavera-Velasco, B.; García-Albuerne, Y.; Martín-García, J. Symptoms of Posttraumatic Stress, Anxiety, Depression, Levels of Resilience and Burnout in Spanish Health Personnel during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 5514. [Google Scholar] [CrossRef] [PubMed]
- Orrù, G.; Marzetti, F.; Conversano, C.; Vagheggini, G.; Miccoli, M.; Ciacchini, R.; Panait, E.; Gemignani, A. Secondary Traumatic Stress and Burnout in Healthcare Workers during COVID-19 Outbreak. Int. J. Environ. Res. Public Health 2021, 18, 337. [Google Scholar] [CrossRef]
- Dobson, H.; Malpas, C.B.; Burrell, A.J.; Gurvich, C.; Chen, L.; Kulkarni, J.; Winton-Brown, T. Burnout and psychological distress amongst Australian healthcare workers during the COVID-19 pandemic. Australas. Psychiatry 2021, 29, 26–30. [Google Scholar] [CrossRef]
- Drager, L.F.; Pachito, D.V.; Moreno, C.R.C.; Tavares, A.R.; Conway, S.G.; Assis, M.; Sguillar, D.A.; Moreira, G.A.; Bacelar, A.; Genta, P.R. Sleep Disturbances, Anxiety, and Burnout during the COVID-19 Pandemic: A nationwide cross-sectional study in Brazilian Healthcare Professionals. medRxiv 2020, 20190603. [Google Scholar] [CrossRef]
- Barello, S.; Palamenghi, L.; Graffigna, G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. 2020, 290, 113129. [Google Scholar] [CrossRef] [PubMed]
- Duarte, I.; Teixeira, A.; Castro, L.; Marina, S.; Ribeiro, C.; Jácome, C.; Martins, V.; Ribeiro-Vaz, I.; Pinheiro, H.C.; Silva, A.R.; et al. Burnout among Portuguese healthcare workers during the COVID-19 pandemic. BMC Public Health 2020, 20, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S. Burnout and Job Satisfaction in New Zealand Psychiatrists: A National Follow-up Study. Ph.D. Thesis, The University of Auckland, Auckland, New Zealand, 2011. [Google Scholar]
- Terrones-Rodríguez, J.F.; Cisneros-Pérez, V.; Arreola-Rocha, J.J. Burnout syndrome in medical residents at the General Hospital of Durango, México. Rev. Medica Inst. Mex. Seguro Soc. 2016, 54, 242–248. [Google Scholar]
- Ballenger-Browning, K.K.; Schmitz, K.J.; Rothacker, J.A.; Hammer, P.S.; Webb-Murphy, J.A.; Johnson, D.C. Predictors of Burnout Among Military Mental Health Providers. Mil. Med. 2011, 176, 253–260. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jalili, M.; Niroomand, M.; Hadavand, F.; Zeinali, K.; Fotouhi, A. Burnout among healthcare professionals during COVID-19 pandemic: A cross-sectional study. medRxiv 2020, 20129650. [Google Scholar] [CrossRef]
- Khasne, R.W.; Dhakulkar, B.S.; Mahajan, H.C. Burnout among Healthcare Workers during COVID-19 Pandemic in India: Results of a Questionnaire-based Survey. Indian J. Crit. Care Med. 2020, 24, 664–671. [Google Scholar] [CrossRef]
- Mohammed, K.; Ali, E.; Youssef, I.; Fahmy, M.; Haggag, W. Burnout and Personality among Egyptian Residents. Arab J. Psychiatry 2013, 24, 148–160. [Google Scholar] [CrossRef]
- AlDrees, T.M.; AlEissa, S.; Zamakhshary, M.; Badri, M.; Sadat-Ali, M. Physician well-being: Prevalence of burnout and associated risk factors in a tertiary hospital, Riyadh, Saudi Arabia. Ann. Saudi Med. 2013, 33, 451–456. [Google Scholar] [CrossRef] [Green Version]
- Ashkar, K.; Romani, M.; Musharrafieh, U.; Chaaya, M. Prevalence of burnout syndrome among medical residents: Experience of a developing country. Postgrad. Med. J. 2010, 86, 266–271. [Google Scholar] [CrossRef]
- Xiao, X.; Zhu, X.; Fu, S.; Hu, Y.; Li, X.; Xiao, J. Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: A multi-center cross-sectional survey investigation. J. Affect. Disord. 2020, 274, 405–410. [Google Scholar] [CrossRef]
- Salem, M.; Taher, M.; Alsaadi, H. Prevalence and Determinants of Burnout among Primary Healthcare Physicians in Qatar. World Fam. Med. 2018, 16, 22–28. [Google Scholar] [CrossRef]
- Soltan, M.R.; Soliman, S.S.; Al-Hassanin, S.A.; ElSherief, W.A.; Elnaggar, M.S.; Gohar, S.F. Burnout and work stress among medical oncologists: Egyptian multi-centric study. Middle East Curr. Psychiatry 2020, 27, 1–6. [Google Scholar] [CrossRef]
- Farahat, T.M.; Hegazy, N.N.; Mohamed, D.H. Burnout among Physicians in Qalubia Primary Health Care Facilities, Egypt. J. Fam. Med. Health Care 2016, 2, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Mazhar, S.B.; Gilani, S.; Ain, Q.T.; Khan, S. High burn out among doctors working in a tertiary care hospital; a wakeup call. J Pak Med. Assoc. 2019, 69, 349–354. [Google Scholar] [PubMed]
- Montemurro, N. The emotional impact of COVID-19: From medical staff to common people. Brain Behav. Immun. 2020, 87, 23–24. [Google Scholar] [CrossRef] [PubMed]
- Elbarazi, I.; Loney, T.; Yousef, S.; Elias, A. Prevalence of and factors associated with burnout among health care professionals in Arab countries: A systematic review. BMC Health Serv. Res. 2017, 17, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Hamdan, M.; Hamra, A.A. Burnout among workers in emergency Departments in Palestinian hospitals: Prevalence and associated factors. BMC Health Serv. Res. 2017, 17, 407. [Google Scholar] [CrossRef] [Green Version]
- Abbas, A.; Ali, A.; Bahgat, S.; Shouman, W. Prevalence, associated factors, and consequences of burnout among ICU healthcare workers: An Egyptian experience. Egypt. J. Chest Dis. Tuberc. 2019, 68, 514–525. [Google Scholar]
- Abd EL Latief, O.; Mahfouz, E.; Ewis, A.; Seedhom, A. Burnout syndrom among healthcare providers in different hospitals in minya city. Egypt. J. Occup. Med. 2018, 42, 21–31. [Google Scholar]
- Celebi, E. Burnout among Psychiatric Nurses and Associated Factors. Int. J. Basic Sci. Appl. Res. 2014, 3, 765–771. [Google Scholar]
- Sabbah, I.; Sabbah, H.; Sabbah, S.; Akoum, H.; Droubi, N. Burnout among Lebanese nurses: Psychometric properties of the Maslach Burnout Inventory-Human Services Survey (MBI-HSS). Health 2012, 4, 644–652. [Google Scholar] [CrossRef] [Green Version]
- Al-Dubai, S.A.R.; Rampal, K.G. Prevalence and associated factors of burnout among doctors in Yemen. J. Occup. Health 2010, 52, 58–65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hua, D.; Kongb, Y.; Lic, W.; Hand, Q.; Zhange, X.; Zhuf, L.; Wanf, S.; Liuc, Z.; Shenc, Q.; Yangc, J.; et al. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: A large-scale cross-sectional study. EClinicalMedicine 2020, 24, 100424. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Frequency | Percentage |
|---|---|---|
| Gender | ||
| Male/female | 70/131 | 34.8%/65.2% |
| Age group | ||
| 20-/30-/40- | 89/73/39 | 44.3%/36.3%/19.4% |
| Residence | ||
| Urban/rural | 180/21 | 89.6%/10.4% |
| Marital Status | ||
| Single/Married | 78/123 | 38.8%/61.2% |
| Smoking History | ||
| Non-smokers/Smokers | 187/14 | 93%/7% |
| Characteristics | N (%) (N = 201) | Emotional Exhaustion | Depersonalization | Personal Accomplishment | |||
|---|---|---|---|---|---|---|---|
| Mean (SE) | p Value * | Mean (SE) | p Value * | Mean (SE) | p Value * | ||
| Gender | |||||||
| Male | 70 (34.8%) | 22.7 (1.4) | 0.24 | 19.3 (1.4) | 0.74 | 32.7 (1.3) | 0.01 |
| female | 131 (65.2%) | 24.8 (0.9) | 18.1 (0.8) | 28.9 (0.9) | |||
| Age group | |||||||
| 20- | 89 (44.3%) | 28.3 (1.1) | <0.001 | 22.9 (1.0) | <0.001 | 27.1 (1.2) | <0.001 |
| 30- | 73 (36.3%) | 22.5 (1.3) | 16.7 (1.2) | 30.6 (1.1) | |||
| 40- | 39 (19.4%) | 17.5 (1.6) | 1.6 (1.4) | 36.7 (1.7) | |||
| Residence | |||||||
| Urban | 180 (89.6%) | 24.2 (0.8) | 0.72 | 18.6 (0.8) | 0.65 | 30.2 (0.8) | 0.75 |
| Rural | 21 (10.4%) | 23.1 (2.8) | 17.3 (2.1) | 31.2 (2.3) | |||
| Marital Status | |||||||
| Single | 78 (38.8%) | 26.6 (1.1) | 0.01 | 22.8 (1.1) | <0.001 | 27.1 (1.1) | 0.001 |
| Married | 123 (61.2%) | 22.5 (1.1) | 15.7 (0.9) | 32.2 (0.9) | |||
| Smoking History | |||||||
| Non-smokers | 187 (93%) | 24.2 (0.8) | 0.56 | 18.3 (0.8) | 0.48 | 30.2 (0.8) | 0.95 |
| Smokers | 14 (7%) | 22.4 (2.9) | 20.7 (3.1) | 30.9 (2.5) | |||
| Chronic disease | |||||||
| Yes | 31 (15.4%) | 24.3 (2.2) | 0.90 | 19.5 (2.2) | 0.70 | 32.2 (2.1) | 0.25 |
| No | 170 (84.6%) | 24.1 (0.8) | 18.3 (0.8) | 29.8 (0.8) | |||
| Characteristics | N (%) (N = 201) | Emotional Exhaustion | Depersonalization | Personal Accomplishment | |||
|---|---|---|---|---|---|---|---|
| Mean (SE) | p Value * | Mean (SE) | p Value * | Mean (SE) | p Value * | ||
| Job title | |||||||
| Resident doctor | 67 (33.3%) | 27.4 (1.3) | 0.01 | 23.6 (1.3) | <0.001 | 26.1 (1.4) | <0.001 |
| Assistant lecturer | 74 (36.8%) | 25.9 (1.2) | 19.0 (1.1) | 29.9 (1.2) | |||
| Specialist/Lecturer | 25 (12.4%) | 18.7 (2.3) | 12.5 (1.5) | 34.5 (1.8) | |||
| Assistant prof/Professors | 35 (17.4%) | 17.9 (1.6) | 11.9 (1.4) | 35.8 (1.8) | |||
| Working specialty: | |||||||
| Medical | 92 (45.8%) | 22.9 (1.1) | 0.41 | 17.2 (0.9) | 0.37 | 31.9 (1.1) | <0.001 |
| Surgical/Anesthesia and ICU | 59 (29.4%) | 24.9 (1.6) | 19.8 (1.6) | 32.8 (1.5) | |||
| Academic | 50 (24.9%) | 25.2 (1.5) | 19.3 (1.5) | 23.9 (1.5) | |||
| Direct exposure with COVID-19 case | |||||||
| Yes | 63 (31.3%) | 26.1 (1.4) | 0.08 | 21.6 (1.4) | 0.01 | 30.7 (1.3) | 0.78 |
| No | 23.1 (0.9) | 17.1 (0.8) | 30.0 (0.9) | ||||
| Working system | |||||||
| Morning Shifts | 85 (42.3%) | 22.4 (1.2) | 0.06 | 16.5 (1.2) | 0.02 | 31.3 (1.1) | 0.24 |
| Mixed shifts | 115 (57.5%) | 25.4 (1.1) | 19.9 (0.9) | 29.4 (1.1) | |||
| Working hours per day | |||||||
| <4 h | 26 (12.9%) | 15.8 (2.2) | <0.001 | 11.5 (1.8) | <0.001 | 34.6 (1.9) | 0.04 |
| 4–8 h | 95 (47.3%) | 23.2 (1.1) | 16.3 (0.9) | 30.6 (1.1) | |||
| >8 h | 80 (39.8%) | 27.8 (1.2) | 23.3 (1.1) | 28.3 (1.3) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elghazally, S.A.; Alkarn, A.F.; Elkhayat, H.; Ibrahim, A.K.; Elkhayat, M.R. Burnout Impact of COVID-19 Pandemic on Health-Care Professionals at Assiut University Hospitals, 2020. Int. J. Environ. Res. Public Health 2021, 18, 5368. https://doi.org/10.3390/ijerph18105368
Elghazally SA, Alkarn AF, Elkhayat H, Ibrahim AK, Elkhayat MR. Burnout Impact of COVID-19 Pandemic on Health-Care Professionals at Assiut University Hospitals, 2020. International Journal of Environmental Research and Public Health. 2021; 18(10):5368. https://doi.org/10.3390/ijerph18105368
Chicago/Turabian StyleElghazally, Shimaa A., Atef F. Alkarn, Hussein Elkhayat, Ahmed K. Ibrahim, and Mariam Roshdy Elkhayat. 2021. "Burnout Impact of COVID-19 Pandemic on Health-Care Professionals at Assiut University Hospitals, 2020" International Journal of Environmental Research and Public Health 18, no. 10: 5368. https://doi.org/10.3390/ijerph18105368
APA StyleElghazally, S. A., Alkarn, A. F., Elkhayat, H., Ibrahim, A. K., & Elkhayat, M. R. (2021). Burnout Impact of COVID-19 Pandemic on Health-Care Professionals at Assiut University Hospitals, 2020. International Journal of Environmental Research and Public Health, 18(10), 5368. https://doi.org/10.3390/ijerph18105368






