A Transnational and Transregional Study of the Impact and Effectiveness of Social Distancing for COVID-19 Mitigation
Abstract
:1. Introduction
2. Material and Methods
2.1. Effective Reproduction Number
2.2. Infection Rate
2.3. Social Distancing Metric
2.4. Spearman’s Rank-Order Correlation
2.5. Data Sources
- Population by age for Europe: World Population Prospects—United Nations—Available online: https://population.un.org/wpp (accessed on 4 September 2021).
- Time series of deaths and cases by country: World Health Organization—Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 4 September 2021).
- Time series of cases and deaths by US counties and states: New York Times COVID-19 Tracker dataset—Available online: https://raw.githubusercontent.com/nytimes/covid-19-data/master/us-counties.csv (accessed on 4 September 2021).
- Population by age group in US counties and states: United States Census Bureau—Available online: https://www.census.gov/data/tables/time-series/demo/popest/2010s-counties-detail.html (accessed on 4 September 2021).
- Data on days of mask mandate in the US: Center for Disease Control and Prevention—Available online: https://data.cdc.gov/Policy-Surveillance/U-S-State-and-Territorial-Public-Mask-Mandates-Fro/62d6-pm5i (accessed on 4 September 2021).
- Population by age group for Brazilian municipalities and states: Brazilian Institute for Geography and Statistics—Available online: https://brasilemsintese.ibge.gov.br/populacao (accessed on 4 September 2021).
- Time series for cases and deaths by COVID-19 by municipality and state in Brazil: Brazilian Ministry of Health—Available online: https://covid.saude.gov.br (accessed on 4 September 2021).
- Detailed data on vaccination in Brazil: Brazilian Ministry of Health—Available online: https://opendatasus.saude.gov.br/dataset/covid-19-vacinacao (accessed on 4 September 2021).
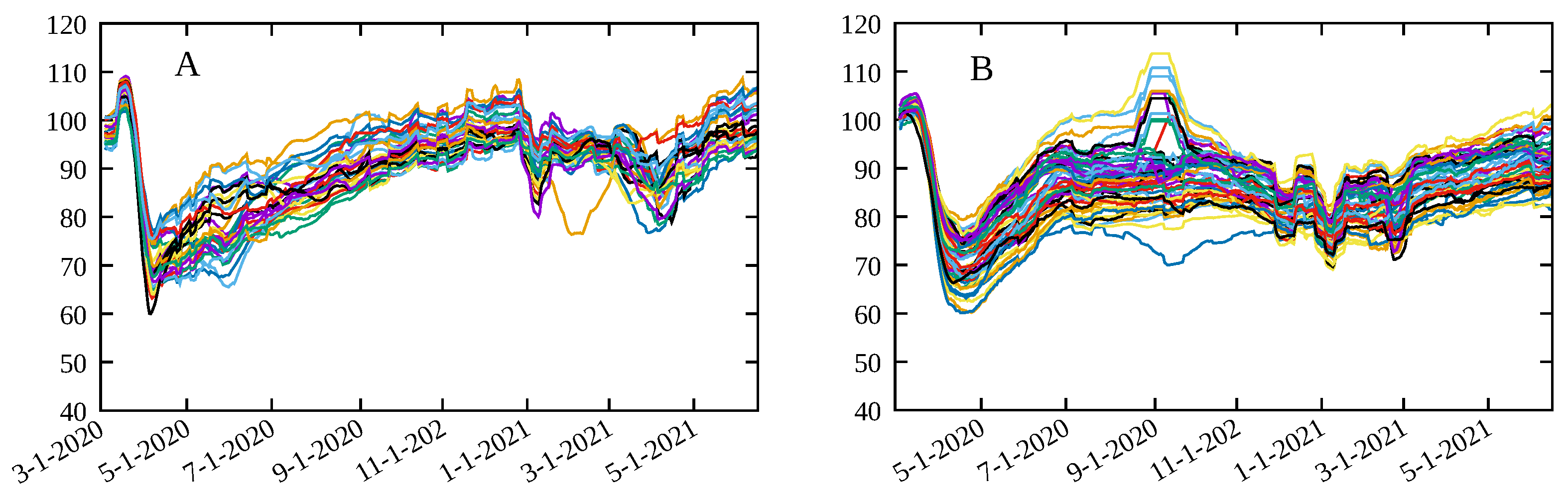
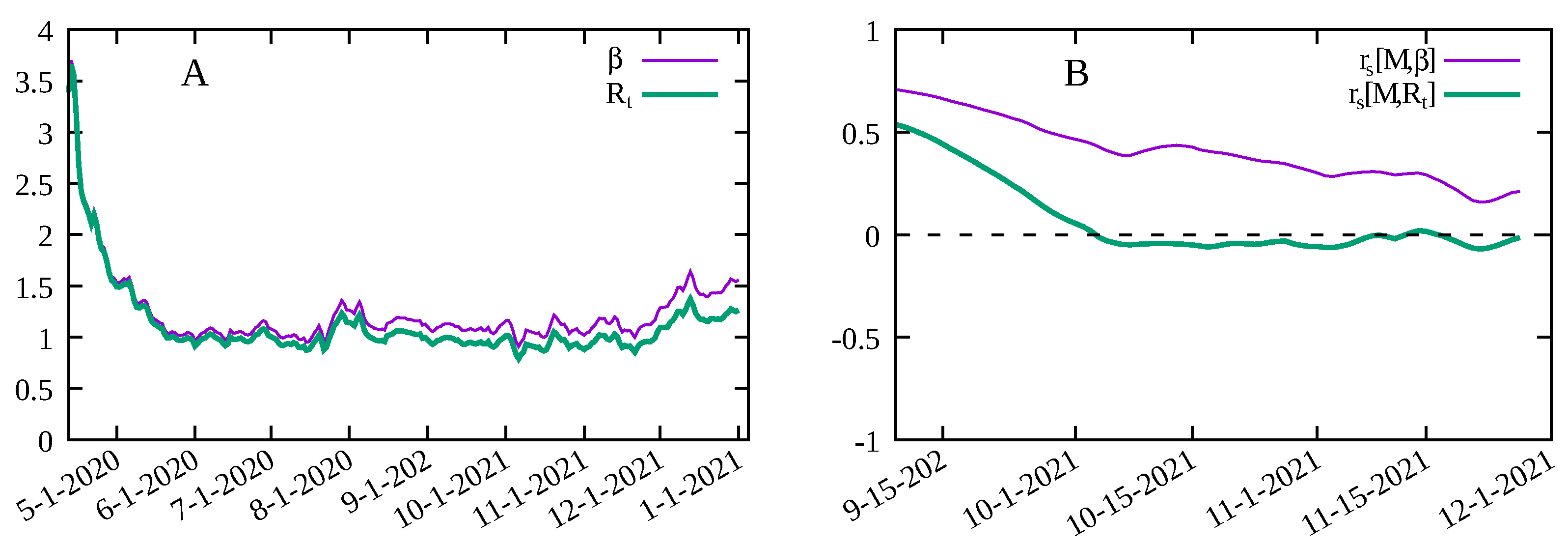
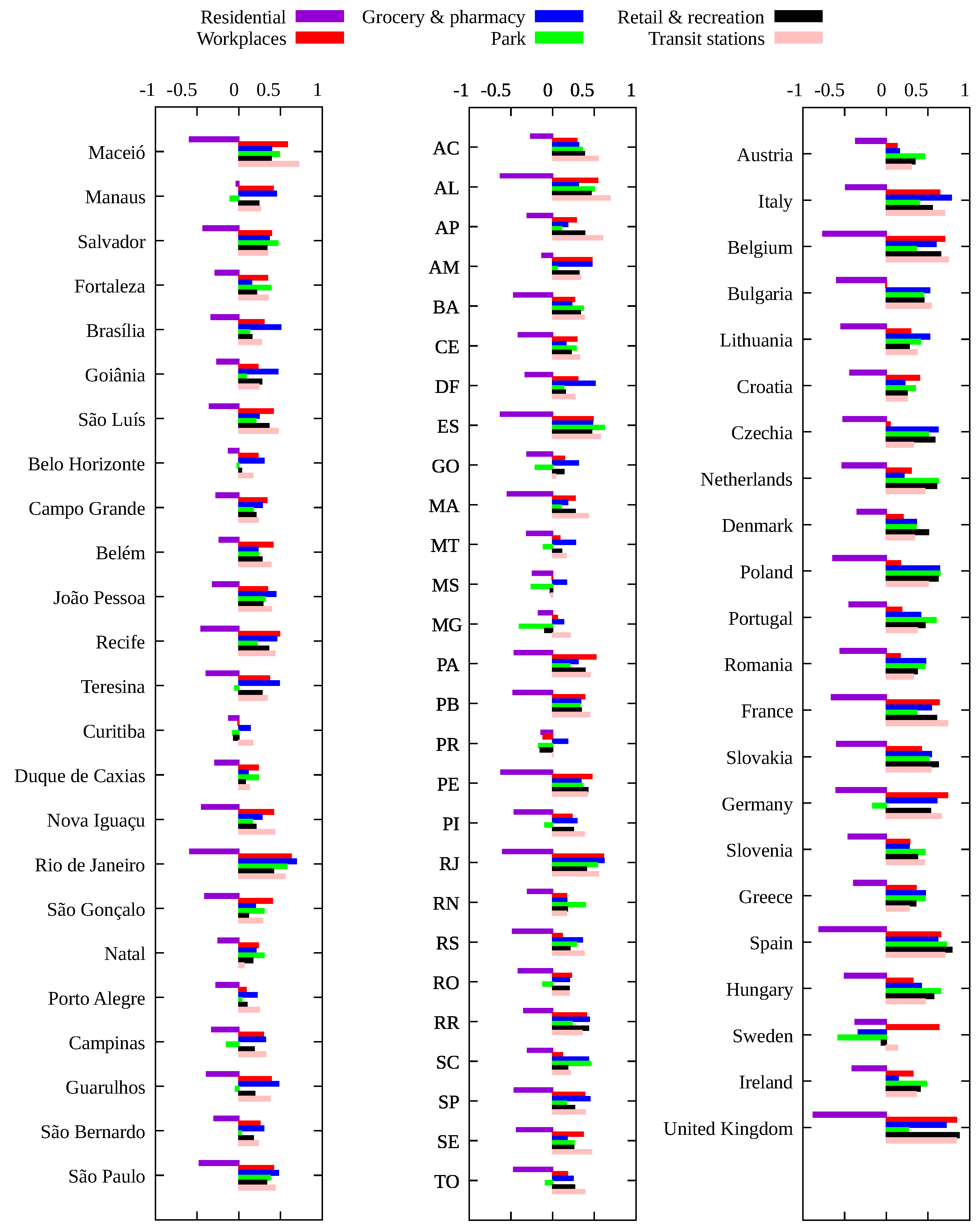
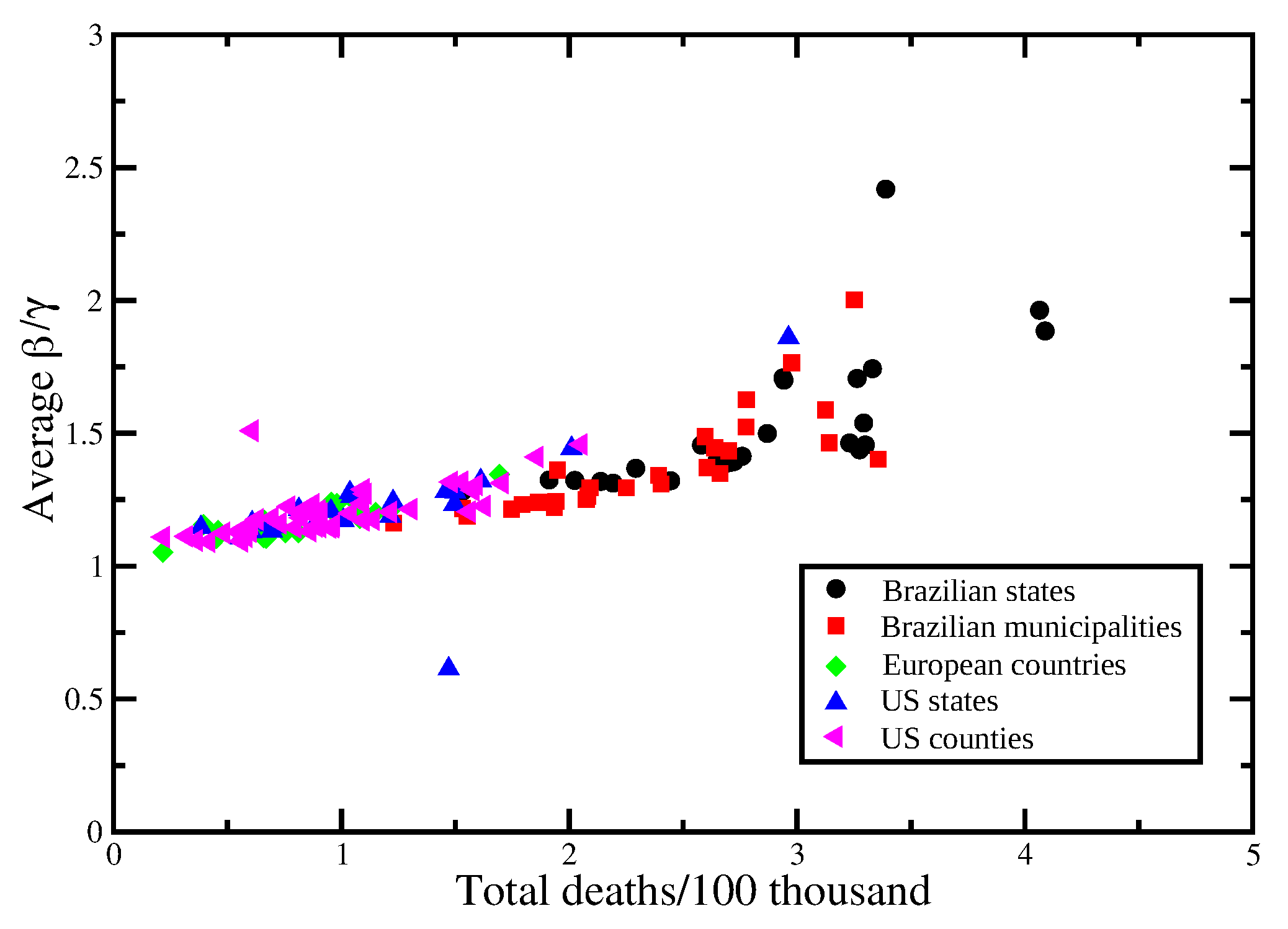
3. Results and Discussion
- All 50 US states, from the first reported case up to 20 December 2020;
- The 24 US counties with a population of at least one million and at least 1000 deaths in 2020 (Nassau was not considered due to inconsistent data for the number of deaths), from the first reported case in each county up to 20 December 2020;
- All 27 Brazilian states, from 26 February 2020 to 14 June 2021;
- The 22 Brazilian cities (municipalities) with a population of at least 750 thousand from 26 February 2020 to 14 June 2021;
- All countries in the European Economic Community and the United Kingdom with Google Mobility data and at least one thousand deaths by COVID-19 in 2020, from 1 March 2020 to 31 December 2020, with a total of 22 countries.
4. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Epidemiological Model
| Variable | Description |
|---|---|
| Susceptible individuals | |
| Exposed individuals (non-contagious) | |
| Infected symptomatic individuals (contagious) | |
| Asymptomatic symptomatic individuals (contagious) | |
| Hospitalized individuals | |
| Vaccinated individual with l doses with vaccine of type k without primary vaccination failure | |
| Vaccinated individual with l doses with vaccine of type k with primary vaccination failure | |
| Recovered individuals. | |
| Individuals vaccinated per unit of time with the l-th dose of vaccine of type k. | |
| Efficacy of vaccine of type k withe l doses. |
References
- John Hopkins University. John Hopkins Coronavirus Resource Center. 2021. Available online: https://coronavirus.jhu.edu/map.html (accessed on 4 September 2021).
- Perra, N. Non-pharmaceutical interventions during the COVID-19 pandemic: A review. Phys. Rep. 2021, 913, 1. [Google Scholar] [CrossRef] [PubMed]
- Chiesa, V.; Antony, G.; Wismar, M.; Rechel, B. COVID-19 pandemic: Health impact of staying at home, social distancing and ‘lockdown’ measures—A systematic review of systematic reviews. J. Public Health 2021, 43, e462–e481. [Google Scholar] [CrossRef]
- Margraf, J.; Brailovskaia, J.; Schneider, S. Adherence to behavioral COVID-19 mitigation measures strongly predicts mortality. PLoS ONE 2021, 16, e0249392. [Google Scholar] [CrossRef]
- Zhang, J.; Litvinova, M.; Liang, Y.; Wang, Y.; Wang, W.; Zhao, S. Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science 2021, 368, 1481. [Google Scholar] [CrossRef] [PubMed]
- Thu, T.P.B.; Ngoc, P.N.H.; Hai, N.M.; Tuan, L. Effect of the social distancing measures on the spread of COVID-19 in 10 highly infected countries. Sci. Total Environ. 2020, 742, 140430. [Google Scholar] [CrossRef] [PubMed]
- Ayouni, I.; Maatoug, J.; Dhouib, W.; Zammit, N.; Fredj, S.B.; Ghammam, R.; Ghannem, H. Effective public health measures to mitigate the spread of COVID-19: A systematic review. BMC Public Health 2021, 21, 1015. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Wang, S.; Hu, T.; Fu, X.; Wang, X.; Hu, Y.; Halloran, B.; Cui, Y.; Liu, H.; Liu, Z.; et al. Human mobility and COVID-19 transmission: A systematic review and future directions. medRxiv 2021. [Google Scholar] [CrossRef]
- Oh, J.; Lee, H.Y.; Khuong, Q.L.; Markuns, J.F.; Bullen, C.; Barrios, O.E.A.; Hwang, S.-S.; Suh, Y.S.; McCool, J.; Kachur, S.P.; et al. Mobility restrictions were associated with reductions in COVID-19 incidence early in the pandemic: Evidence from a real-time evaluation in 34 countries. Sci. Rep. 2021, 11, 13717. [Google Scholar] [CrossRef]
- Mendez-Brito, A.; Bcheraoui, C.E.; Pozo-Martina, F. Systematic review of empirical studies comparing the effectiveness of non-pharmaceutical interventions against COVID-19. J. Infect. 2021, 83, 281. [Google Scholar] [CrossRef]
- Chinazzi, M.; Davis, J.T.; Ajelli, M.; Gioannini, C.; Litvinova, M.; Merler, S.; y Pionti, A.P.; Mu, K.; Rossi, L.; Sun, K.; et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science 2020, 368, 395. [Google Scholar] [CrossRef] [Green Version]
- Jarvis, C.I.; Van Zandvoor, K.; Gimma, A.; Prem, K.; working group, C.C.; Klepac, P.; Rubin, G.J.; Edmunds, W.J. Quantifying the impact of physical distance measures on the transmission of COVID-19 in the UK. BMC Med. 2020, 18, 124. [Google Scholar] [CrossRef]
- Badr, H.S.; Du, H.; Marshall, M.; Dong, E.; Squire, M.M.; Gardner, L.M. Association between mobility patterns and COVID-19 transmission in the USA: A mathematical modelling study. Lancet Infect. Dis. 2020, 20, 1247. [Google Scholar] [CrossRef]
- Candido, D.S.; Claro, I.M.; Jesus, J.G.; Souza, W.M.; Moreira, F.R.R.; Dellicour, S. Evolution and epidemic spread of SARS-CoV-2 in Brazil. Science 2020, 369, 1255. [Google Scholar] [CrossRef] [PubMed]
- Wellenius, G.A.; Vispute, S.; Espinosa, V.; Fabrikant, A.; Tsai, T.C.; Hennessy, J. Impacts of social distancing policies on mobility and COVID-19 case growth in the US. Nat. Commun. 2021, 12, 3118. [Google Scholar] [CrossRef]
- Singh, B.B.; Lowerison, M.; Lewinson, R.T.; Vallerand, I.A.; Deardon, R.; Gill, J.P.S.; Sing, B.; Barkema, H.W. Public health interventions slowed but did not halt the spread of COVID-19 in India. Transbound. Emerg. Dis. 2021, 68, 2171. [Google Scholar] [CrossRef] [PubMed]
- Nouvellet, P.; Bhatia, S.; Cori, A.; Ainslie, K.E.C.; Baguelin, M.; Bhatt, S. Reduction in mobility and COVID-19 transmission. Nat. Commun. 2021, 12, 1090. [Google Scholar] [CrossRef] [PubMed]
- Yilmazkuday, H. Stay-at-home works to fight against COVID-19: International evidence from Google mobility data. J. Hum. Behav. Soc. Environ. 2021, 31, 210. [Google Scholar] [CrossRef]
- Nova, A.C.; Ferreira, P.; Almeira, D.; Dionísio, A.; Quintino, D. Are Mobility and COVID-19 Related? A Dynamic Analysis for Portuguese Districts. Entropy 2021, 23, 786. [Google Scholar] [CrossRef]
- Gatalo, O.; Tseng, K.; Hamilton, A.; Lin, G.; Klein, E. Associations between phone mobility data and COVID-19 cases. Lancet Infect. Dis. 2020, 21, E111. [Google Scholar] [CrossRef]
- Fraser, C. Estimating Individual and Household Reproduction Numbers in an Emerging Epidemic. PLoS ONE 2007, 2, e758. [Google Scholar] [CrossRef]
- Russell, T.W.; Hellewell, J.; Jarvis, C.I.; van Zandvoort, K.; Abbott, S.; Ratnayake, R.; Flasche, S.; Eggo, R.M.; Edmunds, W.J.; CMMID COVID-19 working group; et al. Estimatins the infection and case fatality ratio for coronavirus disease (COVID-19) using age-adjusted data from the outbreak on the Diamond Princess cruise ship, February 2020. Eurosurveillance 2020, 25, 2000256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verity, R.; Okell, L.C.; Dorigatti, I. Estimates of the severity of coronavirus disease 2019: A model-based analysis. Lancet Infect. Dis. 2020, 20, 669. [Google Scholar] [CrossRef]
- Kermack, W.O.; McKendrick, A.G. A contribution to the mathematical theory of epidemics. Proc. R. Soc. A 1927, 115, 700. [Google Scholar] [CrossRef] [Green Version]
- Li, R.; Pei, S.; Chen, B.; Song, Y.; Zhang, T.; Yang, W.; Shaman, J. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2). Science 2020, 368, 489. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Google. Google COVID-19 Comunity Mobility Reports. 2021. Available online: https://www.google.com/covid19/mobility/ (accessed on 4 September 2021).
- Teralytics. Teralytics Matrix; Teralytics: Zürich, Switzerland, 2021. [Google Scholar]
- Unacast. Unacast Social Distancing Scorecard, 2021. Available online: https://www.unacast.com/covid19/social-distancing-scoreboard (accessed on 4 September 2021).
- Apple. Apple Mobility Trends, 2021. Available online: https://covid19.apple.com/mobility (accessed on 4 September 2021).
- Myers, J.L.; Well, A.D. Research Design and Statistical Analysis; Lawrence Erlbaum: London, UK, 2003. [Google Scholar]
- Rocha-Filho, T.M.; Mendesc, J.F.F.; Chow, C.C.; Phillips, J.C.; Cordeiro, A.J.A.; Scorza, F.A.; Almeidai, A.C.G.; Mendes, J.F.F. A data-driven model for COVID-19 pandemic—Evolution of the attack rate and prognosis for Brazil. Chaos Solitons Fractals 2021, 152, 111359. [Google Scholar] [CrossRef]
- Lachassinne, E.; de Pontual, L.; Caseris, M.; Lorrot, M.; Guilluy, C.; Naud, A.; Dommergues, M.A.; Pinquier, D. SARS-CoV-2 transmission among children and staff in daycare centres during a nationwide lockdown in France: A cross-sectional, multicentre, seroprevalence study. Lancet Child Adolesc. Health 2021, 5, 256. [Google Scholar] [CrossRef]
- Jrahmandad, J.; Lim, T.Y.; Sterman, J. Behavioral dynamics of COVID-19: Estimating under-reporting, multiple waves, and adherence fatigue across 92 nations. SSRN 2021. [Google Scholar] [CrossRef]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Filho, T.M.R.; Moret, M.A.; Mendes, J.F.F. A Transnational and Transregional Study of the Impact and Effectiveness of Social Distancing for COVID-19 Mitigation. Entropy 2021, 23, 1530. https://doi.org/10.3390/e23111530
Filho TMR, Moret MA, Mendes JFF. A Transnational and Transregional Study of the Impact and Effectiveness of Social Distancing for COVID-19 Mitigation. Entropy. 2021; 23(11):1530. https://doi.org/10.3390/e23111530
Chicago/Turabian StyleFilho, Tarcísio M. Rocha, Marcelo A. Moret, and José F. F. Mendes. 2021. "A Transnational and Transregional Study of the Impact and Effectiveness of Social Distancing for COVID-19 Mitigation" Entropy 23, no. 11: 1530. https://doi.org/10.3390/e23111530
APA StyleFilho, T. M. R., Moret, M. A., & Mendes, J. F. F. (2021). A Transnational and Transregional Study of the Impact and Effectiveness of Social Distancing for COVID-19 Mitigation. Entropy, 23(11), 1530. https://doi.org/10.3390/e23111530







