Working Hours, Job Burnout, and Subjective Well-Being of Hospital Administrators: An Empirical Study Based on China’s Tertiary Public Hospitals
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Procedures
2.2. Measures
2.2.1. Demographics
2.2.2. Working Hours
2.2.3. Job Burnout
2.2.4. Subjective Well-Being (SWB)
2.3. Ethics Statement
2.4. Data Analysis
3. Results
3.1. The Scores of Various Dimensions of Job Burnout among Hospital Administrators
3.2. Demographic Distribution of Job Burnout and SWB among Hospital Administrators
3.3. Correlation Analysis between SWB and Various Factors of Working Hours and Job Burnout in Hospital Administrators
3.4. Testing of Common Deviation Method
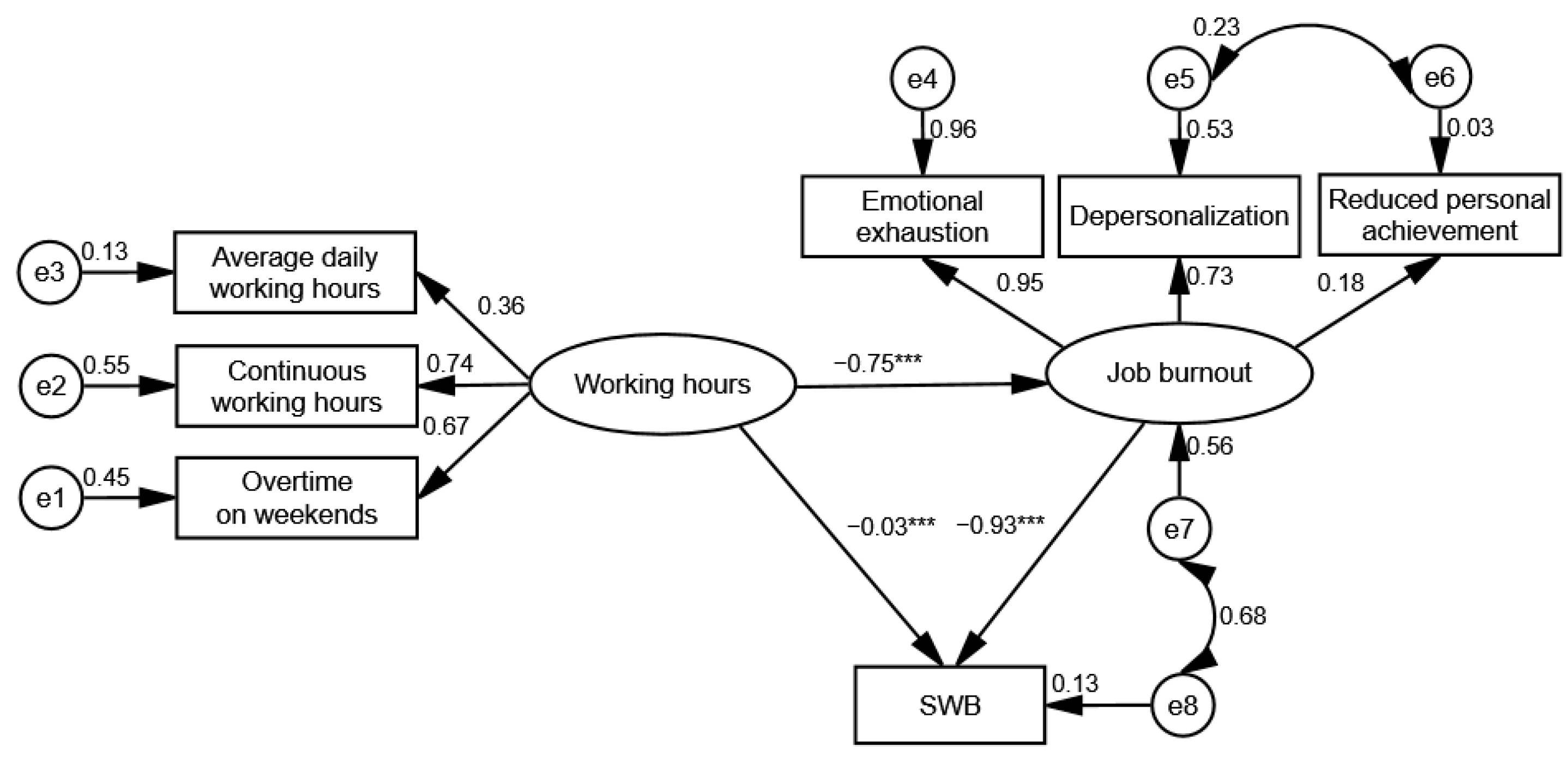
3.5. Mediating Effect of Job Burnout between Working Hours and SWB
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chang, H.H.; Lin, R.T. Policy changes for preventing and recognizing overwork-related cardiovascular diseases in taiwan: An overview. J. Occup. Health 2019, 1, 1–10. [Google Scholar] [CrossRef]
- Thompson, S.L.; Salmon, J.W. Strikes by physicians: A historical perspective toward an ethical evaluation. Int. J. Health Serv. 2006, 36, 331–354. [Google Scholar] [CrossRef]
- Wang, Q.Y.; Tang, C.M. Analysis of the state of overwork of the medical staff in tertiary hospitals and its influence. Chin. Hosp. Manag. 2018, 38, 71–73. (In Chinese) [Google Scholar]
- Baldwin, P.J.; Dodd, M.; Wrate, R.M. Young doctors’ health—ii. Health and health behaviour. Soc. Sci. Med. 1997, 45, 41–44. [Google Scholar] [CrossRef]
- Dick, B.M. Emotional distress in junior house officers. Brit. Med. J. 1987, 295, 780–781. [Google Scholar] [CrossRef][Green Version]
- Chang, R.-E.; Yu, T.-H.; Shih, C.-L. The number and composition of work hours for attending physicians in taiwan. Sci. Rep. 2020, 10, 14934–14945. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E. The measurement of experienced burnout. J. Organ. Behav. 1981, 2, 99–113. [Google Scholar] [CrossRef]
- Chen, H.; Liu, F.; Pang, L.; Liu, F.; Gu, X. Are you tired of working amid the pandemic? The role of professional identity and job satisfaction against job burnout. Int. J. Environ. Res. Public. Health 2020, 17, 9188. [Google Scholar] [CrossRef] [PubMed]
- Adan, J.C.M.; Jimenez, B.M.; Herrer, M.G. Burnout and the health of the medical professionals: Review and preventive options. Med. Clin. (Barc.) 2004, 123, 265–270. [Google Scholar]
- Sofology, M.; Efstratopoulou, M.; Dunn, T. Predicting burnout syndrome in greek mental health professionals. J. Soci. Serv. Res. 2019, 45, 142–149. [Google Scholar] [CrossRef]
- Hamdan, M.; Hamra, A.A. Burnout among workers in emergency departments in palestinian hospitals: Prevalence and associated factors. BMC Health Serv. Res. 2017, 17, 407–414. [Google Scholar] [CrossRef]
- Elbarazi, I.; Loney, T.; Yousef, S.; Elias, A. Prevalence of and factors associated with burnout among health care professionals in arab countries: A systematic review. BMC Health Serv. Res. 2017, 17, 491–501. [Google Scholar] [CrossRef]
- Ramirez, M.R.; Otero, P.; Blanco, V.; Ontaneda, M.P.; Diaz, O.; Vazquez, F.L. Prevalence and correlates of burnout in health professionals in ecuador. Compr. Psychiatry 2018, 82, 73–83. [Google Scholar] [CrossRef]
- Thorsen, V.C.; Tharp, A.L.T.; Meguid, T. High rates of burnout among maternal health staff at a referral hospital in malawi: A cross-sectional study. BMC Nurs. 2011, 10, 1–7. [Google Scholar] [CrossRef]
- Zutautiene, R.; Radisauskas, R.; Kaliniene, G.; Ustinaviciene, R. The prevalence of burnout and its associations with psychosocial work environment among kaunas region (lithuania) hospitals’ physicians. Int. J. Environ. Res. Public Health 2020, 17, 3739. [Google Scholar] [CrossRef]
- Lo, D.; Wu, F.; Chan, M.; Chu, R.; Li, D. A systematic review of burnout among doctors in China: A cultural perspective. Asia Pac. Fam. Med. 2018, 17, 1–13. [Google Scholar] [CrossRef]
- Wang, H.; Jin, Y.; Wang, D.; Zhao, S.; Sang, X.; Yuan, B. Job satisfaction, burnout, and turnover intention among primary care providers in rural china: Results from structural equation modeling. BMC Fam. Peact. 2020, 21, 12–22. [Google Scholar] [CrossRef]
- World Health Organization. Health 2020. In A European Policy Framework and Strategy for the 21st Century; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Sletta, C.; Tyssen, R.; Løvseth, L. Change in subjective well-being over 20 years at two norwegian medical schools and factors linked to well-being today: A survey. BMC Med. Educ. 2019, 19, 45–57. [Google Scholar] [CrossRef]
- Qian, G. Associations between longevity and subjective well-being by country. Curr. Sci. 2017, 112, 941–945. [Google Scholar] [CrossRef]
- Malone, C.; Wachholtz, A. The relationship of anxiety and depression to subjective well-being in a mainland chinese sample. J. Relig. Health 2018, 57, 266–278. [Google Scholar] [CrossRef]
- Lizano, L.E. Examining the impact of job burnout on the health and well-being of human service workers: A systematic review and synthesis. Hum. Serv. Organ. Manag. Lea. Gov. 2015, 39, 167–181. [Google Scholar] [CrossRef]
- Barck-Holst, P.; Nilsonne, S.; Kerstedt, T.; Hellgren, C. Coping with stressful situations in social work before and after reduced working hours, a mixed-methods study. Eur. J. Soc. Work. 2021, 24, 94–108. [Google Scholar] [CrossRef]
- Khodadadizadeh, A. Occupational burnout assessment among nurses working in iranian hospital of ali-ebn abitaleb, rafsanjan-iran. J. Occup. Health Epidemiol. 2012, 1, 103–110. [Google Scholar]
- Garcia, E.; Kundu, I.; Kelly, M.; Soles, R.; Mulder, L.; Talmon, G.A. The american society for clinical pathology’s job satisfaction, well-being, and burnout survey of pathologists. Am. J. Clin. Pathol. 2020, 153, 435–448. [Google Scholar] [CrossRef]
- Rudman, A.; Gustavsson, J.P. Early-career burnout among new graduate nurses: A prospective observational study of intra-individual change trajectories. Int. J. Nurs. Stud. 2011, 48, 292–306. [Google Scholar] [CrossRef]
- Song, Y.-J.; Lee, Y.-S. Work hours, work schedules, and subjective well-being in korea. Int. Soc. 2021, 36, 25–48. [Google Scholar] [CrossRef]
- Van der Doef, M.; Maes, S. The job demand-control (-support) model and psychological well-being: A review of 20 years of empirical research. Work Stress 1999, 13, 87–114. [Google Scholar] [CrossRef]
- Karhula, K.; Woehrmann, A.M.; Brauner, C.; Harma, M.; Kivimaki, M.; Michel, A.; Oksanen, T. Working time dimensions and well-being: A cross-national study of finnish and german health care employees. Chronoblol. Int. 2020, 37, 1312–1324. [Google Scholar] [CrossRef]
- Zhujun, L. The effect of occupational burnout and sleep quality on subjective well-being of medical personnel. Chin. Health Serv. Manag. 2018, 35, 866–869. [Google Scholar]
- Kim, S.R.; Park, O.L.; Kim, H.Y.; Kim, J.Y. Factors influencing well-being in clinical nurses: A path analysis using a multi-mediation model. J. Clin. Nurs. 2019, 28, 4549–4559. [Google Scholar] [CrossRef]
- Maslach, C.; Schaufeli, W.B.; Leiter, M.P. Job burnout. Annu. Rev. Psychol. 2001, 52, 397–422. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E.; De Boer, E.; Schaufeli, W.B. Job demands and job resources as predictors of absence duration and frequency. J. Vocat. Behav. 2003, 2, 341–356. [Google Scholar] [CrossRef]
- Demerouti, E.; Bakker, A.B.; Nachreiner, F.; Schaufeli, W.B. The job demands-resources model of burnout. J. Appl. Psychol. 2001, 86, 499–512. [Google Scholar] [CrossRef]
- Kim, S.; Wang, J. The role of job demands–resources (jdr) between service workers’ emotional labor and burnout: New directions for labor policy at local government. Int. J. Environ. Res. Public Health 2018, 15, 2894. [Google Scholar] [CrossRef]
- Duan, J.; Jiao, F.; Zhang, Q.; Lin, Z. Predicting urban medical services demand in china: An improved grey markov chain model by taylor approximation. Int. J. Environ. Res. Public Health 2017, 14, 883. [Google Scholar] [CrossRef] [PubMed]
- National Bureau of Health Statistics. China Health and Family Planning Statistical Yearbook 2019. Available online: http://www.stats.gov.cn/tjsj/ndsj/ (accessed on 15 April 2021).
- Rabbani, F.; Hashmani, F.N.; Mukhi, A.; Gul, X.; Pradhan, N.; Hatcher, P.; Farag, M.; Abbas, F. Hospital management training for the eastern mediterranean region: Time for a change? J. Health Org. Manag. 2015, 29, 965–972. [Google Scholar] [CrossRef] [PubMed]
- Hong, B.; Zhang, D.H.; Zuo, T.M.; Xue, D.B.; Zhou, J. Survey and analysis of the current state of residency training in medical-school-affiliated hospitals in china. BMC Med. Educ. 2014, 14, 111–120. [Google Scholar]
- Zhou, H.; Han, X.; Zhang, J.; Jing, S.; Hu, L.; Hu, G.; Wu, S.; Zhao, P.; Jiang, F.; Liu, Y. Job satisfaction and associated factors among medical staff in tertiary public hospitals: Results from a national cross-sectional survey in china. Int. J. Environ. Res. Public Health 2018, 15, 1528. [Google Scholar] [CrossRef] [PubMed]
- Li, Y. Subjective well-being of medical personnel of third class a hospitals in hebei province. Chin. J. Clin. Psychol. 2012, 20, 407–410. (In Chinese) [Google Scholar]
- Yuan, Y.; Chen, Y.; Han, H.H.; Wang, Q.Q.; Wu, J.F.; Lu, Y.; Luo, W.P.; Xu, H.F.; Tang, H.Y. Anxiety and depression of medical workers and their relationship with work intensity. Chin. J. Health Psycholo. 2019, 27, 1059–1063. (In Chinese) [Google Scholar]
- Ahola, K.; Gould, R.; Virtanen, M.; Honkonen, T.; Aromaa, A.; Lönnqvist, J. Occupational burnout as a predictor of disability pension: A population-based cohort study. Occup. Environ. Medic. 2009, 5, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Fazio, A.F. A concurrent validational study of the nchs general well-being schedule. Vital Health Stat. 1977, 73, 1–53. [Google Scholar]
- Jianhua, D. Overview of subjective well-being. Adv. Psycholo. Sci. 1996, 1, 46–51. (In Chinese) [Google Scholar]
- Zito, M.; Colombo, L.; Borgogni, L.; Callea, A.; Cortese, C.G. The nature of job crafting: Positive and negative relations with job satisfaction and work-family conflict. Int. J. Environ. Res. Public Health 2019, 16, 1176. [Google Scholar] [CrossRef]
- Chen, Y.C.; Guo, Y.; Chin, W.S.; Cheng, N.Y.; Shiao, S.C. Patient–nurse ratio is related to nurses’ intention to leave their job through mediating factors of burnout and job dissatisfaction. Int. J. Environ. Res. Public Health 2019, 16, 4801. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zhou, S.; Kwan, M.-P.; Chen, F.; Lin, R. Impacts of individual daily greenspace exposure on health based on individual activity space and structural equation modeling. Int. J. Environ. Res. Public Health 2018, 15, 2323. [Google Scholar] [CrossRef]
- Aldrees, T.M.; Aleissa, S.; Zamakhshary, M.; Badri, M.; Sadat-Ali, M. Physician well-being: Prevalence of burnout and associated risk factors in a tertiary hospital, riyadh, saudi arabia. Ann. Saudi. Med. 2013, 33, 451–456. [Google Scholar] [CrossRef]
- Sabbah, I.; Sabbah, H.; Sabbah, S.; Akoum, H.; Droubi, N. Burnout among lebanese nurses: Psychometric properties of the maslach burnout inventory-human services survey (mbi-hss). Health 2012, 4, 644–652. [Google Scholar] [CrossRef]
- Wang, Z.; Xie, Z.; Dai, J.; Zhang, L.; Huang, Y.; Chen, B. Physician burnout and its associated factors: A cross-sectional study in shanghai. J. Occup. Health 2005, 56, 73–83. [Google Scholar] [CrossRef]
- Zhou, T. Analysis of occupational burnout of young medical personnel in beijing and its influencing factors. Prac. Prevent. Medic. 2020, 27, 1118–1121. [Google Scholar]
- Zarei, E.; Ahmadi, F.; Sial, M.S.; Hwang, J.; Thu, P.A.; Usman, S.M. Prevalence of burnout among primary health care staff and its predictors: A study in iran. Int. J. Environ. Res. Public. Health 2019, 16, 2249. [Google Scholar] [CrossRef]
- Wood, W.; Rhodes, N.; Whelan, M. Sex-differences in positive well-being-a consideration of emotional style and marital-status. Psychol. Bull. 1989, 106, 249–264. [Google Scholar] [CrossRef]
- Xing, Z.J.; Huang, L.Q. The relationship between age and subjective well-being: Evidence from five capital cities in mainland china. Soc. Ind. Res. 2014, 117, 743–756. (In Chinese) [Google Scholar] [CrossRef]
- Costa, P.T.; Mccrae, R.R.; Zonderman, A.B. Environmental and dispositional influences on wellbeing: Longitudinal follow up of an american national sample. British journal of psychology. Brit. J. Psychol. 1987, 78 Pt 3, 299–306. [Google Scholar] [CrossRef]
- Louis, V.V.; Zhao, S. Effects of family structure, family ses, and adulthood experiences on life satisfaction. J. Fam. Issues 2002, 23, 986–1005. [Google Scholar] [CrossRef]
- Dolan, P.; Peasgood, T.; White, M. Do we really know what makes us happy? A review of the economic literature on the factors associated with subjective well-being-sciencedirect. J. Econ. Psychol. 2008, 29, 94–122. [Google Scholar] [CrossRef]
- Lorber, M.; Treven, S.; Mumel, D. Well-being and satisfaction of nurses in slovenian hospitals: A cross-sectional study. Slov. J. Public Health 2020, 59, 180–188. [Google Scholar] [CrossRef]
- Diener, E.; Suh, E.M.; Lucas, R.E.; Smith, H.L. Subjective well-being: Three decades of progress. Psychol. Bull. 1999, 125, 276–302. [Google Scholar] [CrossRef]
- De Moortel, D.; Thévenon, O.; De Witte, H.; Vanroelen, C. Working hours mismatch, macroeconomic changes, and mental well-being in europe. J. Health Soc. Behav. 2017, 58, 217–231. [Google Scholar] [CrossRef]
- Beckers, D.G.J.; Dimitri, V.D.L.; Smulders, P.G.W.; Kompier, M.A.J.; Taris, T.W.; Geurts, S.A.E. Voluntary or involuntary? Control over overtime and rewards for overtime in relation to fatigue and work satisfaction. Work Stress 2008, 22, 33–50. [Google Scholar] [CrossRef]
- Craig, L.; Brown, J.E. Weekend work and leisure time with family and friends: Who misses out? J. Mar. Fam. 2014, 76, 710–727. [Google Scholar] [CrossRef]
- Lizano, E.L.; Hsiao, H.-Y.; Mor Barak, M.E.; Casper, L.M. Support in the workplace: Buffering the deleterious effects of work–family conflict on child welfare workers’ well-being and job burnout. J. Soc. Serv. Res. 2014, 40, 178–188. [Google Scholar] [CrossRef]
- Song, X.; Xiang, M.; Liu, Y.; Yu, C. Relationship between job satisfaction and burnout based on a structural equation model. J. Occup. Environ. Med. 2020, 62, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.D.; Boone, S.; Tan, L.; Dyrbye, L.N.; Sotile, W.; Satele, D.; West, C.P.; Sloan, J.; Oreskovich, M.R. Burnout and satisfaction with work-life balance among us physicians relative to the general us population. Arch. Intern. Med. 2012, 172, 1377–1385. [Google Scholar] [CrossRef] [PubMed]
| Level | M ± SD | Low | Moderate | High |
|---|---|---|---|---|
| EE (9 items, 0–54) | 17.31 ± 11.58 | 233 (53.8) | 109 (25.2) | 91 (21.0) |
| DP (5 items, 0–30) | 5.94 ± 5.71 | 269 (62.1) | 99 (22.9) | 65 (15.0) |
| PA (8 items, 0–48) | 20.71 ± 10.19 | 121 (27.9) | 116 (26.8) | 196 (45.3) |
| Variables | Total | Job Burnout | SWB | ||
|---|---|---|---|---|---|
| ± s | t/F-Value | ± s | t/F-Value | ||
| Sex | 0.539 | 0.157 | |||
| Male | 158 (36.5) | 54.55 ± 16.03 | 42.68 ± 14.83 | ||
| Female | 275 (63.5) | 53.63 ± 17.72 | 42.47 ± 13.05 | ||
| Age (year) | 0.840 | 1.403 | |||
| ≤30 | 123 (28.4) | 54.67 ± 19.35 | 42.12 ± 13.94 | ||
| 31–40 | 176 (40.7) | 54.49 ± 16.01 | 41.9 ± 12.88 | ||
| 41–50 | 84 (19.4) | 53.94 ± 16.59 | 42.31 ± 13.1 | ||
| ≥51 | 50 (11.6) | 50.42 ± 15.88 | 46.26 ± 16.58 | ||
| Marital status | −0.124 | −1.230 | |||
| Married | 344 (79.5) | 53.76 ± 17.95 | 41.00 ± 15.50 | ||
| Not married | 89 (20.6) | 54.02 ± 16.1 | 43.00 ± 13.20 | ||
| Education | −3.209 ** | 2.222 * | |||
| Junior college and below | 62 (14.3) | 47.58 ± 18.15 | 46.11 ± 15.88 | ||
| Bachelor’s degree and above | 371 (85.7) | 55.03 ± 16.72 | 41.95 ± 13.24 | ||
| Hospital category | −0.009 | 0.546 | |||
| Specialized | 56 (12.9) | 53.95 ± 15.01 | 43.48 ± 11.41 | ||
| General | 377 (87.1) | 53.97 ± 17.42 | 42.41 ± 14.03 | ||
| Average daily working hours (h) | −4.240 *** | 5.155 *** | |||
| ≤8 | 103 (23.8) | 47.85 ± 19.44 | 49.09 ± 15.39 | ||
| >8 | 330 (76.2) | 55.88 ± 15.87 | 40.51 ± 12.48 | ||
| Continuous working hours (h) | 65.07 *** | 96.58 *** | |||
| ≤8 | 50 (11.6) | 39.74 ± 18.50 | 60.98 ± 12.71 | ||
| 9–16 | 302 (69.7) | 52.28 ± 14.35 | 42.19 ± 10.90 | ||
| >16 | 81 (18.7) | 69.04 ± 15.15 | 32.52 ± 12.45 | ||
| Overtime on weekends (d) | 30.91 *** | 49.86 *** | |||
| 0 | 81 (18.7) | 42.52 ± 16.58 | 55.49 ± 1375 | ||
| ≤1 | 275 (63.5) | 54.11 ± 15.22 | 41.30 ± 10.91 | ||
| >1 | 71 (16.4) | 64.18 ± 14.95 | 34.15 ± 13.06 | ||
| 2 | 6 (1.4) | 81.17 ± 23.96 | 24.33 ± 10.38 | ||
| Variable | R | P value | |
|---|---|---|---|
| Working hours | Average daily working hours | −0.267 | <0.001 |
| Continuous working hours | −0.536 | <0.001 | |
| Overtime on weekends | −0.493 | <0.001 | |
| Job burnout | Emotional exhaustion | −0.556 | <0.001 |
| Depersonalization | −0.372 | <0.001 | |
| Reduced personal achievement | −0.128 | <0.001 | |
| Index | Suggested Values | Initial (M1) | Final (M2) | ||
|---|---|---|---|---|---|
| Measured Value | Evaluate | Measured Value | Evaluate | ||
| χ2/df | <3.00 | 8.537 | Poor | 2.521 | Good |
| GFI | >0.90 | 0.928 | Good | 0.981 | Good |
| RMR | <0.05 | 0.072 | Poor | 0.035 | Good |
| RMSEA | <0.08 | 0.132 | Poor | 0.059 | Good |
| AGFI | >0.90 | 0.855 | Poor | 0.955 | Good |
| NFI | >0.90 | 0.888 | Poor | 0.972 | Good |
| TLI | >0.90 | 0.849 | Poor | 0.969 | Good |
| CFI | >0.90 | 0.899 | Poor | 0.983 | Good |
| Item | Path | 95% CI Value | Effect Size | Relative Effect Value | |
|---|---|---|---|---|---|
| Lower Limit | Upper Limit | ||||
| Direct effect | Working hours → SWB | −0.039 | −0.027 | −0.033 | 4.5% |
| Mesomeric effect | Working hours → Job burnout → SWB | −0.746 | −0.614 | −0.695 | 95.5% |
| Total effect | −0.779 | −0.644 | −0.728 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jia, Z.; Wen, X.; Lin, X.; Lin, Y.; Li, X.; Li, G.; Yuan, Z. Working Hours, Job Burnout, and Subjective Well-Being of Hospital Administrators: An Empirical Study Based on China’s Tertiary Public Hospitals. Int. J. Environ. Res. Public Health 2021, 18, 4539. https://doi.org/10.3390/ijerph18094539
Jia Z, Wen X, Lin X, Lin Y, Li X, Li G, Yuan Z. Working Hours, Job Burnout, and Subjective Well-Being of Hospital Administrators: An Empirical Study Based on China’s Tertiary Public Hospitals. International Journal of Environmental Research and Public Health. 2021; 18(9):4539. https://doi.org/10.3390/ijerph18094539
Chicago/Turabian StyleJia, Zhihui, Xiaotong Wen, Xiaohui Lin, Yixiang Lin, Xuyang Li, Guoqing Li, and Zhaokang Yuan. 2021. "Working Hours, Job Burnout, and Subjective Well-Being of Hospital Administrators: An Empirical Study Based on China’s Tertiary Public Hospitals" International Journal of Environmental Research and Public Health 18, no. 9: 4539. https://doi.org/10.3390/ijerph18094539
APA StyleJia, Z., Wen, X., Lin, X., Lin, Y., Li, X., Li, G., & Yuan, Z. (2021). Working Hours, Job Burnout, and Subjective Well-Being of Hospital Administrators: An Empirical Study Based on China’s Tertiary Public Hospitals. International Journal of Environmental Research and Public Health, 18(9), 4539. https://doi.org/10.3390/ijerph18094539





