Review of Current Healthcare Waste Management Methods and Their Effect on Global Health
Abstract
1. Introduction
2. Methodology
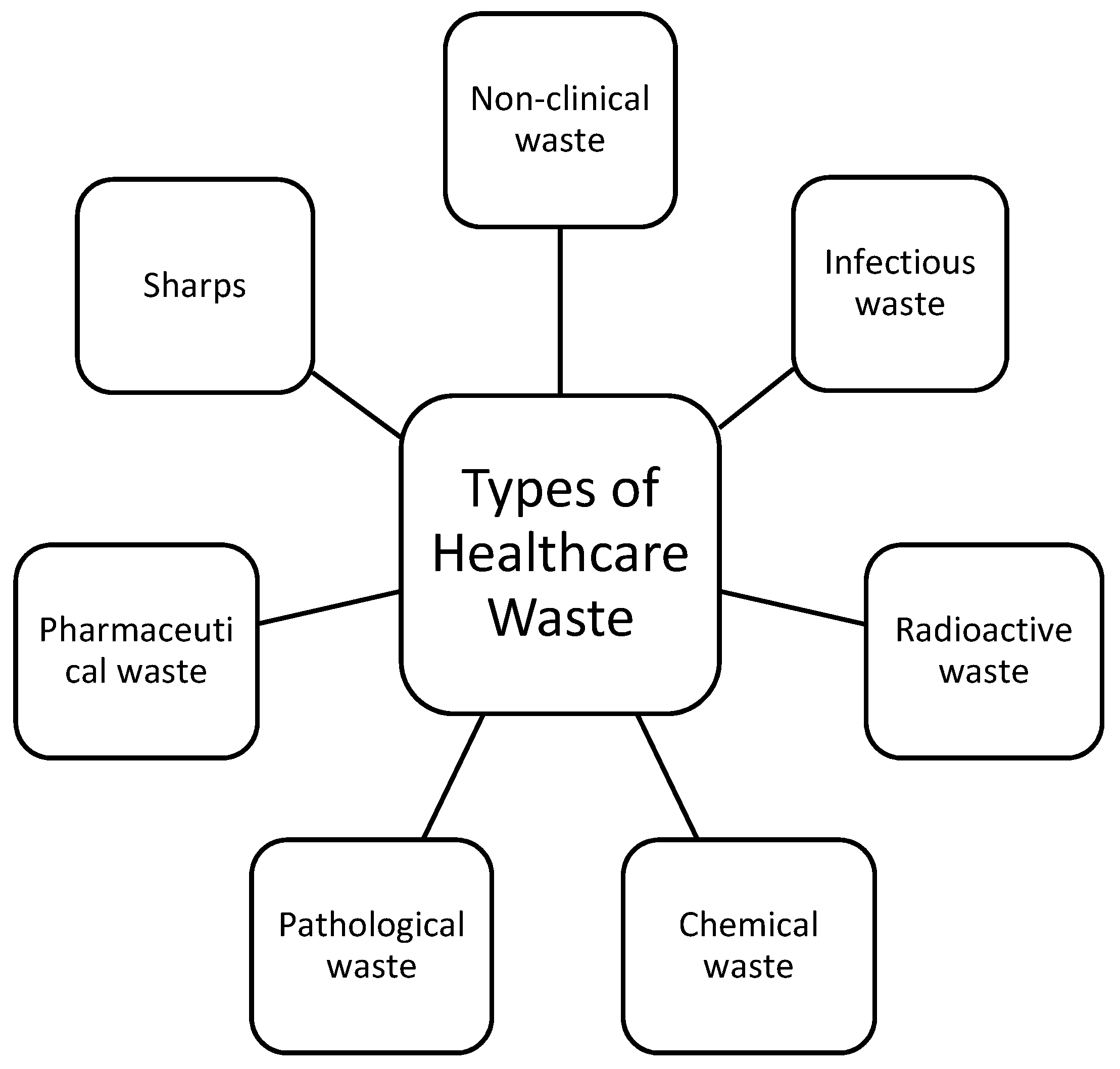
3. Sources of HCW
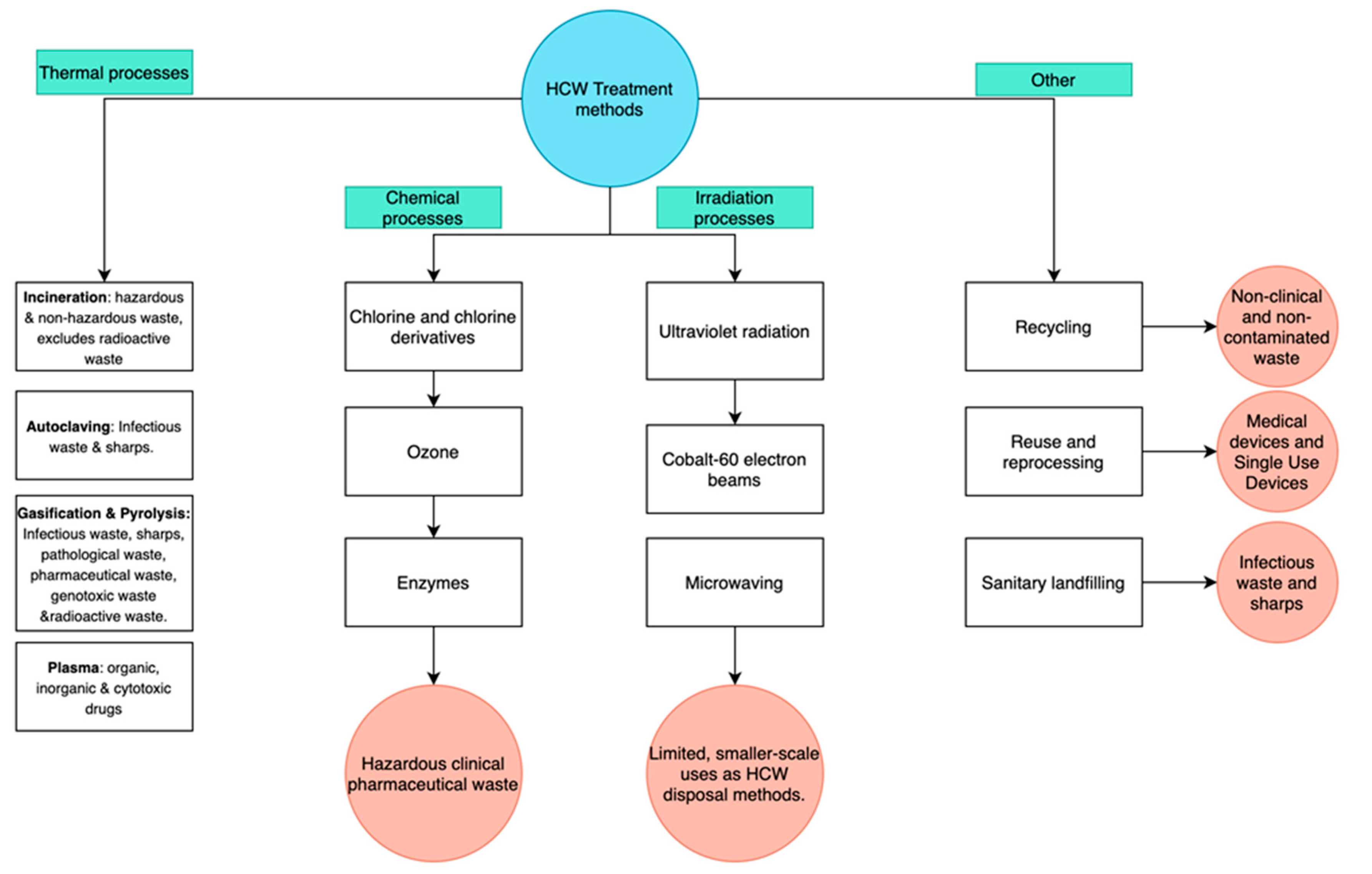
4. Currently Utilised Methods of HCW Treatment and Disposal
4.1. Thermal Processes
4.1.1. Incineration
4.1.2. Autoclaving
4.1.3. Steam Augur
4.1.4. Gasification and Pyrolysis
4.1.5. Plasma
4.2. Chemical Processes
4.3. Irradiation Processes
4.3.1. Ultraviolet
4.3.2. Cobalt-60 Electron Beams
4.3.3. Microwaving
4.4. Other Methods of HCW Treatment and Disposal
4.4.1. Recycling
4.4.2. Reuse and Reprocessing
4.4.3. Sanitary Landfilling
5. Global Health Consequences of Proper and Improper HCW Disposal
Developing and Under-Developed Countries
6. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yeoh, E.; Othman, K.; Ahmad, H. Understanding medical tourists: Word-of-mouth and viral marketing as potent marketing tools. Tour. Manag. 2013, 34, 196–201. [Google Scholar] [CrossRef]
- Global Spending on Health: A World in Transition-WHO. Available online: https://www.who.int/health_financing/documents/health-expenditure-report-2019.pdf?ua=1 (accessed on 10 July 2020).
- Wilson, D.C.; Rodic, L.; Modak, P.; Soos, R.; Carpintero, A.; Velis, K.; Simonett, O. Global Waste Management Outlook. UNEP United Nations Environment Programme. Available online: https://www.unenvironment.org/resources/report/global-waste-management-outlook (accessed on 10 July 2020).
- McPhail, S.M. Multimorbidity in chronic disease: Impact on health care resources and costs. Risk Manag. Healthc. Policy 2016, 9, 143–156. [Google Scholar] [CrossRef] [PubMed]
- Rapoport, J.; Jacobs, P.; Bell, N.R.; Klarenbach, S. Refining the measurement of the economic burden of chronic diseases in Canada. Chronic. Dis. Can. 2004, 20, 1–643. [Google Scholar]
- Raghupathi, W.; Raghupathi, V. An empirical study of chronic diseases in the United states: A visual analytics approach. Int. J. Environ. Res. Public Health 2018, 15, 431. [Google Scholar] [CrossRef]
- Edmunds, K.L.; Elrahman, S.A.; Bell, D.J.; Brainard, J.; Dervisevic, S.; Fedha, T.P.; Few, R.; Howard, G.; Lake, I.; Maes, P.; et al. Recommendations for dealing with waste contaminated with Ebola virus: A Hazard Analysis of Critical Control Points approach. Bull. World Health Organ. 2016, 94, 424–432. [Google Scholar] [CrossRef]
- Peng, J.; Wu, X.; Wang, R.; Li, C.; Zhang, Q.; Wei, D. Medical waste management practice during the 2019-2020 novel coronavirus pandemic: Experience in a general hospital. Am. J. Infect. Control 2020, 48, 918–921. [Google Scholar] [CrossRef]
- Lafferty, K.D.; Mordecai, E.A. The rise and fall of infectious disease in a warmer world. F1000Research 2016, 5. [Google Scholar] [CrossRef]
- Zaman, A. A comprehensive study of the environmental and economic benefits of resource recovery from global waste management systems. J. Clean. Prod. 2016, 124, 41–50. [Google Scholar] [CrossRef]
- Voudrias, E.A. Healthcare waste management from the point of view of circular economy. Waste Manag. 2018, 75, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Vlachokostas, C.; Michailidou, A.V.; Achillas, C. Multi-Criteria Decision Analysis towards promoting Waste-to-Energy Management Strategies: A critical review. Renew. Sustain. Energy Rev. 2020, 138, 110563. [Google Scholar] [CrossRef]
- Management of Solid Health-Care Waste at Primary Healthcare Centres: A Decision Making Guide, 1st ed.; World Health Organisation: Geneva, Switzerland, 2005; ISBN 9241592745.
- Healthcare Waste-WHO. Available online: https://www.who.int/news-room/fact-sheets/detail/health-care-waste (accessed on 11 August 2020).
- Reducing Waste in Irish Healthcare Facilities- Environmental Protection Agency. Available online: https://www.epa.ie/pubs/reports/green%20business/Reducing-waste-in-Irish-Healthcare-Facilities-waste-guidance-booklet-reduced-size.pdf (accessed on 14 January 2021).
- Windfeld, E.S.; Brooks, M.S. Medical waste management—A review. J. Envrion. Manag. 2015, 163, 98–108. [Google Scholar] [CrossRef]
- Eker, H.H.; Bilgili, M.S. Statistical analysis of waste generation in healthcare services: A case study. Waste Manag. Res. 2011, 29, 791–796. [Google Scholar] [CrossRef]
- Farzadkia, M.; Emamjomeh, M.M.; Golbaz, S.; Sajadi, H.S. An investigation in hospital solid waste management in Iran. Glob. NEST J. 2015, 17, 771–783. [Google Scholar]
- Komilis, D.; Fouki, A.; Papadopoulos, D. Hazardous medical waste generation rates of different categories of health-care facilities. Waste Manag. 2012, 32, 1434–1441. [Google Scholar] [CrossRef]
- Gusca, J.; Kalnins, S.A.; Blumberga, D.; Bozhko, L.; Khabdullina, Z.; Khabdullin, A. Assessment method of healthcare waste generation in Latvia and Kazakhstan. Energy Procedia 2015, 72, 175–179. [Google Scholar] [CrossRef]
- Hossain, S.; Santhanam, A.; Nik Norulaini, N.A.; Mohd Omar, M.K. Clinical solid waste management practices and its impact on human health and environment—A review. Waste Manag. 2011, 31, 754–766. [Google Scholar] [CrossRef] [PubMed]
- Pruss, A.; Giroult, E.; Rushbrook, P. Safe Management of Wastes from Health-Care Activities; World Health Organization: Geneva, Switzerland, 1999. [Google Scholar]
- Diaz, L.F.; Eggerth, L.L.; Enkhtsetseg, S. Anejo de Residuos de Establecimientos de Salud en Guayaquil, Ecuador; Pan American Health Organization: Quito, Equador, 2001. [Google Scholar]
- Johnson, M.K.; Gonzalez, L.M.; Duenas, L.; Gamero, M.; Relyea, G.; Luque, E.L.; Caniza, A.M. Improving waste segregation while reducing costs in a tertiary-care hospital in a lower-middle income country in Central America. Waste Manag. Res. 2013, 31, 733–738. [Google Scholar] [CrossRef]
- Rabeie, O.L.; Miranzadeh, M.B.; Fallah, S.H.; Dehqan, S.; Moulana, Z.; Amouei, A.; Mohammadi, A.A.; Asgharnia, H.A.; Babaei, M. Determination of Hospital Waste Composition and Management in Amol City, Iran. Health Scope 2012, 1, 127–131. [Google Scholar] [CrossRef]
- Yong, Z.; Gang, X.; Guanxing, W.; Tao, Z.; Dawei, J. Medical waste management in China: A case study of Nanjing. Waste Manag. 2009, 29, 1376–1382. [Google Scholar] [CrossRef]
- Ananth, A.P.; Prashanthini, V.; Visvanathan, C. Healthcare waste management in Asia. Waste Manag. 2010, 30, 154–161. [Google Scholar] [CrossRef]
- Mohee, R. Medical wastes characterization in healthcare institutions of Mauritius. Waste Manag. 2005, 25, 575–581. [Google Scholar] [CrossRef]
- Jang, Y.C.; Lee, C.; Yoon, O.S.; Kim, H. Medical waste management in Korea. J. Envrion. Manag. 2006, 80, 107–115. [Google Scholar] [CrossRef]
- Phengxay, S.; Okumura, J.; Miyoshi, M.; Sakisaka, K.; Kuroiwa, C. Health-care waste management in Lao PDR: A case study. Waste Manag. Res. 2005, 23, 571–581. [Google Scholar] [CrossRef] [PubMed]
- Eleyan, D.; Al-Khatib Issam, A.; Garfield, J. System dynamics model for hospital waste characterization and generation in developing countries. Waste Manag. Res. 2013, 31, 986–995. [Google Scholar] [CrossRef] [PubMed]
- Suwannee, A. Study on waste from hospital and clinics in Phitsanulok. Online J. Health Allied Sci. 2002, 1, 6–14. [Google Scholar]
- Maamari, O.; Brandam, C.; Lteif, R.; Salameh, D. Health care waste generation rates and patterns: The case of Lebanon. Waste Mang. 2015, 43, 550–554. [Google Scholar] [CrossRef]
- Bendjoudi, Z.; Taleb, F.; Abdelmalek, F.; Addou, A. Healthcare waste management in Algeria and Mostaganem department. Waste Manag. 2009, 29, 1383–1387. [Google Scholar] [CrossRef]
- Manga, E.V.; Forton, O.T.; Mofor, A.L.; Woodard, R. Health care waste management in Cameroon: A case study from the Southwestern Region. Resour. Conserv. Recycl. 2011, 57, 108–116. [Google Scholar] [CrossRef]
- Abd El-Salam, M.M. Hospital waste management in El-Beheira Governorate, Egypt. J. Envrion. Manag. 2010, 91, 618–629. [Google Scholar] [CrossRef] [PubMed]
- Tesfahun, E.; Kumie, A.; Beyene, A. Developing models for the prediction of hospital healthcare waste generation rate. Waste Manag. Res. 2015, 34, 219–220. [Google Scholar] [CrossRef]
- Mbarki, A.; Kabbachi, B.; Ezaidi, A.; Benssaou, M. Medical waste management: A case study of the souss-massa-draa region, morocco. J. Environ. Prot. 2013, 4, 914–919. [Google Scholar] [CrossRef]
- Suhair, A.; Gayoum, S. Management of hospital solid waste in Khartoum State. Environ. Monit. Assess. 2013, 185, 8567–8582. [Google Scholar]
- Minoglou, M.; Gerassimidou, S.; Komilis, D. Healthcare Waste Generation Worldwide and Its Dependence on Socio-Economic and Environmental Factors. Sustainability 2017, 9, 220. [Google Scholar] [CrossRef]
- Khobragade, D. Health Care Waste: Avoiding Hazards to Living and Non-Living Environment by Efficient Management. Fortune J. Health Sci. 2019, 2, 14–29. [Google Scholar] [CrossRef]
- Sharma, R.; Sharma, M.; Sharma, R.; Sharma, V. The impact of incinerators on human health and environment. Rev. Envrion. Health 2013, 28, 67–72. [Google Scholar] [CrossRef]
- Darbre, P. Overview of air pollution and endocrine disorders. Int. J. Gen. Med. 2018, 11, 191–207. [Google Scholar] [CrossRef]
- Thakur, V.; Ramesh, A. Healthcare waste management research: A structured analysis and review (2005–2014). Waste Manag. Res. 2015, 33, 855–870. [Google Scholar] [CrossRef]
- Alvim-Ferraz, M.C.M.; Afonso, S.A.V. Incineration of healthcare wastes: Management of atmospheric emissions through waste segregation. Waste Manag. 2005, 25, 638–648. [Google Scholar] [CrossRef]
- EC. Directive 2000/76/EC of the European Parliament and of the Council of December 4th 2000 on the Incineration of Waste. Off. J. Eur. Communities 2000, 43, 91–111. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/HTML/?uri=CELEX:32000L0076&from=EN (accessed on 17 December 2020).
- James, R. Incineration: Why this may be the most environmentally sound method of renal healthcare waste disposal. J. Ren. Care 2010, 36, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Tudor, T.L.; Noonan, C.L.; Jenkin, L.E.T. Healthcare waste management: A case study from the National Health Service in Cornwall, United Kingdom. Waste Manag. 2005, 25, 606–615. [Google Scholar] [CrossRef]
- Bashaar, M.; Thawani, V.; Hassali, M.A.; Saleem, F. Disposal practices of unused and expired pharmaceuticals among general public in Kabul. BMC Public Health 2017, 17, 45. [Google Scholar]
- Azmal, M.; Kalhor, R.; Dehcheshmeh, N.F.; Goharinezhad, S.; Heidari, Z.; Farzianpour, F. Going toward Green Hospital by Sustainable Healthcare Waste Management: Segregation, Treatment and Safe Disposal. Health 2014, 6, 2632–2640. [Google Scholar] [CrossRef]
- Hossain, M.; Balakrishnan, V.; Rahman, N.N.N.A.; Sarker, M.; Islam, Z.; Kadir, M.O.A. Treatment of clinical solid waste using a steam autoclave as a possible alternative technology to incineration. Int. J. Environ. Res. Public Health 2012, 9, 855–867. [Google Scholar] [CrossRef]
- Padmanabhan, K.; Barik, D. Health hazards of medical waste and its disposal. Energy Toxic Org. Waste Heat Power Gener. 2019, 99–118. [Google Scholar] [CrossRef]
- Lee, B.K.; Ellenbecker, M.J.; Moure-Eraso, R. Alternatives for treatment and disposal cost reduction of regulated medical waste. Waste Manag. 2004, 24, 143–151. [Google Scholar] [CrossRef]
- Hagen, D.L.; Al-Humaidi, F.; Blake, M. Infectious waste surveys in a Saudi Arabian hospital: An important quality improvement tool. Am. J. Infect. Control 2001, 29, 198–202. [Google Scholar] [CrossRef]
- Marincovic, N.; Vitale, K.; Holcer, N.; Dzakula, A.; Pavic, T. Management of Hazardous medical waste in Croatia. Waste Manag. 2008, 28, 1049–1056. [Google Scholar] [CrossRef]
- Chauhan, A.; Singh, A. Healthcare waste management: A state-of-the-art literature review. Int. J. Environ. Waste Manag. 2016, 18, 120–144. [Google Scholar] [CrossRef]
- Tudor, T.L.; Townend, W.K.; Cheeseman, C.R.; Edgar, J.E. An overview of arisings and large-scale treatment technologies for healthcare waste in the United Kingdom. Waste Manag. Res. 2009, 27, 374–383. [Google Scholar] [CrossRef]
- Zimmermann, K. Microwave as an emerging technology for the treatment of biohazardous waste: A mini-review. Waste Manag. Res. 2017, 35, 471–479. [Google Scholar] [CrossRef]
- Oliveira, E.A.; Nogueira, N.G.P.; Innocentini, M.D.M.; Pisani, R. Microwave inactivation of Bacillus atrophaeus spores in healthcare waste. Waste Manag. 2010, 30, 2327–2335. [Google Scholar] [CrossRef]
- Environment and Sustainability: Health Technical Memorandum 07-01: Safe Management of Healthcare Waste, Department of Health. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/167976/HTM_07-01_Final.pdf (accessed on 7 October 2020).
- Estates Returns Information Collection (ERIC) 2018/19: Data Quality Report 2019, Department of Health. Available online: http://hefs.hscic.gov.uk/ERIC.asp (accessed on 7 October 2020).
- Ferraz, M.C.M.A.; Cardoso, J.I.B.; Pontes, S.L.R. Concentration of Atmospheric Pollutants in the Gaseous Emissions of Medical Waste Incinerators. J. Air Waste Manag. Assoc. 2000, 50, 131–136. [Google Scholar] [CrossRef]
- Hoyos, A.; Cobo, M.; Aristizábal, B.; Córdoba, F.; Montes de Correa, C. Total suspended particulate (TSP), polychlorinated dibenzodioxin (PCDD) and polychlorinated dibenzofuran (PCDF) emissions from medical waste incinerators in Antioquia, Colombia. Chemosphere 2008, 73, S137–S142. [Google Scholar] [CrossRef]
- Njagi, N.A.; Oloo, M.A.; Kithinji, J.; Kithinji, M.J. Health-Care Waste Incineration and Related Dangers to Public Health: Case Study of the Two Teaching and Referral Hospitals in Kenya. J. Community Health 2012, 37, 1168–1171. [Google Scholar] [CrossRef] [PubMed]
- Njoroge, S.M.; Koskei, P.; Chepngeno, E.; Lutukai, L.; Okwiri, R.; Maluki, A. Effectiveness of incinerators in the management of medical wastes in hospitals within Eldoret municipality. East Afr. J. Public Health 2011, 8, 196–198. [Google Scholar]
- Salkin, I.F. Conventional and alternative technologies for the treatment of infectious waste. J. Mater. Cycles Waste Manag. 2003, 5, 9–12. [Google Scholar] [CrossRef]
- Al-Khatib, I.A.; Sato, C. Solid health care waste management status at health care centers in the West Bank–Palestinian Territory. Waste Manag. 2009, 29, 2398–2403. [Google Scholar] [CrossRef]
- Sartaj, M.; Arabgol, R. Assessment of healthcare waste management practices and associated problems in Isfahan Province (Iran). J. Mater Cycles Waste Manag. 2015, 17, 99–106. [Google Scholar] [CrossRef]
- Ghasemi, M.K.; Yusuff, R.M. Advantages and disadvantages of healthcare waste treatment and disposal alternatives: Malaysian scenario. Pol. J. Environ. Stud. 2016, 25, 17–25. [Google Scholar] [CrossRef]
- Klinghoffer, N.B.; Castaldi, M.J. Gasification and Pyrolysis of Municipal Solid Waste (MSW), 1st ed.; Woodhead Publishing Series in Energy, Waste to Energy Conversion Technology; Woodhead Publishing: Boston, MA, USA, 2013; pp. 146–176. ISBN 9780857090119. [Google Scholar]
- Christenson, T. Solid Waste Technology and Management, 1st ed.; Wiley-Blackwell: London, UK, 2010; ISBN 9780470666883. [Google Scholar]
- Messerle, V.E.; Mosse, A.L.; Ustimenko, A.B. Processing of biomedical waste in plasma gasifier. Waste Manag. 2018, 79, 791–799. [Google Scholar] [CrossRef]
- Cai, X.; Du, C. Thermal Plasma Treatment of Medical Waste. Plasma Chem. Plasma Process 2020. [Google Scholar] [CrossRef]
- Diaz, L.F.; Savage, G.M.; Eggerth, L.L. Alternatives for the treatment and disposal of healthcare wastes in developing countries. Waste Manag. 2005, 25, 626–637. [Google Scholar] [CrossRef]
- Tsukamoto, A.; Ishiwata, S.; Kajimoto, A.; Murata, R.; Kitano, R.; Inoue, T.; Kotake, T. Application of ozone gas for decontamination of nucleoside anticancer drugs. J. Pharm. Health Care Sci. 2016, 2. [Google Scholar] [CrossRef] [PubMed]
- Coronel, B.; Duroselle, P.; Behr, H.; Moskovtchenko, J.-F.; Freney, J. In situ decontamination of medical wastes using oxidative agents: A 16-month study in a polyvalent intensive care unit. J. Hosp. Infect. 2002, 50, 207–212. [Google Scholar] [CrossRef]
- Grellier, J.; Rushton, L.; Briggs, D.J.; Nieuwenhuijsen, M.J. Assess ing the human health impacts of exposure to disinfection by-products — A critical review of concepts and methods. Environ. Int. 2015, 78, 61–81. [Google Scholar] [CrossRef] [PubMed]
- LaKind, J.S.; Richardson, S.D.; Blount, B.C. The Good, the Bad, and the Volatile: Can We Have Both Healthy Pools and Healthy People? Environ. Sci. Technol. 2010, 44, 3205–3210. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Shen, J.; Ye, D.; Yan, X.; Zhang, Y.; Yang, W.; Li, X.; Junqi, W.; Zhang, L.; Pan, L. Disinfection technology of hospital wastes and wastewater: Suggestions for disinfection strategy during coronavirus Disease 2019 (COVID-19) pandemic in China. Environ. Pollut. 2020, 262. [Google Scholar] [CrossRef]
- Ravanat, J.-L.; Douki, T.; Cadet, J. Direct and indirect effects of UV radiation on DNA and its components. J. Photochem. Photobiol. B Biol. 2001, 63, 88–102. [Google Scholar] [CrossRef]
- Rabenau, H.F.; Kampf, G.; Cinatl, J.; Doerr, H.W. Efficacy of various disinfectants against SARS coronavirus. J. Hosp. Infect. 2005, 61, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Kozmenko, V.; Gonzales, R.; Riopelle, J.; Kaye, A.D. Disinfection Agents and Antiseptics, 1st ed.; Springer: New York, NY, USA, 2014; pp. 573–580. ISBN 978-1-4614-8947-4. [Google Scholar]
- Ikome Kuwoh Mochungong, P.; Gulis, G.; Sodemann, M. Clinical waste incinerators in Cameroon–a case study. Int. J. Health Care Qual. Assur. 2012, 25, 6–18. [Google Scholar] [CrossRef]
- DeBo, R.J.; Lees, C.J.; Dugan, G.O.; Caudell, D.L.; Michalson, K.T.; Hanbury, D.B.; Register, T.C. Late Effects of Total-Body Gamma Irradiation on Cardiac Structure and Function in Male Rhesus Macaques. Radiat. Res. 2016, 186, 55–64. [Google Scholar] [CrossRef]
- Edlich, R.F.; Borel, L.; Jensen, G.; Winters, K.L.; Long III, W.B.; Dean Gubler, K.; Buschbacher, R.M.; Becker, D.G.; Chang, D.E.; Korngold, J.; et al. Revolutionary advances in medical waste management the Sanitec system. J. Long Term Eff. Med. Implant. 2006, 16, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Padder, A.H. Healthcare waste management. Int. J. Trend Sci. Res. Dev. 2019, 3, 908–911. [Google Scholar]
- Saving Carbon, Improving Health, NHS. Available online: File:///Users/christinakenny/Downloads/1237308334_qylG_saving_carbon,_improving_health_nhs_carbon_reducti.pdf (accessed on 10 October 2020).
- Hutchins, D.; White, S. Coming around to recycling. BMJ 2009, 338, 746–748. [Google Scholar] [CrossRef]
- Wang, D.; Wu, J. Reprocessing and reuse of single-use medical devices in China: A pilot survey. BMC Public Health 2019, 19, 461. [Google Scholar] [CrossRef]
- Luijt, D. Risk of infection by reprocessed and resterilized virus-contaminated catheters; an in-vitro study. Eur. Heart J. 2001, 22, 378–384. [Google Scholar] [CrossRef]
- Lakhouit, A.; Schirmer, W.N.; Johnson, T.R.; Cabana, H.; Cabral, A.R. Evaluation of the efficiency of an experimental biocover to reduce BTEX emissions from landfill biogas. Chemosphere 2014, 97, 98–101. [Google Scholar] [CrossRef]
- Xu, Y.; Xue, X.; Dong, L.; Nai, C.; Liu, Y.; Huang, Q. Long-term dynamics of leachate production, leakage from hazardous waste landfill sites and the impact on groundwater quality and human health. Waste Manag. 2018, 82, 156–166. [Google Scholar] [CrossRef] [PubMed]
- Nwachukwu, A.N.; Anonye, D. The effect of atmospheric pressure on CH4 and CO2 emission from a closed landfill site in Manchester, UK. Environ. Monit. Assess. 2013, 185, 5729–5735. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Vaccari, M.; Tudor, T. Considerations for choosing appropriate healthcare waste management treatment technologies: A case study from an East Midlands NHS Trust, in England. J. Clean. Prod. 2016, 135, 139–147. [Google Scholar] [CrossRef]
- Nock, W.J.; Walker, M.; Kapoor, R.; Heaven, S. Modeling the water scrubbing process and energy requirements for CO2 capture to upgrade biogas to biomethane. Ind. Eng. Chem. Res. 2014, 53, 12783–12792. [Google Scholar] [CrossRef]
- Evangelisti, S.; Clift, R. Life cycle assessment of energy from waste via anaerobic digestion: A UK case study. Waste Manag. 2014, 34, 226–237. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Liu, H.C.; Li, P.; Xu, X.G. An integrated decision-making approach for assessing healthcare waste treatment technologies from a multiple stakeholder. Waste Manag. 2017, 59, 508–517. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Li, J.; Zhang, Z.; Cao, X.; Zhu, J.; Chen, W. Establishing an interval-valued fuzzy decision-making method for sustainable selection of healthcare waste treatment technologies in the emerging economies. J. Mater. Cycles Waste Manag. 2020, 22, 501–514. [Google Scholar] [CrossRef]
- Liu, H.C.; You, J.X.; Lu, C.; Chen, Y.Z. Evaluating health-care waste treatment technologies using a hybrid multi-criteria decision-making model. Renew. Sustain. Energy Rev. 2015, 41, 932–942. [Google Scholar] [CrossRef]
- Özkan, A. Evaluation of healthcare waste treatment/disposal alternatives by using multi-criteria decision-making techniques. Waste Manag. Res. 2013, 31, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Hariz, H.A.; Dönmez, C.Ç.; Sennaroglu, B. Siting of a central healthcare waste incinerator using GIS-based Multi-Criteria Decision Analysis. J. Clean. Prod. 2017, 166, 1031–1042. [Google Scholar] [CrossRef]
- Liu, H.C.; Wu, J.; Li, P. Assessment of health-care waste disposal methods using a VIKOR-based fuzzy multi-criteria decision making method. Waste Manag. 2013, 33, 2744–2751. [Google Scholar] [CrossRef] [PubMed]
- Dursun, M.; Karsak, E.E.; Karadayi, M.A. Assessment of health-care waste treatment alternatives using fuzzy multi-criteria decision making approaches. Resour. Conserv. Recycl. 2011, 57, 98–107. [Google Scholar] [CrossRef]
- Ciplak, N.; Kaskun, S. Healthcare waste management practice in the west black sea region, Turkey: A comparative analysis with the developed and developing countries. J. Air Waste Manag. Assoc. 2015, 65, 12. [Google Scholar] [CrossRef]
- Eckelman, M.J.; Sherman, J. Environmental Impacts of the U.S. Health Care System and Effects on Public Health. PLoS ONE 2016, 11. [Google Scholar] [CrossRef]
- Landrigan, P.J.; Fuller, R.; Acosta, N.J.R.; Adeyi, O.; Arnold, R.; Basu, N.; Balde, A.; Bertollini, R.; Bose-O’Reilly, S.; Boufford, J.; et al. The Lancet Commission on pollution and health. Lancet 2018, 391, 462–512. [Google Scholar] [CrossRef]
- Rabl, A.; Spadaro, J.V.; Zoughaib, A. Environmental impacts and costs of solid waste: A comparison of landfill and incineration. Waste Manag. Res. 2008, 26, 147–162. [Google Scholar] [CrossRef] [PubMed]
- Vlachokostas, C.; Achillas, C.; Moussiopoulos, Ν.; Kalogeropoulos, K.; Sigalas, G.; Kalognomou, E.A.; Banias, G. Health effects and social costs of particulate and photochemical urban air pollution: A case study for Thessaloniki, Greece. Air Qual. Atmos. Health 2012, 5, 325–334. [Google Scholar] [CrossRef]
- Honest, A.; Manyele, S.; Saria, J.; Mbuna, J. Assessment of air pollutant emissions from healthcare waste incinerators of different design features. Afr. J. Environ. Sci. Technol. 2020, 4, 311–328. [Google Scholar]
- Manisalidis, I.; Stavropoulou, E.; Stavropoulou, A.; Bezirtzoglou, E. Environmental and health impacts of air pollution: A review. Front. Public Health 2020, 8. [Google Scholar] [CrossRef]
- Ahmadalipour, A.; Moradkhani, H.; Kumar, M. Mortality risk from heat stress expected to hit poorest nations the hardest. Clim. Chang. 2019, 152, 569–579. [Google Scholar] [CrossRef]
- Keatinge, W.R.; Donaldson, G.C. The Impact of Global Warming on Health and Mortality. South. Med J. 2004, 97, 1093–1099. [Google Scholar] [CrossRef]
- Williams, M. Global-Warming heat related illnesses and the dermatologist. Int. J. Women’s Dermatol. 2020. [Google Scholar] [CrossRef]
- Short, E.E.; Caminade, C.; Thomas, B.N. Climate Change Contribution to the Emergence or Re-Emergence of Parasitic Diseases. Infect. Dis. 2017, 10. [Google Scholar] [CrossRef] [PubMed]
- Mohankumar, S.; Kottaiveeran, K. Hospital waste management and environmental problems in India. Int. J. Pharm. Biol. Arch. 2011, 2, 1621–1626. [Google Scholar]
- Caniato, M.; Tudor, T.L.; Vaccari, M. Assessment of health-care waste management in a humanitarian crisis: A case study of the Gaza Strip. Waste Manag. 2016, 58, 386–396. [Google Scholar] [CrossRef]
- Leisinger, K.M.; Garabedian, L.F.; Wagner, A.K. Improving access to medicines in low- and middle-income countries: Corporate responsibilities in context. South. Med Rev. 2012, 5, 3–8. [Google Scholar]
- Vellinga, A.; Cormican, S. Public practice regarding disposal of unused medicines in Ireland. Sci. Total Environ. 2014, 478, 98–102. [Google Scholar] [CrossRef]
- Wieczorkiewicz, S.M.; Kassamali, Z.; Danziger, L.H. Behind Closed Doors: Medication Storage and Disposal in the Home. Ann. Pharmacother. 2013, 47, 482–489. [Google Scholar] [CrossRef]
- Antibiotics in Water and the Risk of Drug Resistant Bacteria, European Commission. Available online: https://ec.europa.eu/jrc/en/news/antibiotics-water-and-risk-drug-resistant-bacteria (accessed on 12 September 2020).
- Klemeš, J.J.; Van Fan, Y.; Tan, R.R.; Jiang, P. Minimising the present and future plastic waste, energy and environmental footprints related to COVID-19. Renew. Sustain. Energy Rev. 2020, 127. [Google Scholar] [CrossRef]
- Singh, N.; Tang, Y.; Zhang, Z.; Zheng, C. COVID-19 waste management: Effective and successful measures in Wuhan, China. Resour. Conserv. Recycl. 2020, 163. [Google Scholar] [CrossRef] [PubMed]
- Silva, P.L.; Prata, J.C.; Walker, T.R.; Campos, D.; Duarte, A.C.; Soares, A.M.V.M.; Rocha-Santos, T.; Barcelo, D. Rethinking and optimising plastic waste management under COVID-19 pandemic: Policy solutions based on redesign and reduction of single-use plastics and personal protective equipment. Sci. Total Environ. 2020, 742. [Google Scholar] [CrossRef]
- Sharma, H.B.; Vanapalli, K.R.; Cheela, V.S.; Ranjan, V.P.; Jaglan, A.K.; Dubey, B.; Goel, S.; Bhattacharya, J. Challenges, opportunities, and innovations for effective solid waste management during and post COVID-19 pandemic. Resour. Conserv. Recycl. 2020, 162. [Google Scholar] [CrossRef] [PubMed]
- Wilson, D.; Rodic, L.; Cowing, M.; Velis, C.; Whiteman, A.; Scheinberg, A.; Vilches, R.; Masterson, D.; Stretz, J.; Oelz, B. ‘Wasteaware’ benchmark inidicators for integrated sustainable waste management in cities. Waste Manag. 2015, 35, 329–342. [Google Scholar] [CrossRef] [PubMed]
- Khan, B.A.; Cheng, L.; Khan, A.A.; Ahmed, H. Healthcare waste management in Asian developing countries: A mini review. Waste Manag. Res. 2019, 37, 863–875. [Google Scholar] [CrossRef]
- Mohamed, L.F.; Ebrahim, S.A.; Al-Thukair, A.A. Hazardous healthcare waste management in the Kingdom of Bahrain. Waste Manag. 2009, 29, 2404–2409. [Google Scholar] [CrossRef] [PubMed]
- Deneke, I.; Aqiel, M.; Desalegn, B.; Atsbeha, H. Assessing the management of healthcare waste in Hawassa city, Ethiopia. Waste Manag. Res. 2011, 29, 854–862. [Google Scholar] [CrossRef] [PubMed]
- Sawalem, M.; Selic, E.; Herbell, J.-D. Hospital waste management in Libya: A case study. Waste Manag. 2009, 29, 1370–1375. [Google Scholar] [CrossRef] [PubMed]
- Safe Management of Wastes from Healthcare Activities, 2nd ed.; World Health Organisation: Geneva, Switzerland, 2014; ISBN 9789241548564.
- Mbongwe, B.; Mmereki, B.T.; Magashula, A. Healthcare waste management: Current practices in selected healthcare facilities, Botswana. Waste Manag. 2008, 28, 226–233. [Google Scholar] [CrossRef]
- Patwary, M.A.; O’Hare, W.T.; Sarker, M.H. Assessment of occupational and environmental safety associated with medical waste disposal in developing countries: A qualitative approach. Saf. Sci. 2011, 49, 1200–1207. [Google Scholar] [CrossRef]
- Mujeeb, S.A.; Adil, M.M.; Altaf, A.; Hutin, Y.; Luby, S. Recycling of Injection Equipment in Pakistan. Infect. Control Hosp. Epidemiol. 2003, 24, 145–146. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Becher, S.; Lichtnecker, H. Immunological aspects and affections of rubbish collectors caused by bioaerosols. J. Occup. Health 2002, 44, 125–130. [Google Scholar] [CrossRef]
- Elnour, A.M.; Reda Moussa, M.M.; El-Borgy, M.D.; Fadelella, N.E.E.; Hanafy Mahmoud, A. Impacts of health education on knowledge and practice of hospital staff with regard to Healthcare waste management at White Nile State main hospitals, Sudan. Int. J. Health Sci. (Qassim) 2015, 9, 315–331. [Google Scholar] [CrossRef]
- Ngwuluka, N.; Ochekpe, N.; Odumosu, P.; John, S.A. Waste management in healthcare establishments within Jos Metropolis, Nigeria. Afr. J. Environ. Sci. Technol. 2009, 3, 459–465. [Google Scholar]
- Kumar, M.; Kushwaha, R.; Maurya, M.K.; Singh, G.; Kumari, R. Knowledge, awareness and attitude regarding biomedical waste management among medical students in a tertiary health care centre: A cross sectional study. Indian J. Res. Med. Sci. 2017, 6, 611–614. [Google Scholar]
- Raila, E.M.; Anderson, D.O. Healthcare waste management during disasters and its effects on climate change: Lessons from 2010 earthquake and cholera tragedies in Haiti. Waste Manag. Res. 2017, 35, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Askarian, M.; Heidarpoor, P.; Assadian, O. A total quality management approach to healthcare waste management in Namazi Hospital, Iran. Waste Manag. 2010, 30, 2321–2326. [Google Scholar] [CrossRef] [PubMed]
- Adar, T.; Delice, E.K. New integrated approaches based on MC-HFLTS for healthcare waste treatment technology selection. J. Enterp. Inf. Manag. 2019, 32, 688–711. [Google Scholar] [CrossRef]
- Yazie, T.D.; Tebeje, M.G.; Chufa, K.A. Healthcare waste management current status and potential challenges in Ethiopia: A systematic review. BMC Res. Notes 2019, 12. [Google Scholar] [CrossRef] [PubMed]
| Region | Country | HCW Generated (kg/bed/day) | References |
|---|---|---|---|
| Europe | Ireland | 7.7 | [15] |
| UK | 3.3 | [16] | |
| Bulgaria | 2 | [16] | |
| Italy | 4 | [17] | |
| France | 3.3 | [16] | |
| Germany | 3.6 | [18] | |
| Greece | 3.6 | [19] | |
| Netherlands | 1.7 | [18] | |
| Norway | 3.9 | [16] | |
| Spain | 4.4 | [16] | |
| Latvia | 1.18 | [20] | |
| America | USA | 8.4 | [16] |
| Canada | 8.2 | [21] | |
| Argentina | 3 | [22] | |
| Brazil | 2.94 | [21] | |
| Ecuador | 2.09 | [23] | |
| El Salvador | 1.85 | [24] | |
| Asia | Bangladesh | 1.24 | [25] |
| China | 4.03 | [26] | |
| India | 1.55 | [25] | |
| Indonesia | 0.75 | [27] | |
| Iran | 3.04 | [25] | |
| Japan | 2.15 | [17,28] | |
| Jordan | 2.69 | [17] | |
| Korea | 2.4 | [29] | |
| Laos | 0.51 | [30] | |
| Malaysia | 1.9 | [25] | |
| Pakistan | 2.07 | [16] | |
| Palestine | 2.02 | [31] | |
| Thailand | 2.05 | [32] | |
| Turkey | 4.55 | [17] | |
| Nepal | 0.5 | [25] | |
| Lebanon | 5.7 | [33] | |
| Kazakhstan | 5.34 | [20] | |
| Vietnam | 1.57 | [25] | |
| Africa | Algeria | 0.96 | [34] |
| Cameroon | 0.55 | [35] | |
| Egypt | 1.03 | [36] | |
| Ethiopia | 1.1 | [37] | |
| Mauritius | 0.44 | [28] | |
| Morocco | 0.53 | [38] | |
| Sudan | 0.87 | [39] | |
| Tanzania | 0.75 | [17] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kenny, C.; Priyadarshini, A. Review of Current Healthcare Waste Management Methods and Their Effect on Global Health. Healthcare 2021, 9, 284. https://doi.org/10.3390/healthcare9030284
Kenny C, Priyadarshini A. Review of Current Healthcare Waste Management Methods and Their Effect on Global Health. Healthcare. 2021; 9(3):284. https://doi.org/10.3390/healthcare9030284
Chicago/Turabian StyleKenny, Christina, and Anushree Priyadarshini. 2021. "Review of Current Healthcare Waste Management Methods and Their Effect on Global Health" Healthcare 9, no. 3: 284. https://doi.org/10.3390/healthcare9030284
APA StyleKenny, C., & Priyadarshini, A. (2021). Review of Current Healthcare Waste Management Methods and Their Effect on Global Health. Healthcare, 9(3), 284. https://doi.org/10.3390/healthcare9030284







