Hand Areas Which Are Commonly Missed during Hand Disinfection by Nursing Students Who Completed a Basic Educational Course in Hand Hygiene
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Procedures
2.2. Statistical Analysis
3. Results
4. Discussion
5. Limitations of the Study
6. Conclusions
- The method of assessing the quality of disinfection applied in this study makes it possible to assess the correct performance of this procedure among nursing students.
- In the examined group of students significant problems in performing the procedure of hand disinfection were observed and they were connected mostly with thumbs of both hands and backs of both hands.
- It seems legitimate that regular training and assessment of the compliance with hand hygiene procedures should take place after completing each cycle of nursing education and special attention should be paid to controlling if the person responsible for training and assessing students also performs hand hygiene procedures in the correct way.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Liu, S.; Wang, M.; Wang, G.; Wu, X.; Guan, W.; Ren, J. Microbial characteristics of nosocomial infections and their association with the utilization of hand hygiene products: A hospital-wide analysis of 78,344 cases. Surg. Infect. 2017, 18, 676–683. [Google Scholar] [CrossRef] [PubMed]
- Jayaraman, S.; Klompas, M.; Bascom, M.; Liu, X.; Piszcz, R.; Rogers, S.; Askari, R. Hand-hygiene compliance does not predict rates of resistant infections in critically ill surgical patients. Surg. Infect. 2014, 15, 533–539. [Google Scholar] [CrossRef] [PubMed]
- Allegranzi, B.; Pittet, D. Role of hand hygiene in healthcare-associated infection prevention. Rev. J. Hosp. Infect. 2009, 73, 305–315. [Google Scholar] [CrossRef]
- Luangasanatip, N.; Hongsuwan, M.; Limmathurotsakul, D.; Lubell, Y.; Lee, A.; Harbarth, S.; Day, N.; Graves, N.; Cooper, B. Comparative efficacy of interventions to promote hand hygiene in hospital: Systematic review and network meta-analysis. BMJ 2015, 28, 351:h3728. [Google Scholar] [CrossRef]
- Rosenthal, V.D.; Pawar, M.; Leblebicioglu, H.; Navoa-Ng, J.A.; Villamil-Gómez, W.; Armas-Ruiz, A.; Cuéllar, L.E.; Medeiros, E.A.; Mitrev, Z.; Gikas, A.; et al. Impact of the International Nosocomial Infection Control Consortium (INICC) Multidimensional Hand Hygiene Approach over 13 Years in 51 Cities of 19 Limited-Resource Countries from Latin America, Asia, the Middle East, and Europe. Infect. Control Hosp. Epidemiol. 2013, 34, 415–423. [Google Scholar] [CrossRef]
- Szczypta, A.; Różańska, A.; Bulanda, M. Analysis of occupational exposure of healthcare workers in the years 1998-2013 for bloodborne pathogens on the example of the hospital of the surgical profile. Med. Pr. 2014, 65, 723–732. [Google Scholar] [CrossRef] [PubMed]
- Cristina, M.L.; Sartini, M.; Spagnolo, A.M. Serratia marcescens infections in Neonatal Intensive Care Units (NICUs). Int. J. Environ. Res. Public Health 2019, 16, 610. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Guidelines on Hand Hygiene in Health Care. First. Global Patient Safety Challenge. In Clean Care is Safer Care; WHO Press: Geneva, Swizerland, 2009. [Google Scholar]
- Sax, H.; Allegranzi, B.; Uckay, I.; Larson, E.; Boyce, J.; Pittet, D. My five moments for hand hygiene: A user-centred design approach to understand, train, monitor and report hand hygiene. J. Hosp. Infect. 2007, 67, 9–12. [Google Scholar] [CrossRef]
- Allegranzi, B.; Gayet-Ageron, A.; Damani, N.; Bengaly, L.; McLaws, M.L.; Moro, M.L.; Memish, Z.; Urroz, O.; Richet, H.; Storr, J.; et al. Global implementation of WHO’s multimodal strategy for improvement of hand hygiene: A quasi-experimental study. Lancet Infect. Dis. 2013, 13, 843–851. [Google Scholar] [CrossRef]
- Denisiewicz, B. Znaczenie higieny rąk w profilaktyce zakażeń związanych z opieką zdrowotną. Zakażenia XXI Wieku 2020, 3, 23–29. [Google Scholar]
- Pittet, D.; Simon, A.; Hugonnet, S.; Pessoa-Silva, C.L.; Sauvan, V.; Perneger, T.V. Hand hygiene among physicians: Performance, beliefs, and perceptions. Ann. Intern. Med. 2004, 141, 1–8. [Google Scholar] [CrossRef]
- Fredj, S.; Cheikh, A.B.; Bhiri, S.; Ghali, H.; Khefacha, S.; Dhidah, L.; Merzougui, L.; Rejeb, M.; Latiri, H.S. Multimodal intervention program to improve hand hygiene compliance: Effectiveness and challenges. J. Egypt. Public Health Assoc. 2020, 95, 11. [Google Scholar] [CrossRef] [PubMed]
- Ward, M.A.; Schweizer, M.L.; Polgreen, P.M.; Gupta, K.; Reisinger, H.S.; Perencevich, E.N. Automated and electronically assisted hand hygiene monitoring systems: A systematic review. Am. J. Infect. Control 2014, 42, 472–478. [Google Scholar] [CrossRef]
- Azim, S.; Juergens, C.; McLaws, M.L. An average hand hygiene day for nurses and physicians: The burden is not equal. Am. J. Infect. Control 2016, 44, 777–781. [Google Scholar] [CrossRef]
- Aghdassi, S.J.; Schröder, C.; Lemke, E.; Behnke, M.; Fliss, P.M.; Plotzki, C.; Wenk, J.; Gastmeier, P.; Kramer, S.Z. A multimodal intervention to improve hand hygiene compliance in peripheral wards of a tertiary care university centre: A cluster randomised controlled trial. Antimicrob. Resist. Infect. Control 2020, 18, 113. [Google Scholar] [CrossRef] [PubMed]
- Hynes, N. A Hand Hygiene Education and Training Improvement Strategy in an Acute Hospital Setting. Master’s Thesis, Dublin Royal College of Surgeons, Dublin, Ireland, 2015. [Google Scholar]
- Sopjani, I.; Jahn, P.; Behrens, J. Training as an effective tool to increase the knowledge about hand hygiene actions. An evaluation study of training effectiveness in Kosovo. Med. Arch. 2017, 71, 16–19. [Google Scholar] [CrossRef] [PubMed]
- Ellingson, K.; Haas, J.P.; Aiello, A.E.; Kusek, L.; Maragakis, L.L.; Olmsted, R.N.; Perencevich, E.; Polgreen, P.M.; Schweizer, M.L.; Trexler, P.; et al. Strategies to prevent healthcare-associated infections through hand hygiene. Infect. Control Hosp. Epidemiol. 2014, 35, 937–960. [Google Scholar] [CrossRef]
- Harbarth, S. What can we learn from each other in infection control? Experience in Europe compared with the USA. J. Hosp. Infect. 2013, 83, 173–184. [Google Scholar] [CrossRef] [PubMed]
- Barrett, R.; Randle, J. Hand hygiene practices: Nursing students’ perceptions. J. Clin. Nurs. 2008, 17, 1851–1857. [Google Scholar] [CrossRef]
- Nasirudeen, A.M.A.; Koh, J.W.N.; Lee, A.; Lau, C.; Li, W.; Lim, L.S.; Yi, C.; Ow, X. Hand hygiene knowledge and practices of nursing students in Singapore. Am. J. Infect. Control 2012, 40, e241–e243. [Google Scholar] [CrossRef]
- Bargellini, A.; Borella, P.; Ferri, P.; Ferranti, G.; Marchesi, I. Hand hygiene of medical and nursing students during clinica rotations: A pilot study on knowledge, attitudes and impact on bacterial contamination. Assist. Inferm. Ric. 2012, 31, 123–130. [Google Scholar]
- Cruz, J.C.; Bashtawi, M.A. Predictors of hand hygiene practice among Saudi nursing students: A cross-sectional self-reported study. J. Infect. Public Health 2016, 9, 485–493. [Google Scholar] [CrossRef]
- Różańska, A.; Wójkowska-Mach, J.; Bulanda, M. Work experience and seniority in health care vs. medical students’ knowledge of selected hand hygiene procedures. Med. Pr. 2016, 67, 623–633. [Google Scholar] [CrossRef]
- Khubrani, A.; Albesher, M.; Alkahtani, A.; Alamri, F.; Alshamrani, M.; Masuadi, E. Knowledge and information sources on standard precautions and infection control of health sciences students at King Saud bin Abdulaziz University for Health Sciences, Saudi Arabia, Riyadh. J. Infect. Public Health 2018, 11, 546–549. [Google Scholar] [CrossRef]
- Oyapero, A.; Oyapero, O. An assessment of hand hygiene perception and practices among undergraduate nursing students in Lagos State: A pilot study. J. Educ. Health Promot. 2018, 27, 150. [Google Scholar]
- Wałaszek, M.; Gniadek, A.; Kołpa, M.; Ogórek-Tęcza, B.; Szczypta, A.; Pustułka, B. Evaluation of nursing students’ preparation for their first contact with the patient in terms of hand hygiene. Nurs. Probl. 2018, 26, 123–129. [Google Scholar]
- Tem, C.; Kong, C.; Him, N.; Sann, N.; Chang, S.B.; Choi, J. Hand hygiene of nursing and midwifery students in Cambodia. Int. Nurs. Rev. 2019, 66, 523–529. [Google Scholar] [CrossRef]
- Elola-Vicente, P.; Aroca-Palencia, J.; Huertas-Paredero, M.V.; Díez-Sebastián, J.; Rivas-Bellido, L.; Martínez-Martínez, G.; Nájera-Santos, M.C.; Muñoz-García, M.L. A hand hygiene education program. Comparison between handwashing and the use of alcohol solutions. Comp. Study Enferm. Clin. 2008, 18, 5–10. [Google Scholar] [CrossRef]
- Piscitelli, A.; Agodi, A.; Agozzino, E.; Arrigoni, C.; Barchitta, M.; Brusaferro, S.; Castaldi, S.; Castiglia, P.; Cozzi, L.; D’Errico, M.M.; et al. The Clean Care Contest: Promoting hand hygiene among healthcare and medical students. Ann. Ig. 2020, 32, 462–471. [Google Scholar]
- Ott, L.K.; Irani, V.K. Evaluating the effectiveness of real-time feedback on the bedside hand hygiene behaviors of nursing students. J. Nurs. Educ. 2015, 54, 286–289. [Google Scholar] [CrossRef]
- Snow, M.; White, G.L.; Alder, S.C.; Stanford, S.B. Mentor’s hand hygiene practices influence student’s hand hygiene rates. Am. J. Infect. Control 2006, 34, 18–24. [Google Scholar] [CrossRef]
- Dembilio-Villar, T.; González-Chordá, V.M.; Cervera-Gasch, Á.; Mena-Tudela, D. Cooperative learning and hand disinfection in nursing students. Invest. Educ. Enferm. 2018, 36. [Google Scholar] [CrossRef] [PubMed]
- Ceylan, B.; Gunes, U.; Baran, L.; Ozturk, H.; Sahbudak, G. Examining the hand hygiene beliefs and practices of nursing students and the effectiveness of their handwashing behaviour. J. Clin. Nurs. 2020, 29, 4057–4065. [Google Scholar] [CrossRef]
- Kısacık, Ö.G.; Ciğerci, Y.; Güneş, Ü. Impact of the fluorescent concretization intervention on effectiveness of hand hygiene in nursing students: A randomized controlled study. Nurse Educ. Today 2021, 97, 104719. [Google Scholar] [CrossRef]
- Martos-Cabrera, M.B.; Mota-Romero, E.; Martos-García, R.; Gómez-Urquiza, J.L.; Suleiman-Martos, N.; Albendín-García, L.; A Cañadas-De la Fuente, G. Hand hygiene teaching strategies among nursing staff: A systematic review. Int. J. Environ. Res. Public Health 2019, 22, 3039. [Google Scholar] [CrossRef]
- Scheithauer, S.; Haefner, H.; Schwanz, T.; Lopez-Gonzalez, L.; Bank, C.; Schulze-Röbbecke, R.; Weishoff-Houben, M.; Lemmen, S. Hand hygiene in medical students: Performance, education and knowledge. Int. J. Hyg. Environ. Health 2012, 215, 536–539. [Google Scholar] [CrossRef]
- Öncü, E.; Vayısoğlu, S.K.; Lafcı, D.; Yıldız, E. An evaluation of the effectiveness of nursing students’ hand hygiene compliance: A cross-sectional study. Nurse Educ. Today 2018, 65, 218–224. [Google Scholar] [CrossRef]
- Graveto, J.M.; Figueira Rebola, J.B.; Fernandes, I.A.; Dos Santos Costa, P.J. Hand hygiene: Nurses’ adherence after training. Rev. Bras. Enferm. 2018, 71, 1189–1193. [Google Scholar] [CrossRef]
- van de Mortel, T.F.; Apostolopoulou, E.; Petrikkos, G. A comparison of the hand hygiene knowledge, beliefs, and practices of Greek nursing and medical students. Am. J. Infect. Control 2010, 38, 75–77. [Google Scholar] [CrossRef]
- Colosi, A.; Ergasti, G.; Murzilli, G.; Paolini, V.; Semeraro, V.; Trapani, M.M.; D’Alessandro, D. Healthcare students and their knowledge of healthcareassociated infections. Ann. Ig. 2011, 23, 203–208. [Google Scholar] [PubMed]
- Wałaszek, M.; Kołpa, M.; Różańska, A.; Wolak, Z.; Bulanda, M.; Wójkowska-Mach, J. Practice of hand hygiene and use of protective gloves: Differences in the perception between patients and medical staff. Am. J. Infect. Control 2018, 46, 1074–1076. [Google Scholar] [CrossRef]
- Oh, H.S. Knowledge, perception, performance, and attitude regarding hand hygiene and related factors among infection control nurses in South Korea: A cross-sectional study. Am. J. Infect. Control 2019, 47, 258–263. [Google Scholar] [CrossRef]
- Kelcikova, S.; Mazuchova, L.; Bielena, L.; Filova, L. Flawed self-assessment in hand hygiene: A major contributor to infections in clinical practice? J. Clin. Nurs. 2019, 28, 2265–2275. [Google Scholar] [CrossRef] [PubMed]
- Garus-Pakowska, A.; Sobala, W.; Szatko, F. Observance of hand washing procedures performed by the medical personnel before patient contact. Part I. Int. J. Occup. Med. Environ. Health 2013, 26, 113–121. [Google Scholar] [CrossRef]
- Onyedibe, K.I.; Shehu, N.Y.; Pires, D.; Isa, S.E.; Okolo, M.O.; Gomerep, S.S.; Ibrahim, C.; Igbanugo, S.J.; Odesanya, R.U.; Olayinka, A.; et al. Assessment of hand hygiene facilities and staff compliance in a large tertiary health care facility in northern Nigeria: A cross sectional study. Antimicrob. Resist. Infect. Control 2020, 11, 30. [Google Scholar] [CrossRef]
- Keller, J.; Wolfensberger, A.; Clack, L.; Kuster, S.P.; Dunic, M.; Eis, D.; Flammer, Y.; Keller, D.I.; Sax, H. Do wearable alcohol-based handrub dispensers increase hand hygiene compliance?—a mixed-methods study. Antimicrob. Resist. Infect. Control 2018, 23, 143. [Google Scholar] [CrossRef]
- Gould, D.J.; Moralejo, D.; Drey, N.; Chudleigh, J.H.; Taljaard, M. Interventions to improve hand hygiene compliance in patient care. Cochrane Database Syst. Rev. 2017, 9, CD005186. [Google Scholar]
- Stone, P.S.; Fuller, C.; Savage, J.; Cookson, B.; Hayward, A.; Cooper, B.; Duckworth, G.; Michie, S.; Murray, M.; Jeanes, A.; et al. Evaluation of the national Cleanyourhands campaign to reduce Staphylococcus aureus bacteraemia and Clostridium difficile infection in hospitals in England and Wales by improved hand hygiene: Four year, prospective, ecological, interrupted time series study. BMJ 2012, 344, e3005. [Google Scholar] [CrossRef]
- Zomer, T.P.; Erasmus, V.; Looman, C.W.; Tjon-A-Tsien, A.; Van Beeck, E.F.; De Graaf, J.M.; Van Beeck, A.H.E.; Richardus, J.H.; Voeten, H.C.M.V. A hand hygiene intervention to reduce infections in child day care: A randomized controlled trial. Epidemiol. Infect. 2015, 143, 2494–2502. [Google Scholar] [CrossRef]
- Kawalec, A.; Pawlas, K. Compliance with hygiene procedures among medical faculty students. Med. Pr. 2014, 65, 593–599. [Google Scholar]
- Wałaszek, M.; Kołpa, M.; Wolak, Z.; Różańska, A.; Wójkowska-Mach, J. Poor hand hygiene procedure compliance among Polish medical students and physicians-the result of an ineffective education basis or the impact of organizational culture? Int. J. Environ. Res. Public Health 2017, 14, 1026. [Google Scholar] [CrossRef]
- Kelcíkova, S.; Skodova, Z.; Straka, S. Effectiveness of hand hygiene education in a basic nursing school curricula. Public Health Nurs. 2012, 29, 152–159. [Google Scholar] [CrossRef]
- Huis, A.; Achterberg, T.; Bruin, M.; Grol, R.; Schoonhoven, L.; Hulscher, M. A systematic review of hand hygiene improvement strategies: A behavioural approach. Implement. Sci. 2012, 7, 92. [Google Scholar] [CrossRef]
- Kim, E.; Kim, S.S.; Kim, S. Effects of infection control education for nursing students using standardized patients vs. peer role-play. J. Environ. Res. Public Health 2021, 18, 107. [Google Scholar] [CrossRef]
- Widmer, A.E.; Dangel, M. Alcohol-based handrub: Evaluation of technique and microbiological efficacy with international infection control professionals. Infect. Control Hosp. Epidemiol. 2004, 25, 207–209. [Google Scholar] [CrossRef]
- Szilágyi, L.; Haidegger, T.; Lehotsky, Á.; Nagy, M.; Csonka, E.-A.; Sun, X.; Li Ooi, K.; Fisher, D. A large-scale assessment of hand hygiene quality and the effectiveness of the “WHO 6-steps”. BMC Infect. Dis. 2013, 13, 249. [Google Scholar] [CrossRef]
- Cichońska, M. Profesjonalne rozwiązania w higienie rąk personelu medycznego zwiększające skuteczność walki z zakażeniami szpitalnymi. Zakażenia XXI Wieku 2019, 2, 249–252. [Google Scholar]
- Kingston, L.M.; Slevin, B.L.; O’Connell, N.H.; Dunne, C.P. Hand hygiene: Attitudes and practices of nurses, a comparison between 2007 and 2015. Am. J. Infect. Control 2017, 45, 1300–1307. [Google Scholar] [CrossRef]
- Al Kuwaiti, A. Impact of a multicomponent hand hygiene intervention strategy in reducing infection rates at a university hospital in Saudi Arabia. Int. Med. Appl. Sci. 2017, 9, 137–143. [Google Scholar] [CrossRef]
- Al-Khawaldeh, O.A.; Al-Hussami, M.; Darawad, M. Influence of nursing students handwashing knowledge, beliefs, and attitudes on their handwashing compliance. Health 2015, 7, 572–579. [Google Scholar] [CrossRef]
- Kingston, L.M.; O’Connell, N.H.; Dunne, C.P. Survey of attitudes and practices of Irish nursing students towards hand hygiene, including handrubbing with alcohol-based hand rub. Nurse Educ. Today 2017, 52, 57–62. [Google Scholar] [CrossRef] [PubMed]
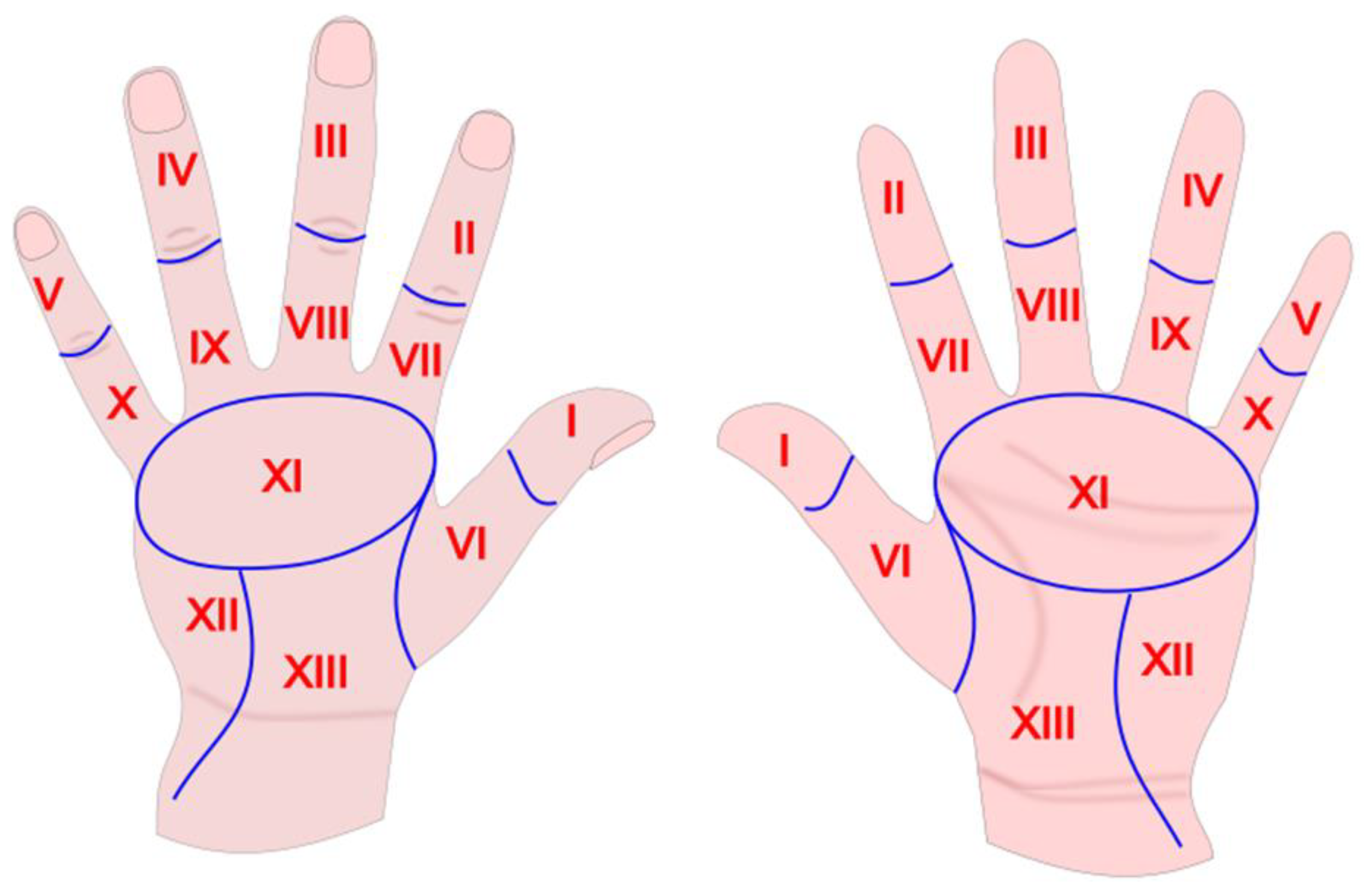


| Statistics | Area of the Hand | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I n = 190 | II n = 190 | III n = 190 | IV n = 190 | V n = 190 | VI n = 190 | VII n = 190 | VIII n = 190 | IX n = 190 | X n = 190 | XI n = 190 | XII n = 190 | XIII n = 190 | p * | |
| Palm of the left hand | ||||||||||||||
| completely clean, n (%) | 171 (90) | 179 (94) | 182 (96) | 182 (96) | 169 (89) | 168 (88) | 179 (94) | 180 (95) | 179 (94) | 177 (93) | 186 (98) | 184 (97) | 175 (92) | |
| completely dirty, n (%) | 6 (3) | 5 (3) | 4 (2) | 4 (2) | 9 (5) | 6 (3) | 4 (2) | 4 (2) | 4 (2) | 8 (4) | 4 (2) | 4 (2) | 5 (3) | |
| percentiles 90 (85–95) | 0 (0–42) | 0 (0–5) | 0 (0–0) | 0 (0–0) | 5 (0–72) | 5 (0–40) | 0 (0–5) | 0 (0–3) | 0 (0–5) | 0 (0–5) | 0 (0–0) | 0 (0–0) | 0 (0–28) | 0.0201 |
| Palm of the right hand | ||||||||||||||
| completely clean, n (%) | 173 (91) | 181 (95) | 181 (95) | 179 (94) | 178 (94) | 169 (89) | 183 (96) | 181 (95) | 179 (94) | 180 (95) | 184 (97) | 183 (96) | 174 (92) | |
| completely dirty, n (%) | 8 (4) | 6 (3) | 5 (3) | 7 (4) | 7 (4) | 7 (4) | 4 (2) | 4 (2) | 5 (3) | 5 (3) | 4 (2) | 3 (2) | 5 (3) | |
| percentiles 90 (85–95) | 0 (0–78) | 0 (0–0) | 0 (0–0) | 0 (0–8) | 0 (0–8) | 6 (0–58) | 0 (0–0) | 0 (0–0) | 0 (0–8) | 0 (0–3) | 0 (0–0) | 0 (0–0) | 0 (0–21) | 0.0455 |
| Back of the left hand | ||||||||||||||
| completely clean, n (%) | 106 (56) | 112 (59) | 113 (59) | 119 (63) | 122 (64) | 117 (62) | 143 (75) | 145 (76) | 147 (77) | 149 (78) | 154 (81) | 146 (77) | 134 (71) | |
| completely dirty, n (%) | 29 (15) | 26 (14) | 30 (16) | 29 (15) | 30 (16) | 4 (2) | 24 (13) | 24 (13) | 19 (10) | 22 (12) | 20 (11) | 16 (8) | 18 (9) | |
| percentiles 80 (70–90) | 52 (20–100) | 32 (16–100) | 35 (17–100) | 36 (15–100) | 40 (11–100) | 20 (15–36) | 10 (0–100) | 10 (0–100) | 5 (0–82) | 5 (0–100) | 0 (0–100) | 10 (0–66) | 20 (0–81) | 0.0548 |
| Back of the right hand | ||||||||||||||
| completely clean, n (%) | 89 (47) | 112 (59) | 106 (56) | 115 (61) | 119 (63) | 108 (57) | 136 (72) | 130 (68) | 136 (72) | 139 (73) | 147 (77) | 141 (74) | 123 (65) | |
| completely dirty, n (%) | 37 (19) | 34 (18) | 33 (17) | 32 (17) | 32 (17) | 16 (8) | 33 (17) | 33 (17) | 25 (13) | 30 (16) | 26 (14) | 25 (13) | 32 (17) | |
| percentiles 80 (70–90) | 91 (37–100) | 65 (20–100) | 72 (30–100) | 50 (20–100) | 50 (15–100) | 30 (15–90) | 16 (0–100) | 51 (5–100) | 11 (0–100) | 10 (0–100) | 16 (0–100) | 20 (0–100) | 36 (15–100) | 0.0001 |
| Palm of the Left Hand (n = 190) | Palm of the Right Hand (n = 190) | Back of the Left Hand (n = 190) | Back of the Right Hand (n = 190) | |
|---|---|---|---|---|
| Area | Dirt ≥ 10% | Dirt ≥ 10% | Dirt ≥ 10% | Dirt ≥ 10% |
| I | 14 (7.37) | 14 (7.37) | 76 (40) | 89 (46.84) |
| II | 8 (4.21) | 7 (3.68) | 69 (36.32) | 71 (37.37) |
| III | 5 (2.63) | 6 (3.16) | 69 (36.32) | 78 (41.05) |
| IV | 5 (2.63) | 10 (5.26) | 63 (33.16) | 71 (37.37) |
| V | 16 (8.42) | 10 (5.26) | 59 (31.05) | 66 (34.74) |
| VI | 18 (9.47) | 19 (10) | 66 (34.74) | 78 (41.05) |
| VII | 8 (4.21) | 5 (2.63) | 41 (21.58) | 46 (24.21) |
| VIII | 7 (3.68) | 7 (3.68) | 39 (20.53) | 53 (27.89) |
| IX | 7 (3.68) | 10 (5.26) | 36 (18.95) | 45 (23.68) |
| X | 9 (4.74) | 8 (4.21) | 34 (17.89) | 44 (23.16) |
| XI | 4 (2.11) | 6 (3.16) | 31 (16.32) | 42 (22.11) |
| XII | 6 (3.16) | 7 (3.68) | 43 (22.63) | 48 (25.26) |
| XIII | 15 (7.89) | 14 (7.37) | 51 (26.84) | 64 (33.68) |
| χ2 | 55.7 | 40.6 | 141.6 | 136.6 |
| p ** | <0.001 | <0.001 | <0.001 | <0.001 |
| Total Number of Areas with Dirt ≥ 10% | 0 | 1–2 | 3–10 | >10 |
|---|---|---|---|---|
| Palm of left hand, areas I-XIII | 148 (78) | 32 (17) | 6 (3) | 4 (2) |
| Palm of right hand, areas I-XIII | 148 (78) | 30 (16) | 9 (5) | 3 (2) |
| Back of left hand, areas I-XIII | 59 (31) | 48 (25) | 63 (33) | 20 (11) |
| Back of right hand, areas I-XIII | 44 (23) | 54 (28) | 64 (34) | 28 (15) |
| Both palms of hands, areas 2x (I-XIII) | 140 (74) | 25 (13) | 20 (11) | 5 (3) |
| Both backs of hands, areas 2x (I-XIII) | 34 (18) | 50 (26) | 43 (23) | 63 (33) |
| Both palms, backs of hands, areas 4x (I-XIII) | 30 (16) | 50 (26) | 47 (25) | 63 (33) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gniadek, A.; Ogórek-Tęcza, B.; Inglot, A.; Nowacka, A.; Micek, A. Hand Areas Which Are Commonly Missed during Hand Disinfection by Nursing Students Who Completed a Basic Educational Course in Hand Hygiene. Int. J. Environ. Res. Public Health 2021, 18, 2590. https://doi.org/10.3390/ijerph18052590
Gniadek A, Ogórek-Tęcza B, Inglot A, Nowacka A, Micek A. Hand Areas Which Are Commonly Missed during Hand Disinfection by Nursing Students Who Completed a Basic Educational Course in Hand Hygiene. International Journal of Environmental Research and Public Health. 2021; 18(5):2590. https://doi.org/10.3390/ijerph18052590
Chicago/Turabian StyleGniadek, Agnieszka, Beata Ogórek-Tęcza, Anna Inglot, Anna Nowacka, and Agnieszka Micek. 2021. "Hand Areas Which Are Commonly Missed during Hand Disinfection by Nursing Students Who Completed a Basic Educational Course in Hand Hygiene" International Journal of Environmental Research and Public Health 18, no. 5: 2590. https://doi.org/10.3390/ijerph18052590
APA StyleGniadek, A., Ogórek-Tęcza, B., Inglot, A., Nowacka, A., & Micek, A. (2021). Hand Areas Which Are Commonly Missed during Hand Disinfection by Nursing Students Who Completed a Basic Educational Course in Hand Hygiene. International Journal of Environmental Research and Public Health, 18(5), 2590. https://doi.org/10.3390/ijerph18052590






