Abstract
This study investigated the feasibility of using an automated facial coding engine, Affectiva (integrated in iMotions, version 8.2), for evaluating facial expression after traumatic brain injury (TBI). An observational cross-sectional study was conducted based on facial expression data from videos of participants with TBI and control participants. The aims were to compare TBI and control groups, and identify confounding factors affecting the data analysis. Video samples of two narrative tasks (personal event and story retell) from ten participants with severe TBI and ten control participants without TBI were analyzed using Affectiva. Automated data on participants’ engagement, smile and brow furrow were compared statistically between and within groups. Qualitative notes for each sample were also recorded. Affectiva detected a higher percentage of time of engagement for TBI participants than for control participants on both tasks. There was also a higher percentage of time of smiling for TBI participants in one task. Within groups, there were no significant differences between the two narrative tasks. Affectiva provides standardized data about facial expression and may be sensitive to detecting change in the use of facial expression after TBI. This study also identified factors to avoid during videorecording to ensure high quality samples for future research.
1. Introduction
Social communication deficits are common after people sustain a traumatic brain injury (TBI) [1]. These communication difficulties are at the level of discourse often beyond words and sentences so that people with TBI may struggle to communicate well in social and conversational contexts but show no marked deficits in speech or language [2].
A successful conversation is dependent on the content of discourse and the non-verbal aspects of communication, including the ability to interpret and use facial expression. Ruusuvuori and Peräkylä [3] noted that facial expression is a resource both for the person and their conversation partners, and it serves in the construction of meaning and formation of relationships between them. People with TBI have difficulties identifying people’s emotions based on situational and contextual cues [4,5]. Furthermore, difficulty using facial expressions after TBI can also impair their ability to react in socially appropriate ways to different communication situations [6]. Deficits in the interpretation and use of facial expression could lead to communication breakdown, and consequently, difficulty with social integration [7,8]. As a result, people with TBI may be perceived as less socially competent [9,10], and interactions with them regarded as less enjoyable and rewarding [9]. This breakdown in social communication can be a barrier in the formation and maintenance of relationships [11,12,13,14] and can be associated with decline in social networks, strain on families, and disruption to social lives [14,15,16].
While the impact of difficulty in interpreting facial expressions on social communication after brain injury is well recognized, the ability to use facial expression successfully is less well understood. For some individuals with TBI, facial expression during social communication is impaired, including a lack of expression [17], or using facial expression inappropriately due to disinhibition [6,18]. One study found that people with TBI had difficulty adapting their facial expressions to show different emotions while reading neutral sentences in a structured assessment task, as compared to people without a TBI [19]. However, there is limited research in this field, and it is important to investigate the use of facial expression to better understand the profile of impairments after TBI that could be targeted during rehabilitation to support more successful and enjoyable conversations. Given that the use of facial expression during communication will be affected by context, it is also relevant to explore whether different communication tasks elicit greater display of expression, whether negative or positive. For example, speakers retelling a significant injury or illness may use facial expression to underscore the seriousness of the event. A retelling of an impersonal narrative, such as a fairytale, may have less emotional weight, but speakers might still use facial expression for dramatic effect to engage the listener. Therefore, the use of facial expression in different communication contexts is an area worthy of further investigation, which could help develop future research and clinical tools for people with TBI.
There are standardized assessment measures to evaluate recognition of facial expression, such as The Awareness of Social Inference Test (TASIT) [20]. However, there are no standardized measures to evaluate the use of facial expression after brain injury. Existing tools for evaluating non-verbal communication of people with TBI, including facial expression, are based on the subjective judgment of the speech pathologist, and involve global ratings, such as whether a behavior is appropriate or inappropriate [21,22]. The development of technology has allowed automated recognition of facial expressions during video samples of conversation, which could provide more specific information about how people with TBI use facial expressions. Affectiva is a potential, and yet untapped, automated software analysis resource that may be beneficial in evaluating the use of facial expression by people with TBI. Affectiva’s AFFDEX [23] is a software program integrated into the platform called iMotions (Version 8.2). iMotions combines and synchronizes different types of biosensors such as eye tracking, facial expression analysis, electrodermal activity, from various independent vendors into a single platform [24]. Affectiva is the automated facial coding engine used by iMotions for facial expression analysis. The software has a coding system which analyzes facial expressions based on processing video samples using automated computer algorithms [25]. It measures ‘7 core emotions—joy, anger, fear, disgust, contempt, sadness, and surprise’ through 20 facial action units [25]. Affectiva has been measured against results produced by facial electromyography, and demonstrated validity, with high correlations, in identifying facial expressions and related emotions [26]. Affectiva has been used in previous clinical studies examining facial expression of individuals with autism and individuals with dementia in Parkinson’s Disease. In autism research, Affectiva was integrated into an emotion recognition game to provide automatic recognition and evaluation of users’ emotions from facial expression [27]. In a study focusing on dementia in individuals with Parkinson’s Disease, Affectiva was used to quantify the participants’ difficulty in facial expression imitation tasks [28]. These studies indicate that Affectiva may be useful to evaluate facial expression in clinical populations, but this software has not previously been applied to research in TBI. Furthermore, the feasibility of using Affectiva to evaluate use of facial expression during communication tasks has not been investigated.
Aims
This study investigated the use of Affectiva as a potential objective measure of facial expression during communication in speakers with TBI to answer the following research questions:
- Were there any differences in the use of facial expression between TBI participants and controls during narrative tasks using Affectiva?
- Were there any differences in the use of facial expression between a personal event narrative task and a story narrative retell task?
- Were there any confounding factors in video samples that may influence the validity or feasibility of the Affectiva analysis?
2. Materials and Methods
2.1. Study Design
An observational, cross-sectional study was conducted using previously collected video samples from an existing database namely TalkBank [29]. The original data was obtained within ethical protocols. TalkBank had received informed consent release from the individual participants when the data was collected. The participants understood that the data collected would be used by researchers and educators. As Affectiva has not previously been used for evaluating the use of facial expression during communication tasks, this was considered to be a pilot feasibility study.
2.2. Participants
2.2.1. Selection of Participants
Participants for this study were drawn from TalkBank, specifically the TBI Bank [30] and Aphasia Bank corpora [31].TBI Bank is a databank that includes people with TBI whereas Aphasia Bank is a databank that includes controls without a brain injury and people with aphasia. The controls without a brain injury drawn from Aphasia Bank were the control group for this study. Both databanks comprise videotaped samples of participants completing standardized discourse tasks based on a structured protocol, including a personal event narrative task and a story narrative retell. Demographic data for participants who have contributed video samples is also available within these established databanks.
The inclusion criteria for selection of participant video samples were:
- (a)
- Participants were aged between 18–65 years;
- (b)
- Video samples were available for both a personal event narrative task and a story narrative retell. For participants with TBI, it was required that these video samples be available from their 6 month post-injury assessment.
- (c)
- Participants had a severe TBI, with injury severity determined by length of post traumatic amnesia (PTA), whereby a person with severe injury has PTA > 24 h [32,33].
- (d)
- Narrative tasks were spoken in English
The exclusion criterion for selection of video samples was:
- (a)
- Participant videos that were unable to be processed sufficiently for analysis (less than 70% of the video sample processed) by Affectiva. For example, where the participant was not front-facing the camera, or poor lighting conditions.
2.2.2. Matching of TBI and Control Participants
A sample of 10 participants who had a TBI and 10 participants who did not have a TBI (control participants) was included in this study, with participants matched in pairs based on demographic characteristics. Figure 1 is a flow diagram showing the criteria and process for matching participants. Participants were first selected according to the four inclusion criteria. Participants with TBI were then matched with controls according to gender, age, and years of education following a two-step process as shown in Figure 1. Matched pairs in which either participant had samples which did not meet the criterion for video quality were excluded. The matching process created a cohort of eight matched pairs. To increase our sample size to ten matched pairs, we repeated the matching process according to our inclusion, exclusion, and matching criteria and identified a further two matched pairs by re-matching individuals with adequate video quality from the originally excluded pairs.
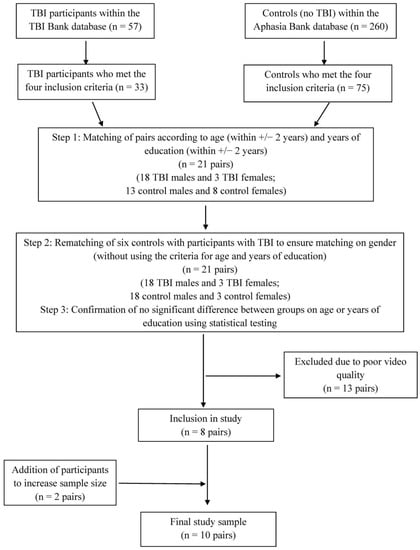
Figure 1.
Flow diagram for study participants.
2.2.3. Participants with TBI
There were nine males and one female, with ages ranging from 24 to 54 years (mean = 37.8, SD = 10.63), and years of education ranging from 10 to 18 (mean = 14.5, SD = 2.88). All participants resided in Australia at the time of data collection. All participants had severe TBI, with PTA ranging from 14–103 days. Table 1 below presents further information on the participants with TBI.

Table 1.
Demographics of participants with TBI.
2.2.4. Controls
The control group comprised of nine males and one female, with ages ranging from 23 to 57.5 years (mean = 38.3, SD = 11.42), and years of education ranging from 12 to 18 years (mean = 15.3, SD = 2.11). All the participants in the control group resided in the United States at the time of data collection and had no history of stroke, head injury, neurological condition, or communication disorder. Table 2 below presents further information on the controls.

Table 2.
Demographics of controls.
2.2.5. Comparison between Groups
Comparison between groups demonstrated the TBI and control groups were well-matched. The gender distributions in both TBI and control groups were the same (nine males and one female). There were no significant differences statistically between the two groups for age (t = 0.09, p = 0.93) or years of education (t = 0.71, p = 0.49).
2.3. Video Samples
2.3.1. Narrative Tasks
This study focused on two narrative tasks, which were personal event narrative and story narrative retell. Narrative story telling is a well-researched discourse type [34] commonly used in daily conversations [35]. Stark [36] found that narrative discourse elicited the densest language as compared to picture description and procedural discourse (with procedural discourse eliciting the shortest mean length of utterance). It was of interest to compare two different narrative discourse tasks, to determine whether speakers with or without a TBI adapt their use of facial expression for different contexts. For example, it is possible that the personal event narrative, about a significant illness or injury, may elicit more use of facial expression than a story narrative retell task.
Elicitation of the narrative discourse tasks was undertaken by qualified speech pathologists who used standardized protocol instructions and scripts [30,31].
- (a)
- Personal event narrative
Participants with TBI and controls were asked to talk about their brain injury and an episode of personal illness, respectively. Step-by-step instructions were given to the examiner to follow. The elicitation prompts are as follows:
- i.
- For participants with TBI, “Tell me what you remember about when you had your head injury”.
- ii.
- For controls, “I wonder if you could tell me what you remember about any illness or injury you’ve had”.
When the participants had difficulties providing responses, the examiner would proceed to use troubleshooting questions.
- (b)
- Story narrative retell
Story narrative was elicited using the ‘Cinderella’ story. The person was asked to tell the story of Cinderella, following the viewing of a wordless picture book. Similar to the personal event narrative, the examiner provided elicitation prompts according to the protocol instructions. If the participant had any difficulty, the examiner would prompt further for more information.
For the TBI participants, video samples ranged in length from 00:16 to 02:08 min for the personal event narrative task, and 00:56 to 03:33 for the story narrative retell task. For the control participants, video samples ranged in length from 00:22 to 03:01 for the personal event narrative task, and 01:03 to 05:31 for the story narrative retell task. There was no significant difference (p = 0.052, U = 24.00) between the TBI and control groups on the personal event narrative. The TBI group tended to speak for a shorter duration (median = 00:34) as compared to the control group (median = 01:20). For the story narrative retell task, there was a significant difference (t = 2.64, p = 0.02) between the duration of video samples of TBI (mean = 02:22, SD = 00:54) and control (mean= 03:44, SD = 01:21) participants.
2.3.2. Affectiva Analysis
The last author completed two, one-hour iMotions onboarding sessions to learn about the functionality of the platform and the analysis, and then provided orientation training to the first author. Videos extracted from TBI Bank and Aphasia Bank were edited by the first author to create video samples for analysis. Video samples commenced from when the participant started speaking and finished when the participant stopped speaking. Any verbal prompts from the examiner were cropped out of the sample. The first author then imported the video samples into the iMotions platform and analyzed them using the automated facial coding engine Affectiva. According to iMotions’ facial expression analysis guidebook [23], automatic facial coding consists of three elemental steps: face detection, feature detection, and feature classification. An example demonstrating the three steps of automatic facial coding in Affectiva is shown in Figure 2. In face detection, the face is detected and framed in a box. The next step is feature detection, where facial landmarks (e.g., eyes, brows, and mouth corners) are detected (as marked by dot points in Figure 2) and adjusted according to scale. Lastly, in feature classification, information on the key features is obtained and inputted into the classification algorithms. The program then translates the features into facial expression metrics, represented in the three traces, with engagement, brow furrow, and smile being analyzed in Figure 2.
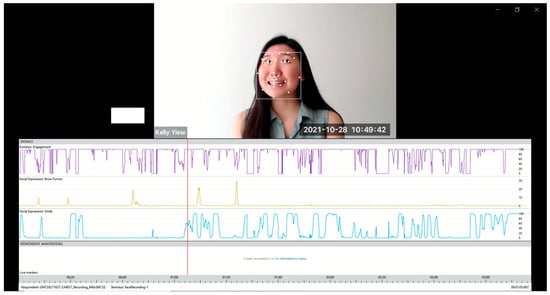
Figure 2.
Screenshot demonstrating Affectiva functions.
2.3.3. Facial Measures
This study focused on three facial measures, which were engagement, smile, and brow furrow. When using Affectiva, engagement is described as a measure of facial muscle activation that displays the individual’s expressiveness [37]. ‘Engagement’ was a relevant measure as it allowed us to examine the overall facial animation of the participants, which we anticipated would provide an overall measure of whether speakers were displaying flattened or heightened affect during the discourse sample. ‘Smile’ and ‘brow furrow’ were selected as facial expression measures to include measures associated with positive and negative emotions, respectively. These two expressions also have a high accuracy of detection [37]. A low threshold of 2/100 (representing a 2% probability that the expression was present) was set to ensure that all data was presented in order to assess the data optimally. Time percentages for engagement, smile, and brow furrow across the participants’ interactions were generated by Affectiva. The use of time percentages in the analysis of the measures controlled for the differences in sample duration between the groups.
2.3.4. Qualitative Observation
Qualitative notes for the video samples were recorded by the first author using an observation guide. Table 3 shows an example of how the qualitative observations were recorded. A frequency rating scale of 1 to 5 was used to rate the video samples to provide an overall, global clinical impression of the frequency of facial expression during a video sample. A rating of 1 represented the participant never showed any signs of the specific facial measure, 2 represented rarely, 3 represented sometimes, 4 represented often, and 5 represented always. This simple scale provided a clinician-driven gauge of the frequency of the participants using their facial expressions according to the facial measures, to categorise whether they were overly expressive or having a flat affect. This process also guided the analysis of our results as we reviewed Affectiva outlier data by comparing it against our qualitative observations. Clinical impressions included any other observations such as pragmatics and discourse. An overall impression of whether the participant’s interaction was socially appropriate was recorded. To reduce bias on clinical impressions, the qualitative observation process was conducted before statistical analysis of the Affectiva data.

Table 3.
Example of qualitative notes using an observation guide.
To develop consensus between study authors in the use of the observation guide, 13 video samples were selected at random (33%) from both TBI and control groups to be clinically analyzed between all authors. The authors included a student speech pathologist and four speech pathologists experienced in the field of TBI rehabilitation. The authors first rated the video samples independently. Consensus discussions were then held to establish agreement of the ratings between the authors, with qualitative notes on the clinical contexts and clinical impressions also discussed. Once consensus regarding the procedure was established, the first author then independently rated the remaining samples.
2.4. Data Analysis
Data analysis was supported using SPSS statistical software (IBM SPSS, Version 26). Firstly, the duration of the video samples for the personal event narrative and story narrative retell tasks were compared to identify any differences between the two tasks. Independent samples t-tests were used for normally distributed data and independent-samples Mann–Whitney U tests were used for non-normally distributed data.
For research question 1, independent-samples Mann–Whitney U tests were conducted to compare data between TBI and control participants for each narrative type. For research question 2, related-samples Wilcoxon signed rank tests were conducted to determine whether there were significant differences within the two different narrative types for the TBI participants, and for the control participants. The Bonferroni correction was considered but due to the need guard against type 2 errors in early pilot research, the correction was not applied [38,39]. For research question 3, samples where outliers were identified in the Affectiva data were examined as case studies to explore any confounding factors.
3. Results
3.1. Affectiva Data
Data for individual participants are reported in Table 4 and Table 5. To address research question 1, statistical comparisons between participants with TBI and controls for the personal event narrative and story narrative retell are presented in Table 6 and Table 7, respectively.

Table 4.
Results generated by Affectiva of TBI participants and control participants on personal event narrative.

Table 5.
Results generated by Affectiva of TBI participants and control participants on story narrative retell.

Table 6.
Comparison of TBI and control participants on personal event narrative.

Table 7.
Comparison of TBI and control participants on story narrative retell.
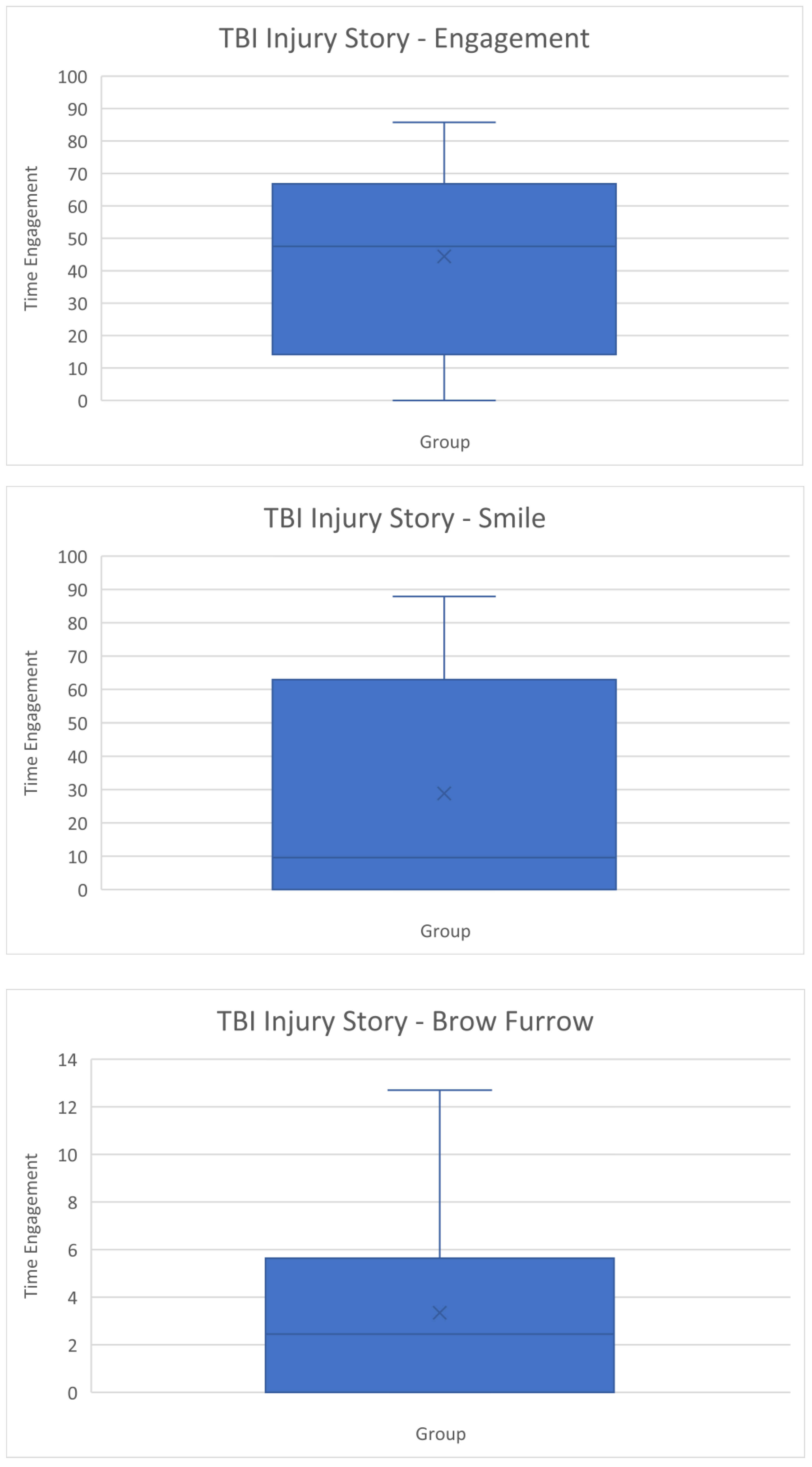
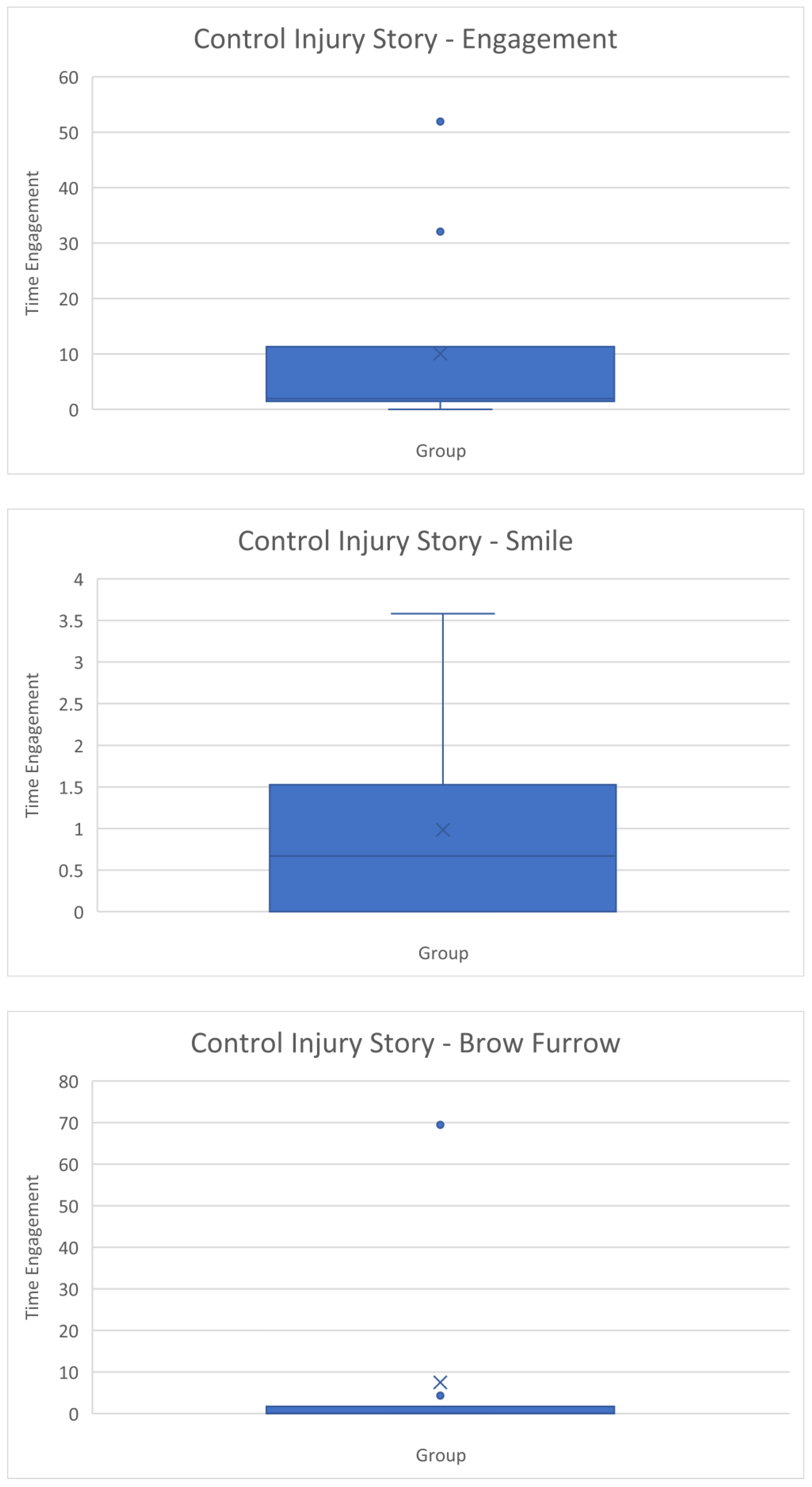
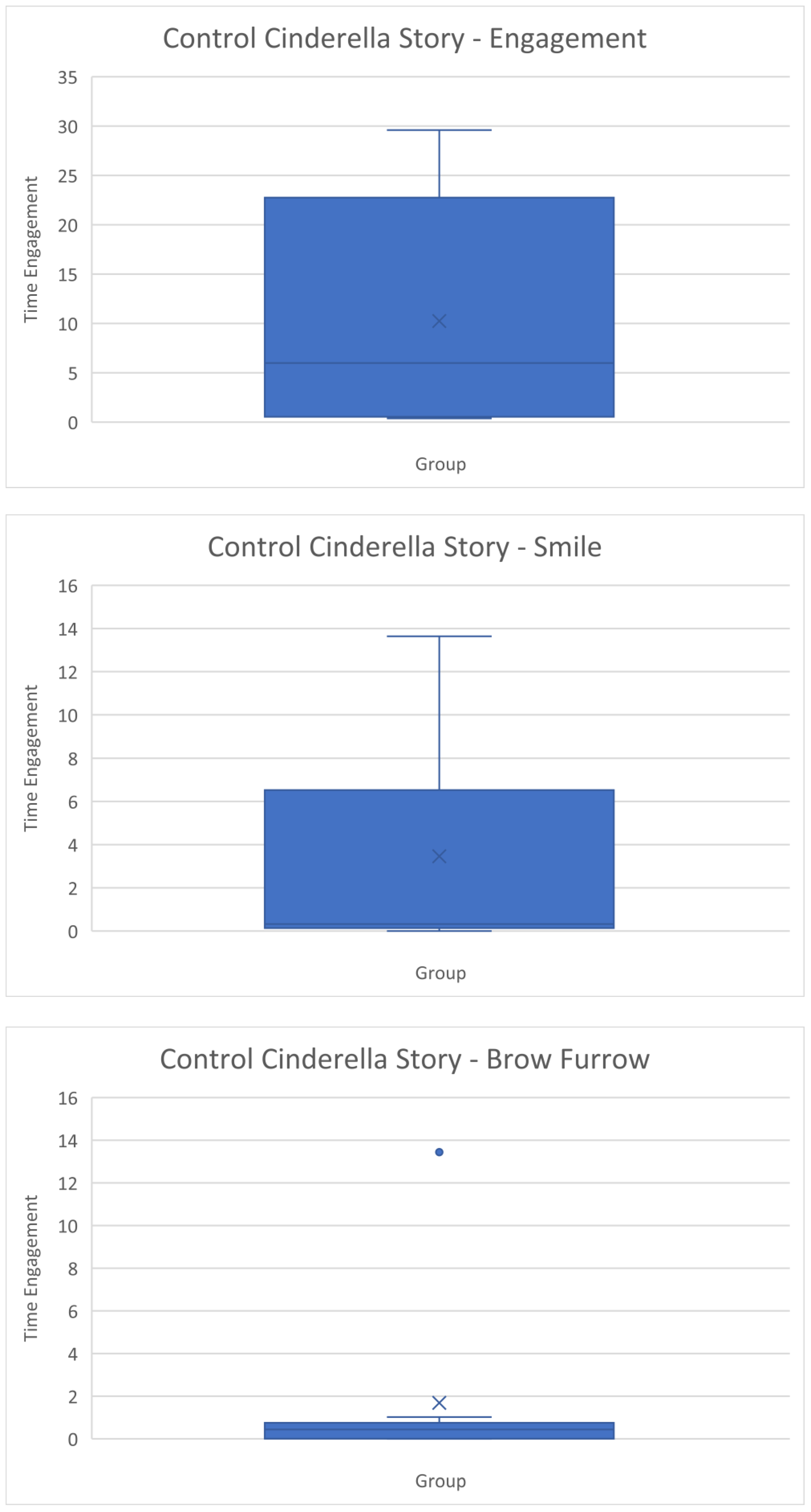
When examining the results for the personal event narrative, there was a significant difference (p = 0.011, U = 82.50) in engagement between TBI participants and controls but not for smile or frown. Higher engagement was detected for participants with TBI (median = 47.53) compared with control participants (median = 1.96).
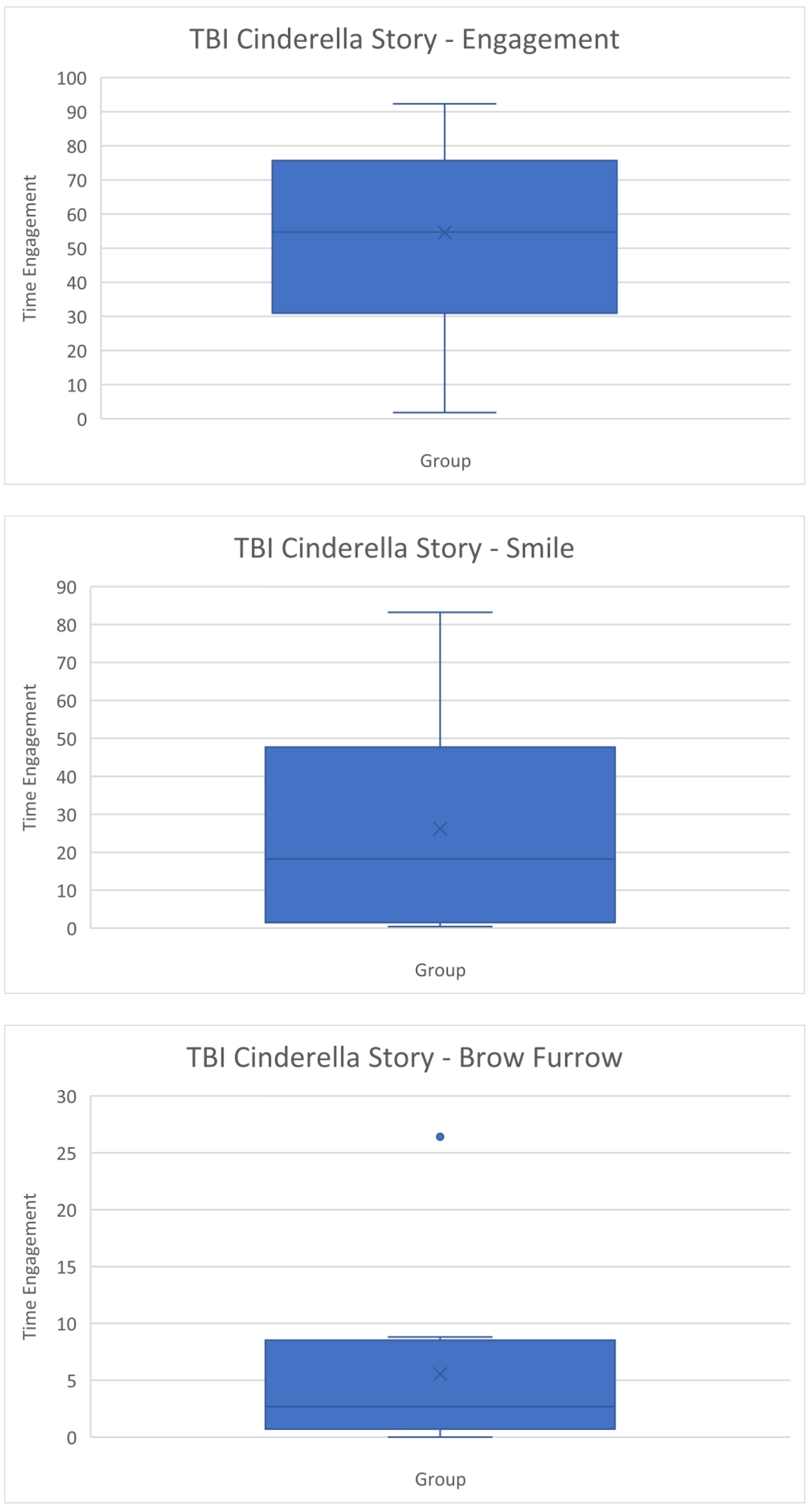
For the story narrative retell task, there was a significant difference (p ≤ 0.001, U = 93.00) was observed in engagement between TBI and control participants, with higher engagement for TBI participants (median = 54.73) than for control participants (median = 5.98). There was also a significant difference in smile (p = 0.0015, U = 82.00) between the groups, with a higher median time percentage detected for TBI participants (18.23) compared to control participants (0.32). No significant difference between groups was observed in brow furrow.
To address research question 2, statistical comparisons were conducted to compare data within TBI and control participants for the personal event narrative and story narrative retell. Table 8 and Table 9 display the median of differences between the facial measures in the TBI and control participants, respectively. There were no significant statistical differences observed between the facial measures within the TBI group and control group on the two different discourse genres.

Table 8.
Comparison between narrative tasks for the TBI group.

Table 9.
Comparison between narrative tasks for the control group.
3.2. Qualitative Observations
Qualitative observation data is presented in Appendix A. For engagement and smile, the ratings ranged between 1 and 4 for the participants with TBI. The control participants had the same range of scores for engagement and smile. For brow furrow, ratings ranged from 1 to 3 for the participants with TBI, and the control participants had the same range of scores. Both TBI and control groups were judged as presenting with socially appropriate use of facial expression, with only one participant with TBI presenting with less appropriate use of facial expression during the narrative tasks. This participant was observed to have a fixed facial expression throughout the narrative tasks, and a raised brow when speaking.
3.3. Case Studies
To address research question 3, samples with extreme data points from the Affectiva analysis (i.e., zero values for all measures, or with data identified as outliers using a box and whisker plot) or unusual values (i.e., participants with highly contrasting data for the two tasks) were identified. Seven out of the 40 samples had extreme data points, and one participant with TBI had highly contrasting data between the tasks. These identified samples were then further explored by comparing data from Affectiva and qualitative observations. We also consulted specialists from iMotions to review the data generated from Affectiva to examine plausible factors resulting in the outliers. To illustrate these findings and our interpretations, case studies are presented below where zero values, outlier data, and divergent data were observed for individual participants.
3.3.1. Case Study 1—Zero Values
The data as generated by Affectiva showed that TBI4 and C8 during the personal event narrative task recorded 0 for all measures. Review of these samples showed that the participants were not directly front-facing the camera. It seemed that they were facing the interviewer during the task instead. This could have impacted Affectiva’s ability to accurately analyze the video samples. Given these participants did have facial expressions detected in the story narrative retell, the video samples for these two participants were compared. We found that in the story narrative retell video sample of C8, their whole face could be seen. However, only half of their face was captured in the personal event narrative task. This could potentially contribute to the outlier data during the personal event narrative task as Affectiva might not be able to accurately analyze the participant’s face when they are side-facing the camera. On review of the two samples for TBI4, there were no observable differences in the participant’s positioning. However, a possible confounding factor present in both samples was the participant’s glasses. It appeared that in the story narrative retell task, TBI4’s eyes were blocked by the frame of their glasses, whereas their eyes were not blocked by glasses in the personal event narrative task
3.3.2. Case Study 2—Outlier Data
Results identified as outliers are represented by dots on the box and whisker plots (refer to Appendix B). Samples with data identified as outliers were C2, C3, C10 from the personal event narrative task, and TBI2 and C2 from the story narrative retell task. These video samples were reviewed again using iMotions to identify any factors impacting detection of participants’ facial landmarks. There was evidence that the use of accessories interfered with Affectiva’s facial detection. In C3’s video sample during the personal event narrative task, Affectiva was detecting the participant’s hat in some instances. The participant was also slightly side-facing the camera, thus occasionally causing the facial detection to get lost momentarily. Another possible factor that could have contributed to the outliers was the distance between the camera and the participants. Upon review of the video samples, we concluded that some outliers could be explained by the facial features of the participants. For example, there was one participant with a much higher brow furrow time percentage than others, as he had an observable furrow on his forehead as part of his usual expression.
3.3.3. Case Study 3—Divergent Data between Narrative Tasks
TBI10 had divergent data between the personal event narrative task and story narrative retell task for engagement, with the second lowest engagement data in personal event narrative (4.03) but the second highest engagement data in the story narrative retell (85.53). Upon reviewing the video samples of TBI10 across both narrative tasks, a potential reason that could have impacted our data is the change in use of glasses. In the personal event narrative task, TBI10 did not wear glasses, but in the story narrative retell task TBI10 wore glasses. Similar to case study 1, this suggests that the use of glasses could have influenced Affectiva analysis, thus generating a difference in engagement value.
4. Discussion
Use of facial expression is an important aspect of everyday communication that may be affected following severe TBI, leading to impaired social communication outcomes [8]. Facial expression has not previously been measured in a quantified and reliable manner, with a reliance on subjective impressions or ratings on pragmatic communication protocols such as the Profile of Pragmatic Impairment in Communication [22]. This is the first research conducted to investigate the use of Affectiva as a potential objective measure of facial expression in speakers with TBI compared to those without TBI. For research question 1, the Affectiva data showed some differences between the use of facial expression between the TBI and control groups. There were significant differences in engagement scores on Affectiva between TBI and control participants across both narrative tasks. This preliminary data suggests that the global measure of engagement (which is a composite measure across multiple expressions) may have more potential to demonstrate differences between TBI and control group as compared to specific action units of smile and brow furrow. A significant difference between groups in the smile time percentage was detected during the story narrative retell, but not in the personal event narrative. It is possible that the story narratives had a more consistent emotional tone across participants, compared to the personal narratives, which may have been either a positive or negative topic. The higher degree of structure in the story narrative task may make this task more suitable for future group studies investigating the use of facial expression during communication. There were no significant differences in the use of brow furrow detected between groups in this pilot study.
This study also investigated whether any differences were detected in the use of facial expression between the two different narrative tasks, to understand if speakers differentiated their use of facial expression between these two genres. From our investigation, there were no differences in the use of facial expression between a personal event narrative task and a story narrative retell task. This finding provides preliminary evidence that speakers with and without a TBI use similar frequency and types of facial expression when completing different narrative tasks, regardless of the topic. However, this finding should be interpreted with caution due to the small sample size in this pilot study. Further research involving comparison of topics across a larger number of participants would be needed to validate this result.
A pattern observed across both narrative tasks was that TBI participants had higher engagement, smile and brow furrow than the control participants, as evaluated by the Affectiva analysis. This result was surprising as it contrasted with previous research indicating that individuals with TBI had difficulties using facial expression to express themselves [8,19]. A possible reason for this discrepancy is that participants with TBI could have increased their use of facial expression to compensate for other factors that could be impacting their communication, for example, verbal output and memory abilities. Another factor could be the duration of the video samples. TBI participants had a shorter video sample than control participants across both narrative tasks. Momentary peaks in the use of facial expression in shorter samples would have a larger impact on the results, compared to a longer video sample. Future research in the use of facial expression during communication could ensure consistency of speaking duration across samples to address this issue.
Given the unexpected findings, it was important to review the samples to identify any confounding factors which influenced the data. This study used video samples from a databank, rather than samples collected for the specific purpose of evaluating facial expression. This provided an opportunity to observe factors in the recordings which influenced the data, so that these factors can be avoided when collecting samples for future research. From our qualitative observations, one confounding factor was that some participants were not directly front-facing the camera. As the whole face could not be detected, this may have affected Affectiva’s sensitivity when analyzing facial movements. This observation is consistent with the iMotions guidebook [23], in which it is stated that the camera should be placed approximately at the participant’s eye level and facing the participant directly. Another confounding factor which appeared to influence the data was the participant’s use of accessories such as glasses and hats. These could interfere with Affectiva’s detection of the participant’s face. Again, this is consistent with the iMotions guidebook [23], which notes that glasses covering the eyebrows and hats could occlude facial landmarks, which may lead to partial results. Beyond these expected observations, some instances of outlier data appeared to relate to Affectiva accurately detecting features of an individual’s facial structure. We observed that there were participants with a more furrowed brow even at rest, which was detected as a higher brow furrow time percentage. These individual differences in facial structures appeared to impact the results generated by Affectiva. Future research may need to include a baseline task to control for individual differences. A final consideration is the impact of the facial movements used for speaking on the Affectiva analysis. It did not appear that the speech movements were detected as expressions based on review of the video samples. However, speaking has been previously identified as an issue that can influence Affectiva analysis [23].
Aside from the factors affecting quality of the video samples, it should be noted that the automated facial coding system in Affectiva analyzes the facial expression without consideration of the context of the discourse. Affectiva is unable to identify the appropriateness of use of facial expression, such as a mismatch of facial expression to the context and content of what was said. As such, our qualitative observations took into account the context and content of what participants said before making judgments on whether their use of facial expression was socially appropriate overall. For example, a participant could score a low level of engagement, smile, and brow furrow from the Affectiva data. However, the participant’s use of facial expression could still be socially appropriate given that the context being talked about did not involve any strong emotions, thus their facial expression appropriately matched the discourse. Although it has been suggested that people with TBI have difficulty with use of facial expression [6,17,18], only one of the ten participants with TBI in this study was judged as using facial expression inappropriately on qualitative observation of the narrative samples. This suggests that further research is needed to understand the prevalence of difficulties with using facial expression after TBI.
4.1. Limitations
This exploratory investigation used a small sample size of 10 participants in each group, with the majority of participants being male. Future research with a larger sample size could provide greater insights and strengthen results. It would also be valuable for future research to aim for a gender balance in the participant sample, given that gender may influence use of facial expression during communication. Additionally, secondary data were used in this study. Therefore, the video samples were not optimally set up for Affectiva analysis. Although inclusion criteria were used to ensure that the selected samples could be successfully processed, there were factors identified in the samples which may have influenced the analysis. For example, some participants were side-facing the camera, and wore glasses and hats which interfered with the facial detection software that could have generated inaccurate results. Therefore, due to the small sample size and the factors affecting the video quality, a definite conclusion cannot be drawn. Lastly, even though the participants were well-matched on their demographic characteristics, the participants’ cultural backgrounds were different, with the TBI participants from Australia and the control participants were all monolingual and from the United States. Both groups completed the narrative tasks in English, but the differences in culture could have affected the data nonetheless.
4.2. Clinical Implications and Directions for Future Research
Although differences in the facial expression data were detected between groups, further research will be needed to understand the use of facial expression in communication situations after brain injury, and clinical implications for assessment and treatment. A clear recommendation for future research investigating facial expression is to standardize the recording set-up to optimize video samples for Affectiva analysis. It is recommended that participants are all fully front-facing the camera and not wearing any accessories that could interfere with Affectiva facial detection and analysis. It has been found that telehealth as a service delivery option has sizeable potential benefits for individuals with TBI [40], and so it may be feasible to engage participants in data collection for future studies via telehealth, following a protocol to ensure that participants are in an optimal recording environment, for example, front-facing positions, with appropriate lighting and distance to the camera. With these practices in place, Affectiva could potentially serve as an objective clinical and research tool for assessments and therapy interventions focusing on social communication. Larger studies with greater numbers of participants using standardized elicitation measures and formatting as outlined here would enable further understanding of the degree and nature of potential facial expression deficits in TBI, as currently this is not known.
With the advancement of technology, the use of automated software in other areas of speech pathology has become increasingly prevalent. For instance, there is now automated software for speech and voice analysis such as Praat [41] and Visi-Pitch [42], where traditionally analysis was dependent on the clinician’s subjective judgment during assessments and treatments. Similarly, we envision Affectiva could be used as an objective guide to support clinicians’ decision-making process in planning therapy intervention and improving outcomes. Affectiva could also be a source of data for clinicians and researchers in relation to social cognition, specifically to evaluate a person’s ability to use facial expression appropriately to interact and to respond to other people. TalkBank, which includes different corpora such as TBI Bank, Aphasia Bank, Dementia Bank, and RHD Bank, currently has automated software programs such as spoken dictation systems and automated analysis tools for language and speech available [43]. Affectiva could similarly be applied to the analysis of TalkBank data to provide a fine understanding in the use of facial expression of people with different communication disorders. It is noteworthy that the speech movements during the narrative tasks did not appear to be a confounding factor, which opens up the potential for continued use of Affectiva in research related to communication.
The use of technology as a clinical tool also has the potential to increase efficiency of clinicians [44] by reducing time taken for assessment analysis. Affectiva on iMotions is easy to set up, requires minimal technical skill, and provides immediate feedback on the use of facial expression [23]. This reduces time required for clinicians to conduct the assessment and analyze the results, as real-time data is provided by Affectiva. Lastly, Affectiva is a non-invasive tool that people with TBI could use independently as it provides direct and understandable feedback to people with TBI. Affectiva provides standardized quantifying data in the form of numeric scores for facial expression [23]. This could be used to measure change during the therapy and recovery period, and track progress. It could also function as a sensitive measure to determine treatment effectiveness.
Furthermore, future studies could evaluate different facial expressions during communication, and integrate different data using the iMotions software to gain a clearer picture of the cognitive impairments people have after TBI. The iMotions software has the capability of combining facial coding with other biosensors such as eye tracking [25], to quantify people’s attentional processes and behaviors, or electrodermal activity, to quantify emotional arousal [45]. Given there are strong correlations between attentional and emotional regulation impairments after TBI and social communication difficulties [46,47], integration of facial analysis, eye tracking and electrodermal activity could provide a more comprehensive objective assessment to guide and manage future therapy interventions.
5. Conclusions
This was the first study conducted to investigate the use of facial expression during a communication task by individuals with TBI using Affectiva. Affectiva detected differences between participants with TBI and control participants, with higher engagement on both tasks and greater smiling on one task found for participants with TBI. A key strength of the study design was that the TBI and control participants were well-matched according to demographics. However, there were other factors such as the positioning of the participants and the wearing of accessories that impacted on the automated facial expression analysis, and therefore influenced our findings. A key contribution of this study has been developing recommendations about future data collection to ensure high quality samples for analysis using Affectiva or similar technology. Future research could replicate this study with a standardized recording protocol using a larger and more diverse sample to investigate whether Affectiva can provide an objective and efficient clinical tool for assessment and intervention.
Author Contributions
Conceptualization, K.Y., L.T., E.P., M.B. and R.R.; methodology, K.Y., L.T., E.P., M.B. and R.R.; formal analysis, K.Y. and R.R.; investigation, K.Y.; writing—original draft preparation, K.Y.; writing—review and editing, K.Y., L.T., E.P., M.B. and R.R.; supervision, L.T., E.P., M.B. and R.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding. Author R.R. was supported by funding through icare NSW.
Institutional Review Board Statement
Original data in TalkBank was obtained within ethical protocols.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the individual pictured in Figure 2 (who is not a research subject) to publish this paper.
Data Availability Statement
Data is available on request from the author. The data are not publicly available for privacy reasons, as the dataset includes videos of participants.
Acknowledgments
We would like to thank the contributors to TBI Bank and Aphasia Bank, the participants, as well as the advisors from iMotions for their assistance in helping us interpret data from Affectiva.
Conflicts of Interest
The authors report no conflict of interest. The authors alone are responsible for the writing and content of this paper. The authors report no financial support received in conjunction with the generation of this submission. Author R.R. was supported by funding through icare NSW. The company had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Appendix A. Qualitative Observation Form

| TBI Participant/Control | Rating | Describing the Context | Impression | Is the Use of Facial Expression Socially Appropriate? | ||
|---|---|---|---|---|---|---|
| Engagement (Rating 1–5) | Smile (Rating 1–5) | Brow Furrow (Rating 1–5) | ||||
| TBI Participant Brain Injury Story | ||||||
| TBI1 | 1 | 1 | 1 | Brain injury story—cannot remember the incident, but remember events 3 weeks afterwards, remember the treatment, but cannot remember details |
| Appropriate. |
| TBI2 | 1 | 1 | 1 | Brain injury story—talked about how he remembered being aggressive after coming out of coma, snapping at things, how he coped with it, and how it improved over time |
| Appropriate facial expression in the context of story recount. Facial expression matched tone of voice, flat. |
| TBI3 | 3 | 3 | 1 | Brain injury story—talked about what he remembered and his body functions |
| Appropriate facial expression. |
| TBI4 | 2 | 1 | 1 | Brain injury story—talked about how his injury happened
|
| Appropriate facial expression according to context. |
| TBI5 | 2 | 1 | 1 | Brain injury story—talked about what people told him
|
| Appropriate in terms on facial expression, but inappropriate in terms of conversation (impoverished) |
| TBI6 | 1 | 2 | 1 | Brain injury story—unsure topic content
|
| Appropriate facial expression. Inappropriate. The participant’s conversation lacked content, was confused. |
| TBI7 | 2 | 2 | 1 | Brain injury story—talked about what he remembered → cannot remember about the accident day, cannot remember that he went to the doctor or CT scan, but remembered events at the rehabilitation centre
|
| Appropriate in this context—conversation topic did not involve strong emotions Monotonous voice, flat voice throughout |
| TBI8 | 4 | 3 | 1 | Brain injury story—talked about his hospital experience/memories → peed in bed, on crutches, having lunch, talking to nurses and doctors
|
| Appropriate. |
| TBI9 | 4 | 3 | 1 | Brain injury story—talked about her accident → could not eat, could not remember her husband, parents, only remembered her son
|
| Appropriate in terms on facial expression, but inappropriate in terms of conversation (impoverished) |
| TBI10 | 2 | 1 | 1 | Brain injury story—talked about his accident → reported the accident to the police, waiting for police report
|
| Inappropriate. The participant maintained a fixed facial expression throughout the 1 min conversation. |
| Control Injury/Illness Story | ||||||
| C1 | 4 | 2 | 3 | Injury story—talked about his hip replacement
|
| Appropriate. |
| C2 | 2 | 1 | 1 | Injury story—described how he sprained his ankle
|
| Appropriate. |
| C3 | 3 | 2 | 1 | Injury story—described how they found out about his meningitis and events at the hospital and how he had no TV for 4 days Situation: retell |
| Appropriate. |
| C4 | 1 | 2 | 1 | Injury story—tackled by a jock, broken wrist Situation: retell, no strong emotion involved |
| Appropriate. |
| C5 | 3 | 2 | 3 | Injury story—went to freshman camp, bitten by fleas/bed bugs all over, broke out into rashes/hives Situation: retell |
| Appropriate. |
| C6 | 2 | 1 | 1 | Injury story—“cracked” his shoulders during a football drill (dislocation) |
| Appropriate. |
| C7 | 3 | 4 | 2 | Injury story—talked about his meningitis |
| Appropriate. |
| C8 | 1 | 1 | 1 | Injury story—talked about how she got diagnosed with type 1 diabetes |
| Appropriate. |
| C9 | 3 | 3 | 1 | Injury story—talked about his accident, hospitalised and how he got stitched up without anaesthesia Situation: retell, no strong emotions involved |
| Appropriate. |
| C10 | 2 | 1 | 1 | Injury story—talked about hurting his back, went for physical therapy |
| Appropriate. |
| TBI Participant Cinderella Story | ||||||
| TBI1 | 2 | 2 | 1 | Cinderella story |
| Appropriate. |
| TBI2 | 1 | 1 | 1 | Cinderella story |
| Appropriate. |
| TBI3 | 3 | 4 | 1 | Cinderella story |
| Appropriate. |
| TBI4 | 1 | 1 | 1 | Cinderella story |
| Appropriate in terms on facial expression, but inappropriate in terms of narrative retell. |
| TBI5 | 2 | 2 | 1 | Cinderella story |
| Appropriate. |
| TBI6 | 2 | 2 | 3 | Cinderella story |
| Appropriate in terms on facial expression, but inappropriate in terms of narrative retell. |
| TBI7 | 1 | 1 | 1 | Cinderella story |
| Appropriate in terms on facial expression, but inappropriate in terms of narrative retell. |
| TBI8 | 3 | 1 | 1 | Cinderella story |
| Appropriate. |
| TBI9 | 2 | 2 | 1 | Cinderella story |
| Appropriate in terms on facial expression, but inappropriate in terms of conversation (impoverished). |
| TBI10 | 1 | 2 | 1 | Cinderella story |
| Inappropriate. The participant maintained a fixed facial expression throughout the narrative retell (except when he turned away on one occasion, and on another occasion, smiled when he finished). |
| Control Cinderella Story | ||||||
| C1 | 2 | 2 | 1 | Cinderella story |
| Appropriate. |
| C2 | 1 | 2 | 2 | Cinderella story |
| Appropriate. |
| C3 | 1 | 1 | 1 | Cinderella story |
| Appropriate. |
| C4 | 1 | 2 | 1 | Cinderella story |
| Appropriate. |
| C5 | 1 | 1 | 1 | Cinderella story |
| Appropriate. |
| C6 | 1 | 2 | 1 | Cinderella story |
| Appropriate. |
| C7 | 2 | 2 | 1 | Cinderella story |
| Appropriate. |
| C8 | 2 | 2 | 1 | Cinderella story |
| Appropriate. |
| C9 | 2 | 3 | 1 | Cinderella story |
| Appropriate. |
| C10 | 2 | 2 | 1 | Cinderella story |
| Appropriate. |
Appendix B. Box and Whisker Plots
References
- Johnson, J.E.; Turkstra, L.S. Inference in conversation of adults with traumatic brain injury. Brain Inj. 2012, 26, 1118–1126. [Google Scholar] [CrossRef] [PubMed]
- Sarno, M.T. The Nature of Verbal Impairment after Closed Head Injury. J. Nerv. Ment. Dis. 1980, 168, 685–692. [Google Scholar] [CrossRef] [PubMed]
- Ruusuvuori, J.; Peräkylä, A. Facial and verbal expressions in assessing stories and topics. Res. Lang. Soc. Interact. Assess. Soc. Interact. 2009, 42, 377–394. [Google Scholar] [CrossRef]
- Croker, V.; McDonald, S. Recognition of emotion from facial expression following traumatic brain injury. Brain Inj. 2005, 19, 787–799. [Google Scholar] [CrossRef] [PubMed]
- Zupan, B.; Neumann, D.; Babbage, D.; Willer, B. Exploration of a new tool for assessing emotional inferencing after traumatic brain injury. Brain Inj. 2015, 29, 877–887. [Google Scholar] [CrossRef] [PubMed]
- Karow, C.M.; Connors, E.C. Affective Communication in Normal and Brain-Damaged Adults: An Overview. Semin. Speech Lang. 2003, 24, 69–92. [Google Scholar] [CrossRef]
- Struchen, M.A.; Pappadis, M.R.; Sander, A.M.; Burrows, C.S.; Myszka, K.A. Examining the Contribution of Social Communication Abilities and Affective/Behavioral Functioning to Social Integration Outcomes for Adults With Traumatic Brain Injury. J. Head Trauma Rehabil. 2011, 26, 30–42. [Google Scholar] [CrossRef]
- Wauters, L.; Marquardt, T.P. Disorders of Emotional Communication in Traumatic Brain Injury. Semin. Speech Lang. 2019, 40, 13–26. [Google Scholar] [CrossRef]
- Bond, F.; Godfrey, H.P.D. Conversation with traumatically brain-injured individuals: A controlled study of behavioural changes and their impact. Brain Inj. 1997, 11, 319–330. [Google Scholar] [CrossRef]
- Rigon, A.; Turkstra, L.S.; Mutlu, B.; Duff, M.C. Facial-affect recognition deficit as a predictor of different aspects of social-communication impairment in traumatic brain injury. Neuropsychology 2018, 32, 476–483. [Google Scholar] [CrossRef]
- Shorland, J.; Douglas, J.M. Understanding the role of communication in maintaining and forming friendships following traumatic brain injury. Brain Inj. 2010, 24, 569–580. [Google Scholar] [CrossRef] [PubMed]
- Morton, M.V.; Wehman, P. Psychosocial and emotional sequelae of individuals with traumatic brain injury: A literature review and recommendations. Brain Injury. J. Head Trauma Rehabil. 1996, 11, 104. [Google Scholar] [CrossRef]
- Rauch, R.J.; Ferry, S.M. Social networks as support interventions following traumatic brain injury. NeuroRehabilitation 2001, 16, 11–16. [Google Scholar] [CrossRef]
- Paterson, J.; Stewart, J. Adults with Acquired Brain Injury: Perceptions of Their Social World. Rehabil. Nurs. 2002, 27, 13–18. [Google Scholar] [CrossRef]
- Temkin, N.R.; Corrigan, J.D.; Dikmen, S.S.; Machamer, J. Social Functioning After Traumatic Brain Injury. J. Head Trauma Rehabil. 2009, 24, 460–467. [Google Scholar] [CrossRef] [PubMed]
- Finch, E.; French, A.; Ou, R.J.; Fleming, J. Participation in communication activities following traumatic brain injury: A time use diary study. Brain Inj. 2016, 30, 883–890. [Google Scholar] [CrossRef] [PubMed]
- Arnould, A.; Rochat, L.; Azouvi, P.; Van Der Linden, M. Apathetic symptom presentations in patients with severe traumatic brain injury: Assessment, heterogeneity and relationships with psychosocial functioning and caregivers’ burden. Brain Inj. 2015, 29, 1597–1603. [Google Scholar] [CrossRef]
- Roy, D.; McCann, U.; Han, D.; Rao, V. Pathological Laughter and Crying and Psychiatric Comorbidity After Traumatic Brain Injury. J. Neuropsychiatry Clin. Neurosci. 2015, 27, 299–303. [Google Scholar] [CrossRef]
- Marquardt, T.P.; Rios-Brown, M.; Richburg, T.; Seibert, L.K.; Cannito, M.P. Comprehension and expression of affective sentences in traumatic brain injury. Aphasiology 2001, 15, 1091–1101. [Google Scholar] [CrossRef]
- McDonald, S.; Bornhofen, C.; Shum, D.H.K.; Long, E.; Saunders, C.; Neulinger, K. Reliability and validity of The Awareness of Social Inference Test (TASIT): A clinical test of social perception. Disabil. Rehabil. 2006, 28, 1529–1542. [Google Scholar] [CrossRef]
- Prutting, C.A.; Kirchner, D.M. A clinical appraisal of the pragmatic aspects of language. J. Speech Hear. Disord. 1987, 52, 105–119. [Google Scholar] [CrossRef] [PubMed]
- Linscott, R.; Knight, R.G.; Godfrey, H.P.D. The Profile of Functional Impairment in Communication (PFIC): A measure of communication impairment for clinical use. Brain Inj. 1996, 10, 397–412. [Google Scholar] [CrossRef] [PubMed]
- iMotions. Facial Expression Analysis: The Complete Pocket Guide; iMotions: Copenhagen, Denmark, 2017. [Google Scholar]
- iMotions. iMotions Core: The World’s Leading Biosensor Platform; iMotions: Copenhagen, Denmark, 2019. [Google Scholar]
- iMotions. Facial Expression Analysis. Available online: https://imotions.com/biosensor/fea-facial-expression-analysis/ (accessed on 25 October 2021).
- Kulke, L.; Feyerabend, D.; Schacht, A. A Comparison of the Affectiva iMotions Facial Expression Analysis Software With EMG for Identifying Facial Expressions of Emotion. Front. Psychol. 2020, 11, 329. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Garcia, J.M.; Penichet, V.M.R.; Lozano, M.D.; Fernando, A. Using emotion recognition technologies to teach children with autism spectrum disorder how to identify and express emotions. Univers. Access Inf. Soc. 2021, 21, 809–825. [Google Scholar] [CrossRef]
- Ho, M.W.-R.; Chien, S.H.-L.; Lu, M.-K.; Chen, J.-C.; Aoh, Y.; Chen, C.-M.; Lane, H.-Y.; Tsai, C.-H. Impairments in face discrimination and emotion recognition are related to aging and cognitive dysfunctions in Parkinson’s disease with dementia. Sci. Rep. 2020, 10, 4367. [Google Scholar] [CrossRef] [PubMed]
- TalkBank. The TalkBank System. Available online: https://www.talkbank.org/ (accessed on 20 August 2022).
- Elbourn, E.; Kenny, B.; Power, E.; Togher, L. Psychosocial Outcomes of Severe Traumatic Brain Injury in Relation to Discourse Recovery: A Longitudinal Study up to 1 Year Post-Injury. Am. J. Speech-Lang. Pathol. 2019, 28, 1463–1478. [Google Scholar] [CrossRef]
- MacWhinney, B.; Fromm, D.; Forbes, M.; Holland, A. AphasiaBank: Methods for studying discourse. Aphasiology 2011, 25, 1286–1307. [Google Scholar] [CrossRef]
- Teasdale, G.M. Head injury. J. Neurol. Neurosurg. Psychiatry 1995, 58, 526–539. [Google Scholar] [CrossRef]
- Russell, W.; Smith, A. A post-traumatic amnesia in head injury. Arch. Neurol. 1961, 5, 16–29. [Google Scholar] [CrossRef]
- Ponsford, J.; Sloan, S.; Snow, P. Traumatic Brain Injury: Rehabilitation for Everyday Adaptive Living, 2nd ed.; Sloan, S., Snow, P., Eds.; Psychology Press: Hove, UK, 2013. [Google Scholar]
- Power, E.; Weir, S.; Richardson, J.; Fromm, D.; Forbes, M.; MacWhinney, B.; Togher, L. Patterns of narrative discourse in early recovery following severe Traumatic Brain Injury. Brain Inj. 2019, 34, 98–109. [Google Scholar] [CrossRef]
- Stark, B.C. A Comparison of Three Discourse Elicitation Methods in Aphasia and Age-Matched Adults: Implications for Language Assessment and Outcome. Am. J. Speech-Lang. Pathol. 2019, 28, 1067–1083. [Google Scholar] [CrossRef] [PubMed]
- Affectiva. Emotion AI 101: All about Emotion Detection and Affectiva’s Emotion Metrics. Available online: https://blog.affectiva.com/emotion-ai-101-all-about-emotion-detection-and-affectivas-emotion-metrics (accessed on 25 October 2021).
- Perneger, T.V. What’s wrong with Bonferroni adjustments. BMJ 1998, 316, 1236–1238. [Google Scholar] [CrossRef] [PubMed]
- Streiner, D.L. Best (but oft-forgotten) practices: The multiple problems of multiplicity—Whether and how to correct for many statistical tests. Am. J. Clin. Nutr. 2015, 102, 721–728. [Google Scholar] [CrossRef] [PubMed]
- Turkstra, L.S.; Quinn-Padron, M.; Johnson, J.E.; Workinger, M.S.; Antoniotti, N. In-Person Versus Telehealth Assessment of Discourse Ability in Adults With Traumatic Brain Injury. J. Head Trauma Rehabil. 2012, 27, 424–432. [Google Scholar] [CrossRef]
- Maryn, Y. Practical Acoustics in Clinical Voice Assessment: A Praat Primer. Perspect. ASHA Spéc. Interes. Groups 2017, 2, 14–32. [Google Scholar] [CrossRef]
- Cohen, N.S. The Effect of Vocal Instruction and Visi-Pitch Feedback on the Speech of Persons with Neurogenic Communication Disorders: Two Case Studies. Music. Ther. Perspect. 1995, 13, 70–75. [Google Scholar] [CrossRef]
- TalkBank. TalkBank Software. Available online: https://talkbank.org/software/ (accessed on 3 November 2021).
- Kabir, M. Does artificial intelligence (AI) constitute an opportunity or a threat to the future of medicine as we know it? Future Healthc. J. 2019, 6, 190–191. [Google Scholar] [CrossRef]
- iMotions. EDA/GSR (Electrodermal Activity). Available online: https://imotions.com/products/imotions-lab/modules/eda-gsr-electrodermal-activity/ (accessed on 19 December 2022).
- VanSolkema, M.; McCann, C.; Barker-Collo, S.; Foster, A. Attention and Communication Following TBI: Making the Connection through a Meta-Narrative Systematic Review. Neuropsychol. Rev. 2020, 30, 345–361. [Google Scholar] [CrossRef]
- Neumann, D.; Westerhof-Evers, H.J.; Visser-Keizer, A.C.; Fasotti, L.; Schönherr, M.C.; Vink, M.; van der Naalt, J.; Spikman, J.M. Effectiveness of a treatment for impairments in social cognition and emotion regulation (T-ScEmo) after traumatic brain injury: A randomized controlled trial. J. Head Trauma Rehabil. 2017, 32, 296–307. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
