Verbal Autopsy as a Tool for Defining Causes of Death in Specific Healthcare Contexts: Study of Applicability through a Traditional Literature Review
Abstract
1. Introduction
2. The Verbal Autopsy: Birth and Evolution
3. Aims and Objectives
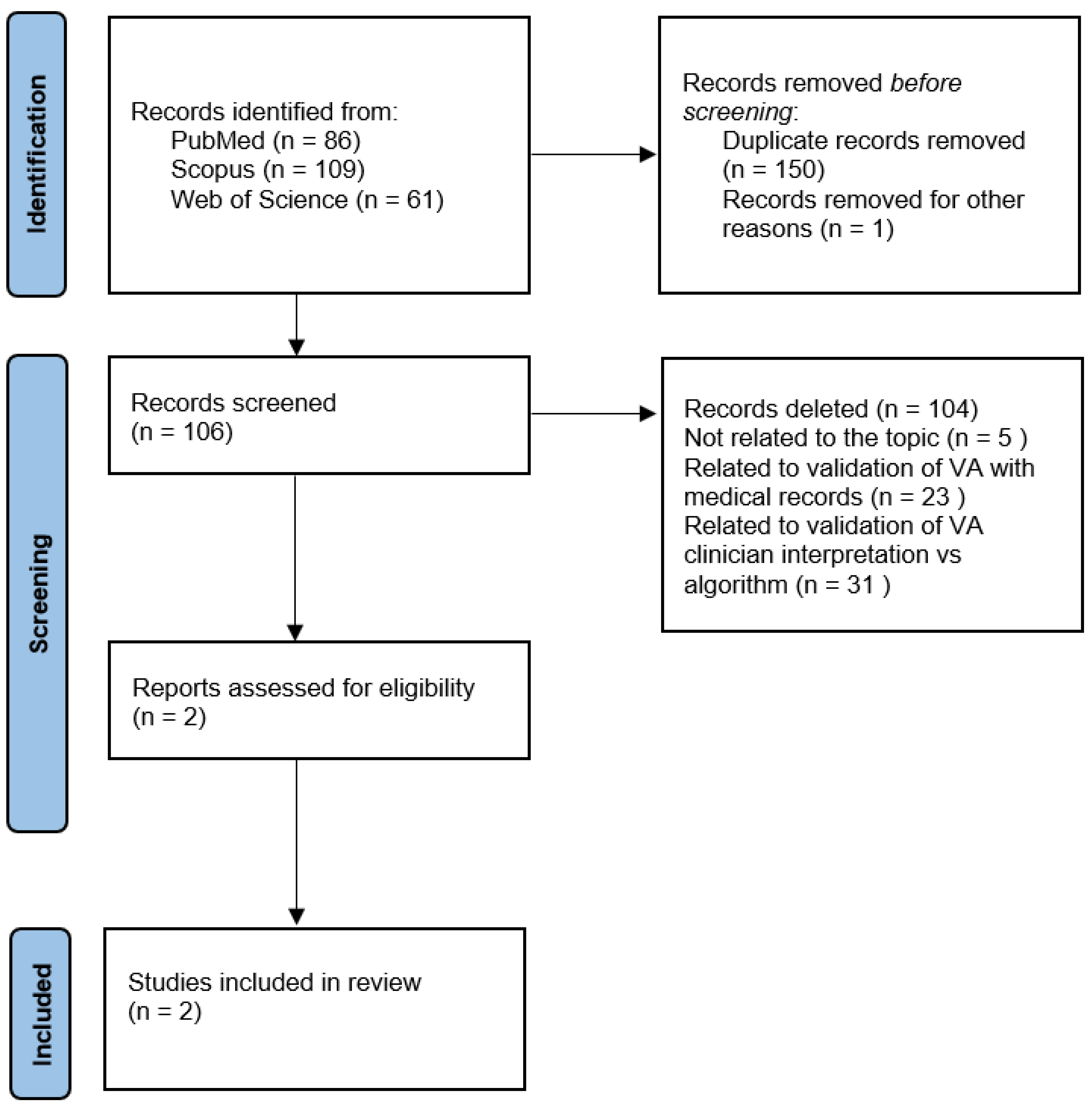
4. Searching Strategy
5. Selection Criteria
6. Quality Evaluation
7. Summary of Article Pool
8. Results
9. Discussion
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mikkelsen, L.; Phillips, D.E.; AbouZahr, C.; Setel, P.W.; de Savigny, D.; Lozano, R.; Lopez, D.L. A global assessment of civil registration and vital statistics systems: Monitoring data quality and progress. Lancet 2015, 386, 1395–1406. [Google Scholar] [CrossRef]
- Waters, B.L. Handbook of Autopsy Practice, 4th ed.; Springer-Verlag: New York, NY, USA, 2009; pp. 3–7. [Google Scholar]
- Madea, B.; Argo, A. Certification of death: External postmortem examination. In Handbook of Forensic Medicine; John Wiley & Sons: Hoboken, NJ, USA, 2014; pp. 57–74. [Google Scholar]
- Groß, D.; Wilhelmy, S. Klinische Obduktionen aus medizinethischer Sicht [Clinical autopsies from a medical ethics perspective]. Pathologe 2017, 38, 396–401. [Google Scholar] [CrossRef] [PubMed]
- Xiao, J.; Krueger, G.R.; Buja, L.M.; Covinsky, M. The impact of declining clinical autopsy: Need for revised healthcare policy. Am. J. Med. Sci. 2009, 337, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Italian Law. Mortuary Police Regulation. Available online: https://www.gazzettaufficiale.it/atto/serie_generale/caricaArticolo?art.versione=1&art.idGruppo=1&art.flagTipoArticolo=1&art.codiceRedazionale=090G0312&art.idArticolo=1&art.idSottoArticolo=1&art.idSottoArticolo1=10&art.dataPubblicazioneGazzetta=1990-10-12&art.progressivo=0 (accessed on 22 August 2022).
- Ministero della Salute; Direzione Generale della Prevenzione Sanitaria Ufficio 4. Indicazioni Emergenziali Connesse Ad Epidemia COVID-19 Riguardanti Il Settore Funebre, Cimiteriale E Di Cremazione. 2020. Available online: https://wwwtesto-unico-sicurezzacom/_media/cimiterialepdf (accessed on 22 August 2022).
- Calabrese, F.; Pezzuto, F.; Fortarezza, F.; Hofman, P.; Kern, I.; Panizo, A.; von der Thüsen, J.; Timofeev, S.; Gorkiewicz, G.; Lunardi, F. Pulmonary pathology and COVID-19: Lessons from autopsy. The experience of European Pulmonary Pathologists. Virchows Arch. 2020, 477, 359–372. [Google Scholar] [CrossRef]
- Odone, A.; Delmonte, D.; Gaetti, G.; Signorelli, C. Doubled mortality rate during the COVID-19 pandemic in Italy: Quantifying what is not captured by surveillance. Public Health 2021, 190, 108–115. [Google Scholar] [CrossRef]
- Melo, D.N.; Mara Coelho, T.; Rolim Pinheiro Lima, G.; Gomes Fernandes, C.; Cavalcante Fales de Brito Alves, B.; Montenegro de Carvalho Araújo, F.; Aparecida de Almeida Monteiro, R.; Ordi, J.; Hilário do Nascimento Saldiva, P.; Pamplona de Góes Cavalcanti, L. Use of minimally invasive autopsy during the COVID-19 pandemic and its possibilities in the context of developing countries. PLoS Negl. Trop. Dis. 2021, 15, e0009629. [Google Scholar] [CrossRef]
- Sankoh, O.; Byass, P. The INDEPTH network: Filling vital gaps in global epidemiology. Int. J. Epidemiol. 2012, 41, 579–588. [Google Scholar] [CrossRef]
- Caleo, G.M.; Sy, A.P.; Balandine, S.; Polonsky, J.; Palma, P.P.; Grais, R.F. The 2012 WHO verbal autopsy instrument. Lancet 2018, 12, 1–11. [Google Scholar]
- Leitao, J.; Desai, N.; Aleksandrowicz, L.; Byass, P.; Miasnikof, P.; Tollman, S.; Alam, D.; Lu, Y.; Rathi, S.K.; Singh, A.; et al. Comparison of physician-certified verbal autopsy with computer-coded verbal autopsy for cause of death assignment in hospitalized patients in low- and middle-income countries: Systematic review. BMC Med. 2014, 12, 22. [Google Scholar] [CrossRef]
- WHO Verbal Autopsy Reference Group. Revision of the 2016 WHO Verbal Autopsy Instrument. 2022. Available online: https://cdn.who.int/media/docs/default-source/classification/other-classifications/autopsy/2022-va-instrument/report---revision-of-the-2016-who-va-instrument_2022.pdf (accessed on 22 August 2022).
- De Souza, P.; Gerson, G.; Dias, J.S.; de Melo, D.N.; de Souza, S.G.; Ruiz, E.M.; Fernandes Tavora, F.R.; Cavalcanti, L. Validation of verbal autopsy and nasopharyngeal swab collection for the investigation of deaths at home during the COVID-19 pandemics in Brazil. PLoS Negl. Trop. Dis. 2020, 14, e0008830. [Google Scholar] [CrossRef]
- WHO. Méthode Pour L’Enregistrement Par Des Non-médecins Des Causes Élémentaires de Décès Dans Des Zones Sous-Développées; WHO: Geneva, Switzerland, 1956.
- WHO. Verbal Autopsy Standards: The 2016 WHO Verbal Autopsy Instrument; WHO: Geneva, Switzerland, 2016.
- Thomas, L.M.; D’Ambruoso, L.; Balabanova, D. Verbal autopsy in health policy and systems: A literature review. BMJ Glob. Health 2018, 3, e000639. [Google Scholar] [CrossRef] [PubMed]
- Ba, M.G.; Kodio, B.; Etard, J.F. Application de l’autopsie verbale dans la mesure de la mortalité maternelle en milieu rural au Sénégal [Verbal autopsy to measure maternal mortality in rural Senegal]. J. Gynecol. Obstet. Biol. Reprod. 2003, 32, 728–735. [Google Scholar]
- Duthé, G.; Faye, S.H.; Guyavarch, E.; Arduin, P.; Kanté, A.M.; Diallo, A.; Laurent, R.; Marra, A.; Pison, G. Changement de protocole dans la méthode d’autopsie verbale et mesure de la mortalité palustre en milieu rural sénégalais [Change of protocol in the verbal autopsy method and measure of malaria mortality in rural areas in Senegal]. Bull. Soc. Pathol. Exot. 2010, 103, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Etard, J.F.; Le Hesran, J.Y.; Diallo, A.; Diallo, J.P.; Ndiaye, J.L.; Delaunay, V. Childhood mortality and probable causes of death using verbal autopsy in Niakhar, Senegal, 1989–2000. Int. J. Epidemiol. 2004, 33, 1286–1292. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chandramohan, D.; Fottrell, E.; Leitao, J.; Nichols, E.; Clark, S.J.; Alsokhn, C.; de Savigny, D. Estimating causes of death where there is no medical certification: Evolution and state of the art of verbal autopsy. Glob. Health Action. 2021, 14, 1982486. [Google Scholar] [CrossRef] [PubMed]
- Baethge, C.; Goldbeck-Wood, S.; Mertens, S. SANRA—A scale for the quality assessment of narrative review articles. Res. Integr. Peer Rev. 2019, 4, 5. [Google Scholar] [CrossRef]
- Menéndez, C.; Quintó, L.; Castillo, P.; Carrilho, C.; Ismail, M.R.; Lorenzoni, C.; Fernandes, F.; Hurtado, J.C.; Rakislova, N.; Munguambe, K.; et al. Limitations to current methods to estimate cause of death: A validation study of a verbal autopsy model. Gates Open Res. 2021, 4, 55. [Google Scholar] [CrossRef]
- Hart, J.D.; de André, P.A.; de André, C.D.S.; Adair, T.; Barroso, L.P.; Valongueiro, S.; Saldiva, P.H.N. Validation of SmartVA using conventional autopsy: A study of adult deaths in Brazil. Lancet Reg. Health-Am. 2022, 5, 100081. [Google Scholar] [CrossRef]
- Costache, M.; Lazaroiu, A.M.; Contolenco, A.; Costache, D.; George, S.; Sajin, M.; Patrascu, O.M. Clinical or post-mortem? The importance of the autopsy; a retrospective study. Maedica 2014, 9, 261–265. [Google Scholar]
- Fottrell, E.; Byass, P. Verbal Autopsy: Methods in Transition. Epidemiol. Rev. 2010, 32, 38–55. [Google Scholar] [CrossRef]
- Crișan, R.M.; Băcilă, C.I.; Morar, S. The role of psychological autopsy in investigating a case of atypical suicide in schizophrenia: A case report with a brief review of literature. Egypt. J. Forensic Sci. 2022, 12, 30. [Google Scholar] [CrossRef] [PubMed]
- Mérelle, S.; Van Bergen, D.; Looijmans, M.; Balt, E.; Rasing, S.; van Domburgh, L.; Nauta, M.; Sijperda, O.; Mulder, W.; Gilissen, R.; et al. A multi-method psychological autopsy study on youth suicides in the Netherlands in 2017: Feasibility, main outcomes, and recommendations. PLoS ONE 2020, 15, e0238031. [Google Scholar] [CrossRef] [PubMed]
- Aquila, I.; Sacco, M.A.; Gratteri, S.; Sirianni, M.; De Fazio, P.; Ricci, P. The “Social-mobile autopsy”: The evolution of psychological autopsy with new technologies in forensic investigations on suicide. Leg. Med. 2018, 32, 79–82. [Google Scholar] [CrossRef] [PubMed]
| Reference and Year of Publication | Justification of the Article’s Importance for the Readership | Statement of Concrete Aims or Formulation of Questions | Description of the Literature Search | Referencing | Scientific Reasoning | Appropriate Presentation of Data | Total Score |
|---|---|---|---|---|---|---|---|
| Menéndez et al. [24] 2021 | 2 | 2 | 1 | 2 | 2 | 2 | 11 |
| Hart et al. [25] 2022 | 2 | 2 | 1 | 2 | 2 | 2 | 11 |
| Reference and Year of Publication | Socio-Environmental Context | Type of Article | Title | Number and Type of Cases | Overall Results |
|---|---|---|---|---|---|
| Menéndez et al. [24] 2021 | Mozambique | Research Article | Limitations to current methods to estimate cause of death: a validation study of a verbal autopsy model | 316 patients, from stillbirth to adults |
|
| Hart et al. [25] 2022 | Brazil | Research Article | Validation of physician certified verbal autopsy using conventional autopsy: a large study of adult non-external causes of death in a metropolitan area in Brazil | 3139 patients, above 18 years (smart VA and PCVA for the 2060 deaths in São Paulo and only smart VA for the 1079 deaths in Recife) |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bailo, P.; Gibelli, F.; Ricci, G.; Sirignano, A. Verbal Autopsy as a Tool for Defining Causes of Death in Specific Healthcare Contexts: Study of Applicability through a Traditional Literature Review. Int. J. Environ. Res. Public Health 2022, 19, 11749. https://doi.org/10.3390/ijerph191811749
Bailo P, Gibelli F, Ricci G, Sirignano A. Verbal Autopsy as a Tool for Defining Causes of Death in Specific Healthcare Contexts: Study of Applicability through a Traditional Literature Review. International Journal of Environmental Research and Public Health. 2022; 19(18):11749. https://doi.org/10.3390/ijerph191811749
Chicago/Turabian StyleBailo, Paolo, Filippo Gibelli, Giovanna Ricci, and Ascanio Sirignano. 2022. "Verbal Autopsy as a Tool for Defining Causes of Death in Specific Healthcare Contexts: Study of Applicability through a Traditional Literature Review" International Journal of Environmental Research and Public Health 19, no. 18: 11749. https://doi.org/10.3390/ijerph191811749
APA StyleBailo, P., Gibelli, F., Ricci, G., & Sirignano, A. (2022). Verbal Autopsy as a Tool for Defining Causes of Death in Specific Healthcare Contexts: Study of Applicability through a Traditional Literature Review. International Journal of Environmental Research and Public Health, 19(18), 11749. https://doi.org/10.3390/ijerph191811749








