Concerns of Home Isolating COVID-19 Patients While Receiving Care via Telemedicine during the Pandemic in the Northern Thailand: A Qualitative Study on Text Messaging
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting and Participants
2.2. Data Collection
2.3. Data Analysis
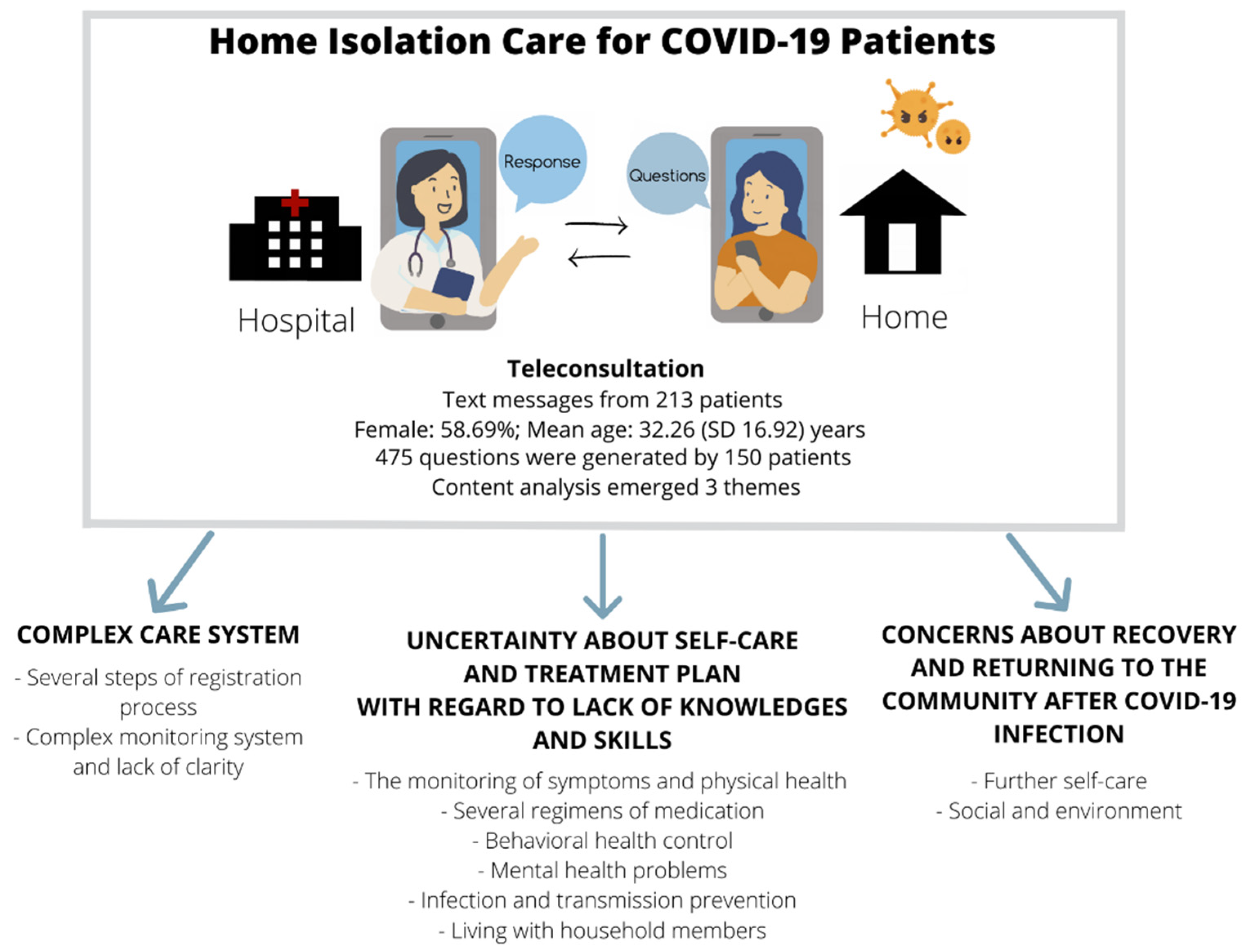
3. Results
3.1. Theme: Complex Care System
3.1.1. Several Steps of Registration Process
3.1.2. Complex Monitoring System and Lack of Clarity Re: Received Services
- -
- Reporting of vital signs: Problems with the system were reported. (n = 28)
“I could not access the system. The system was down. When should I access again?”
- -
- Way to communicate with health care providers: The route and available times were asked in order that the patients could contact the team if there were any problems. (n = 6)
“How do we communicate? Do we chat via this route?”
- -
- Other hospital appointments during the isolation: Those who had had contact with COVID-19 cases, were scheduled in advance for their RT-PCR test. Even if they had tested positive, the scheduled appointment was not canceled automatically, so they still received the reminder message. Some patients had health conditions that had scheduled appointments and received phone calls from other hospitals to confirm them. The question was around what they should do about these appointments. (n = 4)
“I receive a phone call from (hospital name). They asked me to pack my bag and go get the treatment at their place. What should I do?”
- -
- Medical kit box: As some patients received their medication and pulse oximeter, they expressed concern about how long they had to wait to report it. Moreover, the box was provided free of charge, so there was concern as to whether they should return the box and needed to know how. (n = 23)
“My box has not arrived yet; can I use my boyfriend’s pulse oximeter?”
- -
- Need for extra equipment: Some things were asked for during the isolation including new batteries for the pulse oximeter and alcohol spray. (n = 2)
- -
- Change of location to receive care: Some patients were not allowed to continue home isolation by the owner of the place they lived. (n = 8)
“I’m sorry that I cannot continue the home isolation. The owner of the dormitory is not okay with me staying here. It is better for me to stay at the hospital with my friend.”
- -
- Contact other hospital: A patient who’s grandmother was COVID-19 positive and receiving the treatment at another hospital asked for help. (n = 1)
“My grandmother is receiving the treatment at (hospital name). Do you have the contact for that place?
- -
- Documentation: Certificates were requested by most patients for insurance companies or employers. (n = 35)
“I am a teacher. I need the medical certificate for my school that I was absent because of COVID-19 infection.”
- -
- Meal services: Meals for patients in home isolation system were distributed by a specific driver under the hospital home isolation system, there were some questions about the meals during home isolation for example at what exact time the meal would come or when would the electronic meal coupon expire. (n = 3)
3.2. Theme: Uncertainty about Self-Care and Treatment Plan with Regard to Lack of Knowledge and Skills
3.2.1. The Monitoring of Symptoms and Physical Health in Order to Determine the Progression of COVID-19
- -
- Monitoring of vital signs: Questions about ‘How to monitor and how to record the data?’ And ‘How to read pulse oximeter?’ were asked. (n = 12)
“I recorded my vital signs in the system. Did I do it correctly?”
- -
- Symptom concerns: Covid related symptoms including rash, red eyes, high grade fever, cough, dyspnea, vomiting, anosmia/ageusia, dizziness and fatigue were reported. Management of general health issues about symptoms from other causes were also asked. (n = 36)
“My mom fell down after walking out from the bathroom and had a bump on her head. What should I do?”
- -
- Indicator of recovery: Many patients were concerned about how to indicate that they had recovered. Some expressed concern that the disease would get worse after it got better. (n = 8)
“If I had already recovered, can the disease still get worse? Or if it is better will I always be better.”
- -
- Disease progression: Lungs were the organs that caused the highest level of concern amongst patients. Patients asked how would they know if the virus had entered the lungs. Moreover, as the patients were asked to monitor their pulse rate and oxygen saturation, they were sometimes concerned about the numbers. With regard to interventions, chest X-ray was the intervention that the majority of patients believed could help detect the progression of the disease so some requested one. (n = 30)
“How can I know that the virus enters to my lungs? Are my lungs okay now?”
3.2.2. Several Regimens of Medication Resulting from the in-Advance Medical Box Set and Non-Prescribed Medicine
- -
- Prescribed medication: Even though a leaflet about how to take the medication was provided, the patients still asked for confirmation about what medication, how many, when, and how long should they take it for. In one case, the mother of a child asked about how to store the medication (favipiravir syrup). Most concerns about medication were about their side effect(s), what should be done if they forget, and can they take the anti-viral medication with other medication. Also during the isolation, more medication was requested, as there were some new or prolonged symptom(s). (n = 84)
“I have more cough and phlegm. Can I have more medication for my coughing?”
- -
- Non-prescribed medication, herbal medicine or supplements: The extract of Andrographis paniculate was the most common medicine that was mentioned. Questions about other herbal medicines like Kaempferia and supplements such as Vitamin C and Zinc were also asked. (n = 8)
“My friend brought me the capsule of Andrographis paniculate extract. But I don’t trust it. Should I take it?”
3.2.3. Behavioral Health Control While Being Ill with COVID-19
- -
- Diet and drinks: Questions were asked about many kinds of food and drink and if they were fine to be eaten and drunk whilst having COVID-19. The most frequently reported concerns were around alcohol and coffee. (n = 22)
- -
- Exercise: Some questions about doing exercise during COVID-19 infection was raised by several patients. (n = 5)
3.2.4. Mental Health Problems from the Consequences of COVID-19 Infection
- -
- A mother of a boy expressed that she could observe that her son seemed stressed from being in forced isolation. (n = 1)
“I think my son (who is positive and stays in the same house) is not feeling well. He cried and said he was being kept in jail.”
- -
- Another example is a girl reported that she felt stressed as she is due to travel abroad with her boyfriend soon, but because of being sick with COVID-19 she can’t prepare a lot of documents. (n = 1)
“I will have to travel abroad with my boyfriend for which I need to prepare a lot of documents. I have teeth grinding at night and it was bleeding last night because I grind my teeth stronger than usual from the stress.”
3.2.5. Infection and Transmission Prevention
- -
- COVID-19 variants: The patients wanted to know about variants of COVID-19. (n = 2)
“Did you test for COVID-19 variant? Is it Delta variant?”
- -
- Duration of isolation: The first policy stated that the patients need 14 days isolation but later on it was changed to 10 days, so patients were confused with regard to the total number of days required and also the start date of counting. (n = 24)
“How to count the 10 days? Is it from the date we tested positive or what?”
- -
- Prevention strategies: In cases where patients were staying alone at home, the patient asked for permission not to wear a mask. (n = 5)
“I stay alone at home. Can I not wear the mask? I do not feel well when wearing it. I cannot breathe comfortably.”
- -
- Trash management: Difficult issues about trash management were reported by some patients. This was usually from those staying in shared space like an apartment or dormitory. (n = 4)
“After spraying the alcohol on the outside bag, where should I place the trash? The owner said they cannot handle the infected bag.”
3.2.6. Living with Household Members
“Will I get infected (superinfection) from my COVID-19 positive friend?”
“Now that I am infected with COVID-19, can I touch my cat, or do I need to isolate from it?”
3.3. Theme: Concerns about Health Recovery and Returning Safely to the Community after COVID-19 Infection
3.3.1. Further Self-Care
- -
- Vaccination: Most of the patients were in between doses of COVID vaccines and some were about to have the first dose. Other vaccines were also asked about by one patient. (n = 17)
“I received (vaccine name) for my second dose. Which vaccine should I go for next?”
- -
- Rehabilitation: The patient believed that the lungs were destroyed by the virus. He needed to rehabilitate the lung to normal function. (n = 1)
“If I recover, can I do both aerobic and anaerobic exercise. Which one do you think will decrease the fibrosis of the lungs better after 2 months?”
- -
- Chance of reinfection: The possibility of reinfection was of concern. (n = 4)
“Is there any possibility that I will be reinfected?”
- -
- Re-test for COVID-19: Most of the were patients concerned that they still have the virus and can spread it to others. Some asked if a re-test is required. (n = 30)
“When should I test for RT-PCR again? Or will still be positive and not needed?”
3.3.2. Social and Environment
- -
- House cleaning: There was a belief that disinfectant spray is required when cleaning the house to make sure that it is safe for themselves and other people to stay in the house later. (n = 6)
“If I completed my home isolation, will there be someone to come and spray disinfectant in my house?”
- -
- Return to work: Concerns about going back to work were high, as patients needed to make sure that their coworkers will be safe and not feel bad about them. (n = 20)
“Today is my 10th day of isolation. Tomorrow I can go out to work, right?”
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
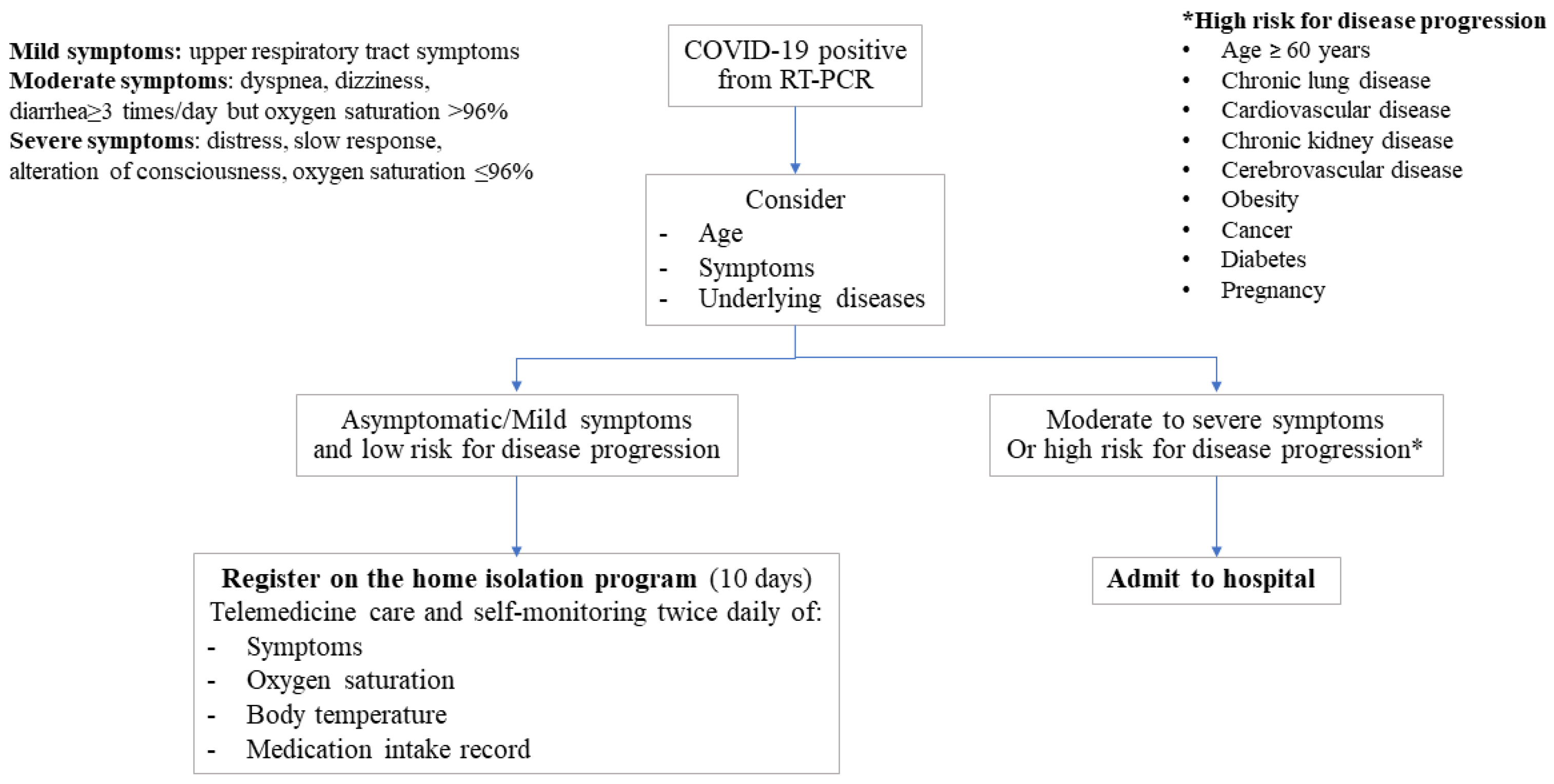
Appendix A. Initial Criteria for Home Isolation
- Live in Chiang Mai
- Confirmed COVID-19 infection by reverse transcriptase polymerase chain reaction (RT-PCR) test
- Asymptomatic or mildly symptomatic
- No lower respiratory tract symptoms (e.g., dyspnea, pleuritic chest pain, etc.)
- Age less than 60 years
- Independent living
- BMI < 30 kg/m2 or body weight < 90 kg
- None of the following health conditions: chronic obstructive pulmonary disease, cardiovascular disease, neurovascular disease, uncontrolled type 2 diabetes, or psychological conditions
- Having a separate room for isolation
- Be able to measure their body temperature and oxygen saturation twice daily.
Appendix B. Instruction for Self-Management for Home Isolation Patients
- Stay strictly within your home. No one apart from those normally residing in the house, should enter your home. You should also not visit anywhere else during home isolation or leave your home.
- Stay in a room on your own, ideally an ensuite, or your own room and a dedicated bathroom. Avoid being in contact with other people in the house. If you have symptoms such as coughing, sneezing, and a runny nose, you must wear a surgical mask even if you are alone in the room or the house.
- If you must have contact with other people in the house, you must wear a surgical mask and keep a distance of at least 1 m during the contact. If you sneeze, you must be at least 2 m distant from others. Try to sneeze or cough in a direction where no one is.
- If you cough, continue to wear a surgical mask. Do not cover the mask with your hand, since your hand might be contaminated by the surgical mask.
- Always wash your hands with soap or hand sanitizer especially after you touch your secretions (e.g., sneezing or blowing nose) or after going to the toilet and before touching things in the house that others can also touch.
- A mother can still breastfeed her child, but she must put on a surgical mask during breastfeeding.
- You need to use a private bathroom, ideally in an ensuite or a dedicated bathroom for the patient, if this is available. If the patient is using a shared bathroom with others, the patient needs to be the last one to use it. Put the toilet lid down before flushing. The bathroom should be cleaned after use.
- Cleanliness of your room: Put on a mask. Clean surfaces in the room, surfaces of toilets or areas that may be contaminated with sputum, mucus, feces, urine or secretions. Use water and bleach at a strength of at least 5% sodium hypochlorite (e.g., Haiter, Clorox).
- Strength: Use 5% Sodium hypochlorite (household bleach), 1 part bleach to 99 parts water (=0.05%) for more delicate surfaces or 1 part bleach to 9 parts water (=0.5%) for more robust and soiled surfaces.
- Do not share personal items with others in the house.
- Do not share meals with others. Someone else should provide food for the patient, leave it outside the door. Do not have direct contact with the food delivery person.
- Wash clothes, bed linen, towels, etc. with normal soap or detergent. If using a washing machine, you can use detergent and fabric softener.
- Dispose of used masks and waste contaminated with secretions into plastic bags. Tie the plastic bag tightly before dropping it into a rubbish bin with a lid. After closing the lid, wash your hands with alcohol or soap and water immediately.
References
- World Health Organization. Coronavirus Disease (COVID-19) Situation Report—102; World Health Organization: Geneva, Switzerland, 2020.
- Thailand Situation Corona Virus Disease (COVID-19). Available online: https://ddc.moph.go.th/viralpneumonia/eng/index.php (accessed on 18 March 2022).
- Coronavirus Disease 2019 (COVID-19) WHO Thailand Situation Report 173-19 April 2021; World Health Organization: Geneva, Switzerland, 2021.
- Yılmaz, Z.; Duman, S.; Öztürk, G.; Özdemir, H.; Hogan, G.; Karataş, K. Evaluating the home isolation of COVID-19 patients in primary care. J. Ideas Health 2021, 4, 357–364. [Google Scholar] [CrossRef]
- Wurzer, D.; Spielhagen, P.; Siegmann, A.; Gercekcioglu, A.; Gorgass, J.; Henze, S.; Kolar, Y.; Koneberg, F.; Kukkonen, S.; McGowan, H.; et al. Remote monitoring of COVID-19 positive high-risk patients in domestic isolation: A feasibility study. PLoS ONE 2021, 16, e0257095. [Google Scholar] [CrossRef] [PubMed]
- Bhardwaj, P.; Joshi, N.K.; Gupta, M.K.; Goel, A.D.; Saurabh, S.; Charan, J.; Rajpurohit, P.; Ola, S.; Singh, P.; Bisht, S.; et al. Analysis of Facility and Home Isolation Strategies in COVID 19 Pandemic: Evidences from Jodhpur, India. Infect. Drug Resist. 2021, 14, 2233–2239. [Google Scholar] [CrossRef] [PubMed]
- Elezkurtaj, S.; Greuel, S.; Ihlow, J.; Michaelis, E.G.; Bischoff, P.; Kunze, C.A.; Sinn, B.V.; Gerhold, M.; Hauptmann, K.; Ingold-Heppner, B.; et al. Causes of death and comorbidities in hospitalized patients with COVID-19. Sci. Rep. 2021, 11, 4263. [Google Scholar] [CrossRef]
- Monaghesh, E.; Hajizadeh, A. The role of telehealth during COVID-19 outbreak: A systematic review based on current evidence. BMC Public Health 2020, 20, 1193. [Google Scholar] [CrossRef]
- Davarpanah, A.H.; Mahdavi, A.; Sabri, A.; Langroudi, T.F.; Kahkouee, S.; Haseli, S.; Kazemi, M.A.; Mehrian, P.; Mahdavi, A.; Falahati, F.; et al. Novel Screening and Triage Strategy in Iran During Deadly Coronavirus Disease 2019 (COVID-19) Epidemic: Value of Humanitarian Teleconsultation Service. J. Am. Coll. Radiol. 2020, 17, 734–738. [Google Scholar] [CrossRef]
- Zhai, Y.; Wang, Y.; Zhang, M.; Gittell, J.H.; Jiang, S.; Chen, B.; Cui, F.; He, X.; Zhao, J.; Wang, X. From Isolation to Coordination: How Can Telemedicine Help Combat the COVID-19 Outbreak? medRxiv 2020. [Google Scholar] [CrossRef]
- Reeves, J.J.; Hollandsworth, H.M.; Torriani, F.J.; Taplitz, R.; Abeles, S.; Tai-Seale, M.; Millen, M.; Clay, B.J.; Longhurst, C.A. Rapid response to COVID-19: Health informatics support for outbreak management in an academic health system. J. Am. Med. Inform. Assoc. 2020, 27, 853–859. [Google Scholar] [CrossRef] [Green Version]
- Nicol, G.E.; Piccirillo, J.F.; Mulsant, B.H.; Lenze, E.J. Action at a Distance: Geriatric Research during a Pandemic. J. Am. Geriatr. Soc. 2020, 68, 922–925. [Google Scholar] [CrossRef] [Green Version]
- Ohannessian, R.; Duong, T.A.; Odone, A. Global Telemedicine Implementation and Integration Within Health Systems to Fight the COVID-19 Pandemic: A Call to Action. JMIR Public Health Surveill. 2020, 6, e18810. [Google Scholar] [CrossRef]
- World Health Organization. Thailand Launches “New Normal” Healthcare System to Build Back Better after COVID-19. Available online: https://www.who.int/thailand/news/feature-stories/detail/thailand-launches-new-normal-healthcare-system-to-build-back-better-after-covid-19 (accessed on 18 March 2022).
- National Statistical Office. National Household Survey of the Use of Information Technology and Communication. 2020. Available online: http://www.nso.go.th/sites/2014/DocLib13/%E0%B8%94%E0%B9%89%E0%B8%B2%E0%B8%99ICT/%E0%B9%80%E0%B8%97%E0%B8%84%E0%B9%82%E0%B8%99%E0%B9%82%E0%B8%A5%E0%B8%A2%E0%B8%B5%E0%B9%83%E0%B8%99%E0%B8%84%E0%B8%A3%E0%B8%B1%E0%B8%A7%E0%B9%80%E0%B8%A3%E0%B8%B7%E0%B8%AD%E0%B8%99/2563/Pocketbook63.pdf (accessed on 18 March 2022).
- Rojanasumapong, A.; Jiraporncharoen, W.; Nantsupawat, N.; Gilder, M.E.; Angkurawaranon, C.; Pinyopornpanish, K. Internet Use, Electronic Health Literacy, and Hypertension Control among the Elderly at an Urban Primary Care Center in Thailand: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 9574. [Google Scholar] [CrossRef] [PubMed]
- Kasatpibal, N.; Oberdorfer, P.; Katip, W.; Mektrirat, R.; Wattananandkul, U.; Thummathai, K. Factors Predicting Practices in Prevention of COVID-19 and Impacts among Population in Chiang Mai, Thailand. Medicina 2022, 58, 505. [Google Scholar] [CrossRef] [PubMed]
- Pawun, V.; Boonchuaythanasit, K.; Ponrachom, C.; Sukolpuk, M. Perception of information, knowledge and protecting behavior of diseases and health hazard of Thai citizens in 2016. J. Health Sci. Res. 2017, 11, 70–79. [Google Scholar]
- Bin Naeem, S.; Kamel Boulos, M.N. COVID-19 Misinformation Online and Health Literacy: A Brief Overview. Int. J. Environ. Res. Public Health 2021, 18, 8091. [Google Scholar] [CrossRef] [PubMed]
- Tojun, S.; Detprapon, M.; Aree-Ue, S. Sources of knowledge, knowledge, and self-care behaviors of older adults with metabolic syndrome. J. Health Sci. Res. 2020, 14, 86–96. [Google Scholar]
- Kuehn, B.M. Health Care Professionals’ Advice Can Increase COVID-19 Vaccination. JAMA 2022, 327, 518. [Google Scholar] [CrossRef]
- Huang, Y.Z.; Kuan, C.C. Vaccination to reduce severe COVID-19 and mortality in COVID-19 patients: A systematic review and meta-analysis. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 1770–1776. [Google Scholar]
- Macchia, A.; Ferrante, D.; Angeleri, P.; Biscayart, C.; Mariani, J.; Esteban, S.; Tablado, M.R.; de Quirós, F.G.B. Evaluation of a COVID-19 Vaccine Campaign and SARS-CoV-2 Infection and Mortality Among Adults Aged 60 Years And Older in a Middle-Income Country. JAMA Netw. Open 2021, 4, e2130800. [Google Scholar] [CrossRef]
- Suthar, A.B.; Wang, J.; Seffren, V.; Wiegand, R.E.; Griffing, S.; Zell, E. Public health impact of covid-19 vaccines in the US: Observational study. BMJ 2022, 377, e069317. [Google Scholar] [CrossRef]
- Van Den Broucke, S. Why health promotion matters to the COVID-19 pandemic, and vice versa. Health Promot. Int. 2020, 35, 181–186. [Google Scholar] [CrossRef] [Green Version]
- Fiske, A.; Schneider, A.; McLennan, S.; Karapetyan, S.; Buyx, A. Impact of COVID-19 on patient health and self-care practices: A mixed-methods survey with German patients. BMJ Open 2021, 11, e051167. [Google Scholar] [CrossRef] [PubMed]
- Quadros, S.; Garg, S.; Ranjan, R.; Vijayasarathi, G.; Mamun, M.A. Fear of COVID 19 Infection Across Different Cohorts: A Scoping Review. Front. Psychiatry 2021, 12, 1289. [Google Scholar] [CrossRef] [PubMed]
- Kato, T.A.; Sartorius, N.; Shinfuku, N. Forced social isolation due to COVID-19 and consequent mental health problems: Lessons from hikikomori. Psychiatry Clin. Neurosci. 2020, 74, 506–507. [Google Scholar] [CrossRef] [PubMed]
- Pancani, L.; Marinucci, M.; Aureli, N.; Riva, P. Forced Social Isolation and Mental Health: A Study on 1006 Italians Under COVID-19 Lockdown. Front. Psychol. 2021, 12, 1540. [Google Scholar] [CrossRef] [PubMed]
- Taiwo, O.; Ezugwu, A.E. Smart healthcare support for remote patient monitoring during covid-19 quarantine. Inform. Med. Unlocked 2020, 20, 100428. [Google Scholar] [CrossRef] [PubMed]
- Davenport, T.; Kalakota, R. The potential for artificial intelligence in healthcare. Future Healthc. J. 2019, 6, 94–98. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- SeyedAlinaghi, S.; Mirzapour, P.; Dadras, O.; Pashaei, Z.; Karimi, A.; MohsseniPour, M.; Soleymanzadeh, M.; Barzegary, A.; Afsahi, A.M.; Vahedi, F.; et al. Characterization of SARS-CoV-2 different variants and related morbidity and mortality: A systematic review. Eur. J. Med. Res. 2021, 26, 51. [Google Scholar] [CrossRef]
- Valentino, L.A.; Skinner, M.W.; Pipe, S.W. The role of telemedicine in the delivery of health care in the COVID-19 pandemic. Haemophilia 2020, 26, e230–e231. [Google Scholar] [CrossRef]
| Themes | Subthemes | Counts |
|---|---|---|
| 1. Complex Care system | Several steps of registration process | |
| Request for registration no. | 4 | |
| Completion of consent form | 19 | |
| Complex monitoring system and lack of clarity re: received services | ||
| Reporting of vital signs | 28 | |
| Ways to communicate with health care providers | 6 | |
| Other hospital appointments during the isolation | 4 | |
| Medical kit box | 23 | |
| Need for extra equipment | 2 | |
| Change of location to receive care | 8 | |
| Contact other hospital | 1 | |
| Documentation | 35 | |
| Meal services | 3 | |
| 2. Uncertainty about self-care and treatment plan with regard to lack of knowledges and skills. | The monitoring of symptoms and physical health in order to determine the progression of COVID-19 | |
| Monitoring of vital signs | 12 | |
| Symptom concerns | 36 | |
| Indicators of recovery | 8 | |
| Disease progression | 30 | |
| Several regimens of medication resulting from the in-advance medical box set and non-prescribed medicine | ||
| Prescribed medication | 84 | |
| Non-prescribed medication, herbal medicine or supplements | 8 | |
| Behavioral health control while being ill with COVID-19 | ||
| Diet and drinks | 22 | |
| Exercise | 5 | |
| Mental health problems from the consequences of COVID-19 infection | ||
| Stress from forced isolation | 1 | |
| Traveling abroad after COVID-19 infection | 1 | |
| Infection and transmission prevention | ||
| COVID-19 variants | 2 | |
| Duration of isolation | 24 | |
| Prevention strategies | 5 | |
| Trash management | 4 | |
| Living with household members | 22 | |
| 3. Concerns about health recovery and returning safely to the community after COVID-19 infection | Further self-care | |
| Vaccination | 17 | |
| Rehabilitation | 1 | |
| Chance of reinfection | 4 | |
| Re-test for COVID-19 | 30 | |
| Social and environment | ||
| House cleaning | 6 | |
| Return to work | 20 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pinyopornpanish, K.; Nantsupawat, N.; Buawangpong, N.; Pliannuom, S.; Vaniyapong, T.; Jiraporncharoen, W. Concerns of Home Isolating COVID-19 Patients While Receiving Care via Telemedicine during the Pandemic in the Northern Thailand: A Qualitative Study on Text Messaging. Int. J. Environ. Res. Public Health 2022, 19, 6591. https://doi.org/10.3390/ijerph19116591
Pinyopornpanish K, Nantsupawat N, Buawangpong N, Pliannuom S, Vaniyapong T, Jiraporncharoen W. Concerns of Home Isolating COVID-19 Patients While Receiving Care via Telemedicine during the Pandemic in the Northern Thailand: A Qualitative Study on Text Messaging. International Journal of Environmental Research and Public Health. 2022; 19(11):6591. https://doi.org/10.3390/ijerph19116591
Chicago/Turabian StylePinyopornpanish, Kanokporn, Nopakoon Nantsupawat, Nida Buawangpong, Suphawita Pliannuom, Tanat Vaniyapong, and Wichuda Jiraporncharoen. 2022. "Concerns of Home Isolating COVID-19 Patients While Receiving Care via Telemedicine during the Pandemic in the Northern Thailand: A Qualitative Study on Text Messaging" International Journal of Environmental Research and Public Health 19, no. 11: 6591. https://doi.org/10.3390/ijerph19116591
APA StylePinyopornpanish, K., Nantsupawat, N., Buawangpong, N., Pliannuom, S., Vaniyapong, T., & Jiraporncharoen, W. (2022). Concerns of Home Isolating COVID-19 Patients While Receiving Care via Telemedicine during the Pandemic in the Northern Thailand: A Qualitative Study on Text Messaging. International Journal of Environmental Research and Public Health, 19(11), 6591. https://doi.org/10.3390/ijerph19116591







