Reducing Medication Problems among Minority Individuals with Low Socioeconomic Status through Pharmacist Home Visits
Abstract
:1. Introduction
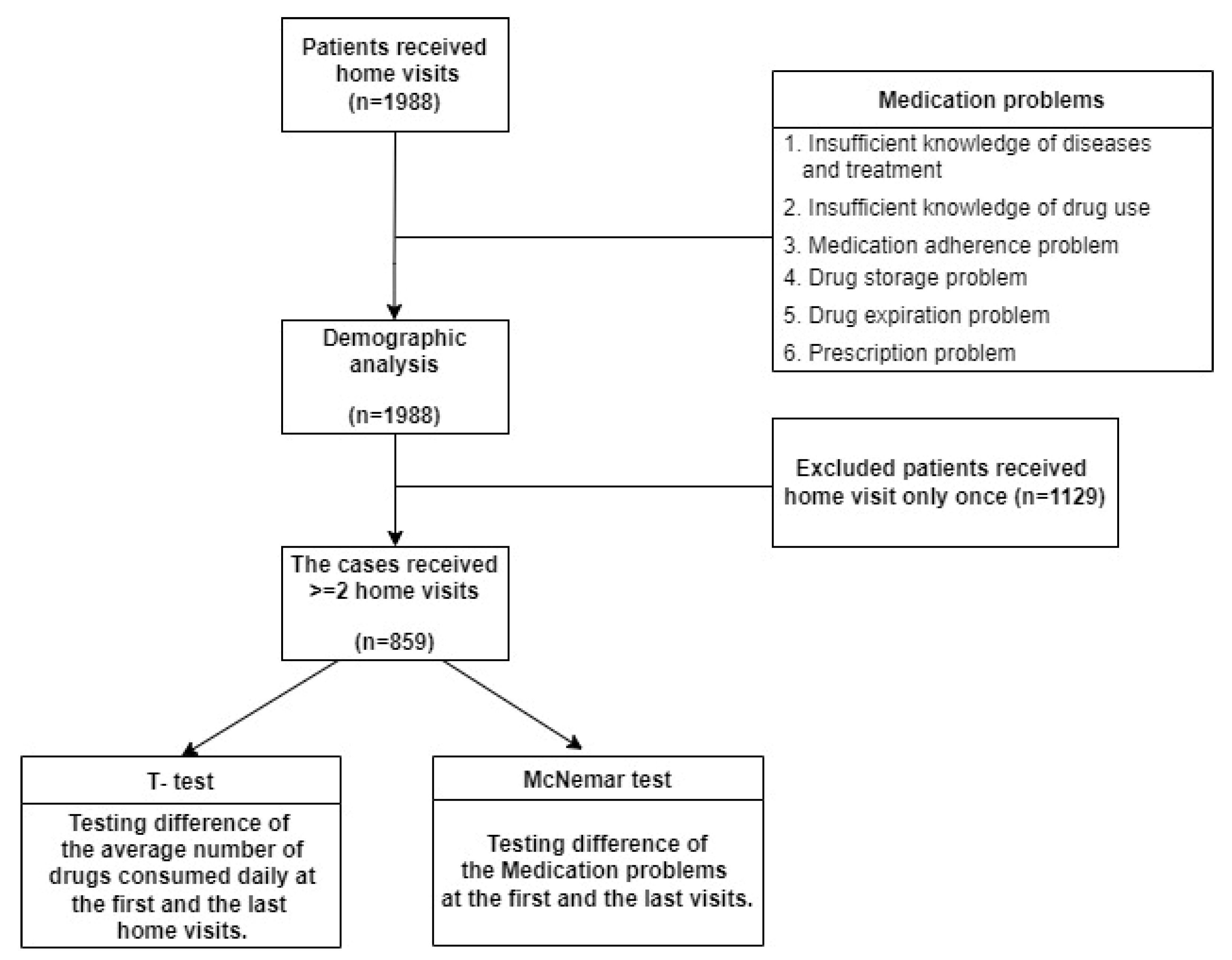
2. Materials and Methods
2.1. Study Population
2.2. Assessments
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Development Council. Estimated Population of the Republic of China. Available online: https://www.ndc.gov.tw/Content_List.aspx?n=695E69E28C6AC7F3 (accessed on 26 April 2021).
- Ministry of Health and Welfare. Annual Report of National Health Insurance Medical Statistics. Available online: https://dep.mohw.gov.tw/nhic/cp-1660-54272-116.html (accessed on 26 April 2021).
- Morath, B.; Mayer, T.; Send, A.F.J.; Hoppe-Tichy, T.; Haefeli, W.E.; Seidling, H.M. Risk factors of adverse health outcomes after hospital discharge modifiable by clinical pharmacist interventions: A review with a systematic approach. Br. J. Clin. Pharmacol. 2017, 83, 2163–2178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Connell, J.; Burke, É.; Mulryan, N.; O’Dwyer, C.; Donegan, C.; McCallion, P.; McCarron, M.; Henman, M.C.; O’Dwyer, M. Drug burden index to define the burden of medicines in older adults with intellectual disabilities: An observational cross-sectional study. Br. J. Clin. Pharmacol. 2018, 84, 553–567. [Google Scholar] [CrossRef] [PubMed]
- Hempstead, K.; Delia, D.; Cantor, J.C.; Nguyen, T.; Brenner, J. The fragmentation of hospital use among a cohort of high utilizers: Implications for emerging care coordination strategies for patients with multiple chronic conditions. Med. Care 2014, 52 (Suppl. S3), S67–S74. [Google Scholar] [CrossRef] [PubMed]
- van den Bussche, H.; Kaduszkiewicz, H.; Schäfer, I.; Koller, D.; Hansen, H.; Scherer, M.; Schön, G. Overutilization of ambulatory medical care in the elderly German population?—An empirical study based on national insurance claims data and a review of foreign studies. BMC Health Serv. Res. 2016, 16, 129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Department of Social Welfare, Taipei City Government. Living Allowance for Low-Income Households. Available online: https://dosw.gov.taipei/cp.aspx?n=E6D700BD37E78592 (accessed on 26 April 2021).
- Pharmaceutical Quality Improvement Association. The Medicine Delivered by the Hospital Seriously Exceeded the Reasonable Limit, and the Quality of the Medicine Used by the Public Is Worrying. Available online: http://tqipa.org.tw/news01.php?nid=NID098090900016 (accessed on 26 April 2021).
- Gillespie, U.; Alassaad, A.; Henrohn, D.; Garmo, H.; Hammarlund-Udenaes, M.; Toss, H.; Kettis-Lindblad, Å.; Melhus, H.; Mörlin, C. A Comprehensive Pharmacist Intervention to Reduce Morbidity in Patients 80 Years or Older: A Randomized Controlled Trial. Arch. Intern. Med. 2009, 169, 894–900. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonnet-Zamponi, D.; d’Arailh, L.; Konrat, C.; Delpierre, S.; Lieberherr, D.; Lemaire, A.; Tubach, F.; Lacaille, S.; Legrain, S. Drug-related readmissions to medical units of older adults discharged from acute geriatric units: Results of the Optimization of Medication in AGEd multicenter randomized controlled trial. J. Am. Geriatr. Soc. 2013, 61, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Freyer, J.; Hueter, L.; Kasprick, L.; Frese, T.; Sultzer, R.; Schiek, S.; Bertsche, T. Drug-related problems in geriatric rehabilitation patients after discharge—A prevalence analysis and clinical case scenario-based pilot study. Res. Soc. Adm. Pharm. 2018, 14, 628–637. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.Y.; Cheng, S.H. A community pharmacist home visit project for high utilizers under a universal health system: A preliminary assessment. Health Policy 2019, 123, 373–378. [Google Scholar] [CrossRef]
- Nkansah, N.; Mostovetsky, O.; Yu, C.; Chheng, T.; Beney, J.; Bond, C.M.; Bero, L. Effect of outpatient pharmacists’ non-dispensing roles on patient outcomes and prescribing patterns. Cochrane Database Syst. Rev. 2010. [Google Scholar] [CrossRef] [PubMed]
- Hamano, J.; Ozone, S.; Tokuda, Y. A comparison of estimated drug costs of potentially inappropriate medications between older patients receiving nurse home visit services and patients receiving pharmacist home visit services: A cross-sectional and propensity score analysis. BMC Health Serv. Res. 2015, 15, 73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abbott, R.A.; Moore, D.A.; Rogers, M.; Bethel, A.; Stein, K.; Coon, J.T. Effectiveness of pharmacist home visits for individuals at risk of medication-related problems: A systematic review and meta-analysis of randomised controlled trials. BMC Health Serv. Res. 2020, 20, 39. [Google Scholar] [CrossRef] [PubMed]
- Shcherbakova, N.; Tereso, G. Clinical pharmacist home visits and 30-day readmissions in Medicare Advantage beneficiaries. J. Eval. Clin. Pract. 2016, 22, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Ensing, H.T.; Vervloet, M.; van Dooren, A.A.; Bouvy, M.L.; Koster, E.S. Patient-pharmacist communication during a post-discharge pharmacist home visit. Int. J. Clin. Pharm. 2018, 40, 712–720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jack, B.W.; Chetty, V.K.; Anthony, D.; Greenwald, J.L.; Sanchez, G.M.; Johnson, A.E.; Forsythe, S.R.; O’Donnell, J.K.; Paasche-Orlow, M.K.; Manasseh, C.; et al. A Reengineered Hospital Discharge Program to Decrease Rehospitalization. Ann. Intern. Med. 2009, 150, 178–187. [Google Scholar] [CrossRef]
- Kansanaho, H.; Isonen-Sjölund, N.; Pietilä, K.; Airaksinen, M.; Isonen, T. Patient counselling profile in a Finnish pharmacy. Patient Educ. Couns. 2002, 47, 77–82. [Google Scholar] [CrossRef]
- Shepperd, S.; Lannin, N.A.; Clemson, L.M.; McCluskey, A.; Cameron, I.D.; Barras, S.L. Discharge planning from hospital to home. Cochrane Database Syst. Rev. 2013. [Google Scholar]
- Olsson, E.; Ingman, P.; Ahmed, B.; Kälvemark Sporrong, S. Pharmacist–patient communication in Swedish community pharmacies. Res. Soc. Adm. Pharm. 2014, 10, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Pousinho, S.; Morgado, M.; Falcão, A.; Alves, G. Pharmacist Interventions in the Management of Type 2 Diabetes Mellitus: A Systematic Review of Randomized Controlled Trials. J. Manag. Care Spec. Pharm. 2016, 22, 493–515. [Google Scholar] [CrossRef] [PubMed]
- Zelko, E.; Klemenc-Ketis, Z.; Tusek-Bunc, K. Medication Adherence in Elderly with Polypharmacy Living at Home: A Systematic Review of Existing Studies. Mater. Sociomed. 2016, 28, 129–132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ministry of Health and Welfare. National Health Insurance Medical Statistics. Available online: https://www.mohw.gov.tw/dl-70641-33764b1d-b662-4c0c-b01a-e57bd6949084.html (accessed on 15 July 2021).
- Monte, S.V.; Passafiume, S.N.; Kufel, W.D.; Comerford, P.; Trzewieczynski, D.P., Jr.; Andrus, K.; Brody, P.M. Pharmacist home visits: A 1-year experience from a community pharmacy. J. Am. Pharm. Assoc. JAPhA 2016, 56, 67–72. [Google Scholar] [CrossRef] [PubMed]
| Items | Definition |
|---|---|
| 1.Insufficient knowledge of disease and treatment | 1.1. Insufficient knowledge/erroneous understanding of disease and personal health condition |
| 1.2. Inadequate self-care skills | |
| 1.3. Inappropriate lifestyle (diet/nutrition/exercise) | |
| 1.4. Insufficient knowledge/erroneous understanding of health promotion/disease prevention | |
| 2.Insufficient knowledge of drug use | 2.1. Patient does not understand medication indications/usage/contraindications |
| 2.2. Patient does not understand precautions/side effects | |
| 2.3. Patient does not understand dosage | |
| 2.4. Patient does not understand correct medication usage | |
| 2.5. Patient does not understand correct storage method | |
| 2.6. Patient is unfamiliar with information labeled on medicine bag | |
| 3.Medication adherence problem | 3.1. Patient often forgets to take medicine |
| 3.2. Patient sometimes forgets to take medicine | |
| 3.3. Patient reduces dosage because of concerns regarding adverse effects of excessive medication use | |
| 3.4. Patient discontinues medication use because of side effects | |
| 3.5. Patient reduces/discontinues medication use because of the unpleasant taste of medicine | |
| 4.Drug storage problem | 4.1. Inappropriate storage environment/location/method |
| 4.2. Inappropriate storage temperature | |
| 4.3. Medicine bag is missing/name of the medicine is unclear | |
| 5.Drug expiration problem | 5.1. Patient continues to take expired medicine |
| 5.2. Patient does not dispose of expired medicine | |
| 5.3. Patient has unused medicine with an unknown expiry date | |
| 5.4. Patient does not routinely check the expiry dates of medicines | |
| 6.Prescription problem | 6.1. Indications |
| 6.2. Duplicate medications | |
| 6.3. Interaction | |
| 6.4. Overdose | |
| 6.5. Under dose | |
| 6.6. Inaccurate dosage | |
| 6.7. Frequency problem | |
| 6.8. Inappropriate medication for the treatment period | |
| 6.9. Monitor lab data/TDM (therapeutic drug monitoring) | |
| 6.10. ADR (adverse drug reaction) |
| Demographic Variables | ||
|---|---|---|
| N | % | |
| N | 1988 | 100 |
| Gender | ||
| man | 975 | 49.0 |
| female | 1013 | 51.0 |
| Age group (years) | ||
| <20 | 6 | 0.3 |
| 21–30 | 3 | 0.2 |
| 31–40 | 32 | 1.6 |
| 41–50 | 89 | 4.5 |
| 51–60 | 154 | 7.7 |
| 61–70 | 259 | 13.0 |
| 71–80 | 355 | 17.9 |
| 81–90 | 665 | 33.5 |
| >90 | 425 | 21.4 |
| Education level | ||
| no education | 750 | 37.7 |
| elementary | 530 | 26.7 |
| secondary | 263 | 13.2 |
| senior high school | 280 | 14.1 |
| university | 165 | 8.3 |
| Activity | ||
| function independent | 1016 | 51.1 |
| use assistive devices | 320 | 16.1 |
| use a wheelchair | 279 | 14.0 |
| long-term bed rest | 373 | 18.8 |
| Non-Middle-Aged/Middle-Aged | Not Living Alone/Living Alone | Non-Disadvantaged/Disadvantaged Status | Have Daily Physical Function/Loss of Daily Physical Function | Non-Dementia/Dementia | ||
|---|---|---|---|---|---|---|
| 1. Insufficient knowledge of diseases and treatment | 1.1 Insufficient knowledge/error of illness and medical treatment | 0.0124 | <0.0001 ** | <0.0001 ** | 0.2598 | 0.0035 * |
| 1.2 Insufficient self-care skills | <0.0001 ** | <0.0001 ** | <0.0001 ** | 0.0148 | 0.0004 ** | |
| 1.3 Inappropriate lifestyle (diet/nutrition/exercise) | <0.0001 ** | <0.0001 ** | <0.0001 ** | 0.0282 | 0.0003 ** | |
| 1.4 Inadequate awareness/errors in health promotion/disease prevention | 0.0867 | 0.0022 * | 0.0059 * | 0.0017 * | 0.0209 | |
| 2. Insufficient knowledge of drug use | 2.1 Do not understand the indications/uses of the drug | 0.2396 | 0.2165 | <0.0001 ** | 0.172 | 0.0107 |
| 2.2 Do not understand the precautions/side effects/contraindications of drug use | 0.037 | 0.2562 | 0.0002 ** | 0.2504 | 0.6017 | |
| 2.3 Do not know the usage and dosage of drugs | 0.2932 | 0.1753 | 0.0004 ** | 0.3443 | 0.0009 ** | |
| 2.4 Don’t understand how the drug is used | 0.2299 | 0.4017 | 0.4529 | 0.1525 | 0.0007 ** | |
| 2.5 Don’t know the correct way to store the medicine | 0.1641 | 0.2874 | 0.1464 | 0.3771 | 0.4712 | |
| 2.6 Not familiar with the labeling information of the medicine bag | 0.3252 | 0.0481 | 0.1695 | 0.986 | 0.0673 | |
| 3. Medication adherence problem | 3.1 Often forget to take medicine | 0.3924 | <0.0001 ** | <0.0001 ** | 0.2155 | 0.1547 |
| 3.2 Occasionally take the wrong medicine | 0.6962 | 0.2523 | 0.0768 | 0.3123 | 0.2275 | |
| 3.3 Feel that taking too much medicine is not good to reduce the amount of medicine | 0.4948 | 0.4069 | 0.1643 | 0.2212 | 0.5779 | |
| 3.4 Discontinue the medication by yourself because of the side effects of the medication | 0.1241 | 0.445 | 0.354 | 0.1483 | 0.0732 | |
| 3.5 Feel that the medicine tastes bad, reduce the dosage or stop the medicine by yourself | 0.6054 | 0.1245 | 0.9354 | 0.2559 | 0.8221 | |
| 4.Drug storage problem | 4.1 Inappropriate storage environment/location/method | 0.0022 * | 0.0031 * | <0.0001 ** | 0.1204 | 0.1656 |
| 4.2 Improper storage temperature | 0.1807 | 0.3846 | 0.7477 | 0.0153 | 0.1106 | |
| 4.3 The medicine bag is not kept or the name of the medicine is unclear | 0.0275 | 0.0714 | 0.0547 | 0.1528 | 0.115 | |
| 5. Drug expiration problem | 5.1 Continue to take expired drugs | 0.0133 | 0.0001 ** | 0.121 | 0.2654 | 0.1128 |
| 5.2 Expired medicines are not discarded | 0.1923 | 0.7748 | 0.7787 | 0.0569 | 0.9934 | |
| 5.3 Remaining medicine with the unknown expiry date | 0.4439 | 0.6784 | 0.3915 | 0.7389 | 0.0942 | |
| 5.4 No habit of regularly checking the expiration date of drugs | <0.0001 ** | 0.0873 | 0.157 | 0.7711 | 0.2279 |
| First Visit | Last Visit | McNemar Test | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | p-Value | ||
| 1. Insufficient knowledge of disease and treatment | 1.1 Insufficient knowledge/error of illness and medical treatment | 291 | 33.9 | 226 | 26.3 | <0.0001 * |
| 1.2 Insufficient self-care skills | 336 | 39.1 | 269 | 31.3 | <0.0001 * | |
| 1.3 Inappropriate lifestyle (diet/nutrition/exercise) | 248 | 28.9 | 206 | 24.0 | <0.0001 * | |
| 1.4 Inadequate awareness/errors in health promotion/disease prevention | 381 | 44.4 | 346 | 40.3 | 00.0161 | |
| 2. Insufficient knowledge of drug use | 2.1 Do not understand the indications/uses of the drug | 284 | 33.1 | 203 | 23.6 | <0.0001 * |
| 2.2 Do not understand the precautions/side effects/contraindications of drug use | 273 | 31.8 | 202 | 23.5 | <0.0001 * | |
| 2.3 Do not know the usage and dosage of drugs | 227 | 26.4 | 152 | 17.7 | <0.0001 * | |
| 2.4 Don’t understand how the drug is used | 167 | 19.4 | 120 | 14.0 | <0.0001 * | |
| 2.5 Don’t know the correct way to store the medicine | 66 | 7.7 | 49 | 5.7 | 0.0063 * | |
| 2.6 Not familiar with the labeling information of the medicine bag | 86 | 10.0 | 63 | 7.3 | 0.0026 * | |
| 3. Medication adherence problem | 3.1 Often forget to take medicine | 87 | 10.1 | 76 | 8.8 | 0.123 |
| 3.2 Occasionally take the wrong medicine | 58 | 6.8 | 47 | 5.5 | 0.055 | |
| 3.3 Feel that taking too much medicine is not good to reduce the amount of medicine | 80 | 9.3 | 59 | 6.9 | 0.0069 * | |
| 3.4 Discontinue the medication by yourself because of the side effects of the medication | 57 | 6.6 | 43 | 5.0 | 0.016 | |
| 3.5 Feel that the medicine tastes bad, reduce the dosage or stop the medicine by yourself | 18 | 2.1 | 17 | 2.0 | 0.7815 | |
| 4. Drug storage problem | 4.1 Inappropriate storage environment/location/method | 112 | 13.0 | 87 | 10.1 | 0.0029 * |
| 4.2 Improper storage temperature | 35 | 4.1 | 28 | 3.3 | 0.1439 | |
| 4.3 The medicine bag is not kept or the name of the medicine is unclear | 74 | 8.6 | 62 | 7.2 | 0.1083 | |
| 5. Drug expiration problem | 5.1 Continue to take expired drugs | 41 | 4.8 | 32 | 3.7 | 0.049 |
| 5.2 Expired medicines are not discarded | 83 | 9.7 | 46 | 5.4 | <0.0001 * | |
| 5.3 Remaining medicine with the unknown expiry date | 63 | 7.3 | 36 | 4.2 | <0.0001 * | |
| 5.4 No habit of regularly checking the expiration date of drugs | 140 | 16.3 | 109 | 12.7 | 0.0031 * | |
| 6. Prescription problem | 6.1 Indication | 72 | 8.4 | 46 | 5.4 | 0.0001 * |
| 6.2 Duplicate medication | 21 | 2.4 | 11 | 1.3 | 0.0037 * | |
| 6.3 Interaction | 13 | 1.5 | 7 | 0.8 | 0.0827 | |
| 6.4 Overdose | 19 | 2.2 | 12 | 1.4 | 0.0890 | |
| 6.5 Under dose | 8 | 0.9 | 4 | 0.5 | 0.1568 | |
| 6.6 Inaccurate dosage | 15 | 1.7 | 9 | 1.0 | 0.0334 | |
| 6.7 Frequency problem | 40 | 4.7 | 31 | 3.6 | 0.1167 | |
| 6.8 Inappropriate medication for the treatment period | 20 | 2.3 | 11 | 1.3 | 0.0197 | |
| 6.9 Monitor lab data/TDM (therapeutic drug monitoring) | 95 | 11.1 | 68 | 7.9 | 0.0006 * | |
| Variable | Average Value | Standard Deviation | Minimum | Max | p | |
|---|---|---|---|---|---|---|
| First visit | Number of oral medications per day | 8.8 | 6.1 | 0 | 36.5 | 0.1125 |
| Last visit | Number of oral medications per day | 8.5 | 5.8 | 0 | 35 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liang, Y.-h.; Wang, K.-H.; Huang, H.-M.; Shia, B.-C.; Chan, S.-Y.; Ho, C.-W.; Liu, C.-K.; Chen, M. Reducing Medication Problems among Minority Individuals with Low Socioeconomic Status through Pharmacist Home Visits. Int. J. Environ. Res. Public Health 2022, 19, 4234. https://doi.org/10.3390/ijerph19074234
Liang Y-h, Wang K-H, Huang H-M, Shia B-C, Chan S-Y, Ho C-W, Liu C-K, Chen M. Reducing Medication Problems among Minority Individuals with Low Socioeconomic Status through Pharmacist Home Visits. International Journal of Environmental Research and Public Health. 2022; 19(7):4234. https://doi.org/10.3390/ijerph19074234
Chicago/Turabian StyleLiang, Ya-hui, Kai-Hsun Wang, Hung-Meng Huang, Ben-Chang Shia, Shang-Yih Chan, Chieh-Wen Ho, Chih-Kuang Liu, and Mingchih Chen. 2022. "Reducing Medication Problems among Minority Individuals with Low Socioeconomic Status through Pharmacist Home Visits" International Journal of Environmental Research and Public Health 19, no. 7: 4234. https://doi.org/10.3390/ijerph19074234
APA StyleLiang, Y.-h., Wang, K.-H., Huang, H.-M., Shia, B.-C., Chan, S.-Y., Ho, C.-W., Liu, C.-K., & Chen, M. (2022). Reducing Medication Problems among Minority Individuals with Low Socioeconomic Status through Pharmacist Home Visits. International Journal of Environmental Research and Public Health, 19(7), 4234. https://doi.org/10.3390/ijerph19074234







