Social-Ecological Barriers to Access to Healthcare for Adolescents: A Scoping Review
Abstract
1. Introduction
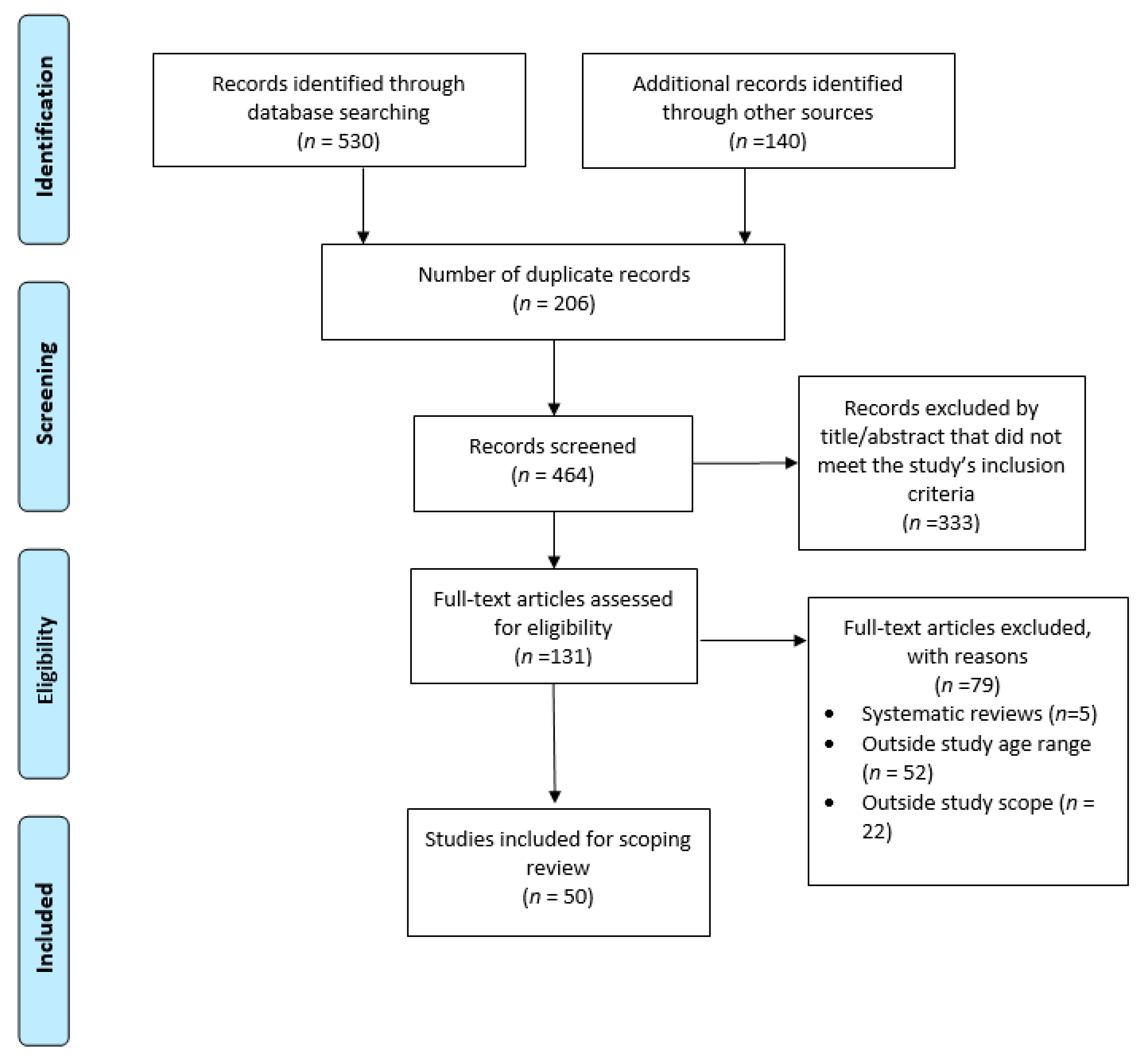
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Abstraction
2.4. Data Organization Using the Social-Ecological Model
3. Results
3.1. Study Characteristics
3.2. Primary Themes: Barriers to Care
3.2.1. Individual Level Factors
3.2.2. Interpersonal Level Factors
3.2.3. Organizational Level Factors
3.2.4. Community Level Factors
3.2.5. Policy Level Factors
3.3. Secondary Theme: Facilitators to Care
4. Discussion
4.1. Future Directions
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Agency for Healthcare Research and Quality. Elements of Access to Healthcare. Available online: https://www.ahrq.gov/research/findings/nhqrdr/chartbooks/access/elements.html (accessed on 19 March 2021).
- Simpson, L.; Owens, P.L.; Zodet, M.W.; Chevarley, F.M.; Dougherty, D.; Elixhauser, A.; McCormick, M.C. Health Care for Children and Youth in the United States: Annual Report on Patterns of Coverage, Utilization, Quality and Expenditures by Income. Ambul. Pediatr. 2005, 5, 6-e20. [Google Scholar] [CrossRef]
- Adams, S.H.; Park, M.J.; Twietmeyer, L.; Brindis, C.D.; Irwin, C.E. Young Adult Preventive Healthcare: Changes in Receipt of Care Pre- to Post-Affordable Care Act. J. Adolesc. Health 2019, 64, 763–769. [Google Scholar] [CrossRef]
- Thomée, S.; Malm, D.; Christianson, M.; Hurtig, A.K.; Wiklund, M.; Waenerlund, A.K.; Goicolea, I. Challenges and Strategies for Sustaining Youth-Friendly Health Services—A Qualitative Study from the Perspective of Professionals at Youth Clinics in Northern Sweden. Reprod. Health 2016, 13, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, A.L.; Rickert, V.I.; Aalsma, M.C. Clinical Conversations about Health: The Impact of Confidentiality in Preventive Adolescent Care. J. Adolesc. Health 2014, 55, 672–677. [Google Scholar] [CrossRef]
- Irwin, C.E.; Adams, S.H.; Jane Park, M.; Newacheck, P.W. Preventive Care for Adolescents: Few Get Visits and Fewer Get Services What’s Known on This Subject. Pediatrics 2009, 123, 2021. [Google Scholar] [CrossRef]
- Gulliver, A.; Griffiths, K.M.; Christensen, H. Perceived Barriers and Facilitators to Mental Health Help-Seeking in Young People: A Systematic Review. BMC Psychiatry 2010, 10, 113. [Google Scholar] [CrossRef]
- Bender, S.S.; Fulbright, Y.K. Content Analysis: A Review of Perceived Barriers to Sexual and Reproductive Health Services by Young People. Eur. J. Contracept. Reprod. Health Care 2013, 18, 159–167. [Google Scholar] [CrossRef]
- Brittain, A.W.; Loyola Briceno, A.C.; Pazol, K.; Zapata, L.B.; Decker, E.; Rollison, J.M.; Malcolm, N.M.; Romero, L.M.; Koumans, E.H. Youth-Friendly Family Planning Services for Young People: A Systematic Review Update. Am. J. Prev. Med. 2018, 725–735. [Google Scholar] [CrossRef]
- Garg, A.; Panda, P.; Neudecker, M.; Lee, S. Barriers to the Access and Utilization of Healthcare for Trafficked Youth: A Systematic Review. Child Abus. Negl. 2020, 100, 104137. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic Review or Scoping Review? Guidance for Authors When Choosing between a Systematic or Scoping Review Approach. BMC Med. Res. Methodol. 2018, 18, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Colquhoun, H.L.; Levac, D.; O’Brien, K.K.; Straus, S.; Tricco, A.C.; Perrier, L.; Kastner, M.; Moher, D. Scoping Reviews: Time for Clarity in Definition, Methods, and Reporting. J. Clin. Epidemiol. 2014, 1291–1294. [Google Scholar] [CrossRef]
- Arksey, H.; O’malley, L. Scoping Studies: Towards a Methodological Framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Sawyer, S.M.; Azzopardi, P.S.; Wickremarathne, D.; Patton, G.C. The Age of Adolescence. Lancet Child Adolesc. Health 2018, 223–228. [Google Scholar] [CrossRef]
- World Health Organization. Adolescent Health. Available online: https://doi.org/https://www.who.int/westernpacific/health-topics/adolescent-health (accessed on 19 March 2021).
- Garrard, J. Health Sciences Literature Review Made Easy, 6th ed.; Jones & Bartlett Learning: Burlington, MA, USA, 2020. [Google Scholar]
- Mcleroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An Ecological Perspective on Health Promotion Programs. Heal. Educ. Behav. 1988, 15, 351–377. [Google Scholar] [CrossRef]
- Diclemente, R.J.; Salazar, L.F.; Crosby, R.A. A Review of STD/HIV Preventive Interventions for Adolescents: Sustaining Effects Using an Ecological Approach. J. Pediatric Psychol. 2007, 32, 888–906. [Google Scholar] [CrossRef]
- Golden, S.D.; Earp, J.A.L. Social Ecological Approaches to Individuals and Their Contexts: Twenty Years of Health Education & Behavior Health Promotion Interventions. Health Educ. Behav. 2012, 39, 364–372. [Google Scholar] [CrossRef]
- Okumura, M.J.; Knauer, H.A.; Calvin, K.E.; Takayama, J.I. Caring for Children with Special Health Care Needs: Profiling Pediatricians and Their Health Care Resources. Matern. Child Health J. 2018, 22, 1042–1050. [Google Scholar] [CrossRef]
- Philbin, M.M.; Tanner, A.E.; DuVal, A.; Ellen, J.; Kapogiannis, B.; Fortenberry, J.D. Linking HIV-Positive Adolescents to Care in 15 Different Clinics across the United States: Creating Solutions to Address Structural Barriers for Linkage to Care. AIDS Care 2014, 26, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Soleimanpour, S.; Geierstanger, S.P.; Kaller, S.; Mccarter, V.; Brindis, C.D. The Role of School Health Centers in Health Care Access and Client Outcomes. Am. J. Public Health 2010, 100, 1597–1603. [Google Scholar] [CrossRef]
- Wilkinson, T.A.; Fahey, N.; Shields, C.; Suther, E.; Cabral, H.J.; Silverstein, M. Pharmacy Communication to Adolescents and Their Physicians Regarding Access to Emergency Contraception. Pediatrics 2012, 129, 624–629. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, T.; Jadwin-Cakmak, L.; Popoff, E.; Reisner, S.L.; Campbell, B.A.; Harper, G.W. Stigma, Gender Affirmation, and Primary Healthcare Use Among Black Transgender Youth. J. Adolesc. Health 2019, 65, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Rider, G.N.; Mcmorris, B.J.; Gower, A.L.; Coleman, E.; Eisenberg, M.E. Health and Care Utilization of Transgender and Gender Nonconforming Youth: A Population-Based Study. Pediatrics 2018, 141, e20171683. [Google Scholar] [CrossRef]
- MacApagal, K.; Bhatia, R.; Greene, G.J. Differences in Healthcare Access, Use, and Experiences Within a Community Sample of Racially Diverse Lesbian, Gay, Bisexual, Transgender, and Questioning Emerging Adults. LGBT Health 2016, 3, 434–442. [Google Scholar] [CrossRef] [PubMed]
- Baggio, S.; Tran, N.T.; Barnert, E.S.; Gétaz, L.; Heller, P.; Wolff, H. Lack of Health Insurance among Juvenile Offenders: A Predictor of Inappropriate Healthcare Use and Reincarceration? Public Health 2019, 166, 25–33. [Google Scholar] [CrossRef]
- Luk, J.W.; Ph, D.; Gilman, S.E.; Sc, D.; Haynie, D.L.; Ph, D.; H, M.P.; Simons-morton, B.G.; Ed, D.; H, M.P. Sexual Orientation Differences in Adolescent Health Care Access and Health-Promoting Physician Advice. J. Adolesc. Health 2017, 61, 555–561. [Google Scholar] [CrossRef]
- Chelvakumar, G.; Ford, N.; Kapa, H.M.; Lange, H.L.H.; Laurie, A.; Andrea, M. Healthcare Barriers and Utilization Among Adolescents and Young Adults Accessing Services for Homeless and Runaway Youth. J. Community Health 2017, 42, 437–443. [Google Scholar] [CrossRef]
- Mcmanus, M.A.; Pollack, L.R.; Cooley, W.C.; Mcallister, J.W.; Lotstein, D.; Strickland, B.; Mann, M.Y. Current Status of Transition Preparation Among Youth With Special Needs in the United States. Pediatrics 2013, 131, 1090–1097. [Google Scholar] [CrossRef]
- Tanner, A.E.; Philbin, M.M.; Chambers, B.D.; Ma, A.; Hussen, S.; Ware, S.; Lee, S.; Fortenberry, J.D. Healthcare Transition for Youth Living with HIV: Outcomes from a Prospective Multi-Site Study. J. Adolesc. Health 2018, 63, 157–165. [Google Scholar] [CrossRef]
- Valenzuela, J.M.; Seid, M.; Waitzfelder, B.; Anderson, A.M.; Beavers, D.P.; Dabelea, D.M.; Dolan, L.M.; Imperatore, G.; Marcovina, S.; Reynolds, K.; et al. Prevalence of and Disparities in Barriers to Care Experienced by Youth with Type 1 Diabetes. J. Pediatr. 2014, 164, 1369–1375.e1. [Google Scholar] [CrossRef]
- Jaacks, L.M.; Oza-Frank, R.A., Jr.; Dolan, L.M.; Dabelea, D.; Lawrence, J.M.; Pihoker, C.; Rebecca, M.O.; Linder, B.; Imperatore, G.; Seid, M.; et al. Migration Status in Relation to Clinical Characteristics and Barriers to Care Among Youth with Diabetes in the US. J. Immigr. Minor. Health 2012, 14, 949–958. [Google Scholar] [CrossRef][Green Version]
- Boulet, S.L.; Yanni, E.A.; Creary, M.S.; Olney, R.S. Health Status and Healthcare Use in a National Sample of Children with Sickle Cell Disease. Am. J. Prev. Med. 2010, S528–S535. [Google Scholar] [CrossRef]
- Kavanaugh, M.L.; Jerman, J.; Ethier, K.; Moskosky, S. Meeting the Contraceptive Needs of Teens and Young Adults: Youth-Friendly and Long-Acting Reversible Contraceptive Services in U.S. Family Planning Facilities. J. Adolesc. Health 2013, 52, 284–292. [Google Scholar] [CrossRef]
- Ralph, L.J.; Brindis, C.D. Access to Reproductive Healthcare for Adolescents: Establishing Healthy Behaviors at a Critical Juncture in the Lifecourse. Curr. Opin. Obstet. Gynecol. 2010, 22, 369–374. [Google Scholar] [CrossRef]
- Strickland, B.B.; Jones, J.R.; Ghandour, R.M.; Kogan, M.D.; Newacheck, P.W. The Medical Home: Health Care Access and Impact for Children and Youth in the United States. Pediatrics 2011, 127, 604–611. [Google Scholar] [CrossRef] [PubMed]
- Islam, J.Y.; Gruber, J.F.; Kepka, D.; Kunwar, M.; Smith, S.B.; Rothholz, M.C.; Brewer, N.T.; Smith, J.S. Human Vaccines & Immunotherapeutics Pharmacist Insights into Adolescent Human Papillomavirus Vaccination Provision in the United States Pharmacist Insights into Adolescent Human Papillomavirus Vaccination Provision in the United States. Hum. Vaccines Immunother. 2019. [Google Scholar] [CrossRef]
- Minnaert, J.; Kenney, M.K.; Ghandour, R.; Koplitz, M.; Silcott, S. CSHCN with Hearing Difficulties: Disparities in Access and Quality of Care. Disabil. Health J. 2020, 13, 100798. [Google Scholar] [CrossRef]
- Dang, M.T.; Whitney, K.D.; Virata, M.C.D.; Binger, M.M.; Miller, E. A Web-Based Personal Health Information System for Homeless Youth and Young Adults. Public Health Nurs. 2011. [Google Scholar] [CrossRef]
- Lai, K.; Guo, S.; Ijadi-Maghsoodi, R.; Puffer, M.; Kataoka, S.H. Bringing Wellness to Schools: Opportunities for and Challenges to Mental Health Integration in School-Based Health Centers. Psychiatr. Serv. 2016, 67, 1328–1333. [Google Scholar] [CrossRef]
- Hallum-Montes, R.; Middleton, D.; Schlanger, K.; Romero, L. Barriers and Facilitators to Health Center Implementation of Evidence-Based Clinical Practices in Adolescent Reproductive Health Services. J. Adolesc. Health 2016, 58, 276–283. [Google Scholar] [CrossRef][Green Version]
- Mullins, T.L.K.; Zimet, G.; Lally, M.; Kahn, J.A. Adolescent Human Immunodeficiency Virus Care Providers’ Attitudes Toward the Use of Oral Pre-Exposure Prophylaxis in Youth. AIDS Patient Care STDS 2016, 30, 339–348. [Google Scholar] [CrossRef]
- Connors, K.M. Barriers Latino Patients Face in the Pediatric Emergency Department. Pediatr. Nurs. 2019, 45, 37–41. [Google Scholar]
- Ozturk, O.D.; McDermott, S.; Mann, J.R.; Hardin, J.W.; Royer, J.A.; Ouyang, L. Disparities in Health Care Utilization by Race among Teenagers and Young Adults with Muscular Dystrophy. Med. Care 2014, 52, S32–S39. [Google Scholar] [CrossRef]
- Miller, R.L.; Chiaramonte, D.; Strzyzykowski, T.; Sharma, D.; Anderson-Carpenter, K.; Fortenberry, J.D. Improving Timely Linkage to Care among Newly Diagnosed HIV-Infected Youth: Results of SMILE. J. Urban Health 2019, 96, 845–855. [Google Scholar] [CrossRef] [PubMed]
- Grossbard, J.R.; Lehavot, K.; Hoerster, K.D.; Jakupcak, M.; Seal, K.H.; Simpson, T.L. Relationships Among Veteran Status, Gender, and Key Health Indicators in a National Young Adult Sample. Psychiatr. Serv. 2013, 64, 547–553. [Google Scholar] [CrossRef]
- Hudson, A.L.; Nyamathi, A.; Greengold, B.; Slagle, A.; Koniak-Griffin, D.; Khalilifard, F.; Getzoff, D. Health-Seeking Challenges among Homeless Youth. Nurs. Res. 2010, 59, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Marks, S.J.; Merchant, R.C.; Clark, M.A.; Liu, T.; Rosenberger, J.G.; Bauermeister, J.; Mayer, K.H. Potential Healthcare Insurance and Provider Barriers to Pre-Exposure Prophylaxis Utilization among Young Men Who Have Sex with Men. AIDS Patient Care STDS 2017, 31, 470–478. [Google Scholar] [CrossRef]
- Bessett, D.; Prager, J.; Havard, J.; Murphy, D.J.; Agénor, M.; Foster, A.M. Barriers to Contraceptive Access after Health Care Reform: Experiences of Young Adults in Massachusetts. Womens Health Issues 2015, 25, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Anderson, C.; Peskoe, S.; Parmer, M.; Eddy, N.; Howe, J.; Fitzgerald, T.N. Children with Appendicitis on the US–Mexico Border Have Socioeconomic Challenges and Are Best Served by a Freestanding Children’s Hospital. Pediatr. Surg. Int. 2018, 34, 1269–1280. [Google Scholar] [CrossRef]
- Smalley, L.P.; Kenney, M.K.; Denboba, D.; Strickland, B. Family Perceptions of Shared Decision-Making with Health Care Providers: Results of the National Survey of Children with Special Health Care Needs, 2009–2010. Matern. Child Health J. 2014, 18, 1316–1327. [Google Scholar] [CrossRef]
- Kreider, A.R.; French, B.; Aysola, J.; Saloner, B.; Noonan, K.G.; Rubin, D.M. Quality of Health Insurance Coverage and Access to Care for Children in Low-Income Families. JAMA Pediatr. 2016, 170, 43–51. [Google Scholar] [CrossRef] [PubMed]
- Mason, M.J.; Keyser-Marcus, L.; Snipes, D.; Benotsch, E.; Sood, B. Perceived Mental Health Treatment Need and Substance Use Correlates Among Young Adults. Psychiatr. Serv. 2013, 64, 871–877. [Google Scholar] [CrossRef] [PubMed]
- Macqueen, K.M.; Chen, M.; Jolly, D.; Mueller, M.P.; Okumu, E.; Eley, N.T.; Laws, M.; Isler, M.R.; Kalloo, A.; Rogers, R.C. HIV Testing Experience and Risk Behavior Among Sexually Active Black Young Adults: A CBPR-Based Study Using Respondent-Driven Sampling in Durham, North Carolina. Am. J. Community Psychol. 2015. [Google Scholar] [CrossRef] [PubMed]
- Avila, R.M.; Bramlett, M.D. Language and Immigrant Status Effects on Disparities in Hispanic Children’s Health Status and Access to Health Care. Matern. Child Health J. 2012. [Google Scholar] [CrossRef]
- Kruszka, J.B.; Lindell, D.; Killion, C.C.S. “It’s Like Pay Or Don’t Have It and Now I’m Doing Without” The Voice of Transitional Uninsured Former Foster Youth. Policy Polit. Nurs. Pract. 2012. [Google Scholar] [CrossRef]
- Kubicek, K.; Beyer, W.J.; Wong, C.F.; Kipke, M.D. Engaging Young Men in the Hiv Prevention and Care Continua: Experiences from Young Men of Color Who Have Sex with Men. AIDS Educ. Prev. 2019, 31, 325–343. [Google Scholar] [CrossRef] [PubMed]
- Sudhinaraset, M.; To, T.M.; Ling, I.; Melo, J.; Chavarin, J. The Influence of Deferred Action for Childhood Arrivals on Undocumented Asian and Pacific Islander Young Adults: Through a Social Determinants of Health Lens. J. Adolesc. Health 2017, 60, 741–746. [Google Scholar] [CrossRef]
- Monz, B.U.; Houghton, R.; Law, K.; Loss, G. Treatment Patterns in Children with Autism in the United States. Autism Res. 2019, 12, 517–526. [Google Scholar] [CrossRef]
- Kelly, M.J.; Sung, L.; Dickens, D.S. Barriers to Medication Access in Pediatric Oncology in the United States. J. Pediatr. Hematol. Oncol. 2019, 41, 286–288. [Google Scholar] [CrossRef]
- Lin, M.H.; Connor, C.G.; Ruedy, K.J.; Beck, R.W.; Kollman, C.; Buckingham, B.; Redondo, M.J.; Schatz, D.; Haro, H.; Lee, J.M.; et al. Race, Socioeconomic Status, and Treatment Center Are Associated with Insulin Pump Therapy in Youth in the First Year Following Diagnosis of Type 1 Diabetes. Diabetes Technol. Ther. 2013, 15, 929–934. [Google Scholar] [CrossRef] [PubMed]
- Berg, C.; Stratton, E.; Esiashvili, N.; Mertens, A.; Vanderpool, R.C. Providers’ Perspectives of Survivorship Care for Young Adult Survivors of Childhood Cancer. J. Cancer Educ. 2016, 31, 31–38. [Google Scholar] [CrossRef]
- Calderon, S.J.; Mallory, C.; Malin, M. Parental Consent and Access to Oral Health Care for Adolescents. Policy Polit. Nurs. Pract. 2017, 18, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Cheak-Zamora, N.C.; Yang, X.; Farmer, J.E.; Clark, M. Disparities in Transition Planning for Youth with Autism Spectrum Disorder. Pediatrics 2013, 131, 447–454. [Google Scholar] [CrossRef]
- Bernstein, J.; Gebel, C.; Vargas, C.; Geltman, P.; Walter, A.; Garcia, R.I.; Tinanoff, N. Integration of Oral Health into the Well-Child Visit at Federally Qualified Health Centers: Study of 6 Clinics, August 2014–March 2015. Prev. Chronic Dis. 2016, 13, 160066. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kaplan, D.W. Barriers and Potential Solutions to Increasing Immunization Rates in Adolescents. J. Adolesc. Health 2010, S24–S33. [Google Scholar] [CrossRef]
- Deutsch, S.A.; Fortin, K. Physical Health Problems and Barriers to Optimal Health Care among Children in Foster Care. Curr. Probl. Pediatr. Adolesc. Health Care 2015, 45, 286–291. [Google Scholar] [CrossRef]
- Keeton, V.F.; Chen, A.K. Immunization Updates and Challenges. Curr. Opin. Pediatr. 2010, 22, 234–240. [Google Scholar] [CrossRef]
- Carr, K.L.; Stewart, M.W. Effectiveness of School-Based Health Center Delivery of a Cognitive Skills Building Intervention in Young, Rural Adolescents: Potential Applications for Addiction and Mood. J. Pediatr. Nurs. 2019, 47, 23–29. [Google Scholar] [CrossRef]
- Pew Research Center. Americans are Closely Divided Over Value of Medical Treatments, But Most Agree Costs are A Big Problem. Available online: https://www.pewresearch.org/fact-tank/2018/07/09/americans-are-closely-divided-over-value-of-medical-treatments-but-most-agree-costs-are-a-big-problem/ (accessed on 19 March 2021).
- Pew Research Center. Health Affairs: Among 11 nations, American Seniors Struggle More with Health Costs. Available online: https://www.pewresearch.org/fact-tank/2014/12/03/health-affairs-among-11-nations-american-seniors-struggle-more-with-health-costs/ (accessed on 19 March 2021).
- Levesque, J.-F.; Harris, M.F.; Russell, G. Patient-Centred Access to Health Care: Conceptualising Access at the Interface of Health Systems and Populations. Int. J. Equity Health 2013. [Google Scholar] [CrossRef]
- Tebb, K.P.; Sedlander, E.; Bausch, S.; Brindis, C.D. Opportunities and Challenges for Adolescent Health Under the Affordable Care Act. Matern. Child Health J. 2015, 19, 2089–2093. [Google Scholar] [CrossRef]
- Guo, S.; Nguyen, H.; Weiss, B.; Ngo, V.K.; Lau, A.S. Linkages between Mental Health Need and Help-Seeking Behavior among Adolescents: Moderating Role of Ethnicity and Cultural Values. J. Couns. Psychol. 2015, 62, 682–693. [Google Scholar] [CrossRef]
- Marsiglia, F.F.; Medina-Mora, M.E.; Gonzalvez, A.; Alderson, G.; Harthun, M.; Ayers, S.; Nuño Gutiérrez, B.; Corona, M.D.; Mendoza Melendez, M.A.; Kulis, S. Binational Cultural Adaptation of the Keepin’ It REAL Substance Use Prevention Program for Adolescents in Mexico. Prev. Sci. 2019, 20, 1125–1135. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Minors’ Consent Laws. Available online: https://www.cdc.gov/hiv/policies/law/states/minors.html (accessed on 19 March 2021).
- Guttmacher Institute. Parental Involvement in Minors’ Abortions. Available online: https://www.guttmacher.org/state-policy/explore/parental-involvement-minors-abortions (accessed on 19 March 2021).
- Braverman, P.K.; Adelman, W.P.; Alderman, E.M.; Breuner, C.C.; Levine, D.A.; Marcell, A.V.; O’Brien, R. The Adolescent’s Right to Confidential Care When Considering Abortion. Pediatrics 2017, 139, e20163861. [Google Scholar] [CrossRef]
- Maslyanskaya, S.; Alderman, E.M. Confidentiality and Consent in the Care of the Adolescent Patient. Pediatr. Rev. 2019, 40, 508–516. [Google Scholar] [CrossRef] [PubMed]
- Aura, A.; Sormunen, M.; Tossavainen, K. The Relation of Socio-Ecological Factors to Adolescents’ Health-Related Behaviour: A Literature Review. Health Educ. 2016, 77–201. [Google Scholar] [CrossRef]

| Author (Year) | Study Design | Healthcare Setting, Type of Care | Study Population, Size | Target Population | Barriers Identified |
|---|---|---|---|---|---|
| Okumara et al. (2018) [20] | Quantitative; Cross-sectional | Primary, a general healthcare | Members of the American Academy of Pediatrics in California, (n = 1203) | Children with special healthcare needs | Pediatricians reported a lack of access to mental health services, care coordination, and case management. |
| Philbin et al. (2014) [21] | Qualitative; Cross-sectional | Primary, other healthcare ! | Staff at 15 Adolescent Trails Network clinics, (n = 124) | HIV-positive adolescents | Barriers identified included health insurance access, transportation, care coordination, physical space, provider procedural issues, geographic location, and teens’ readiness to care. |
| Soleimanpour et al. (2010) [22] | Mixed method; Longitudinal | School-based health center, general healthcare | Clients * from 12 school health centers (n = 7696), and students (n = 105) | Adolescents in middle and high schools | Students do not think they need the needed care, lacked awareness of the school health center’s services, and perceived judgment from peers for seeking care. |
| Wilkinson et al. (2012) [23] | Quantitative; Cross-sectional | Pharmacy, reproductive healthcare | Pharmacies in 5 cities (n = 943) | Adolescents | Adolescent mystery callers received incorrect information about how to obtain emergency contraception. |
| Goldenberg et al. (2019) [24] | Mixed method; Cross-sectional | Primary, general healthcare | Adolescent Medicine Trials Network for HIV/AIDS Interventions from 14 U.S cities | Black transgender youths (n = 110) | Transgender youths with unmet gender affirmation needs had higher shares of anticipated stigma and healthcare nonuse. |
| Rider et al. (2018) [25] | Quantitative; Cross-sectional | Primary, general healthcare | Minnesota Student Survey (n = 80,929; cisgender (n = 78,761; TGNC + (n = 2168) | Adolescents in 9th and 11th grades | Gender expression |
| Macapagal et al. (2016) [26] | Quantitative; Longitudinal | Primary, general healthcare | LGBTQ (n = 206) | LGBTQ youths 13 to 24 years old | Insurance access and patient-provider relationships |
| Baggio et al. (2019) [27] | Quantitative; Longitudinal | Primary, general healthcare | Juvenile offenders (n = 4735) | Juvenile offenders 20 to 23 | Lack of intermittent health insurance coverage |
| Luk et al. (2017) [28] | Quantitative; Longitudinal | Primary, general healthcare | Adolescents (n = 2023) | Adolescents in 10th grade | Sexual orientation disparity in unmet medical needs was found among males only. On the other hand, sexual minority females were more likely to have no routine checkup in the past year |
| Chelvakumar et al. (2017) [29] | Quantitative; Cross-sectional | Primary, general healthcare | Homeless and runaway adolescents and young adults from three centers in Central Ohio (n = 180) | Homeless and runaway adolescents and young adults | Transportation barriers, health insurance access, cost of care, and issues related to confidentiality and trust with providers |
| McManus et al. (2013) [30] | Quantitative; Cross-sectional | Primary, general healthcare | Youths with special healthcare needs (n = 17,114) | Youths with special healthcare needs (YSHCN) ages 12 and 18. | Gender, race/ethnicity, family income, specific health conditions, not having a medical home, and health insurance are associated with transitioning into adult care. |
| Tanner et al. (2018) [31] | Mixed method; Longitudinal | Primary, other healthcare | Electronic medical records (n = 135), interviews with adolescents (n = 28), and adult providers (n = 30) | Youths living with HIV | Individual-level barriers (health insurance status and disclosure-related stigma) and structural barriers within the clinic |
| Valenzuela et al. (2014) [32] | Quantitative; Cross-sectional | Primary, other healthcare | children and youths with type 1 diabetes (n = 780) | children and youths with Type 1 diabetes less than 20 years | Cost of care, communication with providers, getting needed information, problems with access to care, not having a regular provider, and receiving contextual care were associated with poorer glycated hemoglobin levels. |
| Jaacks et al. (2012) [33] | Quantitative; Cross-sectional | Primary, other healthcare | Youths of foreign-born parents with diabetes (n = 3086) | Youths of foreign-born parents with Type 1 and 2 diabetes less than 20 years | In the unadjusted analysis, youths with foreign-born parents experienced barriers related to having a regular doctor, access to care, and contextual care |
| Boulet et al. (2010) [34] | Quantitative; Cross-sectional | Primary, other healthcare | Children with sickle cell disease (n = 19,527) | Children with sickle cell disease (SCD) aged 0–17 | Black children with SCD experienced problems accessing available healthcare services, such as difficulty setting up an appointment, excessive wait times before seeing a doctor, and difficulty in arranging transportation to the site of a healthcare provider. |
| Kavanaugh et al. (2013) [35] | Quantitative; Cross-sectional | Primary, reproductive healthcare | Publicly funded family planning facilities (n = 584) | Adolescents younger than 20 and young adults aged 20 and 24. | Costs to long-acting reversible contraceptives, inconvenient clinic hours, staff concerns, limited training on implant insertion were barriers to provided contraceptive and long-acting reversible contraceptives. |
| Ralph & Brindis (2010) [36] | Review | Primary, reproductive healthcare | Not applicable | Adolescents | Common barriers to care for adolescents include concerns about confidentiality and costs. |
| Strickland et al. (2011) [37] | Quantitative; Cross-sectional | Primary, general healthcare | Adolescents (n = 83,448) | Adolescents aged 1–17 | Disparities to having a medical home included race/ethnic characteristics, socioeconomic status, and existing health conditions. |
| Islam et al. (2019) [38] | Quantitative; Cross-sectional | Pharmacy, reproductive healthcare | Licensed pharmacists in eight states (n = 40) | Adolescents 9–17 | Challenges to HPV vaccination included parental consent, tracking and patient recall, perceived stigma of immunization, and promotion of vaccination |
| Minnaert et al. (2020) [39] | Quantitative; Cross-sectional | Primary, general healthcare | Children with hearing difficulties (n = 40,242) | Children with hearing difficulties aged 0–17 | Children with hearing difficulties did not have access to a medical home, community services, and adequate health insurance coverage |
| Dang et al. (2011) [40] | Qualitative; Cross-sectional | Primary, general healthcare | Youths and young adults enrolled in a Healthshack-a personal health information system (n = 149) | Runaway and homeless youths and young adults ages 9 to 24. | Access and knowledge about care, inconsistence use of medications, lack of medical follow-ups, and transportation issues were reported barriers youths encountered |
| Lai et al. (2016) [41] | Qualitative; Cross-sectional | School-based health center, behavioral healthcare | Mental/primary care providers and care coordinators from 14 SBHCs (n = 43) | Not specified | Providers reported that concerns about trust, confidentiality, and stigma related to mental illness inhibit the use of services among students. |
| Hallum-Montes et al. (2016) [42] | Qualitative; Cross-sectional | Health centers, reproductive healthcare | Staff members of 30 health centers in 7 States (n = 85) | Adolescents | Structural barriers within the health system and community-related factors prevented implementation of evidence-based clinical practice for adolescent’s reproductive healthcare. |
| Mullins et al. (2016) [43] | Qualitative; Cross-sectional | Primary, other healthcare | Clinicians from the Adolescent Medicine Trials Network for HIV/AIDS Interventions (ATN) in 14 U.S. locations (n = 15) | HIV-infected and at-risk adolescents and youths | Barriers to prescribing PrEP to minors and youths were categorized in the patient-level, provider-level, organizational/systems-level, and community-level factors. |
| Connors (2019) [44] | Review/Case study | Primary, general healthcare | Not applicable | Adolescents and youths | Latino children and their families face barriers related to limited English proficiency, poor understanding of the U.S. healthcare system, lack of providers, and immigration status complications. |
| Ozturk et al. (2014) [45] | Quantitative; Cross-sectional | Primary, other healthcare | Teenagers and young adults | Teenagers and young adults aged 15–24 with muscular dystrophy | Race is correlated with healthcare utilization. Blacks have lower overall utilization, less primary/therapy/specialist care, and higher emergency department utilization than other races |
| Miller et al. (2019) [46] | Quantitative; Longitudinal | Primary, other healthcare | Data from eight adolescent medicine clinical trial units (n = 2,142). Key informants (youths, n = 39; adults, n = 152). | Youths aged 12–24 newly diagnosed with HIV | Barriers addressed included linkage to care, the continuation of care, structural barriers, youth-friendly services, and stigma. |
| Grossbard et al. (2013) [47] | Quantitative; Cross-sectional | Primary, general healthcare | Young adults (n = 27,471) | Young adults (veterans and civilians) aged 19–30 | Gender differences in healthcare access and utilization. Women were more likely to have health insurance and being able to see a provider than men |
| Hudson et al. (2010) [48] | Qualitative; Cross-sectional | Primary, general healthcare | Homeless youths (n = 24) | Homeless youths aged 18–25 | Homeless youths experience structural barriers within the health system and social barriers, including law enforcement and society. |
| Marks et al. (2017) [49] | Quantitative; Cross-sectional | Primary, other healthcare | Young men who have sex with men (n = 2297) | Young HIV uninfected men who have sex with men aged 18 –24 | Lack of access to care differed by and associated with age, race/ethnicity, education, and region. |
| Bessett et al. (2015) [50] | Qualitative; Cross-sectional | Primary, reproductive healthcare | Young adults (n = 89) | Young adults aged 18–26 | Young adults seeking contraceptive care had low health insurance literacy and faced barriers related to information and privacy |
| Anderson et al. (2018) [51] | Quantitative; Cross-sectional | Primary, general healthcare | Pediatric patients (n = 98) | Pediatric patients with appendicitis | Structural barriers relating to practitioner misdiagnosis, lack of health insurance coverage, no frequent pediatrician, cost of care, limited knowledge of appendicitis |
| Smalley et al. (2014) [52] | Quantitative; Cross-sectional | Primary, general healthcare | Children with special healthcare needs (n = 40,242) | Children with a special healthcare need aged 0–17 | Families of children with greater functional limitations were less likely to make a shared-decision with their providers. Low socioeconomic status and race were associated with low shared-decision making attainment rates |
| Kreider et al. (2016) [53] | Quantitative; Cross-sectional | Primary, general healthcare | Children with household income between 100% and 300% of the federal poverty line (n = 80,655) | Children from low-income households aged 17 and younger | Access to specialty care, inability to obtain healthcare services, those with special healthcare needs, and health insurance type. |
| Mason et al. (2013) [54] | Quantitative; Cross-sectional | Primary, behavioral healthcare | Young adults aged (n = 14,718) | Young adults aged 18 to 23 | Gender, substance use, and race/ethnicity were associated with perceived mental health treatment needs. |
| MacQueen et al. (2015) [55] | Qualitative; Cross-sectional | Primary, other healthcare | Young adults (n = 508) | Young Black adults aged 18–30 | Barriers to receiving HIV testing were related to perceived risk and stigma. Low-income Black adults experience reduced access to healthcare services. |
| Avila & Bramlett (2013) [56] | Quantitative; Cross-sectional | Primary, general healthcare | Adolescents (n = 91,642) | Adolescents aged 0–17 | Immigration status and non-English speaking household as primary language was associated with disparities to care, dental health, consistent insurance, and having a medical home among first-generation vs. non-immigrant Hispanic children, non-immigrant Hispanic children vs. non-Hispanic white children, and Hispanic children in English speaking household vs. non-Hispanic white children. |
| Kruszka et al. (2012) [57] | Qualitative; Cross-sectional | Primary, general healthcare | Former foster youths (n = 9) | Uninsured former foster youths | Former foster youths reported issues relating to not having the right documentation, roadblocks to securing healthcare insurance, and lack of knowledge about Medicaid eligibility. |
| Kubicek et al. (2019) [58] | Qualitative; Cross-sectional | Primary, other healthcare | Young Black men who have sex with men (n = 49) | Young Black men who have sex with men aged 16 to 24 | Limited health literacy, inability to identify appropriate providers, cultural values, and histories concerning healthcare and cultural competency among community providers were reported barriers to care among Black young men who have sex with men |
| Sudhinaraset et al. (2017) [59] | Qualitative; Cross-sectional | Primary, general healthcare | Undocumented Asians and Pacific Islanders (n = 32) | Undocumented Asians and Pacific Islanders aged 18–31 | Financial costs associated with healthcare services were major barriers undocumented immigrants experienced pre-DACA period. DACA ineligibility for family members prevented others from seeking the needed healthcare services |
| Monz et al. (2019) [60] | Quantitative; Cross-sectional | Primary, other healthcare | Caregivers of children with autism (n = 10,123) | Children with autism aged 3–17 years | Caregivers reported that waiting-list, no-coverage, and costs were common provider and health plan-related barriers. Waiting-list was common in metropolitan areas than non-metropolitan areas. |
| Kelly et al. (2019) [61] | Quantitative; Cross-sectional | Primary, other healthcare | Pediatric oncologists (n = 18) | Pediatrics, adolescents, and young adults | Pediatrics oncologists reported delay in prior authorization requests created a delay in receiving planned chemotherapy, and supportive care treatment and medication access were associated with a delay in starting therapy. |
| Lin et al. (2013) [62] | Quantitative; Cross-sectional | Primary, other healthcare | Youths with Type 1 Diabetes (n = 1012) | Youths below 19 years with Type 1 Diabetes | Racial/ethnic group, insurance status, and household income appeared to influence whether participants were switched from injection to pump therapy |
| Berg et al. (2016) [63] | Qualitative; Cross-sectional | Primary, other healthcare | Healthcare providers of young adult cancer survivors (n = 21) | Adolescents, young adult cancer survivors | Systems-level barriers to engagement in survivorship care included limited resources, role confusion, communication challenges, and lack of insurance coverage. Patient-level barriers include psychological barriers, resistance to survivorship care, and physical barriers. |
| Calderon et al. (2017) [64] | Review | Primary, general healthcare | Parental consent laws for oral health | Adolescents | Barriers to quality care for adolescents are related to variation and lack of clarity in state laws, a strict opt-in approach to obtaining parental consent, and lack of evidence-based approach to determine adolescents’ cognitive ability to consent. |
| Cheak-Zamora et al. (2013) [65] | Quantitative; Cross-sectional | Primary, other healthcare | Youths with and without autism spectrum disorder (n = 19,004) | Youths with and without autism spectrum disorder aged 12–17 | Among youths with an autism spectrum disorder, race/ethnicity and multiple health conditions were associated with not receiving healthcare transitioning services. |
| Bernstein et al. (2016) [66] | Qualitative; Cross-sectional | Primary, other healthcare | Administrators from 6 clinics in 2 states (n = 39) | Pediatrics | Administrators reported that limited time, lack of training and expertise, low caregiver literacy, and lack of shared medical and dental electronic records inhibited cooperation for quality oral healthcare |
| Kaplan (2010) [67] | Review | Primary, general healthcare | Not applicable | Adolescents | Low utilization of preventive and acute services, inadequate or no health insurance, behavioral issues, financial barriers, and parental perspectives about vaccines are associated with vaccination uptake. |
| Deutsch & Fortin (2015) [68] | Review | Primary, general healthcare | Not applicable | Children in foster care | Children in foster care experience barriers to receiving quality care related to factors precipitating their removal from care, including chronic neglect of their physical health, mental health, and developmental needs. |
| Keeton & Chen (2010) [69] | Review | Primary, general healthcare | Not applicable | Adolescents | Barriers to immunizations include infrequent preventive visits, incomplete records, lack of awareness about the risk of serious infectious diseases, and lack of coverage for adolescent vaccination |
| Ecological Level | Themes | Subtheme | Number of Articles |
|---|---|---|---|
| Individual | Diversity | 10 | |
| LGBTQ | 3 | ||
| Race | 7 | ||
| Navigation | 9 | ||
| Socioeconomic status | 6 | ||
| Behavioral health | 5 | ||
| Experiences/knowledge/belief | 18 | ||
| Interpersonal | Lack of youth-friendly services | Patient–provider relationship | 8 |
| Cultural/linguistic barriers | 10 | ||
| Organizational | Healthcare system/structural barriers | 32 | |
| Financial | Cost of care | 18 | |
| Lack of youth-friendly services | 12 | ||
| Confidentiality/trust | 8 | ||
| Physical space | 4 | ||
| Community | Stigma | 8 | |
| Transportation | 7 | ||
| Policy | Lack of youth-friendly services | Parent consent policy | 4 |
| Financial | Health insurance | 20 |
| Ecological Level | Themes | Number of Articles |
|---|---|---|
| Organizational | Changes to the Healthcare system | 16 |
| Organizational | Outreach | 8 |
| Organizational | Youth-friendly services | 3 |
| Organizational | Cost | 2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garney, W.; Wilson, K.; Ajayi, K.V.; Panjwani, S.; Love, S.M.; Flores, S.; Garcia, K.; Esquivel, C. Social-Ecological Barriers to Access to Healthcare for Adolescents: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 4138. https://doi.org/10.3390/ijerph18084138
Garney W, Wilson K, Ajayi KV, Panjwani S, Love SM, Flores S, Garcia K, Esquivel C. Social-Ecological Barriers to Access to Healthcare for Adolescents: A Scoping Review. International Journal of Environmental Research and Public Health. 2021; 18(8):4138. https://doi.org/10.3390/ijerph18084138
Chicago/Turabian StyleGarney, Whitney, Kelly Wilson, Kobi V. Ajayi, Sonya Panjwani, Skylar M. Love, Sara Flores, Kristen Garcia, and Christi Esquivel. 2021. "Social-Ecological Barriers to Access to Healthcare for Adolescents: A Scoping Review" International Journal of Environmental Research and Public Health 18, no. 8: 4138. https://doi.org/10.3390/ijerph18084138
APA StyleGarney, W., Wilson, K., Ajayi, K. V., Panjwani, S., Love, S. M., Flores, S., Garcia, K., & Esquivel, C. (2021). Social-Ecological Barriers to Access to Healthcare for Adolescents: A Scoping Review. International Journal of Environmental Research and Public Health, 18(8), 4138. https://doi.org/10.3390/ijerph18084138








