Co-Creating and Evaluating an App-Based Well-Being Intervention: The HOW (Healthier Outcomes at Work) Social Work Project
Abstract
1. Introduction
1.1. Stress and Health
1.2. Working Conditions and Stress
1.3. Child and Family Social Workers
1.4. Aim and Research Questions
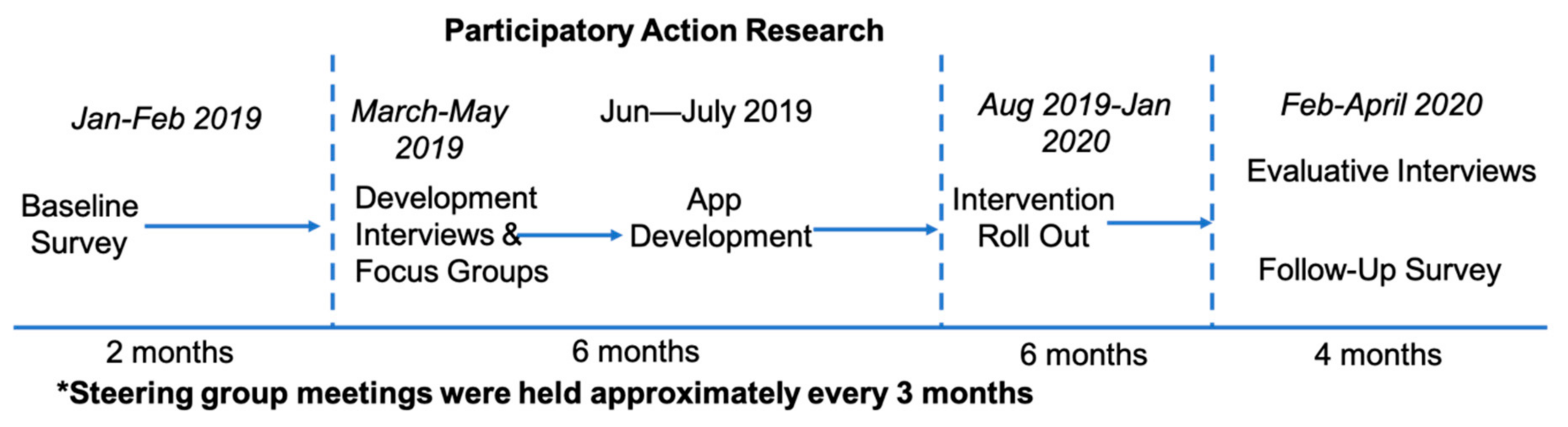
2. Methods
2.1. Design
2.2. Methods and Materials
2.2.1. Qualitative Materials
2.2.2. Instruments and Scales
2.3. Analytical Approach
3. Results
3.1. Intervention Development: Semi-Structured Interviews and Focus Groups
3.2. App/Intervention Contents
3.3. Intervention Implementation
3.4. Interventional Evaluation
3.4.1. Pre- and Post-Surveys
3.4.2. Evaluative Interviews: Working Well
3.4.3. Needing Improvement
4. Discussion
4.1. Findings
4.2. Limitations and Strengths
4.3. Future Research
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ravalier, J.M.; McFadden, P.; Boichat, C.; Clabburn, O.; Moriarty, J. Social worker well-being: A large mixed-methods study. Br. J. Soc. Work 2020. [Google Scholar] [CrossRef]
- Chartered Institute of Personnel Development. Health and Well-Being at Work. Survey Report. Available online: https://www.cipd.co.uk/Images/health-and-well-being-at-work_tcm18-40863.pdf (accessed on 18 July 2019).
- Health and Safety Executive. Work-Related Stress, Anxiety or Depression Statistics in Great Britain. 2019. Available online: https://www.hse.gov.uk/statistics/causdis/stress.pdf (accessed on 10 October 2020).
- Lloyd, C.; King, R.; Chenoweth, L. Social work, stress and burnout: A review. J. Ment. Health 2002, 11, 255–265. [Google Scholar] [CrossRef]
- Ravalier, J.M. Psycho-social working conditions and stress in UK social workers. Br. J. Soc. Work 2019, 49, 371–390. [Google Scholar] [CrossRef]
- West, M.; Dawson, J.F. Employee Engagement and NHS Performance. Available online: https://www.kingsfund.org.uk/sites/default/files/employee-engagement-nhs-performance-west-dawson-leadership-review2012-paper.pdf (accessed on 27 April 2020).
- Department of Health and Social Care, COVID-19: Action Plan for Adult Social Care. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/879639/covid-19-adult-social-care-action-plan.pdf (accessed on 24 April 2020).
- World Health Organization. Mental Health and Psychosocial Considerations during the COVID-19 Outbreak. Available online: https://apps.who.int/iris/bitstream/handle/10665/331490/WHO-2019-nCoV-MentalHealth-2020.1-eng.pdf (accessed on 24 April 2020).
- Huxley, P.; Mohamed, H.; Korer, J.; Jacob, C.; Raval, H.; Anthony, P. Psychiatric morbidity in clients of social workers: Social outcomes. Soc. Psychiatry Psychiatr. Epidemiol. 1989, 24, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Department of Health and Social Care, Guidance: Health and Wellbeing of the Adult Social Care Workforce. Available online: https://www.gov.uk/government/publications/coronavirus-covid-19-health-and-wellbeing-of-the-adult-social-care-workforce/health-and-wellbeing-of-the-adult-social-care-workforce (accessed on 22 October 2020).
- Hasard, J.; Teoh, K.; Visockaire, D.; Dewe, P.; Cox, T. The cost of work-related stress to society: A systematic review. J. Occup. Health Psychol. 2018, 23, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Niedhammer, I.; Milner, A.; Geoffroy-Perez, B.; Coutrot, T.; LaMontagne, A.D.; Chastang, J.-F. Psychosocial work exposures of the job strain model and cardiovascular mortality in France: Results from the STRESSJM prospective study. Scand. J. Work Environ. Health 2020. [Google Scholar] [CrossRef] [PubMed]
- Backe, E.-M.; Seidler, A.; Latza, U.; Rossnagel, K.; Schumann, B. The role of psychosocial stress at work or the development of Cardiovascular diseases: A systematic review. Int. Arch. Occup. Environ. Health 2012, 85, 67–79. [Google Scholar] [CrossRef]
- Chandola, T.; Brunner, E.; Marmot, M. Chronic stress at work and the metabolic syndrome: Prospective study. BMJ 2006, 332, 521–525. [Google Scholar] [CrossRef]
- Steinhardt, M.A.; Smith Jaggars, S.E.; Faulk, K.E.; Gloria, C.T. Chronic work stress and depressive symptoms: Assessing the mediating role of teacher burnout. Stress Health 2011, 27, 420–429. [Google Scholar] [CrossRef]
- Cooper, C.; Dewe, P. Well-being—Absenteeism, presenteeism, costs and challenges. Occup. Med. 2008, 58, 522–524. [Google Scholar] [CrossRef]
- Hall, L.H.; Johnson, J.; Watt, I.; Tsipa, A.; O’Connor, D. Healthcare staff wellbeing, burnout, and patient safety: A systematic review. PLoS ONE 2016, 11, e0159015. [Google Scholar] [CrossRef] [PubMed]
- Hogh, A.; Hoel, H.; Caneiro, I.G. Bullying and employee turnover among healthcare workers: A three-wave prospective study. J. Nurs. Res. 2011, 19, 742–751. [Google Scholar] [CrossRef] [PubMed]
- Vinnerljung, B.; Hjern, A.; Lindbald, F. Suicide attempts and severe psychiatric morbidity among former child welfare clients—A national cohort study. J. Child Psychol. Psychiatry 2006, 47, 723–733. [Google Scholar] [CrossRef] [PubMed]
- Eklof, M.; Torner, M.; Pousette, A. Organizational and social-psychological conditions in healthcare and their importance for patient and staff safety. A critical incident study among doctors and nurses. Saf. Sci. 2014, 70, 211–221. [Google Scholar] [CrossRef]
- Demerouti, E.; Bakker, A.B.; Nachreiner, F.; Schaufeli, W.B. The job demands-resources model of burnout. J. Appl. Psychol. 2001, 86, 499–512. [Google Scholar] [CrossRef] [PubMed]
- Brauchli, R.; Schaufeli, W.B.; Jenny, G.J.; Fullemann, D.; Bauer, G.F. Disentangling stability and change in job resources, job demands, and employee well-being—A three wave study on the Job-Demands Resources model. J. Vocat. Behav. 2013, 83, 117–129. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E. The job demands-resources model: State of the art. J. Manag. Psychol. 2007, 22, 309–328. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Bakker, A.B.; Van Rhenen, W. How changes in job demands and resources predict burnout, work engagement and sickness absenteeism. J. Organ. Behav. 2009, 30, 893–917. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Bakker, A.B. Job demands, job resources, and their relationship with burnout and engagement: A multi-sample study. J. Organ. Behav. 2004, 25, 293–315. [Google Scholar] [CrossRef]
- Cousins, R.; MacKay, C.J.; Clarke, S.D.; Kelly, C.; Kelley, P.J.; McCaig, R.H. ‘Management Standards’ and work-related stress in the UK: Practical development. Work Stress 2004, 18, 113–136. [Google Scholar] [CrossRef]
- Edwards, J.A.; Webster, S. Psychosocial risk assessment: Measurement invariance of the UK Health and Safety Executive’s Management Standards Indicator Tool across public and private sector organizations. Work Stress 2012, 26, 130–142. [Google Scholar] [CrossRef]
- Houdmont, J. UK police custody officers psychosocial hazard exposures and burnout. Policing 2013, 36, 620–635. [Google Scholar] [CrossRef]
- Ravalier, J.M.; Walsh, J. Working conditions and stress in the English education system. Occup. Med. 2018, 68, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Gilligan, R. Promoting resilience in Child and Family social work: Issues for social work practice, education and policy. Soc. Work Educ. 2004, 23, 93–104. [Google Scholar] [CrossRef]
- Department for Education, Experimental Statistics: Children and Family Social Work Workforce in England, Year Ending 30 September 2018. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/782154/Children_s_social_work_workforce_2018_text.pdf (accessed on 23 October 2019).
- National Institute of Clinical Excellence (NICE). Workplace Interventions that Are Effective for Promoting Mental Wellbeing. Synopsis of the Evidence and Cost Effectiveness; NICE: London, UK, 2006. [Google Scholar]
- Northway, R. Participatory research. Part 1: Key features and underlying philosophy. Int. J. Ther. Rehabil. 2010, 17, 174–179. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Successful Qualitative Research: A Practical Guide for Beginners; Sage: London, UK, 2013. [Google Scholar]
- Ravalier, J.M.; McVicar, A.; Munn-Giddings, C. Appreciative Inquiry for stress management. Qual. Res. Organ. Manag. 2018, 14, 260–279. [Google Scholar] [CrossRef]
- Goldberg, D.; Williams, P. A User’s Guide to the General Health Questionnaire; NFER-Nelson: Windsor, UK, 1988. [Google Scholar]
- Banks, M.H.; Clegg, C.W.; Jackson, P.R.; Kemp, N.J.; Stafford, E.M.; Wall, T.D. The use of the General Health Questionnaire as an indicator of mental health in occupational studies. J. Occup. Organ. Psychol. 1980, 53, 187–194. [Google Scholar] [CrossRef]
- El-Metwally, A.; Javed, S.; Razzak, H.A.; Aldossari, K.K.; Aldiab, A.; Al-Ghamdi, S.H.; Househ, M.; Shubair, M.M.; Al-Zahrini, J.M. The factor structure of the general health questionnaire (GHQ12) in Saudi Arabia. BMC Health Serv. Res. 2018, 18. [Google Scholar] [CrossRef]
- Hansson, J.; Hurtig, A.-K.; Lauritz, L.-E.; Padyab, M. Swedish police officer’s job strain, work-related social support and general mental health. J. Police Crim. Psychol. 2017, 32, 128–137. [Google Scholar] [CrossRef]
- Kazi, A.; Haslam, O. Stress management standards: A warning indicator for employee health. Occup. Med. 2013, 63, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Nowell, L.S.; Norris, J.M.; White, D.E.; Moules, N.J. Thematic analysis: Striving to meet the trustworthiness criteria. Int. J. Qual. Methods 2017, 16, 1609406917733847. [Google Scholar] [CrossRef]
- HSE. Signs of Stress at Work. Available online: https://www.hse.gov.uk/stress/signs.htm (accessed on 18 November 2020).
- Guest, G.; Bunce, A.; Johnson, L. How many interviews are enough? An experiment with data saturation and variability. Field Methods 2006, 18, 59–82. [Google Scholar] [CrossRef]
- Van Daele, T.; Hermans, D.; Van Audenhove, C.; Van den Bergh, O. Stress reduction through psychoeducation: A meta-analytic review. Health Educ. Behav. 2011, 39, 474–485. [Google Scholar] [CrossRef] [PubMed]
- Choi, G.-Y. Organizational impacts on the secondary traumatic stress of social workers assisting violence or sexual assault survivors. Adm. Soc. Work 2011, 35, 225–242. [Google Scholar] [CrossRef]
- Rinaldi, M.; Perkins, R. Vocational rehabilitation. Psychiatry 2004, 3, 54–56. [Google Scholar] [CrossRef]
- Wynne-Jones, G.; Artus, M.; Bishop, A.; Lawton, S.A.; Lewis, M.; Jowett, S.; Kigozi, J.; Sowden, G.; Wathall, S.; Burton, A.K.; et al. Effectiveness and costs of a vocational advice service to improve work outcomes in patients with musculoskeletal pain in primary care: A cluster randomised trial (SWAP trial). Pain 2018, 159, 128–138. [Google Scholar] [CrossRef]
- Dwyer, S.C.; Buckle, J.L. The space between: On being an insider-outsider in qualitative research. Int. J. Qual. Methods 2009, 8, 54–63. [Google Scholar] [CrossRef]
| Variable | Baseline or Follow-Up | Mean (SD) | Percentile |
|---|---|---|---|
| MSIT | Time 1 Baseline | 3.66 (0.55) | 50th |
| Time 2 Follow-up aware of HOW-APP | 3.88 (0.45) | 95th | |
| Time 2 Follow-up not aware of HOW-APP | 3.70 (0.52) | 50th | |
| Demands | Baseline | 3.17 (0.85) | 10th |
| Follow-up aware of HOW-APP | 3.49 (0.78) | 50th | |
| Follow-up not aware of HOW-APP | 3.21 (0.88) | 10th | |
| Control | Baseline | 3.48 (0.70) | 50th |
| Follow-up aware of HOW-APP | 3.66 (0.63) | 75th | |
| Follow-up not aware of HOW-APP | 3.46 (0.70) | 50th | |
| Managerial Support | Baseline | 3.72 (0.85) | 75th |
| Follow-up aware of HOW-APP | 4.02 (0.72) | 95th | |
| Follow-up not aware of HOW-APP | 3.89 (0.70) | 95th | |
| Peer Support | Baseline | 4.04 (0.63) | 95th |
| Follow-up aware of HOW-APP | 4.17 (0.49) | 95th | |
| Follow-up not aware of HOW-APP | 4.08 (0.59) | 95th | |
| Relationships | Baseline | 4.39 (0.72) | 50th |
| Follow-up aware of HOW-APP | 4.33 (0.88) | 50th | |
| Follow-up not aware of HOW-APP | 4.31 (0.86) | 50th | |
| Role | Baseline | 4.05 (0.70) | 25th |
| Follow-up aware of HOW-APP | 4.27 (0.62) | 75th | |
| Follow-up not aware of HOW-APP | 4.08 (0.64) | 25th | |
| Change | Baseline | 2.92 (0.86) | 25th |
| Follow-up aware of HOW-APP | 3.42 (0.79) | 90th | |
| Follow-up not aware of HOW-APP | 3.04 (0.77) | 50th | |
| GHQ | Baseline | 15.35 (6.45) | N/A |
| Follow-up aware of HOW-APP | 14.43 (6.67) | ||
| Follow-up not aware of HOW-APP | 17.39 (6.81) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ravalier, J.M.; Wainwright, E.; Smyth, N.; Clabburn, O.; Wegrzynek, P.; Loon, M. Co-Creating and Evaluating an App-Based Well-Being Intervention: The HOW (Healthier Outcomes at Work) Social Work Project. Int. J. Environ. Res. Public Health 2020, 17, 8730. https://doi.org/10.3390/ijerph17238730
Ravalier JM, Wainwright E, Smyth N, Clabburn O, Wegrzynek P, Loon M. Co-Creating and Evaluating an App-Based Well-Being Intervention: The HOW (Healthier Outcomes at Work) Social Work Project. International Journal of Environmental Research and Public Health. 2020; 17(23):8730. https://doi.org/10.3390/ijerph17238730
Chicago/Turabian StyleRavalier, Jermaine M, Elaine Wainwright, Nina Smyth, Oliver Clabburn, Paulina Wegrzynek, and Mark Loon. 2020. "Co-Creating and Evaluating an App-Based Well-Being Intervention: The HOW (Healthier Outcomes at Work) Social Work Project" International Journal of Environmental Research and Public Health 17, no. 23: 8730. https://doi.org/10.3390/ijerph17238730
APA StyleRavalier, J. M., Wainwright, E., Smyth, N., Clabburn, O., Wegrzynek, P., & Loon, M. (2020). Co-Creating and Evaluating an App-Based Well-Being Intervention: The HOW (Healthier Outcomes at Work) Social Work Project. International Journal of Environmental Research and Public Health, 17(23), 8730. https://doi.org/10.3390/ijerph17238730





