Sex-Specific Differences in Hospital Transfers of Nursing Home Residents: Results from the HOspitalizations and eMERgency Department Visits of Nursing Home Residents (HOMERN) Project
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection and Assessed Variables
2.3. Statistical Analyses
3. Results
3.1. Characteristics of Transferred Nursing Home Residents
3.2. Description of Unplanned Hospital Transfers
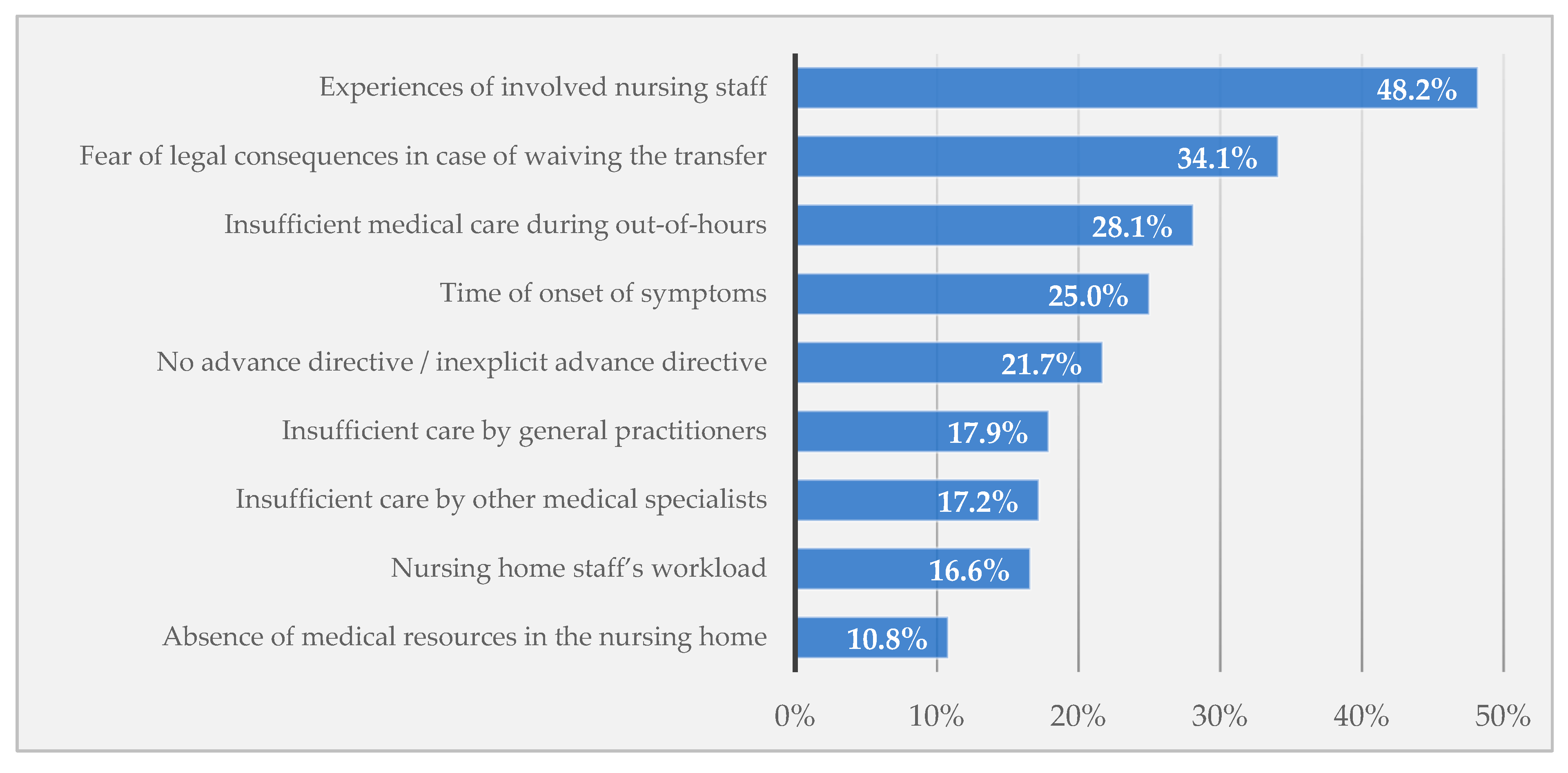
3.3. Nursing Home Staff’s Perceptions on Unplanned Hospital Transfers
4. Discussion
4.1. Comparison of Findings with the Literature
4.2. Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations:
| ACP | advance care planning |
| BI | Barthel Index |
| ED | emergency department |
| GP | general practitioner |
| NH | nursing home |
| ICD-10-GM | German modification of the International Classification of Diseases, 10th Revision |
| PALMA | patient directive for life sustaining measures |
| SAPV | specialized outpatient palliative care |
References
- Eurostat—Statistics Explained Increase in the Share of the Population Aged 65 Years or over between 2007 and 2017. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Population_structure_and_ageing#The_share_of_elderly_people_continues_to_increase (accessed on 4 April 2019).
- Hoffmann, F.; Boeschen, D.; Dörks, M.; Herget-Rosenthal, S.; Petersen, J.; Schmiemann, G. Renal insufficiency and medication in nursing home residents—A cross-sectional study (IMREN). Dtsch. Arztebl. Int. 2016, 113, 92–98. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gordon, A.L.; Franklin, M.; Bradshaw, L.; Logan, P.; Elliott, R.; Gladman, J.R.F. Health status of UK care home residents: A cohort study. Age Ageing 2014, 43, 97–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fassmer, A.M.; Hoffmann, F. Acute health care services use among nursing home residents in Germany: A comparative analysis of out-of-hours medical care, emergency department visits and acute hospital admissions. Aging Clin. Exp. Res. 2019. [Google Scholar] [CrossRef] [PubMed]
- Graverholt, B.; Riise, T.; Jamtvedt, G.; Ranhoff, A.H.; Krüger, K.; Nortvedt, M.W. Acute hospital admissions among nursing home residents: A population-based observational study. BMC Health Serv. Res. 2011, 11, 126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ouslander, J.G.; Lamb, G.; Perloe, M.; Givens, J.H.; Kluge, L.; Rutland, T.; Atherly, A.; Saliba, D. Potentially Avoidable Hospitalizations of Nursing Home Residents: Frequency, Causes, and Costs. J. Am. Geriatr. Soc. 2010, 58, 627–635. [Google Scholar] [CrossRef] [PubMed]
- Kada, O.; Janig, H.; Likar, R.; Cernic, K.; Pinter, G. Reducing Avoidable Hospital Transfers from Nursing Homes in Austria: Project Outline and Baseline Results. Gerontol. Geriatr. Med. 2017, 3, 2333721417696671. [Google Scholar] [CrossRef]
- Lemoyne, S.E.; Herbots, H.H.; De Blick, D.; Remmen, R.; Monsieurs, K.G.; Van Bogaert, P. Appropriateness of transferring nursing home residents to emergency departments: A systematic review. BMC Geriatr. 2019, 19, 17. [Google Scholar] [CrossRef] [Green Version]
- Renom-Guiteras, A.; Uhrenfeldt, L.; Meyer, G.; Mann, E. Assessment tools for determining appropriateness of admission to acute care of persons transferred from long-term care facilities: A systematic review. BMC Geriatr. 2014, 14, 80. [Google Scholar] [CrossRef]
- Allers, K.; Hoffmann, F.; Schnakenberg, R. Hospitalizations of nursing home residents at the end of life: A systematic review. Palliat. Med. 2019, 33, 1282–1298. [Google Scholar] [CrossRef] [Green Version]
- Brucksch, A.; Hoffmann, F.; Allers, K. Age and sex differences in emergency department visits of nursing home residents: A systematic review. BMC Geriatr. 2018, 18, 151. [Google Scholar] [CrossRef]
- Hoffmann, F.; Allers, K. Age and sex differences in hospitalisation of nursing home residents: A systematic review. BMJ Open 2016, 6, e011912. [Google Scholar] [CrossRef]
- Grabowski, D.C.; Stewart, K.A.; Broderick, S.M.; Coots, L.A. Predictors of nursing home hospitalization: A review of the literature. Med. Care Res. Rev. 2008, 65, 3–39. [Google Scholar] [CrossRef]
- Ronald, L.A.; McGregor, M.J.; McGrail, K.M.; Tate, R.B.; Broemling, A.-M. Hospitalization rates of nursing home residents and community-dwelling seniors in British Columbia. Can. J. Aging 2008, 27, 109–115. [Google Scholar] [CrossRef]
- Stall, N.M.; Fischer, H.D.; Fung, K.; Giannakeas, V.; Bronskill, S.E.; Austin, P.C.; Matlow, J.N.; Quinn, K.L.; Mitchell, S.L.; Bell, C.M.; et al. Sex-Specific Differences in End-of-Life Burdensome Interventions and Antibiotic Therapy in Nursing Home Residents with Advanced Dementia. JAMA Netw. Open 2019, 2, e199557. [Google Scholar] [CrossRef]
- Dobalian, A. Nursing Facility Compliance with Do-Not-Hospitalize Orders. Gerontologist 2004, 44, 159–165. [Google Scholar] [CrossRef] [Green Version]
- Sommer, S.; Marckmann, G.; Pentzek, M.; Wegscheider, K.; Abholz, H.-H.; in der Schmitten, J. Advance directives in nursing homes: Prevalence, validity, significance, and nursing staff adherence. Dtsch. Arztebl. Int. 2012, 109, 577–583. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Urotoday Int. J. 2009, 2. [Google Scholar] [CrossRef] [Green Version]
- Unroe, K.T.; Hickman, S.E.; Carnahan, J.L.; Hass, Z.; Sachs, G.; Arling, G. Investigating the Avoidability of Hospitalizations of Long Stay Nursing Home Residents: Opportunities for Improvement. Innov. Aging 2018, 2, igy017. [Google Scholar] [CrossRef] [Green Version]
- Arendts, G.; Quine, S.; Howard, K. Decision to transfer to an emergency department from residential aged care: A systematic review of qualitative research. Geriatr. Gerontol. Int. 2013, 13, 825–833. [Google Scholar] [CrossRef]
- Laging, B.; Ford, R.; Bauer, M.; Nay, R. A meta-synthesis of factors influencing nursing home staff decisions to transfer residents to hospital. J. Adv. Nurs. 2015, 71, 2224–2236. [Google Scholar] [CrossRef]
- O’Neill, B.; Parkinson, L.; Dwyer, T.; Reid-Searl, K. Nursing home nurses’ perceptions of emergency transfers from nursing homes to hospital: A review of qualitative studies using systematic methods. Geriatr. Nurs. 2015, 36, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.; Vanclay, F.; Cooper, B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J. Clin. Epidemiol. 1989, 42, 703–709. [Google Scholar] [CrossRef]
- Nadash, P.; Doty, P.; Von Schwanenflügel, M. The German Long-Term Care Insurance Program: Evolution and Recent Developments. Gerontologist 2018, 58, 588–597. [Google Scholar] [CrossRef]
- White, N.; Kupeli, N.; Vickerstaff, V.; Stone, P. How accurate is the “Surprise Question” at identifying patients at the end of life? A systematic review and meta-analysis. BMC Med. 2017, 15, 139. [Google Scholar] [CrossRef]
- Gerth, M.; Schäufele, M.; Mohr, M.; Laufenberg-Feldmann, R.; Reinholz, U.; Weber, M.; Paul, N. Notfallsituationen und Patientenverfügungen aus der Sicht des Palliativpatienten—Ergebnisse einer Befragung. Z. für Palliativmedizin 2012, 13, 91–96. [Google Scholar] [CrossRef]
- Allers, K.; Fassmer, A.M.; Spreckelsen, O.; Hoffmann, F. End-of-life care of nursing home residents: A survey among general practitioners in northwestern Germany. Geriatr. Gerontol. Int. 2020, 20, 25–30. [Google Scholar] [CrossRef] [Green Version]
- Strautmann, A.; Allers, K.; Fassmer, A.M.; Hoffmann, F. Nursing home staff’s perspective on end-of-life care of German nursing home residents: A cross-sectional survey. BMC Palliat. Care 2020, 19, 2. [Google Scholar] [CrossRef] [Green Version]
- Brinkman-Stoppelenburg, A.; Rietjens, J.A.; van der Heide, A. The effects of advance care planning on end-of-life care: A systematic review. Palliat. Med. 2014, 28, 1000–1025. [Google Scholar] [CrossRef]
- in der Schmitten, J.; Lex, K.; Mellert, C.; RothÄrmel, S.; Wegscheider, K.; Marckmann, G. Patientenverfügungsprogramm: Implementierung in Senioreneinrichtungen. Dtsch. Arztebl. Int. 2014, 111, 50–57. [Google Scholar] [CrossRef] [Green Version]
- Ramroth, H.; Specht-Leible, N.; Brenner, H. Hospitalisations before and after nursing home admission: A retrospective cohort study from Germany. Age Ageing 2005, 34, 291–294. [Google Scholar] [CrossRef] [Green Version]
- Sharma, R.K.; Prigerson, H.G.; Penedo, F.J.; Maciejewski, P.K. Male-female patient differences in the association between end-of-life discussions and receipt of intensive care near death. Cancer 2015, 121, 2814–2820. [Google Scholar] [CrossRef] [Green Version]
- McDermott, C.L.; Fedorenko, C.; Kreizenbeck, K.; Sun, Q.; Smith, B.; Curtis, J.R.; Conklin, T.; Ramsey, S.D. End-of-Life Services Among Patients with Cancer: Evidence from Cancer Registry Records Linked with Commercial Health Insurance Claims. J. Oncol. Pract. 2017, 13, e889–e899. [Google Scholar] [CrossRef]
- Ness, J.; Ahmed, A.; Aronow, W.S. Demographics and payment characteristics of nursing home residents in the United States: A 23-year trend. J. Gerontol. A Biol. Sci. Med. Sci. 2004, 59, 1213–1217. [Google Scholar] [CrossRef] [Green Version]
- Chapman, E.N.; Kaatz, A.; Carnes, M. Physicians and implicit bias: How doctors may unwittingly perpetuate health care disparities. J. Gen. Intern. Med. 2013, 28, 1504–1510. [Google Scholar] [CrossRef] [Green Version]
- Intrator, O.; Zinn, J.; Mor, V. Nursing home characteristics and potentially preventable hospitalizations of long-stay residents. J. Am. Geriatr. Soc. 2004, 52, 1730–1736. [Google Scholar] [CrossRef]
| Total Transfers (n = 535) | Transfers of Females (n = 375) | Transfers of Males (n = 159) | p-Value | ||||
|---|---|---|---|---|---|---|---|
| Age of the residents at time of hospital transfer (years) * | |||||||
| Mean (SD) | 83.8 | (9.3) | 84.7 | (8.8) | 81.7 | (10.1) | |
| ≤69 | 42 | (7.9%) | 22 | (5.9%) | 20 | (12.7) | 0.0033 |
| 70–79 | 95 | (17.9) | 56 | (15.1) | 38 | (24.1) | |
| 80–89 | 252 | (47.5) | 188 | (50.5) | 64 | (40.5) | |
| ≥90 | 142 | (26.7) | 106 | (28.5) | 36 | (22.8) | |
| Marital status of the residents * | |||||||
| Single | 47 | (9.0%) | 32 | (8.7%) | 15 | (9.7%) | <0.0001 |
| Married/in a relationship | 95 | (18.2) | 44 | (12.0% | 50 | (32.5) | |
| Divorced/permanently separated | 48 | (9.2%) | 26 | (7.1%) | 22 | (14.3) | |
| Widowed | 333 | (63.7) | 266 | (72.3) | 67 | (43.5) | |
| Care grade of the residents * | |||||||
| 1 or 2 (few or significant limitations on independence or skills) | 108 | (20.6) | 88 | (23.9) | 20 | (12.9) | 0.0030 |
| 3 (severe limitations on independence or skills) | 173 | (33.0) | 121 | (32.9) | 52 | (33.6) | |
| 4 (extremely severe limitations on independence or skills) | 167 | (31.9) | 101 | (27.5) | 65 | (41.9) | |
| 5 (extremely severe limitations on independence or skills with special demands on care provision) | 76 | (14.5) | 58 | (15.8) | 18 | (11.6) | |
| Dementia diagnosis of the residents * | |||||||
| No | 259 | (48.7) | 178 | (47.6) | 80 | (51.0) | 0.4969 |
| Yes | 273 | (51.3) | 196 | (52.4) | 77 | (49.0) | |
| Stage: mild | 44 | (16.6) | 31 | (16.4) | 13 | (17.1) | 0.0529 |
| Stage: moderate | 124 | (46.8) | 97 | (51.3) | 27 | (35.5) | |
| Stage: severe | 97 | (36.6) | 61 | (32.3) | 36 | (47.4) | |
| Barthel Index: residents’ activities of daily living (points, ICD-10-GM) * | |||||||
| Mean (SD) | 43.4 | (24.9) | 44.6 | (24.5) | 40.9 | (25.5) | |
| 80–100: U50.0/1 (slight/no dependency) | 43 | (8.3%) | 29 | (8.0%) | 14 | (9.2%) | 0.1356 |
| 60–75: U50.2 (mild dependency) | 123 | (23.8) | 98 | (27.0) | 25 | (16.3) | |
| 40–55: U50.3 (moderate dependency) | 141 | (27.3) | 97 | (26.7) | 44 | (28.8) | |
| 20–35: U50.4 (severe dependency) | 105 | (20.3) | 70 | (19.3) | 35 | (22.9) | |
| 0–15: U50.5 (total dependency) | 105 | (20.3) | 69 | (19.0) | 35 | (22.9) | |
| Resident’s wish for end-of-life care * | |||||||
| Unknown | 282 | (53.1) | 191 | (51.3) | 92 | (58.2) | 0.2469 |
| Advance directive available | 249 | (46.9) | 181 | (48.7) | 66 | (41.8) | |
| Full clinical emergency treatment | 9 | (3.7%) | 9 | (5.1%) | 0 | (0.0%) | 0.0338 |
| Limited clinical treatment | 162 | (66.9) | 120 | (67.8) | 41 | (64.1) | |
| Preclinical emergency treatment in the NH | 41 | (16.9) | 22 | (12.4) | 19 | (29.7) | |
| Assessment not possible | 30 | (12.4) | 26 | (14.7) | 4 | (6.3%) | |
| Surprise question (estimating 6-month mortality) * | |||||||
| Likely | 222 | (42.5) | 140 | (38.2) | 82 | (52.9) | 0.0052 |
| Unlikely | 301 | (57.6) | 227 | (61.9) | 73 | (47.1) | |
| Total Transfers (n = 535) | Transfers of Females (n = 375) | Transfers of Males (n = 159) | p-Value | ||||
|---|---|---|---|---|---|---|---|
| Weekday of the hospital transfer * | |||||||
| Monday to Friday | 404 | (75.7%) | 283 | (75.5%) | 120 | (76.0%) | 0.9649 |
| Saturday and Sunday | 130 | (24.3%) | 92 | (24.5%) | 38 | (24.1%) | |
| Outcome of the hospital transfer * | |||||||
| ED visit with discharge to the NH | 195 | (36.9%) | 129 | (34.8%) | 66 | (42.0%) | 0.0937 |
| Hospital admission | 334 | (63.1%) | 242 | (65.2%) | 91 | (58.0%) | |
| Died during hospitalization | 42 | (12.6%) | 28 | (11.6%) | 14 | (15.4%) | 0.3505 |
| Length of hospitalization (days) *,# | |||||||
| Mean (SD) | 8.4 | (7.8) | 8.1 | (7.0) | 9.2 | (9.7) | |
| 1–4 | 95 | (31.4%) | 71 | (32.3%) | 23 | (28.1%) | 0.8045 |
| 5–9 | 123 | (40.6%) | 89 | (40.5%) | 34 | (41.5%) | |
| 10+ | 85 | (28.1%) | 60 | (27.3%) | 25 | (30.5%) | |
| Reason for hospital transfer * | |||||||
| Deterioration of health status (e.g., fever, infection, dyspnea, exsiccosis) | 188 | (35.1%) | 128 | (34.1%) | 60 | (37.7%) | <0.0001 |
| Fall, accident, injury | 179 | (33.5%) | 143 | (38.1%) | 36 | (22.6%) | |
| Psychiatric/neurologic conditions (e.g., challenging behavior, stroke) | 38 | (7.1%) | 21 | (5.6%) | 16 | (10.1%) | |
| Complications with catheter/tube (e.g., blood in urine (hematuria)) | 38 | (7.1%) | 11 | (2.9%) | 27 | (17.0%) | |
| Pain, not fall-induced | 33 | (6.2%) | 27 | (7.2%) | 6 | (3.8%) | |
| Others (e.g., bleedings, gastrointestinal symptoms) | 59 | (11.0%) | 45 | (12.0%) | 14 | (8.8%) | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fassmer, A.M.; Pulst, A.; Schmiemann, G.; Hoffmann, F. Sex-Specific Differences in Hospital Transfers of Nursing Home Residents: Results from the HOspitalizations and eMERgency Department Visits of Nursing Home Residents (HOMERN) Project. Int. J. Environ. Res. Public Health 2020, 17, 3915. https://doi.org/10.3390/ijerph17113915
Fassmer AM, Pulst A, Schmiemann G, Hoffmann F. Sex-Specific Differences in Hospital Transfers of Nursing Home Residents: Results from the HOspitalizations and eMERgency Department Visits of Nursing Home Residents (HOMERN) Project. International Journal of Environmental Research and Public Health. 2020; 17(11):3915. https://doi.org/10.3390/ijerph17113915
Chicago/Turabian StyleFassmer, Alexander Maximilian, Alexandra Pulst, Guido Schmiemann, and Falk Hoffmann. 2020. "Sex-Specific Differences in Hospital Transfers of Nursing Home Residents: Results from the HOspitalizations and eMERgency Department Visits of Nursing Home Residents (HOMERN) Project" International Journal of Environmental Research and Public Health 17, no. 11: 3915. https://doi.org/10.3390/ijerph17113915
APA StyleFassmer, A. M., Pulst, A., Schmiemann, G., & Hoffmann, F. (2020). Sex-Specific Differences in Hospital Transfers of Nursing Home Residents: Results from the HOspitalizations and eMERgency Department Visits of Nursing Home Residents (HOMERN) Project. International Journal of Environmental Research and Public Health, 17(11), 3915. https://doi.org/10.3390/ijerph17113915





