Do Technical Aids for Patient Handling Prevent Musculoskeletal Complaints in Health Care Workers?—A Systematic Review of Intervention Studies
Abstract
1. Introduction
2. Materials and Methods
2.1. Literature Indentification
2.2. Screening
2.3. Data Extraction and Quality Assessment
2.4. Data Synthesis and Evaluation of Evidence
3. Results
3.1. Acute Musculoskeletal Events (Injuries)
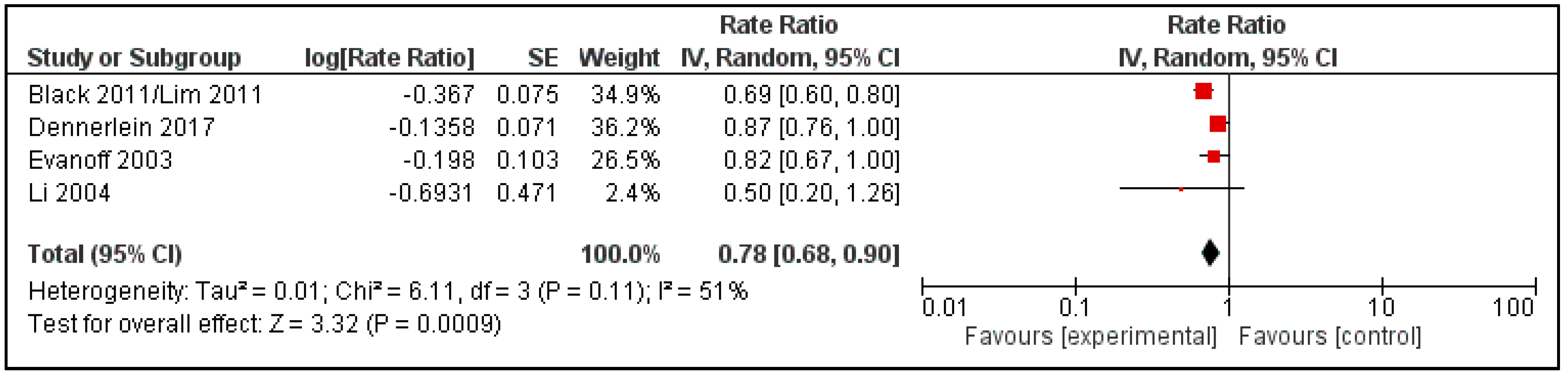
3.1.1. Quantitative Evidence
3.1.2. Repeated Musculoskeletal Injuries
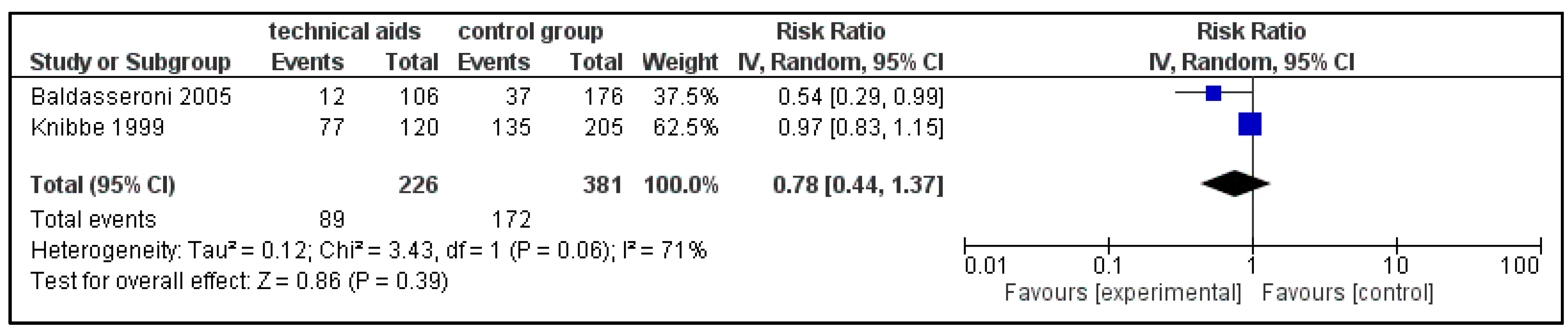
3.2. Back Pain
3.3. Cervical Spine
3.4. Shoulder
3.5. Risk of Bias and GRADE Assessments
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Yassi, A.; Ostry, A.S.; Spiegel, J.; Walsh, G.; de Boer, H.M. A collaborative evidence-based approach to making healthcare a healthier place to work. Hosp. Q. 2002, 5, 70–78. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fragala, G. Striving for zero-lift in healthcare facilities. In Back Injury among Healthcare Workers; CRC Press: Boca Raton, FL, USA, 2003; pp. 53–71. [Google Scholar]
- Maul, I.; Laubli, T.; Klipstein, A.; Krueger, H. Course of low back pain among nurses: A longitudinal study across eight years. Occup. Environ. Med. 2003, 60, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Wasiak, R.; Verma, S.; Pransky, G.; Webster, B. Risk factors for recurrent episodes of care and work disability: Case of low back pain. J. Occup. Environ. Med. 2004, 46, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Bejia, I.; Younes, M.; Jamila, H.B.; Khalfallah, T.; Ben Salem, K.; Touzi, M.; Akrout, M.; Bergaoui, N. Prevalence and factors associated to low back pain among hospital staff. Joint Bone Spine 2005, 72, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Bos, E.; Krol, B.; van der Star, L.; Groothoff, J. Risk factors and musculoskeletal complaints in non-specialized nurses, IC nurses, operation room nurses, and X-ray technologists. Int. Arch. Occup. Environ. Health 2007, 80, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Landry, M.D.; Raman, S.R.; Sulway, C.; Golightly, Y.M.; Hamdan, E. Prevalence and risk factors associated with low back pain among health care providers in a Kuwait hospital. Spine 2008, 33, 539–545. [Google Scholar] [CrossRef] [PubMed]
- Boden, L.I.; Sembajwe, G.; Tveito, T.H.; Hashimoto, D.; Hopcia, K.; Kenwood, C.; Stoddard, A.M.; Sorensen, G. Occupational injuries among nurses and aides in a hospital setting. Am. J. Ind. Med. 2012, 55, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Dennerlein, J.T.; Hopcia, K.; Sembajwe, G.; Kenwood, C.; Stoddard, A.M.; Tveito, T.H.; Hashimoto, D.M.; Sorensen, G. Ergonomic practices within patient care units are associated with musculoskeletal pain and limitations. Am. J. Ind. Med. 2012, 55, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Holtermann, A.; Clausen, T.; Jorgensen, M.B.; Burdorf, A.; Andersen, L.L. Patient handling and risk for developing persistent low-back pain among female healthcare workers. Scand. J. Work Environ. Health 2013, 39, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Bureau of Labor Statistics. Nonfatal Occupational Injuries and Illnesses Requiring Days Away from Work, 2015; US Department of Labor: Washington, DC, USA, 2016.
- Anderson, S.P.; Oakman, J. Allied health professionals and work-related musculoskeletal disorders: A systematic review. Saf. Health Work 2016, 7, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Winkelmolen, G.H.; Landeweerd, J.A.; Drost, M.R. An evaluation of patient lifting techniques. Ergonomics 1994, 37, 921–932. [Google Scholar] [CrossRef] [PubMed]
- Ulin, S.S.; Chaffin, D.B.; Patellos, C.L.; Blitz, S.G.; Emerick, C.A.; Lundy, F.; Misher, L. A biomechanical analysis of methods used for transferring totally dependent patients. SCI Nurs. 1997, 14, 19–27. [Google Scholar] [PubMed]
- National Institute for Occupational Safety and Health. Safe Patient Handling Training for Schools of Nursing; Waters, T.R., Nelson, A., Hughes, N., Menzel, N., Eds.; National Institute for Occupational Safety and Health: Washington, DC, USA, 2009.
- Tinubu, B.M.S.; Mbada, C.E.; Oyeyemi, A.L.; Fabunmi, A.A. Work-related musculoskeletal disorders among nurses in Ibadan, South-West Nigeria: A cross-sectional survey. BMC Musculoskelet. Disord. 2010, 11, 12. [Google Scholar] [CrossRef] [PubMed]
- Trinkoff, A.M.; Lipscomb, J.A.; Geiger-Brown, J.; Brady, B. Musculoskeletal problems of the neck, shoulder, and back and functional consequences in nurses. Am. J. Ind. Med. 2002, 41, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Seidler, A.; Bolm-Audorff, U.; Siol, T.; Henkel, N.; Fuchs, C.; Schug, H.; Leheta, F.; Marquardt, G.; Schmitt, E.; Ulrich, P.T.; et al. Occupational risk factors for symptomatic lumbar disc herniation; a case-control study. Occup. Environ. Med. 2003, 60, 821–830. [Google Scholar] [CrossRef] [PubMed]
- Seidler, A.; Bergmann, A.; Jäger, M.; Ellegast, R.; Ditchen, D.; Elsner, G.; Grifka, J.; Haerting, J.; Hofmann, F.; Linhardt, O.; et al. Cumulative occupational lumbar load and lumbar disc disease—Results of a german multi-center case-control study (EPILIFT). BMC Musculoskelet. Disord. 2009, 10, 48. [Google Scholar] [CrossRef] [PubMed]
- Bergmann, A.; Bolm-Audorff, U.; Ditchen, D.; Ellegast, R.; Grifka, J.; Haerting, J.; Hofmann, F.; Jager, M.; Linhardt, O.; Luttmann, A.; et al. Do occupational risks for low back pain differ from risks for specific lumbar disc diseases?: Results of the german lumbar spine study (EPILIFT). Spine 2017, 42, E1204–E1211. [Google Scholar] [CrossRef] [PubMed]
- Seidler, A.; Bolm-Audorff, U.; Heiskel, H.; Henkel, N.; Roth-Kuver, B.; Kaiser, U.; Bickeboller, R.; Willingstorfer, W.J.; Beck, W.; Elsner, G. The role of cumulative physical work load in lumbar spine disease: Risk factors for lumbar osteochondrosis and spondylosis associated with chronic complaints. Occup. Environ. Med. 2001, 58, 735–746. [Google Scholar] [CrossRef] [PubMed]
- Seidler, A.; Euler, U.; Bolm-Audorff, U.; Ellegast, R.; Grifka, J.; Haerting, J.; Jager, M.; Michaelis, M.; Kuss, O. Physical workload and accelerated occurrence of lumbar spine diseases: Risk and rate advancement periods in a german multicenter case-control study. Scand. J. Work Environ. Health 2011, 37, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Dagenais, S.; Caro, J.; Haldeman, S. A systematic review of low back pain cost of illness studies in the united states and internationally. Spine J. 2008, 8, 8–20. [Google Scholar] [CrossRef] [PubMed]
- Jonsson, E.; Olafsson, G.; Fritzell, P.; Hägg, O.; Borgström, F. Pms88—Productivity loss due to low back pain: Results from Swedish registers. Value Health 2015, 18, A649. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Asche, C.V.; Kirkness, C.S.; McAdam-Marx, C.; Fritz, J.M. The societal costs of low back pain. J. Pain Palliat. Care Pharmacother. 2007, 21, 25–33. [Google Scholar] [PubMed]
- Abenhaim, L.; Rossignol, M.; Gobeille, D.; Bonvalot, Y.; Fines, P.; Scott, S. The prognostic consequences in the making of the initial medical diagnosis of work-related back injuries. Spine 1995, 20, 791–795. [Google Scholar] [CrossRef] [PubMed]
- Frank, J.W.; Brooker, A.-S.; DeMaio, S.E.; Kerr, M.S.; Maetzel, A.; Shannon, H.S.; Sullivan, T.J.; Norman, R.W.; Wells, R.P. Disability resulting from occupational low back pain: Part II: What do we know about secondary prevention? A review of the scientific evidence on prevention after disability begins. Spine 1996, 21, 2918–2929. [Google Scholar] [CrossRef] [PubMed]
- Eurogip. Musculoskeletal Disorders: What Recognition as Occupational Diseases? A Study on 10 European Countries. 2016. Available online: http://www.eurogip.fr/images/pdf/Eurogip120E_ReportMSDs.pdf (accessed on 6 March 2018).
- Seidler, A.L.; Rethberg, C.; Schmitt, J.; Nienhaus, A.; Seidler, A. Health utilities for chronic low back pain. J. Occup. Med. Toxicol. 2017, 12, 28. [Google Scholar] [CrossRef] [PubMed]
- Freiberg, A.; Euler, U.; Girbig, M.; Nienhaus, A.; Freitag, S.; Seidler, A. Does the use of small aids during patient handling activities lead to a decreased occurrence of musculoskeletal complaints and diseases? A systematic review. Int. Arch. Occup. Environ. Health 2016, 89, 547–559. [Google Scholar] [CrossRef] [PubMed]
- Holliday, P.J.; Fernie, G.R.; Plowman, S. The impact of new lifting technology in long term care: A pilot study. AAOHN J. 1994, 42, 582–589. [Google Scholar] [PubMed]
- Laflin, K.; Aja, D. Health care concerns related to lifting: An inside look at intervention strategies. Am. J. Occup. Ther. 1995, 49, 63–72. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Smedley, J.; Egger, P.; Cooper, C.; Coggon, D. Manual handling activities and risk of low back pain in nurses. Occup. Environ. Med. 1995, 52, 160–163. [Google Scholar] [CrossRef] [PubMed]
- Holtermann, A.; Clausen, T.; Jørgensen, M.B.; Aust, B.; Mortensen, O.S.; Burdorf, A.; Fallentin, N.; Andersen, L.L. Does rare use of assistive devices during patient handling increase the risk of low back pain? A prospective cohort study among female healthcare workers. Int. Arch. Occup. Environ. Health 2015, 88, 335–342. [Google Scholar] [CrossRef] [PubMed]
- German Social Accident Insurance Institution for the Health and Welfare Service. Berufsgenossenschaft für Gesundheitsdienst und Wohlfahrtspflege (BGW). (Stronger Back 2017) Starker Rücken 2017. Available online: https://www.bgw-online.de/SharedDocs/Downloads/DE/Medientypen/BGW%20Broschueren/BGW07-00-000_Starker%20R%C3%BCcken_bf_Download.pdf;jsessionid=F11533FF25B625AD0A32C351C433E026?__blob=publicationFile (accessed on 6 March 2018).
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; Wiley: Hoboken, NJ, USA, 2011. [Google Scholar]
- Choi, S.D.; Brings, K. Work-related musculoskeletal risks associated with nurses and nursing assistants handling overweight and obese patients: A literature review. Work 2016, 53, 439–448. [Google Scholar] [CrossRef] [PubMed]
- Dawson, A.P.; McLennan, S.N.; Schiller, S.D.; Jull, G.A.; Hodges, P.W.; Stewart, S. Interventions to prevent back pain and back injury in nurses: A systematic review. Occup. Environ. Med. 2007, 64, 642–650. [Google Scholar] [CrossRef] [PubMed]
- Martimo, K.P.; Verbeek, J.; Karppinen, J.; Furlan, A.D.; Takala, E.P.; Kuijer, P.P.; Jauhiainen, M.; Viikari-Juntura, E. Effect of training and lifting equipment for preventing back pain in lifting and handling: Systematic review. BMJ 2008, 336, 429–431. [Google Scholar] [CrossRef] [PubMed]
- Teeple, E.; Collins, J.E.; Shrestha, S.; Dennerlein, J.T.; Losina, E.; Katz, J.N. Outcomes of safe patient handling and mobilization programs: A meta-analysis. Work 2017, 58, 173–184. [Google Scholar] [CrossRef] [PubMed]
- Tullar, J.M.; Brewer, S.; Amick, B.C.; Irvin, E.; Mahood, Q.; Pompeii, L.A.; Wang, A.; van Eerd, D.; Gimeno, D.; Evanoff, B. Occupational safety and health interventions to reduce musculoskeletal symptoms in the health care sector. J. Occup. Rehabil. 2010, 20, 199–219. [Google Scholar] [CrossRef] [PubMed]
- Verbeek, J.H.; Martimo, K.P.; Karppinen, J.; Kuijer, P.P.; Viikari-Juntura, E.; Takala, E.P. Manual material handling advice and assistive devices for preventing and treating back pain in workers. Cochrane Database Syst. Rev. 2011, CD005958. [Google Scholar] [CrossRef] [PubMed]
- Downs, S.H.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef] [PubMed]
- The Cochrane Collaboration. Review Manager (Revman), 5.3; The Cochrane Collaboration: Copenhagen, Denmark, 2014. [Google Scholar]
- Atkins, D.; Best, D.; Briss, P.A.; Eccles, M.; Falck-Ytter, Y.; Flottorp, S.; Guyatt, G.H.; Harbour, R.T.; Haugh, M.C.; Henry, D.; et al. Grading quality of evidence and strength of recommendations. BMJ 2004, 328, 1490. [Google Scholar] [PubMed]
- Baldasseroni, A.; Abrami, V.; Arcangeli, G.; Cupelli, V.; Fioriti, M.; Guarducci, L.; Sommani, L.; Tartaglia, R. Longitudinal study for assessing the efficacy of preventive measures in a population of health workers exposed to risk in manual patient handling. G. Ital. Med. Lav. Ergon. 2005, 27, 101–105. [Google Scholar] [PubMed]
- Black, T.R.; Shah, S.M.; Busch, A.J.; Metcalfe, J.; Lim, H.J. Effect of transfer, lifting, and repositioning (TLR) injury prevention program on musculoskeletal injury among direct care workers. J. Occup. Environ. Hyg. 2011, 8, 226–235. [Google Scholar] [CrossRef] [PubMed]
- Dennerlein, J.T.; O’Day, E.T.; Mulloy, D.F.; Somerville, J.; Stoddard, A.M.; Kenwood, C.; Teeple, E.; Boden, L.I.; Sorensen, G.; Hashimoto, D. Lifting and exertion injuries decrease after implementation of an integrated hospital-wide safe patient handling and mobilisation programme. Occup. Environ. Med. 2017, 74, 336–343. [Google Scholar] [CrossRef] [PubMed]
- Engst, C.; Chhokar, R.; Miller, A.; Tate, R.B.; Yassi, A. Effectiveness of overhead lifting devices in reducing the risk of injury to care staff in extended care facilities. Ergonomics 2005, 48, 187–199. [Google Scholar] [CrossRef] [PubMed]
- Evanoff, B.; Wolf, L.; Aton, E.; Canos, J.; Collins, J. Reduction in injury rates in nursing personnel through introduction of mechanical lifts in the workplace. Am. J. Ind. Med. 2003, 44, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Fragala, G. Creating safer environments for long-term care staff and residents. Ann. Longterm Care 2012, 20, 42–46. [Google Scholar]
- Knibbe, J.J.; Friele, R.D. The use of logs to assess exposure to manual handling of patients, illustrated in an intervention study in home care nursing. Int. J. Ind. Ergon. 1999, 24, 445–454. [Google Scholar] [CrossRef]
- Li, J.; Wolf, L.; Evanoff, B. Use of mechanical patient lifts decreased musculoskeletal symptoms and injuries among health care workers. Inj. Prev. 2004, 10, 212–216. [Google Scholar] [CrossRef] [PubMed]
- Lim, H.J.; Black, T.R.; Shah, S.M.; Sarker, S.; Metcalfe, J. Evaluating repeated patient handling injuries following the implementation of a multi-factor ergonomic intervention program among health care workers. J. Saf. Res. 2011, 42, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.; Engst, C.; Tate, R.B.; Yassi, A. Evaluation of the effectiveness of portable ceiling lifts in a new long-term care facility. Appl. Ergon. 2006, 37, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Smedley, J.; Trevelyan, F.; Inskip, H.; Buckle, P.; Cooper, C.; Coggon, D. Impact of ergonomic intervention on back pain among nurses. Scand. J. Work Environ. Health 2003, 29, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Yassi, A.; Cooper, J.E.; Tate, R.B.; Gerlach, S.; Muir, M.; Trottier, J.; Massey, K. A randomized controlled trial to prevent patient lift and transfer injuries of health care workers. Spine 2001, 26, 1739–1746. [Google Scholar] [CrossRef] [PubMed]
- GRADEpro GDT. Gradepro Guideline Development Tool (Software), Evidence Prime, Inc., McMaster University: Hamilton, ON, Canada, 2015.

| PICO | Study Inclusion Criteria |
|---|---|
| Participants (P) | Labor force from the field of nursing exerting patient transfers; especially health care workers, therapists (physiotherapists, occupational therapists), as well as volunteer workers from the health care area, and caregiving relatives between the ages of 15 and 70 years. |
| Intervention (I) | Technical patient handling equipment (i.e., nursing beds, low nursing home beds, bed movers, mobile lifts, wall lifts, overhead lifts, ceiling lifts, day care chairs, or mechanical position change aids); as a solitary measure or as part of a multimodal intervention (e.g., combined with education, training, guidance, small assistive devices, etc.). |
| Comparison (C) | Health care and nursing settings lacking technical patient handling equipment. |
| Outcomes (O) | Complaints or disorders (self-reported disorders or pain assessed with any questionnaire e.g., Nordic, Disabilities of the Arm, Shoulder and Hand (DASH), Oswestry), including acute presentations of debilitation and pain ensuing in conjunction with a patient handling maneuver (i.e., injuries), in the (i) lumbar spine area; (ii) cervical spine area; or (iii) shoulder area. |
| Study design | Randomized controlled trials (RCT) and controlled before-after (CBA) studies |
| Study, Year | Study Design (Follow-Up); Setting(s) | Participant Characteristics | Intervention(s) | Comparison | Outcomes | |
|---|---|---|---|---|---|---|
| Baldasseroni 2005 [46] | CBA (1.5 years) five hospitals—Public Health Department Florence, Italy nursing professionals and health care workers involved in patient care | total employed at baseline n = 730 avg. age (at baseline) 38.7 years (±8.0) women 221 (78.1%) intervention group nbaseline = 167 nfollow-up = 136 loss to follow-up = 18.9% response after follow-up n = 106 missing response = 22.1% control group nbaseline = 563 nfollow-up = 297 loss to follow-up = 47.2% response after follow-up n = 176 missing response = 40.7% | total employed at baseline n = 730 avg. age (at baseline) 38.7 years (±8.0) women 221 (78.1%) intervention group nbaseline = 167 nfollow-up = 136 loss to follow-up = 18.9% response after follow-up n = 106 missing response = 22.1% control group nbaseline = 563 nfollow-up = 297 loss to follow-up = 47.2% response after follow-up n = 176 missing response = 40.7% | electromechanical lifts sliding lift sheets height-adjustable stretchers ergonomic lifting belts equipment varied depending on specific needs of the departments equipment was introduced over a 13-month period (between surveys) | no equipment provided | 12-month prevalence of low-back pain (number of episode categories) |
| Black 2011/Lim 2011 [47,54] | CBA (two years) six hospitals in two health regions of Saskatchewan, Canada intervention group: hospital A: large, tertiary hospital with 436 beds hospital B: medium-sized community hospital with 239 beds hospital C: small hospital with long-term care (LTC) facility with 240 residents control group: three hospitals matched to intervention hospitals by hospital types and size | characteristics of injured workers at hospitals A, B, and C (pre-/post-intervention) [47]: intervention group (n = 260/n = 151) avg. age 40.5 years (±10.4)/41.0 years (±10.2) women 236 (91%)/142 (94%) control group (n = 139/n = 165) avg. age 39.2 years (±10.1)/39.1 years (±10.7) women 127 (91%)/161 (94%) employees with a previous patient handling-related injury at hospitals A, B and C (n = 1480) [54]: intervention group (n = 789) avg. age 41.2 years (±10.1) women 734 (93%) control group (n = 691) avg. age 39.3 years (±10.2) women 628 (91%) | Transfer, Lifting, and Repositioning (TLR) program • 2 mechanical lifts distributed to high needs units • eight-hour mandatory educational session (incl. anatomy, injuries, body mechanics, personal health, lifting and patient handling procedures, and patient-handling skills development) + yearly refresher (one hour) + course booklet and training materials program was introduced over a 10 or 12-month period | no injury prevention program, “standard occupational health and safety practice” | back injuries claims neck injury claims shoulder injury claims rate ratios musculoskeletal injury claims, post vs. pre-intervention repeated back injury claims repeated neck injury claims repeated shoulder injury claims odds ratio of repeated musculoskeletal injury claims | |
| Dennerlein 2017 [48] | CBA (one year) two academic hospitals in the metropolitan area of Boston, Massachusetts (one intervention hospital, one control hospital) | random sample of employees in patient care units (with patient care duties) supervised by a nurse manager, employed in 2012, and working more than 20 h per week were surveyed: intervention group randomly selected n = 866 nbaseline = 580 women 528 (93.5%) avg. age 42.7 years (±0.49) nfollow-up = 499 (424 filled out both) response = 67.0% loss to follow-up 26.9% control group a randomly selected n = 1267 nbaseline = 1011 women a (91.4%) avg. age 40.6 years (±0.43) nfollow-up = 971 (785 filled out both) response = 79.8% loss to follow-up 22.4% | hospital-wide safe patient handling and mobilisation program comprising: • investment in ceiling lifts, slings, mechanical sit-to-stand devices, air-assisted lateral transfer devices, mobile lift devices and ceiling lifts in selected units (and no investment in small aids) • patient handling policy • program training (including mobility assessment training) • instructional bedside cards, instructions on mobile equipment, and “decision guides” distribute • new employees trained by a co-worker in a simulation laboratory • implementation of an equipment maintenance plan • information collected in a handbook for each unit • equipment needs assessments • patient mobility needs assessment • internal marketing campaign of the program • patient education material program was introduced over an eight month period | employees of four units in the comparison hospital were offered a well-being intervention unclear amount of technical equipment available (presumably similar to pre-intervention conditions at the intervention hospital) | three-month prevalence of low back pain (NordicQ) three-month prevalence of neck/shoulder pain (NordicQ) three-week intensity of musculoskeletal pain (adapted DASH upper limb score) back injury claim rate ratio (RR, 95% CI), post- vs. pre-intervention neck/shoulder injury claim rate ratio (RR, 95% CI), post- vs. pre-intervention injury claim rate ratio (RR, 95% CI), post- vs. pre-intervention | |
| Engst 2005 [49] | CBA (one year) two 75-bed extended care units of a community hospital in British Columbia, Canada (one intervention unit, one control unit) | aged 19–60+ years sex not reported care aids, licensed practical nurses, registered nurses | • installation of ceiling lift tracks in 75-bed extended care unit • one-hour training session provided by on-site occupational therapist on use and care of ceiling lifts • a “no-unsafe manual lift policy” was developed and implemented ceiling lift renovations and training required six months | 3 mechanical floor lifts, 1 sit-stander) were already available | raw number of claims for “lifting & transferring related injuries” and “repositioning related injuries” | |
| Evanoff 2003 [50] | CBA (2–3 years) 31 intervention nursing units in St. Louis (Missouri), USA b (incl. neurology, orthopedics, intensive care, rehabilitation, general surgery, general medicine) from four acute care hospitals (1 major teaching hospital, 2 large suburban, 1 smaller community hospital) 5 LTC intervention units from 5 facilities in St. Louis (Missouri), USA (included 3 sites in St. Louis + 2 rural sites) | age and sex distribution of intervention and comparison groups not reported nurses, nursing aides, patient care technicians 190 health care workers in interventions units interviewed (with consent) | • 22 stand-up lifts (“EZ-Stand”) and 25 full-body lifts (“EZ-Lift”) distributed among the 36 intervention unit • two-hour hands on instructional course on lift operation Units received either both or only one lift (depending on the unit’s needs) time required to introduce equipment to all units was not reported | compared with injury data from all hospital workers not provided with new technical patient handling equipment at each facility during the same time frame | musculoskeletal injury claims rate ratio (RR, 95% CI), post- vs. pre-intervention | |
| Fragala 2012 [51] | CBA “pilot study” (one year) 2 LTC units of the Radius Mayflower LTC facility in Plymouth (Massachusetts), USA (resident population had high level of dependency) | age and sex distribution of intervention and comparison groups were not reported | “CASE program” c • 4 full sling lifts and 1 stand-assist lift following needs assessment • education and training sessions with vendor demonstration • pre- and post-intervention questionnaire time required to introduce equipment to all units not reported | no equipment provided | raw number of injury claims pre-/post-intervention | |
| Knibbe & Friele 1999 [52] | CBA (one year) 20 teams of home care nurses working in Rotterdam, The Netherlands providing professional nursing care around the clock, seven days/week for patients living at home 8 intervention teams (n = 139) 12 control teams (n = 239) | avg. age 34.6 years (±8.8); range 21–58 years avg. work experience 13.3 years (±8.1); range 1–36 years avg. working hours 26.8 h/week (±11.7); range 2–49 h/week day-shifts 73.3% | • 40 patient hoists provided • training • ergonomic assessment forms • 12 specifically trained ‘lifting coordinators’ program was introduced over a 12-month period | no special equipment provided (two patient hoists already available) | 12-month prevalence of back pain | |
| Li 2004 [53] | CBA (seven months follow-up) three nursing units of a 111 bed community hospital in St. Louis (Missouri), USA (incl. medicine/surgery, intensive care, subacute care units) | health-care workers directly involved with patient handling intervention group 138 health care workers/nurses employed in the three units in 2000 nbaseline = 61 response = 44.2% nfollow-up = 36 loss to follow-up = 41.0% age and sex distribution of intervention and comparison groups not reported | • 1 portable full body sling lift • 2 portable stand-up sling lifts (“EZ-Lift” and “EZ-Stand”) • one time hands-on training sessions offered by hospital personnel at start of intervention equipment was introduced over a six month period | compared with injury data from units not provided with new technical patient handling equipment during the same time frame (mechanical lifts were not available) | musculoskeletal injury claim rate ratio (RR, 95% CI), post- vs. pre-intervention | |
| Miller 2006 [55] | CBA (1 year) 2 LTC facilities in Vancouver (British Columbia), Canada intervention: 63-bed LTC facility (moved into newly constructed facility on same property on 1 August 2002) control: 100-bed LTC facility with similar patients and managed by the same organization | intervention (n = 45) responded to survey n = 17 women 94.1% age distribution 19–29 years 0% 30–39 years 41.2% 40–49 years 35.3% 50–59 years 11.8% 60+ years 5.9% missing: 5.9% control (n = 29) responded to survey n = 15 women 100% age distribution 19–29 years 0% 30–39 years 33.3% 40–49 years 46.7% 50–59 years 13.3% 60+ years 0% missing 6.7% | • ceiling lift tracking from beds to washrooms installed in all rooms; 6 portable ceiling lift motors purchased; 4 portable motors were purchased eight months post-intervention • one-hour training session with vendor demonstration on how to lift, transferring and repositioning patients one day was needed to move to the newly constructed facility | no ceiling-lift tracking both the intervention and control facilities had 4 mechanical lifts prior to and during the intervention | raw number of injury claims pre-/post intervention | |
| Smedley 2003 [56] | CBA (4–14 months d) 2 National Health Service (NHS) hospitals in Southern England, UK providing acute medical and surgical services | baseline questionnaire e intervention (n = 817) response rate 54% age distribution <30 years 20% 30–39 years 36% 40–49 years 25% ≥50 years 19% part-time 45%/full-time 55% control group (n = 340) response rate 61% age distribution <30 years 20% 30–39 years 29% 40–49 years 30% ≥50 years 21% part-time 51%/full-time 49% | • manual-handling policy revised to “minimize unassisted patient handling and exposure to high-risk nursing tasks” • organizational engagement incl. managers from every level • 700 new sliding sheets for all wards • lifting and handling equipment, (incl. height adjustable baths, hoists, transfer belts, and sliding sheets) distributed to selected departments • “link nurses”-network: contact persons on ward; disseminates information to wards; responsible for equipment • two-day training course in health and safety offered; incl. basic aspects of manual handlingprogram was introduced over a ten month period. | “Limited” steps to improve manual-handling training and use of patient-handling equipment was initiated by the control hospital management during the study period. | one-month prevalence of low back pain | |
| Yassi 2001 [57] | 3-arm cluster RCT (one year) Winnipeg’s Health Sciences Centre in Winnipeg (Manitoba), Canada, an acute and tertiary care hospital nine units from medical, surgical, and rehabilitation service areas (three units/area) with high risk for musculoskeletal injury, similar patients, personnel, and size • each unit of a service area randomized to a study-arm • units were physically separate | 346 nurses and unit assistants arm A n = 103/followed n = 82 (80%) arm B n = 116/followed n = 85 (73%) arm C n = 127/followed n = 94 (74%) age and sex distribution not reported | “Safe lifting” (Arm B) biomechanical strain reduced with small aids (e.g., transfer belts and slide devices) • 1 mechanical total body lift/unit • Transfer belt in each room • 2 large & 4 small sliding devices/unit “no strenuous lift” (Arm C) eliminate/reduce patient transfers with help from technical devices • mechanical total body lifts f • sit-stand lifts f • 1 large & 2 small sliding devices/roomboth arms received: • 3-h hands-on education: back care, patient assessment, transfer techniques, use of transfer aid equipment time required to introduce the program was not reported | “Usual practice” (Arm A) • biomechanics & lifting techniques training on request • training for equipment already in use • 1 mechanical total body lift/ward • sliding devices (on request) | musculoskeletal injury claim rate per 100,000 paid h one-week prevalence of work-related low-back pain ratings Oswestry back disability scores one-week prevalence of work-related shoulder pain ratings DASH upper limb score (includes arm, shoulder, and hand) |
| Outcomes | No. of Participants (Studies) Follow-Up | Certainty of the Evidence (GRADE) | Relative Effect (95% CI) | Anticipated Absolute Effects | |
|---|---|---|---|---|---|
| Risk with Few or no Patient Transferring Aids | Risk Difference with Technical Aids (Range Based on 95% CI) | ||||
| musculoskeletal injuries (no site differentiation) assessed with: claims data follow up: range 1 to 2 years | NR (4 observational studies) | ⨁◯◯◯ VERY LOW a | RR 0.78 (0.68 to 0.90) | Not computable due to unreported number of workers at risk in the studies | |
| 12-month prevalence of (low-)back pain assessed with: post-intervention RR follow up: range 1 to 2 years | 607 (2 observational studies) | ⨁◯◯◯ VERY LOW b,c | RR 0.78 (0.44 to 1.37) | 45 per 100 | 10 fewer per 100 (25 fewer to 17 more) |
| repeated musculoskeletal injuries assessed with: claims follow up: 2 years | 1480 (1 observational study) | ⨁◯◯◯ VERY LOW a | OR 0.62 (0.27 to 0.81) | 22 per 100 | 7 fewer per 100 (15 fewer to 3 fewer) |
| cervical spine (neck) injuries assessed with: injury claims follow up: range 1 to 2 years | 1786 (2 observational study) | ⨁◯◯◯ VERY LOW a | One study found the percentage of injury claims involving the neck increased post-intervention in both the group receiving the intervention as well as the control group. The other study found the a nearly statistically significant protective post-intervention RR for neck/shoulder injury claims | ||
| shoulder pain assessed with: 1-week shoulder pain rating follow up: 1 year | 261 (1 RCT) | ⨁⨁◯◯ LOW d | The RCT reported a reduction in 1-week shoulder pain ratings at the 6- and 12-month follow-ups in the intervention group receiving technical aids to prevent strenuous lifting. A similar reduction in pain rating was not observed in the control group or in the second intervention arm receiving primarily small aids. Although the 1-week prevalence of work-related shoulder pain at the 6- and 12-month follow-ups was significantly lower in the second intervention arm receiving primarily small aids | ||
| The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; NR: not reported | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hegewald, J.; Berge, W.; Heinrich, P.; Staudte, R.; Freiberg, A.; Scharfe, J.; Girbig, M.; Nienhaus, A.; Seidler, A. Do Technical Aids for Patient Handling Prevent Musculoskeletal Complaints in Health Care Workers?—A Systematic Review of Intervention Studies. Int. J. Environ. Res. Public Health 2018, 15, 476. https://doi.org/10.3390/ijerph15030476
Hegewald J, Berge W, Heinrich P, Staudte R, Freiberg A, Scharfe J, Girbig M, Nienhaus A, Seidler A. Do Technical Aids for Patient Handling Prevent Musculoskeletal Complaints in Health Care Workers?—A Systematic Review of Intervention Studies. International Journal of Environmental Research and Public Health. 2018; 15(3):476. https://doi.org/10.3390/ijerph15030476
Chicago/Turabian StyleHegewald, Janice, Wera Berge, Philipp Heinrich, Ronny Staudte, Alice Freiberg, Julia Scharfe, Maria Girbig, Albert Nienhaus, and Andreas Seidler. 2018. "Do Technical Aids for Patient Handling Prevent Musculoskeletal Complaints in Health Care Workers?—A Systematic Review of Intervention Studies" International Journal of Environmental Research and Public Health 15, no. 3: 476. https://doi.org/10.3390/ijerph15030476
APA StyleHegewald, J., Berge, W., Heinrich, P., Staudte, R., Freiberg, A., Scharfe, J., Girbig, M., Nienhaus, A., & Seidler, A. (2018). Do Technical Aids for Patient Handling Prevent Musculoskeletal Complaints in Health Care Workers?—A Systematic Review of Intervention Studies. International Journal of Environmental Research and Public Health, 15(3), 476. https://doi.org/10.3390/ijerph15030476








