First Characterization of ADAMTS-4 in Kidney Tissue and Plasma of Patients with Chronic Kidney Disease—A Potential Novel Diagnostic Indicator
Abstract
1. Introduction
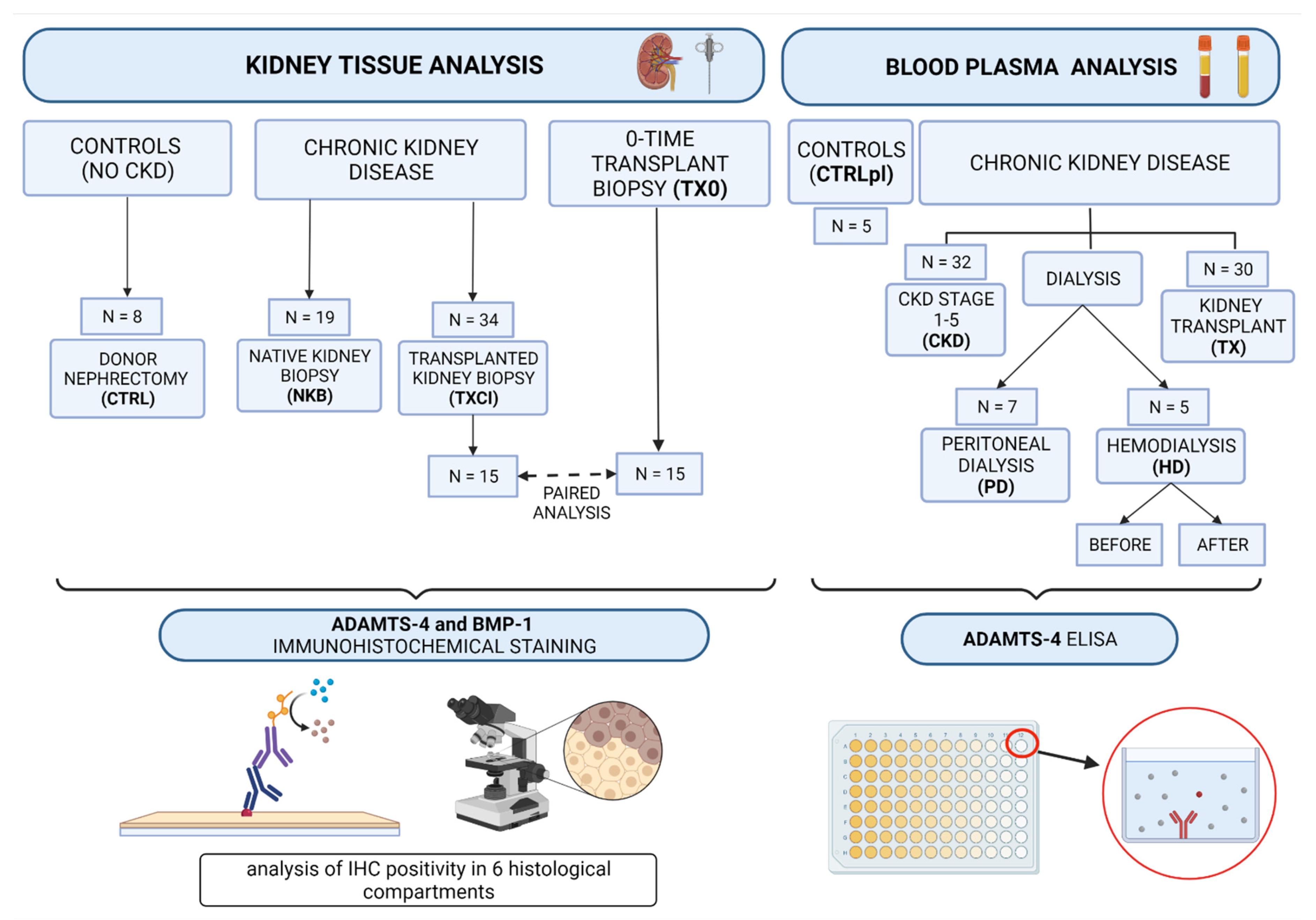
2. Materials and Methods
2.1. Sample Collection and Study Outline
2.2. Kidney Biopsy Sample Collection and Analysis
2.3. Immunohistochemistry Analysis (IHC)
2.4. Enzyme-Linked Immunosorbent Assay (ELISA)
2.5. Statistical Analysis
3. Results
3.1. Immunohistochemistry Analysis of ADAMTS-4 and BMP-1 Molecules in Kidney Biopsy Samples of Patients with CKD
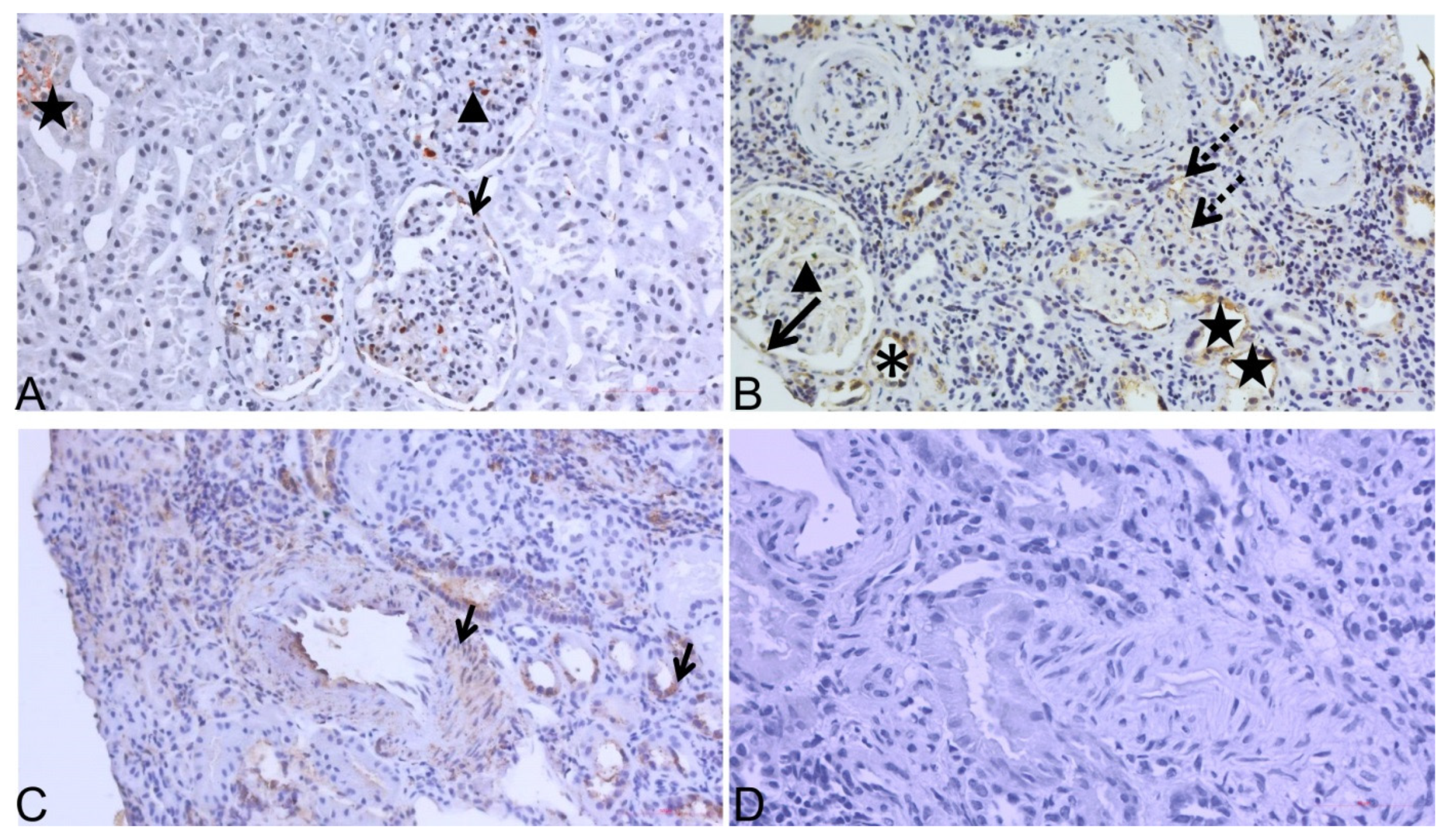
3.2. Distribution of ADAMTS-4 and BMP-1 in Kidney Tissue Samples of CTRL, NKB and TXCI Group
3.2.1. BMP-1 and ADAMTS-4 in Kidney Samples without CKD
3.2.2. BMP-1 and ADAMTS-4 in Kidney Samples with CKD
3.3. Association of ADAMTS-4 Expression in Interstitial Compartment with Chronic Kidney Histology Scores
3.4. Analysis of ADAMTS-4 IHC Expression in 15 Transplant Kidney Biopsy Sample Pairs (TX0-TXCI)
3.5. Detection of ADAMTS-4 in Plasma of Patients with CKD (Elisa Analysis)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study. Lancet 2020, 395, 709–733. [Google Scholar] [CrossRef]
- Stenvinkel, P. Chronic kidney disease: A public health priority and harbinger of premature cardiovascular disease. J. Intern. Med. 2010, 268, 456–467. [Google Scholar] [CrossRef] [PubMed]
- Levey, A.S.; Astor, B.C.; Stevens, L.A.; Coresh, J. Chronic kidney disease, diabetes, and hypertension: What’s in a name? Kidney Int. 2010, 78, 19–22. [Google Scholar] [CrossRef] [PubMed]
- Gansevoort, R.T.; de Jong, P.E. Challenges for the present CKD classification system. Curr. Opin. Nephrol. Hypertens. 2010, 19, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Tampe, D.; Zeisberg, M. Potential approaches to reverse or repair renal fibrosis. Nat. Rev. Nephrol. 2014, 10, 226–237. [Google Scholar] [CrossRef] [PubMed]
- Weiner, D.E.; Tighiouart, H.; Amin, M.G.; Stark, P.C.; MacLeod, B.; Griffith, J.L.; Salem, D.N.; Levey, A.S.; Sarnak, M.J. Chronic Kidney Disease as a Risk Factor for Cardiovascular Disease and All-Cause Mortality: A Pooled Analysis of Community-Based Studies. J. Am. Soc. Nephrol. 2004, 15, 1307–1315. [Google Scholar] [CrossRef]
- Kalluri, R.; Zeisberg, M. Fibroblasts in cancer. Nat. Rev. Cancer 2006, 6, 392–401. [Google Scholar] [CrossRef]
- Boor, P.; Ostendorf, T.; Floege, J. Renal fibrosis: Novel insights into mechanisms and therapeutic targets. Nat. Rev. Nephrol. 2010, 6, 643–656. [Google Scholar] [CrossRef]
- Strutz, F.; Zeisberg, M. Renal Fibroblasts and Myofibroblasts in Chronic Kidney Disease. J. Am. Soc. Nephrol. 2006, 17, 2992–2998. [Google Scholar] [CrossRef]
- Wolfe, R.A.; Ashby, V.B.; Milford, E.L.; Ojo, A.O.; Ettenger, R.E.; Agodoa, L.Y.C.; Held, P.J.; Port, F.K. Comparison of Mortality in All Patients on Dialysis, Patients on Dialysis Awaiting Transplantation, and Recipients of a First Cadaveric Transplant. N. Engl. J. Med. 1999, 341, 1725–1730. [Google Scholar] [CrossRef]
- Little, M.H.; Bertram, J.F. Is There Such a Thing as a Renal Stem Cell?: Figure 1. J. Am. Soc. Nephrol. 2009, 20, 2112–2117. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Grgurevic, L.; Macek, B.; Healy, D.R.; Brault, A.L.; Erjavec, I.; Cipcic, A.; Grgurevic, I.; Rogic, D.; Galesic, K.; Brkljacic, J.; et al. Circulating Bone Morphogenetic Protein 1–3 Isoform Increases Renal Fibrosis. J. Am. Soc. Nephrol. 2011, 22, 681–692. [Google Scholar] [CrossRef]
- Grgurevic, L.; Vukicevic, S. ADAMTS4 as a Blood Biomarker and Therapeutic Target for Chronic Renal Failure. U.S. Patent 8,263,072 B2, 11 September 2012. [Google Scholar]
- Rudnicki, M.; Perco, P.; Neuwirt, H.; Noppert, S.-J.; Leierer, J.; Sunzenauer, J.; Eder, S.; Zoja, C.; Eller, K.; Rosenkranz, A.R.; et al. Increased Renal Versican Expression Is Associated with Progression of Chronic Kidney Disease. PLoS ONE 2012, 7, e44891. [Google Scholar] [CrossRef] [PubMed]
- Novak, R.; Hrkac, S.; Salai, G.; Bilandzic, J.; Mitar, L.; Grgurevic, L. The Role of ADAMTS-4 in Atherosclerosis and Vessel Wall Abnormalities. J. Vasc. Res. 2022, 1–9. [Google Scholar] [CrossRef]
- Engel, J.E.; Chade, A.R. Macrophage polarization in chronic kidney disease: A balancing act between renal recovery and decline? Am. J. Physiol. Physiol. 2019, 317, F1409–F1413. [Google Scholar] [CrossRef]
- Wågsäter, D.; Björk, H.; Zhu, C.; Björkegren, J.; Valen, G.; Hamsten, A.; Eriksson, P. ADAMTS-4 and -8 are inflammatory regulated enzymes expressed in macrophage-rich areas of human atherosclerotic plaques. Atherosclerosis 2008, 196, 514–522. [Google Scholar] [CrossRef]
- Walker, P.D. The Renal Biopsy. Arch. Pathol. Lab. Med. 2009, 133, 181–188. [Google Scholar] [CrossRef]
- Roufosse, C.; Simmonds, N.; Groningen, M.C.-V.; Haas, M.; Henriksen, K.J.; Horsfield, C.; Loupy, A.; Mengel, M.; Perkowska-Ptasińska, A.; Rabant, M.; et al. A 2018 Reference Guide to the Banff Classification of Renal Allograft Pathology. Transplantation 2018, 102, 1795–1814. [Google Scholar] [CrossRef]
- Dong, H.; Du, T.; Premaratne, S.; Zhao, C.X.; Tian, Q.; Li, Y.; Yan, S.; Zhang, W.W. Relationship between ADAMTS4 and carotid atherosclerotic plaque vulnerability in humans. J. Vasc. Surg. 2018, 67, 1120–1126. [Google Scholar] [CrossRef]
- Yuan, C.; Liu, Z.; Yu, Q.; Wang, X.; Bian, M.; Yu, Z.; Yu, J. Expression of PD-1/PD-L1 in primary breast tumours and metastatic axillary lymph nodes and its correlation with clinicopathological parameters. Sci. Rep. 2019, 9, 14356. [Google Scholar] [CrossRef]
- Wang, S.; Lu, Y.; Hong, Q.; Geng, X.; Wang, X.; Zheng, W.; Song, C.; Liu, C.; Fan, M.; Xi, Y.; et al. Protein Array-Based Detection of Proteins in Kidney Tissues from Patients with Membranous Nephropathy. BioMed Res. Int. 2017, 2017, 7843584. [Google Scholar] [CrossRef] [PubMed]
- Boerboom, D.; Lafond, J.-F.; Zheng, X.; Lapointe, E.; Mittaz, L.; Boyer, A.; Pritchard, M.A.; DeMayo, F.J.; Mort, J.S.; Drolet, R.; et al. Partially redundant functions of Adamts1 and Adamts4 in the perinatal development of the renal medulla. Dev. Dyn. 2011, 240, 1806–1814. [Google Scholar] [CrossRef] [PubMed]
- Bábíčková, J.; Klinkhammer, B.M.; Buhl, E.M.; Djudjaj, S.; Hoss, M.; Heymann, F.; Tacke, F.; Floege, J.; Becker, J.U.; Boor, P. Regardless of etiology, progressive renal disease causes ultrastructural and functional alterations of peritubular capillaries. Kidney Int. 2017, 91, 70–85. [Google Scholar] [CrossRef] [PubMed]
- Schrimpf, C.; Xin, C.; Campanholle, G.; Gill, S.E.; Stallcup, W.; Lin, S.L.; Duffield, J.S. Pericyte TIMP3 and ADAMTS1 Modulate Vascular Stability after Kidney Injury. J. Am. Soc. Nephrol. 2012, 23, 868–883. [Google Scholar] [CrossRef]
- Grgic, I.; Krautzberger, A.M.; Hofmeister, A.; Lalli, M.; DiRocco, D.P.; Fleig, S.V.; Humphreys, B.D. Translational Profiles of Medullary Myofibroblasts during Kidney Fibrosis. J. Am. Soc. Nephrol. 2014, 25, 1979–1990. [Google Scholar] [CrossRef]
- Armutcu, F.; Demircan, K.; Yildirim, U.; Namuslu, M.; Yagmurca, M.; Celik, H.T. Hypoxia causes important changes of extracellular matrix biomarkers and ADAMTS proteinases in the adriamycin-induced renal fibrosis model. Nephrology 2019, 24, 863–875. [Google Scholar] [CrossRef]
- Boyd, D.F.; Allen, E.K.; Randolph, A.G.; Guo, X.Z.J.; Weng, Y.; Sanders, C.J.; Thomas, P.G. Exuberant fibroblast activity compromises lung function via ADAMTS4. Nature 2020, 587, 466–471. [Google Scholar] [CrossRef]
- Bülow, R.D.; Boor, P. Extracellular Matrix in Kidney Fibrosis: More Than Just a Scaffold. J. Histochem. Cytochem. 2019, 67, 643–661. [Google Scholar] [CrossRef]
- Bode-Lesniewska, B.; Dours-Zimmermann, M.T.; Odermatt, B.F.; Briner, J.; Heitz, P.U.; Zimmermann, D.R. Distribution of the large aggregating proteoglycan versican in adult human tissues. J. Histochem. Cytochem. 1996, 44, 303–312. [Google Scholar] [CrossRef]
- Islam, S.; Watanabe, H. Versican: A Dynamic Regulator of the Extracellular Matrix. J. Histochem. Cytochem. 2020, 68, 763–775. [Google Scholar] [CrossRef]
- Tang, P.M.-K.; Nikolic-Paterson, D.J.; Lan, H.-Y. Macrophages: Versatile players in renal inflammation and fibrosis. Nat. Rev. Nephrol. 2019, 15, 144–158. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.Y.; Jiang, H.; Pan, J.; Huang, X.R.; Wang, Y.C.; Huang, H.F.; Chen, J.H. Macrophage-to-Myofibroblast Transition Contributes to Interstitial Fibrosis in Chronic Renal Allograft Injury. J. Am. Soc. Nephrol. 2017, 28, 2053–2067. [Google Scholar] [CrossRef] [PubMed]
- Sandy, J.D.; Westling, J.; Kenagy, R.D.; Iruela-Arispe, M.L.; Verscharen, C.; Rodriguez-Mazaneque, J.C.; Clowes, A.W. Versican V1 Proteolysis in Human Aorta in Vivo Occurs at the Glu441-Ala442 Bond, a Site That Is Cleaved by Recombinant ADAMTS-1 and ADAMTS-4. J. Biol. Chem. 2001, 276, 13372–13378. [Google Scholar] [CrossRef] [PubMed]
- Koch, C.D.; Lee, C.M.; Apte, S.S. Aggrecan in Cardiovascular Development and Disease. J. Histochem. Cytochem. 2020, 68, 777–795. [Google Scholar] [CrossRef] [PubMed]
- Vadon-Le Goff, S.; Hulmes, D.J.S.; Moali, C. BMP-1/tolloid-like proteinases synchronize matrix assembly with growth factor activation to promote morphogenesis and tissue remodeling. Matrix Biol. 2015, 44–46, 14–23. [Google Scholar] [CrossRef]
- Bai, M.; Lei, J.; Wang, S.; Ding, D.; Yu, X.; Guo, Y.; Zhang, A. BMP1 inhibitor UK383,367 attenuates renal fibrosis and inflammation in CKD. Am. J. Physiol. Physiol. 2019, 317, F1430–F1438. [Google Scholar] [CrossRef]
- Yong, K.; Dogra, G.; Boudville, N.; Lim, W. Increased Inflammatory Response in Association with the Initiation of Hemodialysis Compared with Peritoneal Dialysis in a Prospective Study of End-Stage Kidney Disease Patients. Perit. Dial. Int. 2018, 38, 18–23. [Google Scholar] [CrossRef]



| CTRL N = 8 | NKB N = 19 | TXCI N = 34 | TXCI-TX0 PAIRS N = 15 | ||
|---|---|---|---|---|---|
| TXCI (N = 15) | TX0 (N = 15) | ||||
| AGE (YEARS) | 53 ± 13 | 43 ± 17 | 50 ± 16 | 51 ± 44 | 51 ± 7 |
| SEX (% MALE) | 2 (25%) | 7 (37%) | 28 (82%) | 14 (93%) | 6 (40%) |
| BMI | 24.3 ± 4.6 | 26.1 ± 5.7 | 27.1 ± 5.4 | 27.9 ± 18.5 | 25.6 ± 2.2 |
| EGFR (ML/MIN) | 108 ± 28 | 56 ± 36 | 37 ± 16 | 38 ± 64 | 91 ± 22 |
| 24-PROT G/L | - | 3.27 ± 2.74 | 1.53 ± 1.50 | 1.22 ± 5.46 | - |
| CKD | N (%) | N (%) | N (%) | N (%) | N (%) |
| NO CKD | 8 (100) | 0 | 0 | 0 | 14 (93) |
| CKD-1 | 5 (26.3) | 0 | 0 | 1 (6.7) | |
| CKD-2 | 4 (21.1) | 3 (8.8) | 1 (6.7) | 0 | |
| CKD-3 | 2 (10.5) | 20 (58.8) | 9 (60) | 0 | |
| CKD-4 | 6 (31.6) | 10 (29.4) | 5 (33.3) | 0 | |
| CKD-5 | 2 (10.5) | 1 (2.9) | 0 | 0 | |
| COMORBIDITIES | N (%) | N (%) | N (%) | N (%) | N (%) |
| AH | 4 (50) | 12 (63.2) | 31 (91.2) | 13 (86.6) | 6 (40) |
| DM | 0 | 0 | 9 (26.5) | 5 (33.3) | 0 |
| SMOK | 0 | 6 (31.6) | 5 (14.7) | 1 (6.7) | 1 (6.7) |
| HLP | 0 | 9 (47.4) | 13 (38.2) | 5 (33.3) | 0 |
| CAD | 0 | 0 | 4 (11.8) | 1 (6.7) | 0 |
| ATH | 0 | 2 (10.5) | 4 (11.8) | 13 (86.6) | 0 |
| KIDNEY DISEASE | N (%) | N (%) | N (%) | N (%) | N (%) |
| NB | 8 (100) | 0 | 2 (5.8) | 2 (13.3) | 13 (86.6) |
| GN | - | 17 (89.5) | 4 (11.7) | 1 (6.6) | - |
| HTN | - | 1 (5.3) | - | - | - |
| ANCA VS | - | 1 (5.3) | - | - | - |
| TCR | - | - | 2 (5.8) | 1 (6.6) | - |
| ABMR | - | - | 5 (14.7) | 1 (6.6) | - |
| TCR + ABMR | - | - | 4 (11.7) | 1 (6.6) | - |
| BKVAN | - | - | 3 (8.8) | 3 (20) | - |
| NC | - | 0 | 14 (41.1) | 6 (40) | 2 (13.3) |
| ATI | 6 (75) | 5 (26.3) | 8 (23.5) | 3 (20) | 8 (53.3) |
| TX0 (N = 15) | TXCI (N = 15) | p | |
|---|---|---|---|
| eGFR (mean) | 91.47 | 37.93 | <0.00001 |
| CKD STAGE (median) | 0 (0–3) | 3 (2–4) | <0.00001 |
| CI SCORE (mean) | 0.07 | 1.27 | 0.000157 |
| ADAMTS-4 INT (n/N) | 1/15 | 10/15 | 0.00169 |
| ADAMTS-4 PTC (n/N) | 0/15 | 15/15 | <0.0001 |
| ADAMTS-4 PXT (n/N) | 6/15 | 2/15 | NS |
| ADAMTS-4 DT (n/N) | 11/15 | 15/15 | NS |
| ADAMTS-4 GC (n/N) | 5/15 | 13/15 | 0.00778 |
| ADAMTS-4 BW (n/N) | 14/15 | 10/15 | NS |
| TIMEPOINT OF BIOPSY (days) | 0 | 690 (28–2340) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vojtusek, I.K.; Laganovic, M.; Burek Kamenaric, M.; Bulimbasic, S.; Hrkac, S.; Salai, G.; Ivkovic, V.; Coric, M.; Novak, R.; Grgurevic, L. First Characterization of ADAMTS-4 in Kidney Tissue and Plasma of Patients with Chronic Kidney Disease—A Potential Novel Diagnostic Indicator. Diagnostics 2022, 12, 648. https://doi.org/10.3390/diagnostics12030648
Vojtusek IK, Laganovic M, Burek Kamenaric M, Bulimbasic S, Hrkac S, Salai G, Ivkovic V, Coric M, Novak R, Grgurevic L. First Characterization of ADAMTS-4 in Kidney Tissue and Plasma of Patients with Chronic Kidney Disease—A Potential Novel Diagnostic Indicator. Diagnostics. 2022; 12(3):648. https://doi.org/10.3390/diagnostics12030648
Chicago/Turabian StyleVojtusek, Ivana Kovacevic, Mario Laganovic, Marija Burek Kamenaric, Stela Bulimbasic, Stela Hrkac, Grgur Salai, Vanja Ivkovic, Marijana Coric, Rudjer Novak, and Lovorka Grgurevic. 2022. "First Characterization of ADAMTS-4 in Kidney Tissue and Plasma of Patients with Chronic Kidney Disease—A Potential Novel Diagnostic Indicator" Diagnostics 12, no. 3: 648. https://doi.org/10.3390/diagnostics12030648
APA StyleVojtusek, I. K., Laganovic, M., Burek Kamenaric, M., Bulimbasic, S., Hrkac, S., Salai, G., Ivkovic, V., Coric, M., Novak, R., & Grgurevic, L. (2022). First Characterization of ADAMTS-4 in Kidney Tissue and Plasma of Patients with Chronic Kidney Disease—A Potential Novel Diagnostic Indicator. Diagnostics, 12(3), 648. https://doi.org/10.3390/diagnostics12030648






