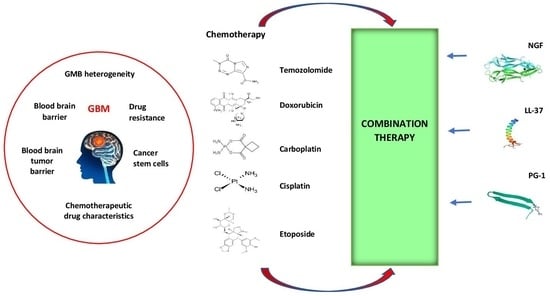
Nerve Growth Factor, Antimicrobial Peptides and Chemotherapy: Glioblastoma Combination Therapy to Improve Their Efficacy
Abstract
1. Introduction
2. Materials and Methods
2.1. Pharmacological Agents, Chemicals, Peptides, and Reagents
2.2. Cell Culture
2.3. Concentrations of Compounds
2.4. MTT Assay
2.5. Assessment of Drug-Concentration Effect and Calculation of the Combination Index
2.6. Assessment of Cell Viability with Flow Cytometry Using YO-PRO-1 and PI
2.7. Caspase Activation Analysis
2.8. Statistical Analysis
3. Results
3.1. Sensitivity of U251GBM Cells to NGF, LL-37, PG-1, and Chemotherapy and IC50 Calculation
3.2. The Combination Index (CI) and Anti-Tumor Activity of Combined Treatment of NGF, LL-37, and PG-1 with Chemotherapy
3.3. Cell Apoptosis Detected with Flow Cytometry
3.4. Activation of Caspase-3 on U251 Cells
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD 2016 Brain and Other CNS Cancer Collaborators. Global, regional, and national burden of brain and other CNS cancer, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 376–393. [Google Scholar] [CrossRef]
- Ferlay, J.; Ervik, M.; Lam, F.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Soerjomataram, I.; Bray, F. Global cancer observatory: Cancer today. Lyon Fr. Int. Agency Res. Cancer 2018, 3, 2019. [Google Scholar]
- Nabors, L.B.; Portnow, J.; Ahluwalia, M.; Baehring, J.; Brem, H.; Brem, S.; Butowski, N.; Campian, J.L.; Clark, S.W.; Fabiano, A.J.; et al. Central Nervous System Cancers, Version 3.2020, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. JNCCN 2020, 18, 1537–1570. [Google Scholar] [CrossRef]
- Stupp, R.; Taillibert, S.; Kanner, A.; Read, W.; Steinberg, D.; Lhermitte, B.; Toms, S.; Idbaih, A.; Ahluwalia, M.S.; Fink, K.; et al. Effect of Tumor-Treating Fields Plus Maintenance Temozolomide vs Maintenance Temozolomide Alone on Survival in Patients With Glioblastoma: A Randomized Clinical Trial. JAMA 2017, 318, 2306–2316. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhang, M.; Gan, H.; Wang, H.; Lee, J.H.; Fang, D.; Kitange, G.J.; He, L.; Hu, Z.; Parney, I.F.; et al. A novel enhancer regulates MGMT expression and promotes temozolomide resistance in glioblastoma. Nat. Commun. 2018, 9, 2949. [Google Scholar] [CrossRef] [PubMed]
- Loeffler, J.S.; Alexander, E., 3rd; Hochberg, F.H.; Wen, P.Y.; Morris, J.H.; Schoene, W.C.; Siddon, R.L.; Morse, R.H.; Black, P.M. Clinical patterns of failure following stereotactic interstitial irradiation for malignant gliomas. Int. J. Radiat. Oncol. Biol. Phys. 1990, 19, 1455–1462. [Google Scholar] [CrossRef]
- Saunders, N.A.; Simpson, F.; Thompson, E.W.; Hill, M.M.; Endo-Munoz, L.; Leggatt, G.; Minchin, R.F.; Guminski, A. Role of intratumoural heterogeneity in cancer drug resistance: Molecular and clinical perspectives. EMBO Mol. Med. 2012, 4, 675–684. [Google Scholar] [CrossRef]
- Furnari, F.B.; Cloughesy, T.F.; Cavenee, W.K.; Mischel, P.S. Heterogeneity of epidermal growth factor receptor signalling networks in glioblastoma. Nat. Rev. Cancer 2015, 15, 302–310. [Google Scholar] [CrossRef]
- Qazi, M.A.; Vora, P.; Venugopal, C.; Sidhu, S.S.; Moffat, J.; Swanton, C.; Singh, S.K. Intratumoral heterogeneity: Pathways to treatment resistance and relapse in human glioblastoma. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2017, 28, 1448–1456. [Google Scholar] [CrossRef]
- Gupta, S.K.; Kizilbash, S.H.; Daniels, D.J.; Sarkaria, J.N. Editorial: Targeted Therapies for Glioblastoma: A Critical Appraisal. Front. Oncol. 2019, 9, 1216. [Google Scholar] [CrossRef]
- Di Tacchio, M.; Macas, J.; Weissenberger, J.; Sommer, K.; Bähr, O.; Steinbach, J.P.; Senft, C.; Seifert, V.; Glas, M.; Herrlinger, U.; et al. Tumor Vessel Normalization, Immunostimulatory Reprogramming, and Improved Survival in Glioblastoma with Combined Inhibition of PD-1, Angiopoietin-2, and VEGF. Cancer Immunol. Res. 2019, 7, 1910–1927. [Google Scholar] [CrossRef] [PubMed]
- Polivka, J.; Polivka, J.; Holubec, L.; Kubikova, T.; Priban, V.; Hes, O.; Pivovarcikova, K.; Treskova, I. Advances in Experimental Targeted Therapy and Immunotherapy for Patients with Glioblastoma Multiforme. Anticancer Res. 2017, 37, 21–33. [Google Scholar] [CrossRef] [PubMed]
- Balandin, S.V.; Emelianova, A.A.; Kalashnikova, M.B.; Kokryakov, V.N.; Shamova, O.V.; Ovchinnikova, T.V. Molecular Mechanisms of Anticancer Action of Natural Antimicrobial Peptides. Bioorganic Chem. 2016, 42, 633–648. [Google Scholar]
- CIBA Foundation Symposium. Growth Factors in Biology and Medicine; Evered, D., Nugent, J., Whelan, J., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2009; ISBN 0470718676/9780470718674. [Google Scholar]
- Apfel, S.C.; Arezzo, J.C.; Brownlee, M.; Federoff, H.; Kessler, J.A. Nerve growth factor administration protects against experimental diabetic sensory neuropathy. Brain Res. 1994, 634, 7–12. [Google Scholar] [CrossRef]
- Aloe, L.; Rocco, M.L.; Balzamino, B.O.; Micera, A. Nerve growth factor: Role in growth, differentiation and controlling cancer cell development. J. Exp. Clin. Cancer Res. CR 2016, 35, 116. [Google Scholar] [CrossRef]
- Verge, V.M.; Merlio, J.P.; Grondin, J.; Ernfors, P.; Persson, H.; Riopelle, R.J.; Hökfelt, T.; Richardson, P.M. Colocalization of NGF binding sites, trk mRNA, and low-affinity NGF receptor mRNA in primary sensory neurons: Responses to injury and infusion of NGF. J. Neurosci. Off. J. Soc. Neurosci. 1992, 12, 4011–4022. [Google Scholar] [CrossRef]
- Chiaretti, A.; Antonelli, A.; Genovese, O.; Fernandez, E.; Di Giuda, D.; Mariotti, P.; Riccardi, R. Intraventricular nerve growth factor infusion improves cerebral blood flow and stimulates doublecortin expression in two infants with hypoxic-ischemic brain injury. Neurol. Res. 2008, 30, 223–228. [Google Scholar] [CrossRef]
- Goretzki, P.E.; Wahl, R.A.; Becker, R.; Koller, C.; Branscheid, D.; Grussendorf, M.; Roeher, H.D. Nerve growth factor (NGF) sensitizes human medullary thyroid carcinoma (hMTC) cells for cytostatic therapy in vitro. Surgery 1987, 102, 1035–1042. [Google Scholar]
- Rakowicz-Szulczyńska, E.M.; Herlyn, M.; Koprowski, H. Nerve growth factor receptors in chromatin of melanoma cells, proliferating melanocytes, and colorectal carcinoma cells in vitro. Cancer Res. 1988, 48 Pt 1, 7200–7206. [Google Scholar]
- Rakowicz-Szulczynska, E.M.; Reddy, U.; Vorbrodt, A.; Herlyn, D.; Koprowski, H. Chromatin and cell surface receptors mediate melanoma cell growth response to nerve growth factor. Mol. Carcinog. 1991, 4, 388–396. [Google Scholar] [CrossRef]
- Revoltella, R.P.; Butler, R.H. Nerve growth factor may stimulate either division or differentiation of cloned C1300 neuroblastoma cells in serum-free cultures. J. Cell. Physiol. 1980, 104, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Yang, Y.; Gong, A.; Wang, C.; Liang, Y.; Chenet, Y. Localization of NGF and TrkA at mitotic apparatus in human glioma cell line U251. Biochem. Biophys. Res. Commun. 2005, 337, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.W.; Friess, H.; Wang, L.; Di Mola, F.F.; Zimmermann, A.; Büchler, M.W. Down-regulation of nerve growth factor in poorly differentiated and advanced human esophageal cancer. Anticancer Res. 2000, 20, 125–132. [Google Scholar] [PubMed]
- Chiaretti, A.; Falsini, B.; Servidei, S.; Marangoni, D.; Pierri, F.; Riccardi, R. Nerve growth factor eye drop administration improves visual function in a patient with optic glioma. Neurorehabilit. Neural Repair 2011, 25, 386–390. [Google Scholar] [CrossRef]
- Falsini, B.; Chiaretti, A.; Barone, G.; Piccardi, M.; Pierri, F.; Colosimo, C.; Lazzareschi, I.; Ruggiero, A.; Parisi, V.; Fadda, A.; et al. Topical nerve growth factor as a visual rescue strategy in pediatric optic gliomas: A pilot study including electrophysiology. Neurorehabilit. Neural Repair 2011, 25, 512–520. [Google Scholar] [CrossRef]
- Falsini, B.; Chiaretti, A.; Rizzo, D.; Piccardi, M.; Ruggiero, A.; Manni, L.; Soligo, M.; Dickmann, A.; Federici, M.; Salerni, A.; et al. Nerve growth factor improves visual loss in childhood optic gliomas: A randomized, double-blind, phase II clinical trial. Brain A J. Neurol. 2016, 139 Pt 2, 404–414. [Google Scholar] [CrossRef]
- Kimura, S.; Yoshino, A.; Katayama, Y.; Watanabe, T.; Fukushima, T. Growth control of C6 glioma in vivo by nerve growth factor. J. Neuro-Oncol. 2002, 59, 199–205. [Google Scholar] [CrossRef]
- Zhao, X.; Wu, H.; Lu, H.; Li, G.; Huang, Q. LAMP: A Database Linking Antimicrobial Peptides. PLoS ONE 2013, 8, e66557. [Google Scholar] [CrossRef]
- Do, N.; Weindl, G.; Grohmann, L.; Salwiczek, M.; Koksch, B.; Korting, H.C.; Schäfer-Korting, M. Cationic membrane-active peptides-anticancer and antifungal activity as well as penetration into human skin. Exp. Dermatol. 2014, 23, 326–331. [Google Scholar] [CrossRef]
- Pushpanathan, M.; Gunasekaran, P.; Rajendhran, J. Antimicrobial peptides: Versatile biological properties. Int. J. Pept. 2013, 2013, 675391. [Google Scholar] [CrossRef]
- Hoskin, D.W.; Ramamoorthy, A. Studies on anticancer activities of antimicrobial peptides. Biochim. Et Biophys. Acta 2008, 1778, 357–375. [Google Scholar] [CrossRef]
- Mader, J.S.; Hoskin, D.W. Cationic antimicrobial peptides as novel cytotoxic agents for cancer treatment. Expert Opin. Investig. Drugs 2006, 15, 933–946. [Google Scholar] [CrossRef] [PubMed]
- Deslouches, B.; Steckbeck, J.D.; Craigo, J.K.; Doi, Y.; Burns, J.L.; Montelaro, R.C. Engineered cationic antimicrobial peptides to overcome multidrug resistance by ESKAPE pathogens. Antimicrob. Agents Chemother. 2015, 59, 1329–1333. [Google Scholar] [CrossRef] [PubMed]
- Steckbeck, J.D.; Deslouches, B.; Montelaro, R.C. Antimicrobial peptides: New drugs for bad bugs? Expert Opin. Biol. Ther. 2014, 14, 11–14. [Google Scholar] [CrossRef] [PubMed]
- Deslouches, B.; Steckbeck, J.D.; Craigo, J.K.; Doi, Y.; Mietzner, T.A.; Montelaro, R.C. Rational design of engineered cationic antimicrobial peptides consisting exclusively of arginine and tryptophan, and their activity against multidrug-resistant pathogens. Antimicrob. Agents Chemother. 2013, 57, 2511–2521. [Google Scholar] [CrossRef] [PubMed]
- Scocchi, M.; Mardirossian, M.; Runti, G.; Benincasa, M. Non-Membrane Permeabilizing Modes of Action of Antimicrobial Peptides on Bacteria. Curr. Top. Med. Chem. 2016, 16, 76–88. [Google Scholar] [CrossRef]
- Lei, J.; Sun, L.; Huang, S.; Zhu, C.; Li, P.; He, J.; Mackey, V.; Coy, D.H.; He, Q. The antimicrobial peptides and their potential clinical applications. Am. J. Transl. Res. 2019, 11, 3919–3931. [Google Scholar]
- Gkeka, P.; Sarkisov, L. Interactions of phospholipid bilayers with several classes of amphiphilic alpha-helical peptides: Insights from coarse-grained molecular dynamics simulations. J. Phys. Chem. B 2010, 114, 826–839. [Google Scholar] [CrossRef]
- Wang, L.; Dong, C.; Li, X.; Han, W.; Su, X. Anticancer potential of bioactive peptides from animal sources (Review). Oncol. Rep. 2017, 38, 637–651. [Google Scholar] [CrossRef]
- Imamovic, L.; Sommer, M.O. Use of collateral sensitivity networks to design drug cycling protocols that avoid resistance development. Sci. Transl. Med. 2013, 5, 204ra132. [Google Scholar] [CrossRef]
- Cokol, M.; Chua, H.N.; Tasan, M.; Mutlu, B.; Weinstein, Z.B.; Suzuki, Y.; Nergiz, M.E.; Costanzo, M.; Baryshnikova, A.; Giaever, G.; et al. Systematic exploration of synergistic drug pairs. Mol. Syst. Biol. 2011, 7, 544. [Google Scholar] [CrossRef] [PubMed]
- Freshney, R.I. Animal Cell Culture: A Practical Approach, 3rd ed.; Oxford University Press: London, UK, 2000. [Google Scholar]
- Zhang, S.; Xie, R.; Wan, F.; Ye, F.; Guo, D.; Lei, T. Identification of U251 glioma stem cells and their heterogeneous stem-like phenotypes. Oncol. Lett. 2013, 6, 1649–1655. [Google Scholar] [CrossRef] [PubMed]
- Florento, L.; Matias, R.; Tuaño, E.; Santiago, K.; Dela Cruz, F.; Tuazon, A. Comparison of Cytotoxic Activity of Anticancer Drugs against Various Human Tumor Cell Lines Using In Vitro Cell-Based Approach. Int. J. Biomed. Sci. IJBS 2012, 8, 76–80. [Google Scholar] [CrossRef]
- Mosmann, T. Rapid colorimetric assay for cellular growth and survival: Application to proliferation and cytotoxicity assays. J. Immunol. Methods 1983, 65, 55–63. [Google Scholar] [CrossRef]
- Mohamadi, N.; Kazemi, S.M.; Mohammadian, M.; Milani, A.T.; Moradi, Y.; Yasemi, M.; Ebrahimifar, M.; Tabrizi, M.M.; Shahmabadi, H.E.; Khiyavi, A.A. Toxicity of Cisplatin-Loaded Poly Butyl Cyanoacrylate Nanoparticles in a Brain Cancer Cell Line: Anionic Polymerization Results. Asian Pac. J. Cancer Prev. APJCP 2017, 18, 629–632. [Google Scholar]
- Svirnovsky, A.I. Methodological studies of drug sensitivity of leukemic cells. Probl. Health Ecol. 2011, 3, 89–91. [Google Scholar]
- Chou, T.C. Theoretical basis, experimental design, and computerized simulation of synergism and antagonism in drug combination studies. Pharmacol. Rev. 2006, 58, 621–681. [Google Scholar] [CrossRef]
- Mindukshev, I.; Kudryavtsev, I.; Serebriakova, M.; Trulioff, A.; Gambaryan, S.; Sudnitsyna, J.; Khmelevskoy, D.; Voitenko, N.; Avdonin, P.; Jenkins, R.; et al. Flow Cytometry and Light Scattering Technique in Evaluation of Nutraceuticals. In Nutraceuticals; Elsevier: Amsterdam, The Netherlands, 2016; pp. 319–332. [Google Scholar]
- Dubashynskaya, N.V.; Golovkin, A.S.; Kudryavtsev, I.V.; Prikhodko, S.S.; Trulioff, A.S.; Bokatyi, A.N.; Poshina, D.N.; Raik, S.V.; Skorik, Y.A. Mucoadhesive cholesterol-chitosan self-assembled particles for topical ocular delivery of dexamethasone. Int. J. Biol. Macromol. 2020, 158, 811–818. [Google Scholar] [CrossRef]
- Caspase 3 Assay Kit, Colorimetric: Technical Bulletin (2004) Sigma-Aldrich, Inc 4 p. Available online: https://www.abcam.com/products/assay-kits/caspase-3-assay-kit-colorimetric-ab39401.html (accessed on 29 October 2023).
- van Belle, G.; Fisher, L.D.; Heagerty, P.J.; Lumley, T. Biostatistics: A Methodology for the Health Sciences; Fisher, L.D., van Belle, G., Eds.; Jonh Wiley and Sons Inc.: Hoboken, NJ, USA, 2004. [Google Scholar]
- Voronina, T.A.; Guzeevatykh, L.S.; Mironov, A.N. Guidelines for Conducting Preclinical Studies of Drugs; Mulyar, A.G., Chichenkov, O.N., Eds.; Grif and K: Moscow, Russia, 2012. [Google Scholar]
- Chernov, A.N.; Tsapieva, A.; Alaverdian, D.A.; Filatenkova, T.A.; Galimova, E.S.; Suvorova, M.; Shamova, O.V.; Suvorov, A.N. In vitro evaluation of the cytotoxic effect of Streptococcus pyogenes strains, protegrin PG-1, cathelicidin LL-37, nerve growth factor and chemotherapy on the C6 glioma cell line. Molecules 2022, 27, 569. [Google Scholar] [CrossRef]
- Chernov, A.N.; Filatenkova, T.A.; Glushakov, R.I.; Buntovskaya, A.S.; Alaverdian, D.A.; Tsapieva, A.N.; Kim, A.V.; Fedorov, E.V.; Skliar, S.S.; Matsko, M.V.; et al. Anticancer effect of cathelicidin LL-37, protegrin PG-1, nerve growth factor NGF, and temozolomide: Impact on the mitochondrial metabolism, clonogenic potential, and migration of human U251 glioma cells. Molecules 2022, 27, 4988. [Google Scholar] [CrossRef]
- Giraud, S.; Loum, E.; Bessette, B.; Mathonnet, M.; Lalloué, F. P75 neurotrophin receptor is sequestered in the Golgi apparatus of the U-87 MG human glioblastoma cell line. Int. J. Oncol. 2011, 38, 391–399. [Google Scholar] [PubMed][Green Version]
- Oelmann, E.; Sreter, L.; Schuller, I.; Serve, H.; Koenigsmann, M.; Wiedenmann, B.; Oberberg, D.; Reufi, B.; Thiel, E.; Berdel, W.E. Nerve growth factor stimulates clonal growth of human lung cancer cell lines and a human glioblastoma cell line expressing high-affinity nerve growth factor binding sites involving tyrosine kinase signaling. Cancer Res. 1995, 55, 2212–2219. [Google Scholar] [PubMed]
- Singer, H.S.; Hansen, B.; Martinie, D.; Karp, C.L. Mitogenesis in glioblastoma multiforme cell lines: A role for NGF and its TrkA receptors. J. Neuro-Oncol. 1999, 45, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.T.; Wang, H.; Wang, F.J.; Xi, Y.F.; Chen, L.H. Expression of nerve growth factor and brain-derived neurotrophic factor in astrocytomas. Oncol. Lett. 2018, 15, 533–537. [Google Scholar] [CrossRef]
- Yang, Y.; Peng, H.; Chen, C.-B.; Yu, H. Expression and biological significance of nerve growth factor and its receptor in human glioma cell line U251. Chin. J. Clin. Rehabil. 2006, 10, 94–96. [Google Scholar]
- Johnston, A.L.; Lun, X.; Rahn, J.J.; Liacini, A.; Wang, L.; Hamilton, M.G.; Parney, I.F.; Hempstead, B.L.; Robbins, S.M.; Forsyth, P.A.; et al. The p75 neurotrophin receptor is a central regulator of glioma invasion. PLoS Biol. 2007, 5, e212. [Google Scholar] [CrossRef]
- Hempstead, B.L.; Martin-Zanca, D.; Kaplan, D.R.; Parada, L.F.; Chao, M.V. High-affinity NGF binding requires coexpression of the trk proto-oncogene and the low-affinity NGF receptor. Nature 1991, 350, 678–683. [Google Scholar] [CrossRef]
- Piktel, E.; Niemirowicz, K.; Wnorowska, U.; Wątek, M.; Wollny, T.; Głuszek, K.; Góźdź, S.; Levental, I.; Bucki, R. The Role of Cathelicidin LL-37 in Cancer Development. Arch. Immunol. Et Ther. Exp. 2016, 64, 33–46. [Google Scholar] [CrossRef]
- Chen, X.; Zou, X.; Qi, G.; Tang, Y.; Guo, Y.; Si, J.; Liang, L. Roles and Mechanisms of Human Cathelicidin LL-37 in Cancer. Cell. Physiol. Biochem. Int. J. Exp. Cell. Physiol. Biochem. Pharmacol. 2018, 47, 1060–1073. [Google Scholar] [CrossRef]
- An, L.L.; Ma, X.-T.; Yang, Y.-H.; Lin, Y.-M.; Song, Y.-H.; Wu, K.-F. Marked reduction of LL-37/hCAP-18, an antimicrobial peptide, in patients with acute myeloid leukemia. Int. J. Hematol. 2005, 81, 45–47. [Google Scholar] [CrossRef]
- Yang, Y.H.; Zheng, G.-G.; Li, G.; Zhang, B.; Song, Y.-H.; Wu, K.-F. Expression of LL-37/hCAP-18 gene in human leukemia cells. Leuk. Res. 2003, 27, 947–950. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.K.; Yiu Sung, J.J.; To, K.F.; Yu, L.; Li, H.T.; Li, Z.J.; Chu, K.M.; Yu, J.; Cho, C.H. The host defense peptide LL-37 activates the tumor-suppressing bone morphogenetic protein signaling via inhibition of proteasome in gastric cancer cells. J. Cell. Physiol. 2010, 223, 178–186. [Google Scholar] [CrossRef] [PubMed]
- Heilborn, J.D.; Nilsson, M.F.; Chamorro Jimenez, C.I.; Sandstedt, B.; Borregaard, N.; Tham, E.; Sørensen, O.E.; Weber, G.; Ståhle, M. Antimicrobial protein hCAP18/LL-37 is highly expressed in breast cancer and is a putative growth factor for epithelial cells. Int. J. Cancer 2005, 114, 713–719. [Google Scholar] [CrossRef] [PubMed]
- Coffelt, S.B.; Waterman, R.S.; Florez, L.; Höner zu Bentrup, K.; Zwezdaryk, K.J.; Tomchuck, S.L.; LaMarca, H.L.; Danka, E.S.; Morris, C.A.; Scandurro, A.B. Ovarian cancers overexpress the antimicrobial protein hCAP-18 and its derivative LL-37 increases ovarian cancer cell proliferation and invasion. Int. J. Cancer 2008, 122, 1030–1039. [Google Scholar] [CrossRef]
- von Haussen, J.; Koczulla, R.; Shaykhiev, R.; Herr, C.; Pinkenburg, O.; Reimer, D.; Wiewrodt, R.; Biesterfeld, S.; Aigner, A.; Czubayko, F.; et al. The host defence peptide LL-37/hCAP-18 is a growth factor for lung cancer cells. Lung Cancer 2008, 59, 12–23. [Google Scholar] [CrossRef]
- Ren, S.X.; Cheng, A.S.; To, K.F.; Tong, J.H.; Li, M.S.; Shen, J.; Wong, C.C.; Zhang, L.; Chan, R.L.; Wang, X.J.; et al. Host immune defense peptide LL-37 activates caspase-independent apoptosis and suppresses colon cancer. Cancer Res. 2012, 72, 6512–6523. [Google Scholar] [CrossRef]
- Colle, J.H.; Périchon, B.; Garcia, A. Antitumor and antibacterial properties of virally encoded cationic sequences. Biol. Targets Ther. 2019, 13, 117–126. [Google Scholar] [CrossRef]
- Coelho Neto, G.T.; de Lima, T.M.; Barbeiro, H.V.; Chammas, R.; César Machado, M.C.; da Silva, F.P. Cathelicidin LL-37 Promotes or Inhibits Cancer Cell Stemness Depending on the Tumor Origin. Oncomedicine 2016, 1, 14–17. [Google Scholar] [CrossRef][Green Version]
- Bolintineanu, D.; Hazrati, E.; Davis, H.T.; Lehrer, R.I.; Kaznessis, Y.N. Antimicrobial mechanism of pore-forming protegrin peptides: 100 pores to kill E. coli. Peptides 2010, 31, 1–8. [Google Scholar] [CrossRef]
- Edwards, I.A.; Elliott, A.G.; Kavanagh, A.M.; Zuegg, J.; Blaskovich, M.A.T.; Cooper, M.A. Contribution of Amphipathicity and Hydrophobicity to the Antimicrobial Activity and Cytotoxicity of β-Hairpin Peptides. ACS Infect. Dis. 2016, 2, 442–450. [Google Scholar] [CrossRef]
- Drin, G.; Temsamani, J. Translocation of protegrin I through phospholipid membranes: Role of peptide folding. Biochim. Et Biophys. Acta 2002, 1559, 160–170. [Google Scholar] [CrossRef]
- Lipkin, R.B.; Lazaridis, T. Implicit Membrane Investigation of the Stability of Antimicrobial Peptide β-Barrels and Arcs. J. Membr. Biol. 2015, 248, 469–486. [Google Scholar] [CrossRef]
- Lam, K.L.; Wang, H.; Siaw, T.A.; Chapman, M.R.; Waring, A.J.; Kindt, J.T.; Lee, K.Y. Mechanism of structural transformations induced by antimicrobial peptides in lipid membranes. Biochim. Et Biophys. Acta 2012, 1818, 194–204. [Google Scholar] [CrossRef]
- Paredes-Gamero, E.J.; Martins, M.N.; Cappabianco, F.A.; Ide, J.S.; Miranda, A. Characterization of dual effects induced by antimicrobial peptides: Regulated cell death or membrane disruption. Biochim. Et Biophys. Acta 2012, 1820, 1062–1072. [Google Scholar] [CrossRef]
- Soletti, R.C.; del Barrio, L.; Daffre, S.; Miranda, A.; Borges, H.L.; Moura-Neto, V.; Lopez, M.G.; Gabilan, N.H. Peptide gomesin triggers cell death through L-type channel calcium influx, MAPK/ERK, PKC and PI3K signaling and generation of reactive oxygen species. Chem.-Biol. Interact. 2010, 186, 135–143. [Google Scholar] [CrossRef]
- Cruz-Chamorro, L.; Gwak, J.W.; Kamarajan, P.; Fenno, J.C.; Rickard, A.H.; Kapila, Y.L. In vitro biological activities of magainin alone or in combination with nisin. Peptides 2006, 27, 1201–1209. [Google Scholar] [CrossRef]
- Soundrarajan, N.; Park, S.; Van Chanh, Q.L.; Cho, H.-S.; Raghunathan, G.; Ahn, B.; Song, H.; Kim, J.-H.; Park, C. Protegrin-1 cytotoxicity towards mammalian cells positively correlates with the magnitude of conformational changes of the unfolded form upon cell interaction. Sci. Rep. 2019, 9, 11569. [Google Scholar] [CrossRef]






| Compounds | N | Monotherapy, IC50 µM | NGF + Chemotherapy, IC50 µM | LL37 + Chemotherapy, IC50 µM | PG1 + Chemotherapy, IC50 µM |
|---|---|---|---|---|---|
| MTT test | |||||
| Doxorubicin | 3 | 1554.98 ± 207.5 | 600.5 ± 55.75 | 5265.5 ± 1031.0 | 730.9 ± 12.43 |
| Carboplatin | 3 | 3652.9 ± 670.8 | 2880.6 ± 275.5 | 3513.3 ± 493.0 | 2938.9 ± 529.7 |
| Temozolomide | 3 | 1725.7 ± 494.0 | 16,804.0 ± 937.4 | 4007.0 ± 365.5 | 9761.7 ± 997.0 |
| Cisplatin | 3 | 371.5 ± 23.50 | 207.4 ± 8.477 | 869 ± 107.5 | 237.9 ± 29.83 |
| Etoposide | 3 | 25.90 ± 0.61 | 13.7 ± 0.1129 | 17.9 ± 3.03 | 17.0 ± 1.80 |
| NGF (nM) | 3 | 2.14 ± 5.0 | |||
| LL-37 | 3 | 3.1 ± 0.4063 | |||
| PG-1 | 3 | 26.1 ± 7.6 |
| Compounds | PG1 + Chemotherapy | LL37 + Chemotherapy | NGF + Chemotherapy |
|---|---|---|---|
| MTT test | |||
| Doxorubicin | 0.94 additivity | 188.6 very strong antagonism | 2.42 antagonism |
| Carboplatin | 1.46 antagonism | 4.31 strong antagonism | 2.69 antagonism |
| Temozolomide | 6.04 strong antagonism | 8.95 strong antagonism | 9.73 strong antagonism |
| Cisplatin | 1.38 antagonism | 2.67 antagonism | 2.78 antagonism |
| Etoposide | 0.65 synergy | 1.85 antagonism | 2.34 antagonism |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chernov, A.; Kudryavtsev, I.; Komlev, A.; Alaverdian, D.; Tsapieva, A.; Galimova, E.; Shamova, O. Nerve Growth Factor, Antimicrobial Peptides and Chemotherapy: Glioblastoma Combination Therapy to Improve Their Efficacy. Biomedicines 2023, 11, 3009. https://doi.org/10.3390/biomedicines11113009
Chernov A, Kudryavtsev I, Komlev A, Alaverdian D, Tsapieva A, Galimova E, Shamova O. Nerve Growth Factor, Antimicrobial Peptides and Chemotherapy: Glioblastoma Combination Therapy to Improve Their Efficacy. Biomedicines. 2023; 11(11):3009. https://doi.org/10.3390/biomedicines11113009
Chicago/Turabian StyleChernov, Alexandr, Igor Kudryavtsev, Aleksei Komlev, Diana Alaverdian, Anna Tsapieva, Elvira Galimova, and Olga Shamova. 2023. "Nerve Growth Factor, Antimicrobial Peptides and Chemotherapy: Glioblastoma Combination Therapy to Improve Their Efficacy" Biomedicines 11, no. 11: 3009. https://doi.org/10.3390/biomedicines11113009
APA StyleChernov, A., Kudryavtsev, I., Komlev, A., Alaverdian, D., Tsapieva, A., Galimova, E., & Shamova, O. (2023). Nerve Growth Factor, Antimicrobial Peptides and Chemotherapy: Glioblastoma Combination Therapy to Improve Their Efficacy. Biomedicines, 11(11), 3009. https://doi.org/10.3390/biomedicines11113009