Analysis of Suicide Methods and Substances Influencing the State of Consciousness of Their Victims in Poland
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gawliński, A.; Sołtyszewski, I.; Wiergowski, M. Epidemiology of suicides in Poland in 1990–2018-changes and new trends. Arch. Med. Sądowej I Kryminol. 2020, 70, 222–234. [Google Scholar]
- Plans, L.; Barrot, C.; Nieto, E.; Rios, J.; Schulze, T.; Papiol, S.; Mitjans, M.; Vieta, E.; Benabarre, A. Association between completed suicide and bipolar disorder: A systematic review of the literature. J. Affect. Disord. 2019, 242, 111–122. [Google Scholar] [CrossRef] [PubMed]
- Mann, J.J. Neurobiology of suicidal behaviour. Nat. Rev. Neurosci. 2003, 4, 819–828. [Google Scholar] [CrossRef] [PubMed]
- Ziółkowski, M.; Czarnecki, D.; Chodkiewicz, J.; Gąsior, K.; Juczyński, A.; Biedrzycka, A.; Gruszczyńska, E.; Nowakowska-Domagała, K. Suicidal thoughts in persons treated for alcohol dependence: The role of selected demographic and clinical factors. Psychiatry Res. 2017, 258, 501–505. [Google Scholar] [CrossRef] [PubMed]
- Jakubczyk, A.; Klimkiewicz, A.; Krasowska, A.; Kopera, M.; Sławińska-Ceran, A.; Brower, K.; Wojnar, M. History of sexual abuse and suicide attempts in alcohol-dependent patients. Child Abuse Negl. 2014, 38, 1560–1568. [Google Scholar] [CrossRef] [Green Version]
- Wojnar, M.; Ilgen, M.A.; Jakubczyk, A.; Wnorowska, A.; Klimkiewicz, A.; Brower, K.J. Impulsive suicide attempts predict post-treatment relapse in alcohol-dependent patients. Drug Alcohol Depend. 2008, 97, 268–275. [Google Scholar] [CrossRef] [Green Version]
- Sher, L.; Oquendo, M.A.; Mann, J. Risk of suicide in mood disorders. Clin. Neurosci. Res. 2001, 1, 337–344. [Google Scholar] [CrossRef]
- Sher, L.; Grunebaum, M.F.; Burke, A.K.; Chaudhury, S.; Mann, J.J.; Oquendo, M.A. Depressed multiple-suicideattempters—A high-risk phenotype. Crisis 2017, 38, 367–375. [Google Scholar] [CrossRef]
- Borges, G.; Bagge, C.; Cherpitel, C.J.; Conner, K.; Orozco, R.; Rossow, I. A meta-analysis of acute use of alcohol and the risk of suicide attempt. Psychol. Med. 2017, 47, 949–957. [Google Scholar] [CrossRef] [Green Version]
- Klimkiewicz, A.; Serafin, P.; Wojnar, M. Risk factors of suicidal behavior in alcohol-dependent individuals. Psychiatria 2011, 8, 7–17. [Google Scholar]
- Sit, D.; Luther, J.; Buysse, D.; Dills, J.L.; Eng, H.; Okun, M.; Wisniewski, S.; Wisner, K.L. Suicidal ideation in depressed postpartum women: Associations with childhood trauma, sleep disturbance and anxiety. J. Psychiatr. Res. 2015, 66–67, 95–104. [Google Scholar] [CrossRef] [Green Version]
- Landheim, A.; Bakken, K.; Vaglum, P. What Characterizes Substance Abusers Who Commit Suicide Attempts? Factors Related to Axis I Disorders and Patterns of Substance Use Disorders. Eur. Addict. Res. 2006, 12, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Knipe, D.; Williams, A.J.; Hannam-Swain, S.; Upton, S.; Brown, K.; Bandara, P.; Chang, S.-S.; Kapur, N. Psychiatric morbidity and suicidal behaviour in low- and middle-income countries: A systematic review and meta-analysis. PLoS Med. 2019, 16, e1002905. [Google Scholar] [CrossRef]
- Headquarters of Polish Police. Prevention and Analysis Office of the Road Traffic. Available online: http://statystyka.policja.pl/st/ruch-drogowy/76562,Wypadki-drogowe-raporty-roczne.html (accessed on 5 September 2018). (In Polish).
- Phillips, M.R.; Yang, G.; Zhang, Y.; Wang, L.; Ji, H.; Zhou, M. Risk factors for suicide in China: A national case-control psychological autopsy study. Lancet 2002, 360, 1728–1736. [Google Scholar] [CrossRef]
- Patel, V.; Ramasundarahettige, C.; Vijayakumar, L.; Thakur, J.; Gajalakshmi, V.; Gururaj, G.; Suraweera, W.; Jha, P. Suicide mortality in India: A nationally representative survey. Lancet 2012, 379, 2343–2351. [Google Scholar] [CrossRef] [Green Version]
- Olszańska, E.; Turska, M.; Balcerowicz, S.; Chobot, A.; Jaszczura, M.; Rojewska, K.; Kwiecień, J. Analysis of suicide attempts among children hospitalised in the Department of Paediatrics in Zabrze in 2010–2016. Pediatr. Pol. Pol. J. Paediatr. 2018, 93, 367–371. [Google Scholar] [CrossRef]
- Lasota, D.; Pawłowski, W.; Krajewski, P.; Staniszewska, A.; Goniewicz, K.; Goniewicz, M. Seasonality of Suicides among Victims Who Are under the Influence of Alcohol. Int. J. Environ. Res. Public Health 2019, 16, 2806. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lasota, D.; Pawłowski, W.; Mirowska-Guzel, D.; Goniewicz, K.; Goniewicz, M. Ethanol as a stimulus to risky and auto-aggressive behaviour. Ann. Agric. Environ. Med. 2020. [Google Scholar] [CrossRef]
- Lasota, D.; Pawłowski, W.; Krajewski, P.; Staniszewska, A.; Goniewicz, K.; Czerski, R.; Goniewicz, M. Alcohol Intoxication and Suicide by Hanging in Poland. Alcohol Alcohol. 2020, 55, 278–283. [Google Scholar] [CrossRef]
- Fudalej, S.; Ilgen, M.; Kołodziejczyk, I.; Podgórska, A.; Serafin, P.; Barry, K.; Wojnar, M.; Blow, F.C.; Bohnert, A. Somatic Comorbidity and Other Factors Related to Suicide Attempt Among Polish Methadone Maintenance Patients. J. Addict. Med. 2015, 9, 433–439. [Google Scholar] [CrossRef] [Green Version]
- Lasota, D.; Al-Wathinani, A.; Krajewski, P.; Mirowska-Guzel, D.; Goniewicz, K.; Hertelendy, A.J.; Alhazmi, R.A.; Pawłowski, W.; Khorram-Manesh, A.; Goniewicz, M. Alcohol and the Risk of Railway Suicide. Int. J. Environ. Res. Public Health 2020, 17, 7003. [Google Scholar] [CrossRef]
- Schneider, B. Substance Use Disorders and Risk for Completed Suicide. Arch. Suicide Res. 2009, 13, 303–316. [Google Scholar] [CrossRef]
- Bohnert, K.M.; Ilgen, M.A.; McCarthy, J.F.; Ignacio, R.V.; Blow, F.C.; Katz, I.R. Tobacco use disorder and the risk of suicide mortality. Addiction 2013, 109, 155–162. [Google Scholar] [CrossRef]
- Armstrong, G.; Vijayakumar, L.; Niederkrotenthaler, T.; Jayaseelan, M.; Kannan, R.; Pirkis, J.; Jorm, A.F. Assessing the quality of media reporting of suicide news in India against World Health Organization guidelines: A content analysis study of nine major newspapers in Tamil Nadu. Aust. N. Z. J. Psychiatry 2018, 52, 856–863. [Google Scholar] [CrossRef]
- Krahé, B. The Social Psychology of Aggression; Routledge: New York, NY, USA, 2020. [Google Scholar]
- Gutwinski, S.; Heinz, A.J.; Heinz, A. Alcohol-Related Aggression and Violence. Wiley Blackwell Handb. Forensic Neurosci. 2018, 1, 455–480. [Google Scholar]
- Puuskari, V.; Aalto-Setälä, T.; Komulainen, E.; Marttunen, M. Suicidal ideation, suicide attempts, and psychological distress among intoxicated adolescents in the pediatric emergency department. Nord. J. Psychiatry 2017, 72, 137–144. [Google Scholar] [CrossRef]
- Kuhns, J.B.; Exum, M.L.; Clodfelter, T.A.; Bottia, M.C. The prevalence of alcohol-involved homicide offending: A meta-analytic review. Homicide Stud. 2014, 18, 251–270. [Google Scholar] [CrossRef]
- Steelesmith, D.L. County Level Suicide Rates in the United States from 2000 to 2014: Changes Over Time and Associations with Contextual Factors; The Ohio State University: Columbus, OH, USA, 2018. [Google Scholar]
- Weiss, D.B.; Testa, A.; Santos, M.R. Hazardous Alcohol Drinking and Cross-National Homicide Rates: The Role of Demographic, Political, and Cultural Context. J. Drug Issues 2018, 48, 246–268. [Google Scholar] [CrossRef]
- Razvodovsky, Y.E. Beverage-Specific Alcohol Sale and Suicide in Russia. Crisis 2009, 30, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Butler, S.; Elmeland, K.; Thom, B.; Nicholls, J. Alcohol, Power and Public Health: A Comparative Study of Alcohol Policy; Taylor & Francis: Abingdon, UK, 2017. [Google Scholar]
- Amiri, S.; Behnezhad, S. Alcohol use and risk of suicide: A systematic review and Meta-analysis. J. Addict. Dis. 2020, 38, 200–213. [Google Scholar] [CrossRef] [PubMed]
- Leenaars, A. Death Systems and Suicide Around the World. Death Bereave. World Reflect. Essays 2009, 5, 5. [Google Scholar] [CrossRef]
- Holder, H.D.; Kühlhorn, E.; Nordlund, S.; Österberg, E.; Romelsjö, A.; Ugland, T. European Integration and Nordic Alcohol Policies: Changes in Alcohol Controls and Consequences in Finland, Norway and Sweden, 1980–1997; Routledge: Abingdon, UK, 2019. [Google Scholar]
- Stockwell, T.; Sherk, A.; Norström, T.; Angus, C.; Ramstedt, M.; Andréasson, S.; Chikritzhs, T.; Gripenberg, J.; Holder, H.; Holmes, J.; et al. Estimating the public health impact of disbanding a government alcohol monopoly: Application of new methods to the case of Sweden. BMC Public Health 2018, 18, 1400. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aaltonen, K.I.; Isometsä, E.; Sund, R.; Pirkola, S. Risk factors for suicide in depression in Finland: First-hospitalized patients followed up to 24 years. Acta Psychiatr. Scand. 2018, 139, 154–163. [Google Scholar] [CrossRef] [PubMed]
- Bilban, M.; Škibin, L. Presence of alcohol in suicide victims. Forensic Sci. Int. 2005, 147, S9–S12. [Google Scholar] [CrossRef]
- Bachmann, S. Epidemiology of Suicide and the Psychiatric Perspective. Int. J. Environ. Res. Public Health 2018, 15, 1425. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hallfors, D.D.; Waller, M.W.; Bauer, D.; Ford, C.A.; Halpern, C.T. Which Comes First in Adolescence—Sex and Drugs or Depression? Am. J. Prev. Med. 2005, 29, 163–170. [Google Scholar] [CrossRef]
- Guerzoni, S.; Pellesi, L.; Pini, L.A.; Caputo, F.; Simona, G.; Lanfranco, P.; Alberto, P.L.; Fabio, C. Drug-drug interactions in the treatment for alcohol use disorders: A comprehensive review. Pharmacol. Res. 2018, 133, 65–76. [Google Scholar] [CrossRef]
- Ksiądzyna, D.; Merwid-Ląd, A.; Matuszewska, A.; Grotthus, B.; Szeląg, A. Withdrawal symptoms of selected drugs. Part II. Med. Rodz. 2019, 1, 33–40. [Google Scholar]
- Raport Teen Marihuana Use Worsnes Depression: An Anaslysis of Recent Data Shows Self Medicating Could Make Things Worse, Office of Natinal Drug Policy Executive of the President. 2008. Available online: https://www.ncjrs.gov/ondcppubs/publications/pdf/marij_mental_hlth.pdf–dostęp (accessed on 20 May 2016).
- Putowski, M.; Piróg, M.; Podgórniak, M.; Zawiślak, J.; Piecewicz-Szczęsna, H. Analiza epidemiologiczna występowania samobójstw w Polsce w latach 2000–2013. Probl. Hig. Epidemiol. 2015, 96, 264–268. [Google Scholar]
- Chmielowska-Marmucka, A. Wpływ dopalaczy i innych substancji psychoaktywnych na funkcjonowanie ludzkiego organizmu. Medyczno-psychologiczne i prawne aspekty. Oblicza Przestępczości 2015, 175–184. Available online: https://core.ac.uk/download/pdf/48037193.pdf#page=175 (accessed on 24 March 2021).
- Zawilska, J.B.; Słomiak, K.; Wasiak, M.; Woźniak, P.; Massalski, M.; Krupa, E.; Wojcieszak, J.Ł. Beta-cathinone derivatives—A new generation of dangerous psychostimulant “designer drugs”. Prz. Lek. 2013, 70, 386–391. [Google Scholar]
- Ostaszewski, K. Używanie substancji psychoaktywnych jako przejaw zachowań ryzykownych młodzieży szkolnej. Dziecko krzywdzone. Teor. Bad. Prakt. 2017, 16, 132–145. [Google Scholar]
- Haerian, K.; Salmasian, H.; Friedman, C. Methods for Identifying Suicide or Suicidal Ideation in EHRs. In Proceedings of the AMIA Annual Symposium, American Medical Informatics Association, Bethesda, MD, USA, 3 November 2012; Volume 2012, pp. 1244–1253. [Google Scholar]
- National Violent Death Reporting System (NVDRS). Coding Manual, Version 3; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2014. Available online: http://www.cdc.gov/violenceprevention/pdf/NVDRS_Coding_Manual_Version_3-a.pdf (accessed on 15 May 2014).
- Paulozzi, L.J.; Mercy, J.; Frazier, L., Jr.; Annest, J.L. CDC’s National Violent Death Reporting System: Background and methodology. Inj. Prev. 2004, 10, 47–52. [Google Scholar] [CrossRef] [Green Version]
- General Police Headquarters of Poland: Zamachy Samobójcze od 2017 (Suicide Attempts Since 2017). Available online: http://www.statystyka.policja.pl/st/wybrane-statystyki/zamachy-samobojcze/63803/ (accessed on 21 November 2018). (In Polish).
- Central Statistical Office of Poland. Available online: https://stat.gov.pl/ (accessed on 1 October 2019). (In Polish)
- Lavigne, J.E.; Lagerberg, T.; Ambrosi, J.W.; Chang, Z. Study designs and statistical approaches to suicide and prevention research in real-world data. Suicide Life-Threat. Behav. 2021, 51, 127–136. [Google Scholar] [CrossRef]
- Polish National Health Program for 2016–2020. Available online: http://www.archiwum.mz.gov.pl/zdrowie-i-profilaktyka/narodowy-program-zdrowia/npz-2016-2020/ (accessed on 13 January 2021).
- Stecz, P. Psychometric evaluation of the Questionnaire on Attitudes Towards Suicide (ATTS) in Poland. Curr. Psychol. 2019, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Orlewska, K.; Orlewska, E. Burden of suicide in Poland in 2012: How could it be measured and how big is it? Eur. J. Health Econ. 2017, 19, 409–417. [Google Scholar] [CrossRef] [Green Version]
- Łyszczarz, B. Production Losses Associated with Alcohol-Attributable Mortality in the European Union. Int. J. Environ. Res. Public Health 2019, 16, 3536. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goniewicz, K.; Carlström, E.; Hertelendy, A.; Burkle, F.; Goniewicz, M.; Lasota, D.; Richmond, J.; Khorram-Manesh, A. Integrated Healthcare and the Dilemma of Public Health Emergencies. Sustainability 2021, 13, 4517. [Google Scholar] [CrossRef]
- Kaminskaite, M.; Pranckeviciene, A.; Bunevicius, A.; Janaviciute, J.; Jokubonis, D.; Plioplyte, A.; Lelyte, I.; Sinkariova, L.; Jokubka, R. Validation of the Substance Use Risk Profile Scale in Lithuanian population. Health Qual. Life Outcomes 2020, 18, 1–12. [Google Scholar] [CrossRef]
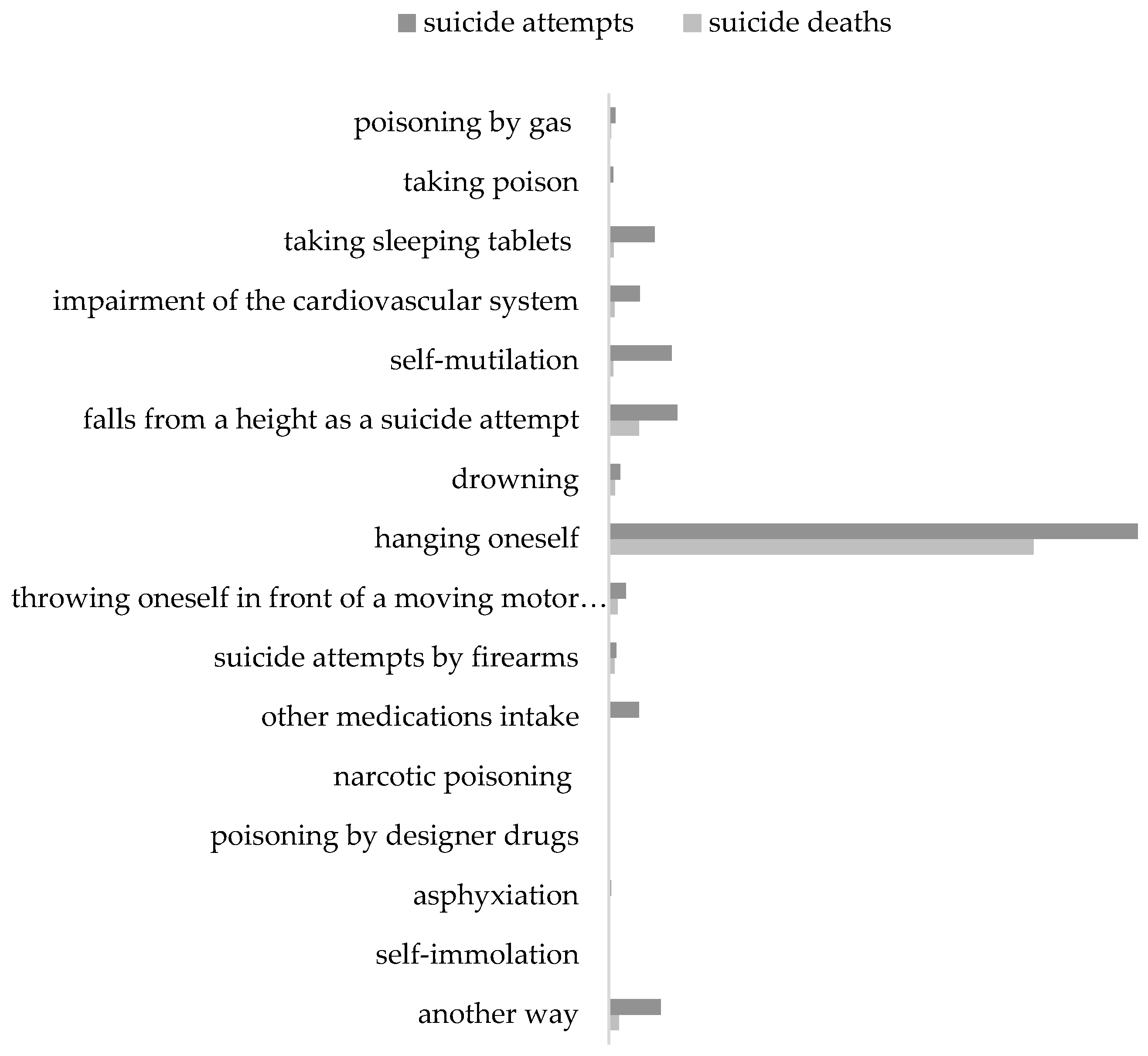
| Method | Number and Percentage of Suicide Attempts Victims | General | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | ||
| Poisoning by gas/exhaust fumes | 41 (0.69) | 38 (0.70) | 39 (0.76) | 33 (0.57) | 47 (0.55) | 67 (0.66) | 85 (0.85) | 73 (0.74) | 92 (0.83) | 104 (0.93) | 114 (0.95) | 733 (0.77) |
| Poisoning with chemicals/ toxic substances | 30 (0.51) | 26 (0.48) | 20 (0.39) | 30 (0.52) | 41 (0.48) | 52 (0.51) | 52 (0.52) | 49 (0.49) | 62 (0.56) | 68 (0.61) | 89 (0.74) | 519 (0.55) |
| Taking sleeping tablets/psychotropic tablets | 199 (3.36) | 214 (3.92) | 192 (3.75) | 193 (3.33) | 314 (3.69) | 474 (4.64) | 520 (5.22) | 572 (5.80) | 674 (6.05) | 774 (6.93) | 894 (7.48) | 5020 (5.28) |
| Impairment of the cardiovascular system | 156 (2.64) | 154 (2.82) | 155 (3.02) | 143 (2.47) | 226 (2.66) | 370 (3.62) | 367 (3.68) | 393 (3.99) | 388 (3.48) | 501 (4.49) | 524 (4.38) | 3377 (3.55) |
| Superficial self-mutilation | 227 (3.84) | 191 (3.50) | 179 (3.49) | 215 (3.71) | 400 (4.70) | 652 (6.39) | 788 (7.90) | 816 (8.28) | 991 (8.90) | 1095 (9.80) | 1299 (10.86) | 6853 (7.20) |
| Falls from a height as a suicide attempt | 408 (6.90) | 323 (5.92) | 325 (6.34) | 443 (7.65) | 675 (7.94) | 856 (8.39) | 877 (8.79) | 798 (8.09) | 934 (8.38) | 911 (8.16) | 912 (7.63) | 7462 (7.85) |
| Drowning | 108 (1.83) | 88 (1.61) | 100 (1.95) | 105 (1.82) | 118 (1.39) | 113 (1.11) | 119 (1.19) | 126 (1.28) | 127 (1.14) | 117 (1.05) | 114 (0.95) | 1235 (1.29) |
| Hanging oneself | 4265 (72.13) | 3973 (72.82) | 3706 (72.33) | 4059 (70.09) | 5955 (70.01) | 6582 (64.49) | 6066 (60.82) | 5819 (59.01) | 5966 (53.55) | 5609 (50.23) | 5740 (47.99) | 57,740 (60.72) |
| Throwing oneself in front of a moving motor vehicle | 81 (1.37) | 103 (1.89) | 77 (1.50) | 110 (1.90) | 158 (1.86) | 184 (1.80) | 207 (2.08) | 216 (2.19) | 241 (2.16) | 222 (1.99) | 275 (2.30) | 1874 (1.97) |
| Suicide attempts by firearms | 46 (0.78) | 44 (0.81) | 32 (0.63) | 58 (1.00) | 83 (0.98) | 86 (0.84) | 79 (0.79) | 104 (1.05) | 90 (0.81) | 96 (0.86) | 102 (0.85) | 820 (0.86) |
| Other medications intake | - | - | - | - | - | - | - | - | 959 (8.61) | 1061 (9.50) | 1289 (10.78) | 3309 (3.48) |
| Narcotic poisoning | - | - | - | - | - | - | - | - | 21 (0.19) | 17 (0.15) | 19 (0.16) | 57 (0.06) |
| Poisoning by designer drugs | - | - | - | - | - | - | - | - | 3 (0.03) | 3 (0.03) | 0 (0.00) | 6 (0.01) |
| Asphyxiation | - | - | - | - | - | - | - | - | 89 (0.80) | 84 (0.75) | 93 (0.78) | 266 (0.28) |
| Self-immolation | - | - | - | - | - | - | - | - | 48 (0.43) | 54 (0.48) | 40 (0.33) | 142 (0.15) |
| Another way | 352 (5.95) | 302 (5.53) | 299 (5.84) | 402 (6.94) | 488 (5.74) | 771 (7.55) | 813 (8.16) | 895 (9.08) | 454 (4.08) | 451 (4.04) | 457 (3.82) | 5684 (5.98) |
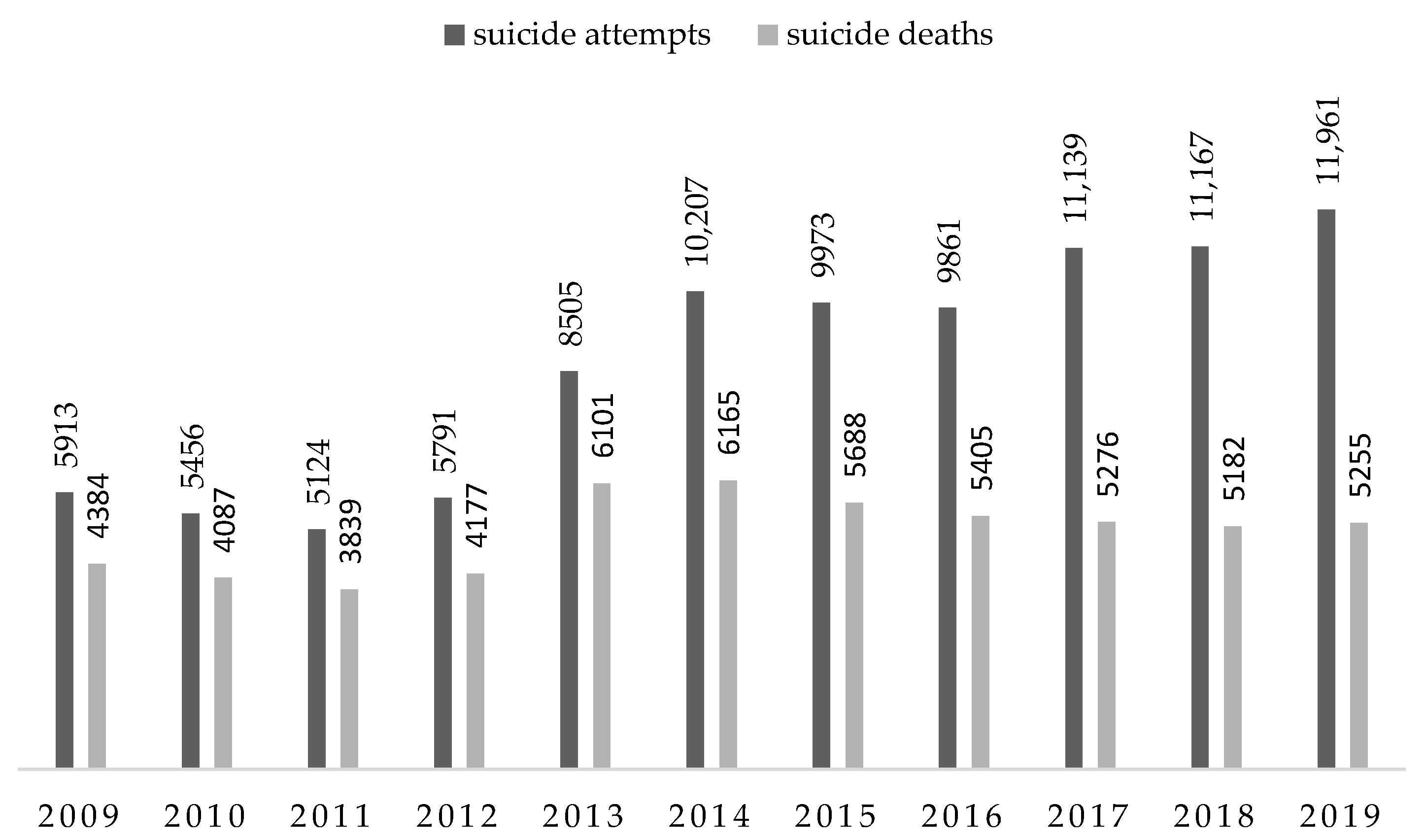
| Overall | 5913 (6.22) | 5456 (5.74) | 5124 (5.39) | 5791 (6.09) | 8505 (8.94) | 10,207 (10.73) | 9973 (10.49) | 9861 (10.37) | 11,139 (11.71) | 11,167 (11.74) | 11,961 (12.58) | 95,097 (100.00) |
| Method | Number and Percentage of Suicide Deaths Victims | General | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | ||
| Poisoning by gas/exhaust fumes | 11 (0.25) | 17 (0.42) | 25 (0.65) | 13 (0.31) | 15 (0.25) | 18 (0.30) | 37 (0.65) | 21 (0.40) | 29 (0.55) | 38 (0.73) | 41 (0.78) | 265 (0.48) |
| Poisoning with chemicals/ toxic substances | 15 (0.34) | 11 (0.27) | 9 (0.24) | 13 (0.31) | 14 (0.23) | 14 (0.23) | 19 (0.33) | 13 (0.24) | 17 (0.32) | 12 (0.23) | 24 (0.46) | 161 (0.29) |
| Taking sleeping tablets/psychotropic tablets | 33 (0.75) | 38 (0.93) | 41 (1.07) | 37 (0.88) | 59 (0.97) | 69 (1.12) | 45 (0.79) | 66 (1.22) | 44 (0.83) | 48 (0.93) | 50 (0.95) | 530 (0.95) |
| Impairment of the cardiovascular system | 38 (0.87) | 39 (0.95) | 33 (0.86) | 36 (0.86) | 56 (0.92) | 53 (0.86) | 62 (1.10) | 51 (0.94) | 75 (1.42) | 83 (1.60) | 96 (1.83) | 622 (1.12) |
| Superficial self-mutilation | 40 (0.91) | 31 (0.76) | 30 (0.78) | 30 (0.72) | 57 (0.93) | 54 (0.88) | 69 (1.21) | 71 (1.31) | 46 (0.87) | 36 (0.69) | 38 (0.72) | 502 (0.90) |
| Falls from a height as a suicide attempt | 231 (5.27) | 165 (4.04) | 185 (4.82) | 243 (5.82) | 392 (6.43) | 373 (6.05) | 361 (6.35) | 344 (6.36) | 342 (6.48) | 330 (6.37) | 330 (6.28) | 3296 (5.93) |
| Drowning | 80 (1.82) | 69 (1.69) | 78 (2.03) | 78 (1.87) | 73 (1.20) | 52 (0.84) | 51 (0.90) | 65 (1.20) | 57 (1.08) | 46 (0.89) | 45 (0.86) | 694 (1.25) |
| Hanging oneself | 3726 (85.00) | 3518 (86.08) | 3274 (85.28) | 3495 (83.67) | 5142 (84.30) | 5241 (85.01) | 4748 (83.47) | 4473 (82.76) | 4313 (81.75) | 4211 (81.26) | 4240 (80.68) | 46 381 (83.48) |
| Throwing oneself in front of a moving motor vehicle | 60 (1.37) | 77 (1.88) | 50 (1.30) | 76 (1.82) | 99 (1.62) | 91 (1.47) | 90 (1.58) | 100 (1.85) | 105 (1.99) | 105 (2.03) | 132 (2.51) | 985 (1.77) |
| Suicide attempts by firearms | 37 (0.84) | 39 (0.95) | 30 (0.78) | 47 (1.13) | 67 (1.10) | 63 (1.02) | 53 (0.93) | 70 (1.30) | 72 (1.36) | 79 (1.52) | 86 (1.64) | 643 (1.16) |
| Other medications intake | - | - | - | - | - | - | - | - | 58 (1.10) | 61 (1.18) | 63 (1.20) | 182 (0.33) |
| Narcotic poisoning | - | - | - | - | - | - | - | - | 4 (0.08) | 3 (0.06) | 4 (0.07) | 11 (0.02) |
| Poisoning by designer drugs | - | - | - | - | - | - | - | - | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| Asphyxiation | - | - | - | - | - | - | - | - | 49 (0.93) | 45 (0.87) | 44 (0.84) | 138 (0.25) |
| Self-immolation | - | - | - | - | - | - | - | - | 12 (0.23) | 15 (0.29) | 11 (0.21) | 38 (0.07) |
| Another way | 113 (2.58) | 83 (2.03) | 84 (2.19) | 109 (2.61) | 125 (2.05) | 137 (2.22) | 153 (2.69) | 131 (2.42) | 53 (1.01) | 70 (1.35) | 51 (0.97) | 1109 (2.00) |
| Overall | 4384 (7.89) | 4087 (7.36) | 3839 (6.91) | 4177 (7.52) | 6101 (10.98) | 6165 (11.09) | 5688 (10.24) | 5405 (9.73) | 5276 (9.49) | 5182 (9.33) | 5255 (9.46) | 55 559 (100.00) |
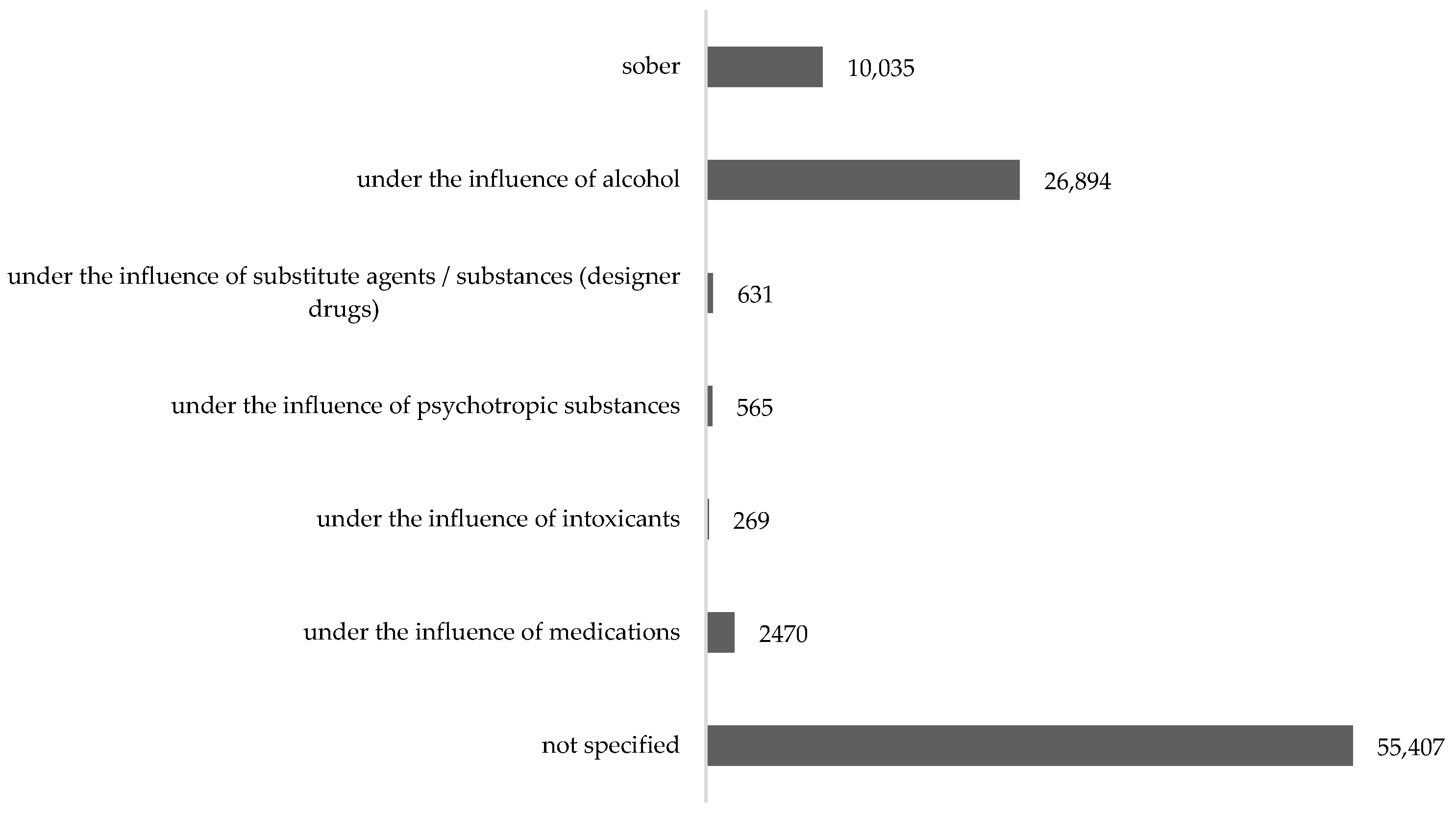
| Consciousness Level | Number and Percentage of Suicide Attempts Victims | General | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | ||
| Sober | 668 (11.29) | 592 (10.85) | 500 (9.76) | 618 (10.67) | 683 (8.03) | 901 (8.83) | 867 (8.69) | 987 (10.01) | 1306 (11.72) | 1342 (12.02) | 1571 (13.13) | 10 035 (10.42) |
| Under the influence of alcohol | 1453 (24.57) | 1341 (24.58) | 1258 (24.55) | 1438 (24.83) | 1857 (21.83) | 2734 (26.78) | 2841 (28.48) | 2899 (29.39) | 3635 (32.63) | 3634 (32.54) | 3804 (31.80) | 26 894 (27.94) |
| Under the influence of substitute agents/substances (designer drugs) | 44 (0.74) | 47 (0.86) | 31 (0.60) | 47 (0.81) | 66 (0.78) | 106 (1.04) | 118 (1.18) | 98 (0.99) | 31 (0.28) | 21 (0.19) | 22 (0.18) | 631 (0.65) |
| Under the influence of psychotropic substances | 44 (0.74) | 32 (0.59) | 27 (0.53) | 45 (0.78) | 62 (0.73) | 109 (1.07) | 133 (1.33) | 113 (1.15) | - | - | - | 565 (0.59) |
| Under the influence of intoxicants | - | - | - | - | - | - | - | - | 79 (0.71) | 92 (0.82) | 98 (0.82) | 269 (0.28) |
| Under the influence of medications | - | - | - | - | - | - | - | - | 732 (6.57) | 809 (7.24) | 929 (7.77) | 2470 (2.57) |
| Not specified/not established the agent | 3733 (63.13) | 3472 (63.64) | 3334 (65.06) | 3676 (63.48) | 5974 (70.24) | 6432 (60.02) | 6093 (61.09) | 5815 (58.96) | 5575 (50.05) | 5526 (49.49) | 5777 (48.30) | 55 407 (57.55) |
| Overall | 5942 (6.17) | 5484 (5.70) | 5150 (5.35) | 5824 (6.05) | 8642 (8.98) | 10,282 (10.68) | 10,052 (10.44) | 9912 (10.30) | 11,358 (11.79) | 11,424 (11.87) | 12,201 (12.67) | 96,271 (100.00) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lasota, D.; Mirowska-Guzel, D.; Goniewicz, K. Analysis of Suicide Methods and Substances Influencing the State of Consciousness of Their Victims in Poland. Int. J. Environ. Res. Public Health 2021, 18, 4936. https://doi.org/10.3390/ijerph18094936
Lasota D, Mirowska-Guzel D, Goniewicz K. Analysis of Suicide Methods and Substances Influencing the State of Consciousness of Their Victims in Poland. International Journal of Environmental Research and Public Health. 2021; 18(9):4936. https://doi.org/10.3390/ijerph18094936
Chicago/Turabian StyleLasota, Dorota, Dagmara Mirowska-Guzel, and Krzysztof Goniewicz. 2021. "Analysis of Suicide Methods and Substances Influencing the State of Consciousness of Their Victims in Poland" International Journal of Environmental Research and Public Health 18, no. 9: 4936. https://doi.org/10.3390/ijerph18094936







