Would the United States Have Had Too Few Beds for Universal Emergency Care in the Event of a More Widespread Covid-19 Epidemic?
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. Data Manipulation
3. Results
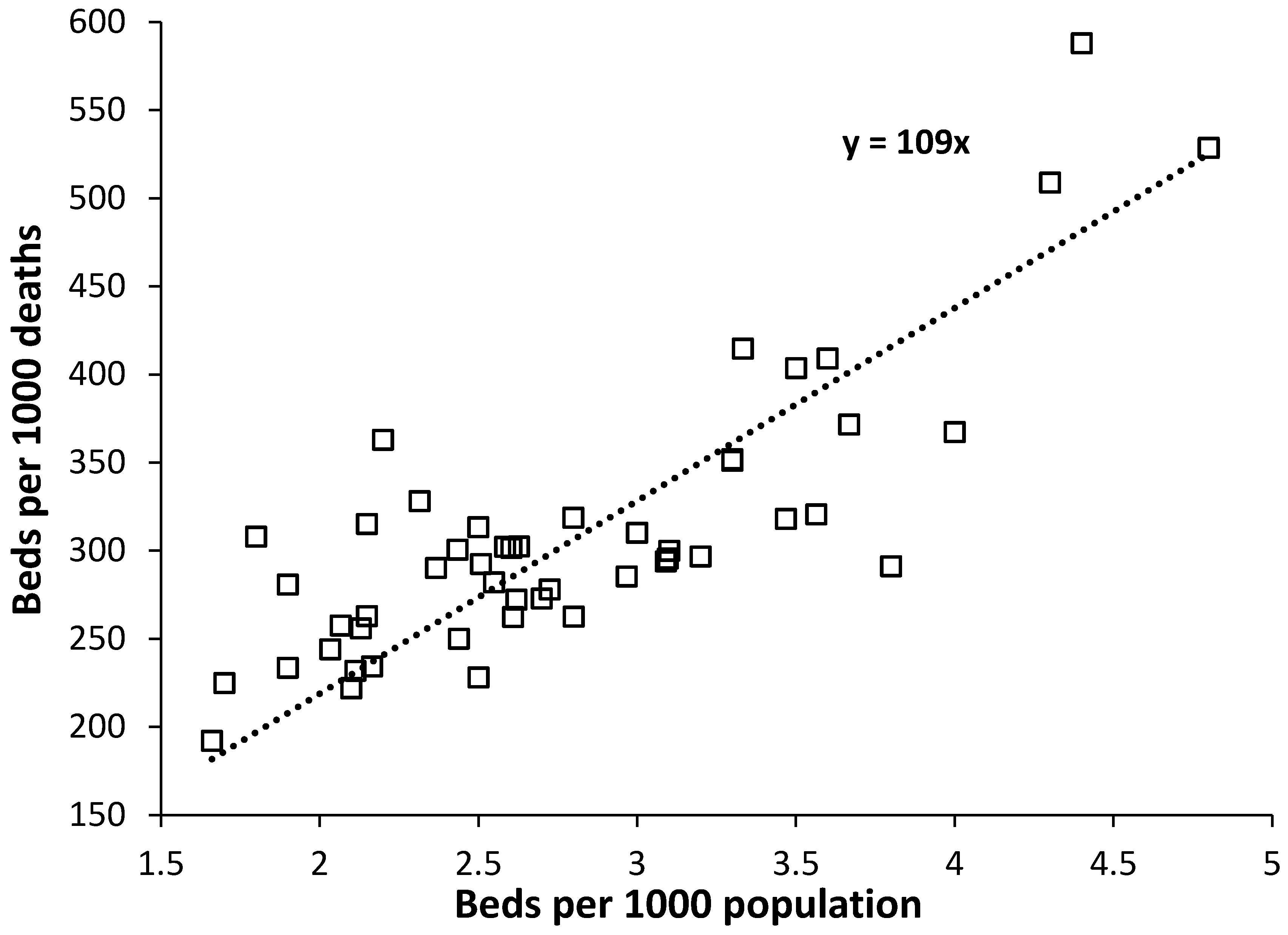
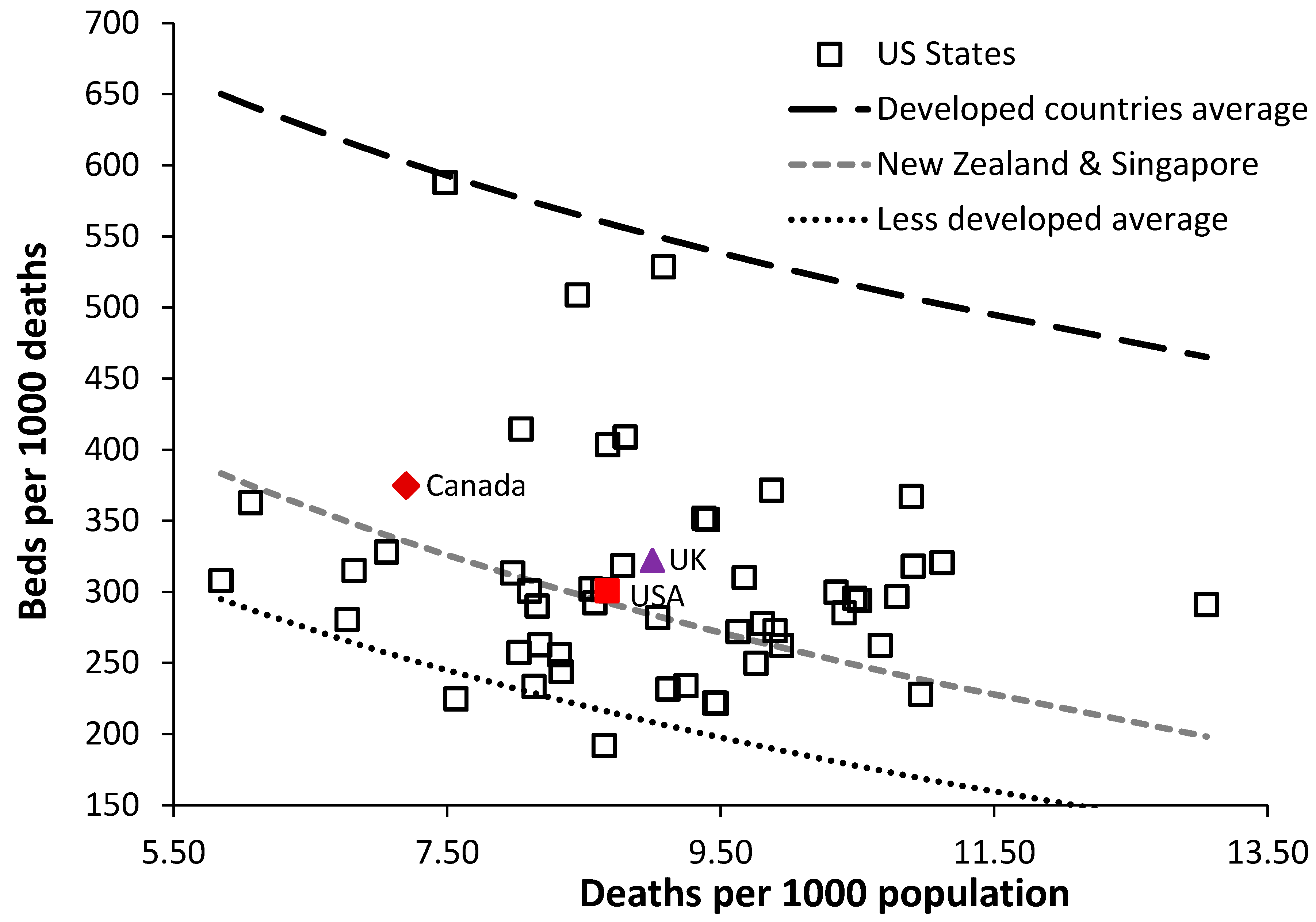
3.1. Beds per 1000 Population and Beds per 1000 Deaths Compared
3.2. Hospital Bed Numbers Compared
3.3. US States with the Least Beds
3.4. Population Density
3.5. Covid-19 Deaths per Bed
4. Discussion
4.1. Healthcare in the U.S.
4.2. Beds in the U.S.
4.3. Medical Beds
4.4. Critical Care Beds
4.5. Specifics to Covid-19
4.6. Population Density
4.7. Why Such Low Bed Numbers in Some States?
4.8. Limitations of the Study
4.9. Further Research
5. Conclusions
Funding
Conflicts of Interest
References
- Li, R.; Rivers, C.; Tan, Q.; Murray, M.B.; Toner, E.; Lipsitch, M. The demand for inpatient and ICU beds for COVID-19 in the US: Lessons from Chinese Cities. Harvard University. 2020. Available online: https://dash.harvard.edu/handle/1/42599304 (accessed on 23 April 2020).
- Argenziano, M.; Bruce, S.; Slater, C.; Tiao, J.; Baldwin, M.; Barr, R.G.; Chang, B.P.; Chau, K.H.; Choi, J.J.; Gavin, N.; et al. Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: Retrospective case series. BMJ 2020, 369, m1996. [Google Scholar] [CrossRef] [PubMed]
- Jombart, T.; Nightingale, E.; Jit, M.; le de Waroux, O.P.; Knight, G.; Flasche, S.; Eggo, R.M.; Kucharski, A.J.; Pearson, C.A.B.; Procter, S.R.; et al. Forecasting Critical Care Bed Requirements for COVID-19 Patients in England, CMMID Repository. 2020. Available online: https://cmmid.github.io/topics/covid19/current-patterns-transmission/ICU-projections.html (accessed on 23 April 2020).
- Kamerow, D. Covid-19: The crisis of personal protective equipment in the US. BMJ 2020, 369, m1367. [Google Scholar] [CrossRef] [PubMed]
- Bing. Com Coronavirus (COVID-19) Statistics. 2020. Available online: https://www.bing.com/search?q=covid+deaths+usa&cvid=8601784d98eb405d8fcd64fd5693255c&FORM=ANSPA1&PC=ASTS (accessed on 10 June 2020).
- The Commonwealth Fund. U.S. Health Care from a Global Perspective, 2019: Higher Spending, worse outcomes? The Commonwealth Fund. 2020. Available online: https://www.commonwealthfund.org/publications/issue-briefs/2020/jan/us-health-care-global-perspective-2019 (accessed on 23 April 2020).
- Ginzberg, E. The high cost of dying. Inquiry 1980, 17, 293–295. [Google Scholar] [PubMed]
- Garber, A.; MaCurdy, T.; McClellan, M. Medical care at the end of life: Diseases, treatment patterns, and costs. NBER Working Paper No. 6748 Issued in October 1998. Available online: https://www.nber.org/papers/w6748 (accessed on 10 June 2020).
- Payne, G.; Laporte, A.; Deber, R.; Coyte, P. Counting backward to health care’s future: Using time-to-death modelling to identify changes in end-of-life morbidity and the impact of aging on health care expenditures. Milbank Q. 2007, 85, 213–257. [Google Scholar] [CrossRef]
- Henderson, J.; Goldacre, M.; Griffith, M. Hospital care for the elderly in the final year of life: A population-based study. BMJ 1990, 301, 17–19. [Google Scholar] [CrossRef] [PubMed]
- Busse, R.; Krauth, C.; Schwartz, F. Use of acute hospital beds does not increase as the population ages: Results from a seven-year cohort study in Germany. J. Epidemiol. Community Health 2002, 56, 289–293. [Google Scholar] [CrossRef] [PubMed]
- Dixon, T.; Shaw, M.; Frankel, S.; Ebrahim, S. Hospital admissions, age, and death: Retrospective cohort study. BMJ 2004, 328, 1288. [Google Scholar] [CrossRef] [PubMed]
- Brameld, K.; Spilsbury, K.; Rosenwax, L.; Leonard, H.; Semmens, J. Use of health services in the last year of life and cause of death in people with intellectual disability: A retrospective matched cohort study. BMJ Open 2018, 8, e0220268. [Google Scholar] [CrossRef]
- Hanlon, P.; Walsh, D.; Whyte, B.W.; Scott, S.N.; Lightbody, P.; Gilhooly, M.L. Hospital use by an ageing cohort: An investigation into the association between biological, behavioural and social risk markers and subsequent hospital utilization. J. Public Health Med. 1998, 20, 467–476. [Google Scholar] [CrossRef]
- Farmer, R.; Emami, J. Models for forecasting hospital bed requirements in the acute sector. J. Epidemiol. Community Med. 1990, 44, 307–312. [Google Scholar] [CrossRef]
- Tate, R.; MacWilliam, L.; Finlayson, G. A methodology for estimating hospital bed need in Manitoba in 2020. Can. J. Aging 2005, 24, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Seematter-Bagnoud, L.; Fustinoni, S.; Dung, D.; Santos-Eggimann, B.; Koehn, V.; Bize, R.; Oettli, A.; Wasserfallen, J.-B. Comparison of different methods to forecast hospital bed needs. Eur. Geriatr. Med. 2015, 6, 262–266. [Google Scholar] [CrossRef]
- Keegan, C.; Brick, A.; Walsh, B.; Bergin, A.; Eighan, J.; Wren, M.-A. How many beds? Capacity implications of hospital care demand projections in the Irish hospital system, 2015–2030. Int. J. Health Plann. Mgmt. 2019, 34, e569–e582. [Google Scholar] [CrossRef] [PubMed]
- Sweeney, T.; Ashley, J. Forecasting hospital bed needs. BMJ 1981, 283, 331–333. [Google Scholar] [CrossRef][Green Version]
- Beeknoo, N.; Jones, R. The demography myth—How demographic forecasting underestimates hospital admissions and creates the illusion that fewer hospital beds or community-based bed equivalents will be required in the future. J. Adv. Med. Med. Res. 2016, 19, 1–27. [Google Scholar] [CrossRef]
- Jones, R. Growth in NHS admissions and length of stay: A policy—based evidence fiasco. Br. J. Healthc. Mgmt. 2017, 23, 603–606. [Google Scholar] [CrossRef]
- Jones, R. Condition specific growth in occupied beds in England following a sudden and unexpected increase in deaths. Br. J. Healthc. Mgmt. 2019, 25, 1–8. [Google Scholar] [CrossRef]
- Jones, R. Have doctors and the public been misled regarding hospital bed requirements? Br. J. Healthc. Mgmt. 2019, 25, 242–250. [Google Scholar] [CrossRef]
- Jones, R. Hospital beds per death how does the UK compare globally. Br. J. Healthc. Mgmt. 2018, 24, 617–622. [Google Scholar] [CrossRef][Green Version]
- Jones, R. A pragmatic method to compare hospital bed provision between countries and regions: Beds in the states of Australia. Int. J. Health Plan. Mgmt. 2020, 35, 746–759. [Google Scholar] [CrossRef]
- World Bank. Hospital Beds (Per Thousand People). World Bank. 2020. Available online: https://data.worldbank.org/indicator/SH.MED.BEDS.ZS?name_desc=false (accessed on 4 June 2020).
- World Health Organisation. Acute Care Hospital Beds, Medical Group of Specialties, World Health Organisation. 2020. Available online: https://gateway.euro.who.int/en/indicators/hfa_480-5062-acute-care-hospital-beds-medical-group-of-specialties/ (accessed on 4 June 2020).
- Petterson, S.; Phillips, R.; Bazemore, A.; Koinis, B. Unequal distribution of the U.S. primary care workforce. Am. Fam. Physician. 2013, 87. [Google Scholar]
- Jones, R. Population density and healthcare costs. Br. J. Healthc. Mgmt. 2013, 19, 44–45. [Google Scholar] [CrossRef]
- Jones, R. Average length of stay in hospitals in the USA. Br. J. Healthc. Mgmt. 2013, 19, 186–191. [Google Scholar] [CrossRef]
- Kaiser Family Foundation. Hospital Beds per 1000 Population by Ownership Type, Kaiser Family Foundation. 2020. Available online: https://www.kff.org/other/state-indicator/beds-by-ownership/?currentTimeframe=0&selectedDistributions=total&selectedRows=%7B%22states%22:%7B%22all%22:%7B%7D%7D,%22wrapups%22:%7B%22united-states%22:%7B%7D%7D%7D&sortModel=%7B%22colId%22:%22Total%22,%22sort%22:%22asc%22%7D (accessed on 23 April 2020).
- The American Hospital Directory. Hospital Statistics by State. AHD. 2020. Available online: https://www.ahd.com/state_statistics.html (accessed on 10 June 2020).
- US Census Bureau. State Population, US Census Bureau. 2020. Available online: https://www.census.gov/data/tables/time-series/demo/popest/2010s-state-total.html (accessed on 23 April 2020).
- US Census Bureau. Median Household Income by US State, US Census Bureau. 2020. Available online: https://www.census.gov/search-results.html?q=average+income+state&page=1&stateGeo=none&searchtype=web&cssp=SERP&_charset_=utf-8 (accessed on 23 April 2020).
- United States Department of Agriculture. State Fact Sheets. 2020. Available online: https://data.ers.usda.gov/reports.aspx?ID=17854 (accessed on 9 July 2020).
- National Park Service. Summary of Acreage. NPS. 2019. Available online: https://www.nps.gov/subjects/lwcf/upload/NPS-Acreage-12-31-2019.pdf (accessed on 11 June 2020).
- Centers for Disease Control and Prevention, Wonder Database. Deaths in US states, Center for Disease Control. 2020. Available online: https://wonder.cD.C..gov/ucd-icd10.html (accessed on 23 April 2020).
- Decision Science News. Weighted Population Density, Decision Science News. 2017. Available online: http://www.decisionsciencenews.com/2017/06/26/weighted-population-density/ (accessed on 23 April 2020).
- Scarpino, S.; Petri, G. On the predictability of infectious disease outbreaks. Nat. Commun. 2019, 10, 898. [Google Scholar] [CrossRef] [PubMed]
- World Atlas. The Most Visited States in the U.S.; World Atlas. 2020. Available online: https://www.worldatlas.com/articles/the-most-visited-states-in-the-us.html (accessed on 23 April 2020).
- JBPub.com. Overview of the United States Healthcare System. Available online: http://samples.jbpub.com/9781284110067/Chapter4.pdf (accessed on 9 July 2020).
- ValuePenguin.com. Largest Health Insurance Companies of 2020. Available online: https://www.valuepenguin.com/largest-health-insurance-companies#:~:text=In%20the%20United%20States%2C%20there%20are%20currently%20more,who%20control%20more%20than%2038%25%20of%20the%20market (accessed on 9 July 2020).
- Weinhold, I.; Gurtner, S. Understanding shortages of sufficient health care in rural areas. Health Policy 2014, 118, 201–214. [Google Scholar] [CrossRef]
- Jones, R. Demand for hospital beds in English Primary Care Organisations. Br. J. Healthc. Mgmt. 2011, 17, 360–367. [Google Scholar] [CrossRef]
- Jones, R. Hospital bed occupancy demystified and why hospitals of different size and complexity must operate at different average occupancy. Br. J. Healthc. Mgmt. 2011, 17, 242–248. [Google Scholar] [CrossRef]
- Jones, R. A guide to maternity costs—Why smaller units have higher costs. Br. J. Midwifery 2013, 21, 54–59. [Google Scholar] [CrossRef]
- SARRAH.org. Demography and population. 2020. Available online: https://sarrah.org.au/content/demography-and-population (accessed on 10 July 2020).
- Sawe, B. US States with the Most Hospital Beds, World Atlas. 2017. Available online: https://www.worldatlas.com/articles/us-states-with-the-most-hospital-beds.html (accessed on 23 April 2020).
- Nelson, B. Too little or too much? Missing the Goldilocks zone of hospital capacity during covid-19. BMJ 2020, 369, m2332. [Google Scholar] [CrossRef]
- Human Rights Watch. US: Address Impact of Covid-19 on the Poor, Human Rights Watch. 2020. Available online: https://www.hrw.org/news/2020/03/19/us-address-impact-covid-19-poor (accessed on 23 April 2020).
- NHS England. Bed Availability and Occupancy Data—Overnight. 2020. Available online: https://www.england.nhs.uk/statistics/statistical-work-areas/bed-availability-and-occupancy/bed-data-overnight/ (accessed on 10 June 2020).
- NHS Digital. Hospital Admitted Patient Care Activity 2018-19, NHS Digital. 2019. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/hospital-admitted-patient-care-activity/2018-19 (accessed on 23 April 2020).
- Jones, R. How many medical beds does a country need? An international perspective. Br. J. Healthc. Mgmt. 2020, in press. [Google Scholar]
- Smith, S. Elective Surgeries Set to Resume, with Complications and Concerns. NBC News. 25 April 2020. Available online: https://www.nbcnews.com/news/us-news/elective-surgeries-set-resume-complications-concerns-n1190461 (accessed on 15 June 2020).
- Jones, R. Trends in critical care bed numbers in England. Br. J. Healthc. Mgmt. 2018, 24, 516–517. [Google Scholar] [CrossRef]
- Wunsch, H.; Angus, D.; Harrison, D.; Collange, O.; Fowler, R.; Hoste, E.A.J.; de Keizer, N.F.; Kersten, A.; Linde-Zwirble, W.T.; Sandiumenge, A.; et al. Variation in critical care services across North America and Western Europe. Crit. Care Med. 2008, 36, 2787-e8. [Google Scholar] [CrossRef] [PubMed]
- The Balance. Medical Bankruptcy and the Economy, The Balance. 2020. Available online: https://www.thebalance.com/medical-bankruptcy-statistics-4154729 (accessed on 23 April 2020).
- Roehr, B. The health of private insurance in the US during Covid-19. BMJ 2020, 370, m2606. [Google Scholar] [CrossRef] [PubMed]
- eHealth. Understanding a Health Insurance Copayment. ehealth. 2019. Available online: https://www.ehealthinsurance.com/resources/small-business/understanding-health-insurance-copayment (accessed on 23 April 2020).
- Trivedi, A.; Moloo, H.; Mor, V. Increased ambulatory care co-payments and hospitalizations among the elderly. NEJM 2010, 362, 320–328. [Google Scholar] [CrossRef] [PubMed]
- Bowden, E. Government Will Pay for Uninsured Americans’ Coronavirus Treatment: Trump, The New York Post. 2020. Available online: https://nypost.com/2020/04/03/us-government-will-cover-uninsured-americans-covid-19-treatment/ (accessed on 23 April 2020).
- Miller, I.; Becker, A.; Grenfell, B.; Metcalf, J. Mapping the Burden of COVID-19 in the United States, 2020. Available online: https://doi.org/10.1101/2020.04.05.20054700 (accessed on 23 April 2020).
- Bradford, C. Density Calculations for U.S. Urbanized Areas, Weighted by Census Tract, Austin Contrarian. 2008. Available online: https://austinzoning.typepad.com/austincontrarian/2008/03/weighted-densit.html (accessed on 23 April 2020).
- Ottensmann, J. On Population-Weighted Density. 2018. Available online: https://www.researchgate.net/publication/322992771 (accessed on 10 July 2020).
- Africa Centre for Strategic Studies. Mapping Risk Factors for the Spread of COVID-19 in Africa, Africa Centre for Strategic Studies. 2020. Available online: https://africacenter.org/spotlight/mapping-risk-factors-spread-covid-19-africa/ (accessed on 24 April 2020).
- Tal, A. The Disconcerting Association between Overpopulation and the Covid-19 Crisis, The Times of Israel. 2020. Available online: https://blogs.timesofisrael.com/the-disconcerting-association-between-overpopulation-and-the-covid-19-crisis/ (accessed on 23 April 2020).
- Jones, R. How Many Extra Deaths Have Really Occurred in the UK Due to the Covid-19 Outbreak? VII. Infectious Granularity, Research Gate. 2020. Available online: https://www.researchgate.net/publication/341776027_How_many_extra_deaths_have_really_occurred_in_the_UK_due_to_the_Covid-19_outbreak_VII_Infectious_granularity (accessed on 4 June 2020).
- Office for National Statistics. Deaths Involving COVID-19 by Local Area and Socioeconomic Deprivation: Deaths Occurring between 1 March and 31 May 2020. 12 June 2020. Available online: https://www.ons.gov.uk/peoplepopulationanD.C.ommunity/birthsdeathsandmarriages/deaths/bulletins/deathsinvolvingcovid19bylocalareasanddeprivation/deathsoccurringbetween1marchand31may2020 (accessed on 17 June 2020).
- EUROSTAT. Length of Stay in Hospital: How Countries Compare. 2019. Available online: https://ec.europa.eu/eurostat/de/web/products-eurostat-news/-/DDN-20190103-1 (accessed on 10 July 2020).
- OECD Data. Length of Hospital Stay. 2019. Available online: https://data.oecd.org/healthcare/length-of-hospital-stay.htm (accessed on 10 July 2020).
- Comas-Herrera, A.; Zalakaín, J.; Litwin, C.; Hsu, A.T.; Lane, N.; Fernández, J.-L. Mortality Associated with COVID19 Outbreaks in Care Homes: Early International Evidence. Article in LTCcovid.org, International Long-Term Care Policy Network, CPEC-LSE. 3 May 2020. Available online: https://ltccovid.org/wp-content/uploads/2020/05/Mortality-associated-with-COVID-3-May-final-1.pdf (accessed on 15 June 2020).
- Worldometer. Age, Sex, Existing Conditions of COVID-19 Cases and Deaths. Available online: https://www.worldometers.info/coronavirus/coronavirus-age-sex-demographics/ (accessed on 15 June 2020).
- Petrilli, C.; Jones, S.; Yang, J.; Rajagopalan, H.; O′Donnell, L.; Chernyak, Y.; Tobin, K.A.; Cerfolio, R.J.; Francois, F.; Horwitz, L.I. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: Prospective cohort study. BMJ 2020, 369, m1966. [Google Scholar] [CrossRef]
- Hicks, N. Health officials ordered coronavirus patients to nursing homes despite empty beds. New York Post. 11 June 2020. Available online: https://nypost.com/2020/06/11/officials-knew-of-empty-beds-as-it-ordered-covid-19-patients-to-nursing-homes/ (accessed on 15 July 2020).
- Weinberger, D.; Chen, J.; Cohen, T.; Crawford, F.W.; Mostashari, F.; Olson, D.; Pitzer, V.E.; Reich, N.G.; Russi, M.; Simonsen, L.; et al. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to May 2020. JAMA Int. Med. 2020. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. CovidView. 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/index.html (accessed on 16 July 2020).


| State | Population | Deaths | Adjusted Beds per 1000 Deaths | Nearest Equivalent |
|---|---|---|---|---|
| Oregon | 4,181,886 | 36,166 | 191.6 | Burundi |
| Washington | 7,523,869 | 56,908 | 212.6 | Costa Rica |
| Idaho | 1,750,536 | 14,243 | 227.4 | Botswana |
| New Hampshire | 1,353,465 | 12,816 | 229.9 | Botswana |
| Vermont | 624,358 | 5904 | 230.1 | Botswana |
| New Mexico | 2,092,741 | 19,075 | 236.5 | Mexico |
| Maryland | 6,035,802 | 50,308 | 239.9 | Mexico |
| Wisconsin | 5,807,406 | 53,696 | 240.3 | Guyana |
| Hawaii | 1,420,593 | 11,401 | 249.3 | Dominican Republic |
| Arizona | 7,158,024 | 59,577 | 251.4 | Ecuador |
| Maine | 1,339,057 | 14,680 | 252.2 | Algeria |
| Colorado | 5,691,287 | 38,517 | 254.5 | Algeria |
| Nevada | 3,027,341 | 24,760 | 256.4 | Thailand |
| Delaware | 965,479 | 9421 | 262.5 | Comoros |
| Utah | 3,153,550 | 18,436 | 264.7 | Peru |
| South Carolina | 5,084,156 | 50,572 | 277.8 | Fiji |
| Virginia | 8,501,286 | 69,360 | 282.7 | South Africa |
| Rhode Island | 1,058,287 | 10,189 | 284.1 | Albania |
| California | 39,461,588 | 269,094 | 286.5 | Albania |
| North Carolina | 10,381,615 | 93,844 | 286.7 | Albania |
| Ohio | 11,676,341 | 124,545 | 286.7 | Albania |
| Michigan | 9,984,072 | 98,822 | 288.2 | Iran |
| Massachusetts | 6,882,635 | 59,054 | 290.8 | Iran |
| Georgia | 10,511,131 | 85,149 | 292.1 | Andorra |
| Indiana | 6,695,497 | 65,646 | 292.5 | Trinidad and Tobago |
| New Jersey | 8,886,025 | 76,002 | 300.2 | Vanuatu |
| Illinois | 12,723,071 | 109,904 | 300.7 | Vanuatu |
| Texas | 28,628,666 | 202,025 | 302.2 | Vanuatu |
| Minnesota | 5,606,249 | 44,737 | 302.7 | Vanuatu |
| U.S. average | 324,883,210 | 2,816,380 | 300.6 | Vanuatu |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jones, R.P. Would the United States Have Had Too Few Beds for Universal Emergency Care in the Event of a More Widespread Covid-19 Epidemic? Int. J. Environ. Res. Public Health 2020, 17, 5210. https://doi.org/10.3390/ijerph17145210
Jones RP. Would the United States Have Had Too Few Beds for Universal Emergency Care in the Event of a More Widespread Covid-19 Epidemic? International Journal of Environmental Research and Public Health. 2020; 17(14):5210. https://doi.org/10.3390/ijerph17145210
Chicago/Turabian StyleJones, Rodney P. 2020. "Would the United States Have Had Too Few Beds for Universal Emergency Care in the Event of a More Widespread Covid-19 Epidemic?" International Journal of Environmental Research and Public Health 17, no. 14: 5210. https://doi.org/10.3390/ijerph17145210
APA StyleJones, R. P. (2020). Would the United States Have Had Too Few Beds for Universal Emergency Care in the Event of a More Widespread Covid-19 Epidemic? International Journal of Environmental Research and Public Health, 17(14), 5210. https://doi.org/10.3390/ijerph17145210





