Consequences of Circadian Disruption in Shift Workers on Chrononutrition and their Psychosocial Well-Being
Abstract
1. Introduction
2. Materials and Methods
3. Results and Discussion
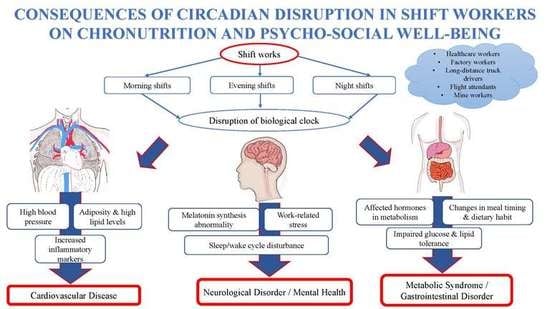
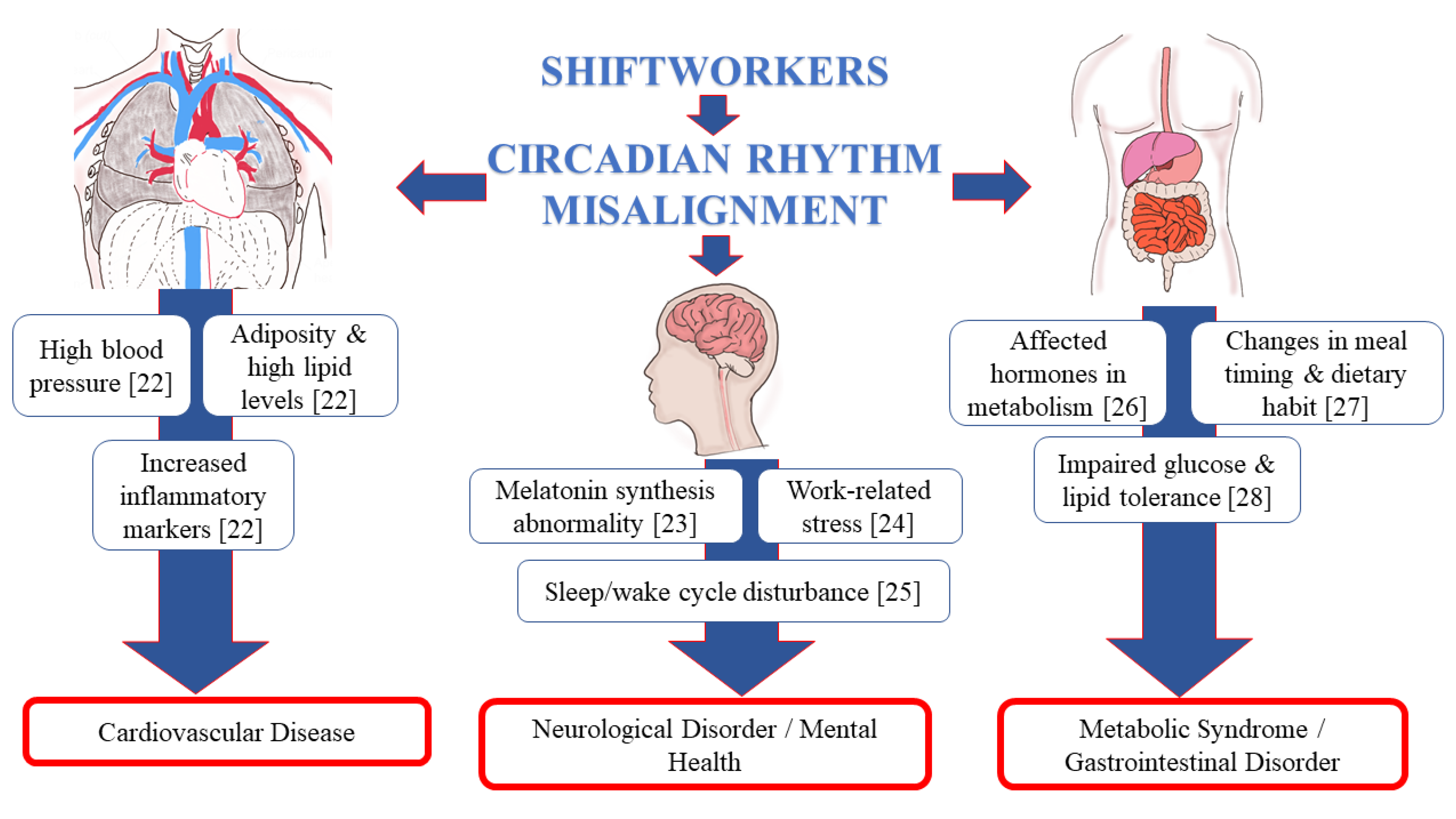
3.1. Nature of Shift Work
3.2. Sleep/Wake Cycle (24-h Circadian)
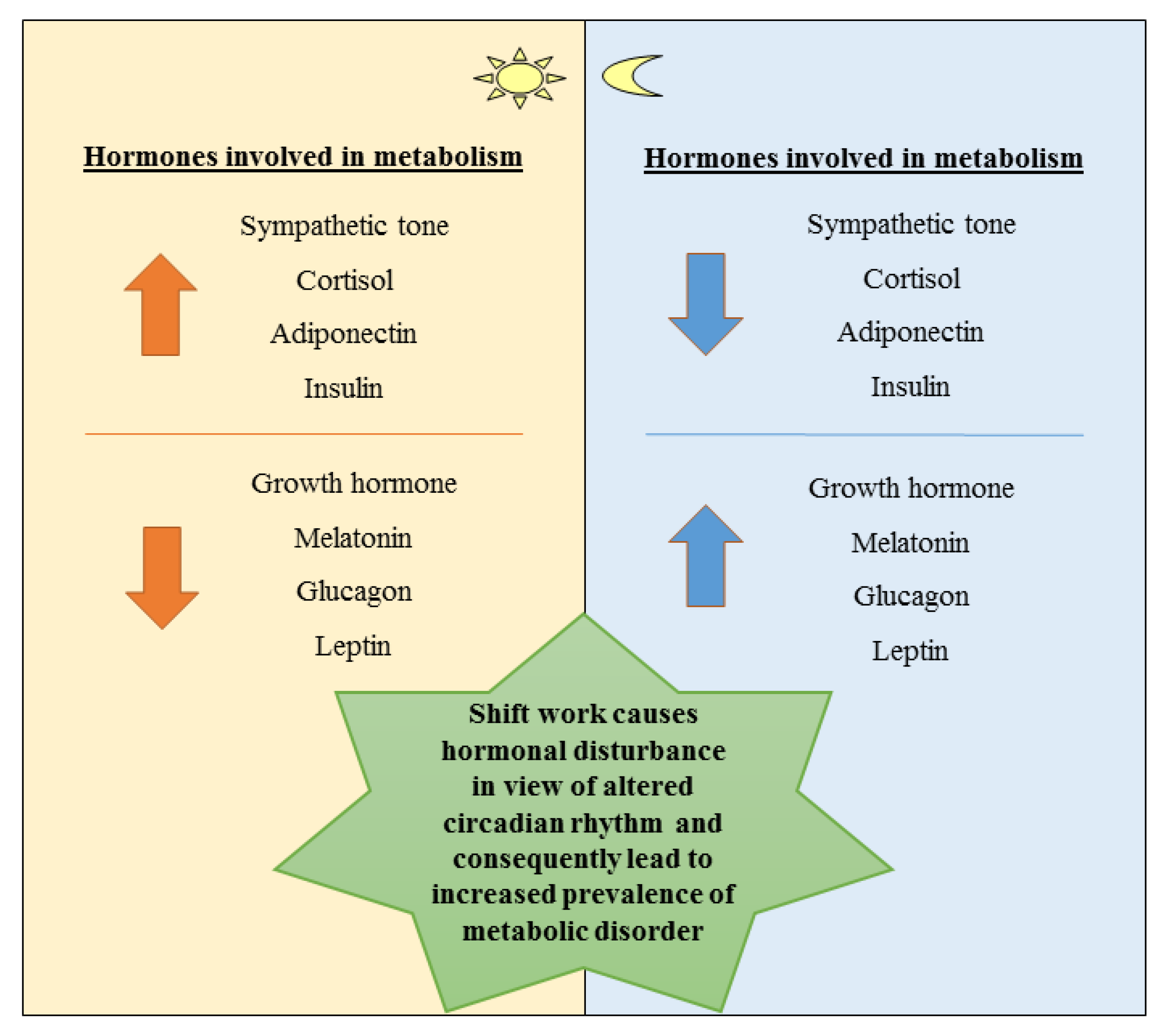
3.3. Chrononutrition
3.4. Daytime Meal
3.5. Late-Night Meal
3.6. Dietary Habit and Meal Changes due to Shift Works
3.7. Altered Sleep/Wake Cycle and Nutritional Intake
3.8. Psychosocial Well-Being and Nature of Work
3.9. Relationship of Nutritional Intake and Psychosocial Well-Being among Shift Workers
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Åkerstedt, T. Psychological and psychophysiological effects of shift work. Scand. J. Work. Environ. Health 1990, 16, 67–73. [Google Scholar] [CrossRef]
- De C Moreno, C.R.; Fischer, F.M.; Rotenberg, L. Worker’s health in society 24 h. São Paulo Em Perspect 2003, 17, 34–46. [Google Scholar]
- Ruddick-Collins, L.C.; Johnston, J.D.; Morgan, P.J.; Johnstone, A.M. The Big Breakfast Study: Chrono-nutrition influence on energy expenditure and bodyweight. Nutr. Bull. 2018, 43, 174–183. [Google Scholar] [PubMed]
- Kawabe, Y.; Nakamura, Y.; Kikuchi, S.; Murakami, Y.; Tanaka, T.; Takebayashi, T.; Okayama, A.; Miura, K.; Okamura, T.; Ueshima, H.; et al. Relationship Between Shift Work and Clustering of the Metabolic Syndrome Diagnostic Components. J. Atheroscler. Thromb. 2014, 21, 703–711. [Google Scholar] [CrossRef] [PubMed]
- Lowden, A.; Moreno, C.; Holmback, U.; Lennernas, M.; Tucker, P. Eating and shift work—Effects on habits, metabolism, and performance. Scand. J. Work Environ. Health 2010, 36, 150–162. [Google Scholar] [CrossRef] [PubMed]
- Waterhouse, J.; Buckley, P.; Edwards, B.; Reilly, T. Measurement of, and some reasons for, differences in eating habits between night and day workers. Chronobio. Int. 2003, 20, 1075–1092. [Google Scholar]
- Waterhouse, J.; Minors, D.; Atkinson, G.; Benton, D. Chronobiology and meal times: Internal and external factors. Br. J. Nutr. 1997, 77, S29–S38. [Google Scholar]
- Antunes, L.; Levandovski, R.; Dantas, G.; Caumo, W.; Hidalgo, M.P. Obesity and shift work: Chronobiological aspects. Nutr. Res. Rev. 2010, 23, 155–168. [Google Scholar]
- Gibson, E.L.; Green, M.W. Nutritional influences on cognitive function: Mechanisms of susceptibility. Nutr. Res. Rev. 2002, 15, 169–206. [Google Scholar]
- Dye, L.; Lluch, A.; Blundell, J.E. Macronutrients and mental performance. Nutrition 2000, 16, 1021–1034. [Google Scholar] [CrossRef]
- Kanarek, R. Psychological effects of snacks and altered meal frequency. Br. J. Nutr. 1997, 77, S105–S120. [Google Scholar] [PubMed]
- The Japan Institute for Labour Policy and Training. 2012. Tokyo: c2003-2013. Available online: http://www.jil.go.jp/kokunai/statistics/databook/2012/06/p195-202_t6-6.pdf (accessed on 13 November 2019).
- Nielsen, N.R.; Stahlberg, C.; Strandberg-Larsen, K.; Kristensen, T.S.; Zhang, Z.-F.; Hundrup, Y.A.; Grønbæk, M. Are work-related stressors associated with diagnosis of more advanced stages of incident breast cancers? Cancer Causes Control 2007, 19, 297–303. [Google Scholar] [PubMed]
- ASEAN Briefing. Labour Contracts in ASEAN. 2019. Available online: https://www.aseanbriefing.com/news/2019/03/21/labor-contracts-asean.html (accessed on 26 November 2019).
- Wang, X.-S.; Armstrong, M.E.G.; Cairns, B.; Key, T.J.; Travis, R.C. Shift work and chronic disease: The epidemiological evidence. Occup. Med. 2011, 61, 78–89. [Google Scholar]
- Faraut, B.; Bayon, V.; Leger, D. Neuroendocrine, immune and oxidative stress in shift workers. Sleep Med. Rev. 2013, 17, 433–444. [Google Scholar] [PubMed]
- International Labour Organization. C171–Night Work Convention. Genebra, 1990; Available online: http://www.ilo.org/dyn/normlex/en/f?p=NORMLEXPUB:12100:0::NO::P12100_ILO_CODE:C171 (accessed on 26 November 2019).
- Harrington, J.M. Health effects of shift work and extended hours of work. Occup. Environ. Med. 2001, 58, 68–72. [Google Scholar] [CrossRef]
- World Health Organization. Basic Documents, 39th ed.; WHO: Geneva, Switzerland, 1992. [Google Scholar]
- Atkinson, G.; Fullick, S.; Grindey, C.; MacLaren, D.; Waterhouse, J. Exercise, Energy Balance and the Shift Worker. Sports Med. 2008, 38, 671–685. [Google Scholar]
- Burch, J.B.; Yost, M.G.; Johnson, W.; Allen, E. Melatonin, Sleep, and Shift Work Adaptation. J. Occup. Environ. Med. 2005, 47, 893–901. [Google Scholar]
- Thomas, C.; Power, C.; Slimings, C. Shift work and risk factors for cardiovascular disease: A study at age 45 years in the 1958 British birth cohort. Eur. J. Epidemiol. 2010, 25, 305–314. [Google Scholar]
- Wright, K.P., Jr.; McHill, A.W.; Birks, B.R.; Griffin, B.R.; Rusterholz, T.; Chinoy, E.D. Entrainment of the human circadian clock to the natural light-dark cycle. Curr. Boil. 2013, 23, 1554–1558. [Google Scholar]
- Ferri, P.; Guadi, M.; Marcheselli, L.; Balduzzi, S.; Magnani, D.; Di Lorenzo, R. The impact of shift work on the psychological and physical health of nurses in a general hospital: A comparison between rotating night shifts and day shifts. Risk Manag. Health Policy 2016, 9, 203–211. [Google Scholar]
- Van Cauter, E.; Aschoff, J. Endocrine and other biological rhythms. In DeGroot L. Endocrinology, 2nd ed.; Saunders: Philadelphia, PA, USA, 1989; pp. 2658–2705. [Google Scholar]
- Froy, O. Metabolism and Circadian Rhythms—Implications for Obesity. Endocr. Rev. 2009, 31, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Gifkins, J.; Johnston, A.N.; Loudoun, R. The impact of shift work on eating patterns and self-care strategies utilised by experienced and inexperienced nurses. Chronobiol Int. 2018, 35, 811–820. [Google Scholar] [CrossRef]
- Al-Naimi, S.; Hampton, S.M.; Richard, P.; Tzung, C.; Morgan, L.M. Postprandial metabolic profiles following meals and snacks eaten during simulated night and day shift work. Chronobiol Int. 2004, 21, 937–947. [Google Scholar] [CrossRef] [PubMed]
- Czeisler, C.A.; Johnson, M.P.; Duffy, J.F.; Brown, E.N.; Ronda, J.M.; Kronauer, R.E. Exposure to Bright Light and Darkness to Treat Physiologic Maladaptation to Night Work. New Engl. J. Med. 1990, 322, 1253–1259. [Google Scholar] [CrossRef] [PubMed]
- McHill, A.W.; Wright, K.P., Jr. Role of sleep and circadian disruption on energy expenditure and in metabolic predisposition to human obesity and metabolic disease. Obes. Rev. 2017, 18, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Mohawk, J.A.; Green, C.B.; Takahashi, J.S. Central and peripheral circadian clocks in mammals. Annu. Rev. Neurosci. 2012, 35, 445–462. [Google Scholar] [CrossRef]
- Teclemariam-Mesbah, R.; Ter Horst, G.J.; Postema, F.; Wortel, J.; Buijs, R.M. Anatomical demonstration of the suprachiasmatic nucleus-pineal pathway. J. Comp. Neurol. 1999, 406, 171–182. [Google Scholar] [CrossRef]
- Ohdo, S. Chronotherapeutic strategy: Rhythm monitoring, manipulation and disruption. Adv. Drug Deliv. Rev. 2010, 62, 859–875. [Google Scholar] [CrossRef]
- Stokkan, K.-A. Entrainment of the Circadian Clock in the Liver by Feeding. Science 2001, 291, 490–493. [Google Scholar] [CrossRef]
- Arble, D.; Bass, J.; Laposky, A.D.; Vitaterna, M.H.; Turek, F.W. Circadian Timing of Food Intake Contributes to Weight Gain. Obes. 2009, 17, 2100–2102. [Google Scholar] [CrossRef]
- Houghton, M. The American Heritage Medical Dictionary; Houghton Mifflin Company: Boston, MA, USA, 2004. [Google Scholar]
- National Sleep Foundation. What Happens When You Sleep? 2011; Available online: http://www.sleepfoundation.org/article/how-sleep-works/what-happens-when-you-sleep (accessed on 17 November 2019).
- Learthart, S. Health effects of internal rotation of shifts. Nurs. Stand. 2000, 14, 34–36. [Google Scholar] [CrossRef] [PubMed]
- Heath, G.; Roach, G.D.; Dorrian, J.; Ferguson, S.A.; Darwent, D.; Sargent, C. The effect of sleep restriction on snacking behaviour during a week of simulated shiftwork. Accid. Anal. Prev. 2012, 45, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Åkerstedt, T. Shift work and disturbed sleep/wakefulness. Occup. Med. 2003, 53, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Shao, M.-F.; Chou, Y.-C.; Yeh, M.-Y.; Tzeng, W.-C. Sleep quality and quality of life in female shift-working nurses. J. Adv. Nurs. 2010, 66, 1565–1572. [Google Scholar] [CrossRef]
- Spiegel, K.; Tasali, E.; Penev, P.; Van Cauter, E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann. Intern. Med. 2004, 141, 846–850. [Google Scholar] [CrossRef]
- Gangwisch, J.; Malaspina, L.; Boden-Albala, B.; Heymsfield, S.B. Inadequate sleep as a risk factor for obesity: Analyses of the NHANES I. Sleep 2005, 28, 1289–1296. [Google Scholar] [CrossRef]
- Gupta, C.C.; Coates, A.; Dorrian, J.; Banks, S. The factors influencing the eating behaviour of shiftworkers: What, when, where and why. Ind. Health 2018, 57, 419–453. [Google Scholar] [CrossRef]
- Persson, M.; Martensson, J. Situations influencing habits in diet and exercise among nurses working night shift. J. Nurs. Manag. 2006, 14, 414–423. [Google Scholar] [CrossRef]
- Czeisler, C.A.; Buxton, O.M.; Khalsa, S.B. The human circadian timing system and sleep-wake regulation. In Principles and Practice of Sleep Medicine; Kryger, M., Roth, T., Dement, W.C., Eds.; Elsevier: Philadelphia, PA, USA, 2005. [Google Scholar]
- Duffy, J.F.; Wright, K.P. Entrainment of the Human Circadian System by Light. J. Boil. Rhythm. 2005, 20, 326–338. [Google Scholar] [CrossRef]
- Boivin, D.B.; Tremblay, G.M.; James, F.O. Working on atypical schedules. Sleep Med. 2007, 8, 578–589. [Google Scholar] [CrossRef]
- Axelsson, J.; Akerstedt, T.; Kecklund, G.; Lowden, A. Tolerance to shift work–how does it relate to sleep and wakefulness? Int. Arch. Occup. Environ. Health 2004, 77, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Folkard, S. Do Permanent Night Workers Show Circadian Adjustment? A Review Based on the Endogenous Melatonin Rhythm. Chonobiol. Int. 2008, 25, 215–224. [Google Scholar] [CrossRef] [PubMed]
- Morris, C.J.; Yang, J.N.; Garcia, J.I.; Myers, S.; Bozzi, I.; Wang, W.; Buxton, O.M.; Shea, S.A.; Scheer, F.A.J.L. Endogenous circadian system and circadian misalignment impact glucose tolerance via separate mechanisms in humans. Proc. Natl. Acad. Sci. USA 2015, 112, E2225–E2234. [Google Scholar] [CrossRef] [PubMed]
- Morris, C.J.; Purvis, T.E.; Mistretta, J.; Scheer, F.A. Effects of the Internal Circadian System and Circadian Misalignment on Glucose Tolerance in Chronic Shift Workers. J. Clin. Endocrinol. Metab. 2016, 101, 1066–1074. [Google Scholar] [CrossRef] [PubMed]
- Baron, K.G.; Reid, K.; Kern-Goldberger, A.; Zee, P.C. Role of Sleep Timing in Caloric Intake and BMI. Obesity 2011, 19, 1374–1381. [Google Scholar] [CrossRef]
- Bandín, C.; Scheer, F.A.J.L.; Luque, A.J.; Àvila-Gandía, V.; Zamora, S.; Madrid, J.A.; Gómez-Abellán, P.; Garaulet, M. Meal timing affects glucose tolerance, substrate oxidation and circadian-related variables: A randomized, crossover trial. Int. J. Obes. 2014, 39, 828–833. [Google Scholar] [CrossRef]
- Nikpour, M.; Tirgar, A.; Hajiahmadi, M.; Hosseini, A.; Heidari, B.; Ghaffari, F.; Ebadi, A.; Nasiri, F.; Firouzbakht, M. Shift work and metabolic syndrome: A multi-center cross-sectional study on females of reproductive age. Biomed. Rep. 2019, 10, 311–317. [Google Scholar]
- Koh, S.J.; Kim, M.; Oh, D.Y.; Kim, B.G.; Lee, K.L.; Kim, J.W. Psychosocial Stress in Nurses With Shift Work Schedule Is Associated With Functional Gastrointestinal Disorders. J. Neurogastroenterol. Motil 2014, 20, 516–522. [Google Scholar] [CrossRef]
- Knutsson, A.; Alfredsson, L.; Karlsson, B.; Åkerstedt, T.; Fransson, E.; Westerholm, P.; Westerlund, H. Breast cancer among shift workers: Results of the WOLF longitudinal cohort study. Scand. J. Work. Environ. Health 2012, 39, 170–177. [Google Scholar] [CrossRef]
- Pot, G.K.; Hardy, R.; Stephen, A.M. Irregular consumption of energy intake in meals is associated with a higher cardiometabolic risk in adults of a British birth cohort. Int. J. Obes. 2014, 38, 1518–1524. [Google Scholar] [CrossRef]
- Pot, G.K. Sleep and dietary habits in the urban environment: The role of chrono-nutrition. Proc. Nutr. Soc. 2017, 77, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Hur, S.J.; Lim, B.O.; Decker, E.A.; McClements, D.J. In vitro human digestion models for food applications. Food Chem. 2011, 125, 1–12. [Google Scholar] [CrossRef]
- Hellström, P.M.; Grybäck, P.; Jacobsson, H. The physiology of gastric emptying. Best Pr. Res. Clin. Anaesthesiol. 2006, 20, 397–407. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Sun, L.; Zhuge, F.; Guo, X.; Zhao, Z.; Tang, R.; Chen, Q.; Chen, L.; Kato, H.; Fu, Z. Differential Roles of Breakfast and Supper in Rats of a Daily Three-Meal Schedule Upon Circadian Regulation and Physiology. Chronobiol. Int. 2011, 28, 890–903. [Google Scholar] [CrossRef]
- Loboda, A.; Kraft, W.K.; Fine, B.; Joseph, J.; Nebozhyn, M.; Zhang, C. Diurnal variation of the human adipose transcriptome and the link to metabolic disease. BMC Med. Genom. 2009, 2, 7. [Google Scholar] [CrossRef]
- Ma, Y.; Bertone, E.R.; Stanek, E.J., 3rd; Reed, G.W.; Hébert, J.R.; Cohen, N.L.; Merriam, P.A.; Ockene, I.S. Association between eating patterns and obesity in a free-living US adult population. Am. J. Epidemiol. 2003, 158, 85–92. [Google Scholar] [CrossRef]
- Sudo, R.O.N. Nutrient intake among female shift workers in a computer factory in Japan. Int. J. Food Sci. Nutr. 2001, 52, 367–378. [Google Scholar]
- De Freitas, E.S.; Canuto, R.; Henn, R.L.; Olinto, B.A.; Macagnan, J.B.A.; Pattussi, M.P.; Busnello, F.M.; Olinto, M.T. Alteration in eating habits among shift workers of a poultry processing plant in Southern Brazil. Ciencia Saude Coletiva 2015, 20, 2401–2410. [Google Scholar]
- Pollitt, E. Does Breakfast Make a Difference in School? J. Am. Diet. Assoc. 1995, 95, 1134–1139. [Google Scholar] [CrossRef]
- Fonken, L.; Workman, J.L.; Walton, J.C.; Weil, Z.; Morris, J.S.; Haim, A.; Nelson, R.J. Light at night increases body mass by shifting the time of food intake. Proc. Natl. Acad. Sci. USA 2010, 107, 18664–18669. [Google Scholar] [CrossRef]
- Adolphus, K.; Lawton, C.; Champ, C.L.; Dye, L. The Effects of Breakfast and Breakfast Composition on Cognition in Children and Adolescents: A Systematic Review. Adv. Nutr. 2016, 7, 590S–612S. [Google Scholar] [CrossRef] [PubMed]
- Matthys, C.; De Henauw, S.; Bellemans, M.; De Maeyer, M.; De Backer, G. Breakfast habits affect overall nutrient profiles in adolescents. Public Health Nutr. 2007, 10, 413–421. [Google Scholar] [CrossRef] [PubMed]
- Leidy, H.J. The Benefits of Breakfast Consumption to Combat Obesity and Diabetes in Young People. Am. J. Lifestyle Med. 2012, 7, 99–103. [Google Scholar] [CrossRef]
- Farshchi, H.R.; Taylor, M.A.; Macdonald, I. Deleterious effects of omitting breakfast on insulin sensitivity and fasting lipid profiles in healthy lean women. Am. J. Clin. Nutr. 2005, 81, 388–396. [Google Scholar] [CrossRef] [PubMed]
- Stote, K.S.; Baer, D.J.; Spears, K.; Paul, D.R.; Harris, G.K.; Rumpler, W.V.; Strycula, P.; Najjar, S.S.; Ferrucci, L.; Ingram, N.K.; et al. A controlled trial of reduced meal frequency without caloric restriction in healthy, normal-weight, middle-aged adults123. Am. J. Clin. Nutr. 2007, 85, 981–988. [Google Scholar] [CrossRef]
- Cahill, L.E.; Chiuve, S.E.; Mekary, R.A.; Jensen, M.K.; Flint, A.J.; Hu, F.B.; Rimm, E.B. Prospective study of breakfast eating and incident coronary heart disease in a cohort of male US health professionals. Circulation 2013, 128, 337–343. [Google Scholar] [CrossRef]
- Song, W.; Chun, O.K.; Obayashi, S.; Cho, S.; Chung, C.E. Is Consumption of Breakfast Associated with Body Mass Index in US Adults? J. Am. Diet. Assoc. 2005, 105, 1373–1382. [Google Scholar] [CrossRef]
- Barr, S.I.; DiFrancesco, L.; Fulgoni, V.L. Consumption of Breakfast and the Type of Breakfast Consumed Are Positively Associated with Nutrient Intakes and Adequacy of Canadian Adults. J. Nutr. 2013, 143, 86–92. [Google Scholar] [CrossRef]
- Nicklas, T.A.; Myers, L.; Reger, C.; Beech, B.; Berenson, G.S. Impact of Breakfast Consumption on Nutritional Adequacy of the Diets of Young Adults in Bogalusa, Louisiana. J. Am. Diet. Assoc. 1998, 98, 1432–1438. [Google Scholar] [CrossRef]
- Leidy, H.J.; Bossingham, M.J.; Mattes, R.; Campbell, W. Increased dietary protein consumed at breakfast leads to an initial and sustained feeling of fullness during energy restriction compared to other meal times. Br. J. Nutr. 2009, 101, 798–803. [Google Scholar] [CrossRef]
- Leidy, H.J.; Racki, E.M. The addition of a protein-rich breakfast and its effects on acute appetite control and food intake in ’breakfast-skipping’ adolescents. Int. J. Obes. 2010, 34, 1125–1133. [Google Scholar] [CrossRef] [PubMed]
- Jakubowicz, D.; Froy, O.; Wainstein, J.; Boaz, M. Meal timing and composition influence ghrelin levels, appetite scores and weight loss maintenance in overweight and obese adults. Steroids 2012, 77, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Almoosawi, S.; Prynne, C.J.; Hardy, R.; Stephen, A.M. Time-of-day and nutrient composition of eating occasions: Prospective association with the metabolic syndrome in the 1946 British birth cohort. Int. J. Obes. 2012, 37, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Haus, E.; Reinberg, A.; Mauvieux, B.; Le Floc’H, N.; Sackett-Lundeen, L.; Touitou, Y. Risk of obesity in male shift workers: A chronophysiological approach. Chronobiol. Int. 2016, 33, 1018–1036. [Google Scholar] [CrossRef]
- St-Onge, M.-P.; Ard, J.; Baskin, M.L.; Chiuve, S.E.; Johnson, H.M.; Kris-Etherton, P.; Varady, K. Meal Timing and Frequency: Implications for Cardiovascular Disease Prevention: A Scientific Statement From the American Heart Association. Circulation 2017, 135, e96–e121. [Google Scholar] [CrossRef]
- Berg, C.; Lappas, G.; Wolk, A.; Strandhagen, E.; Torén, K.; Rosengren, A.; Thelle, D.; Lissner, L. Eating patterns and portion size associated with obesity in a Swedish population. Appetite 2009, 52, 21–26. [Google Scholar] [CrossRef]
- Cleator, J.; Abbott, J.; Judd, P.; Sutton, C.; Wilding, J.P. Night eating syndrome: Implications for severe obesity. Nutr. Diabetes 2012, 2, e44. [Google Scholar] [CrossRef]
- Striegel-Moore, R.H.; Rosselli, F.; Wilson, G.T.; Perrin, N.; Harvey, K.; DeBar, L. Nocturnal eating: Association with binge eating, obesity, and psychological distress. Int. J. Eat. Disord. 2010, 43, 520–526. [Google Scholar] [CrossRef]
- Paz, A.; Berry, E.M. Effect of meal composition on alertness and performance of hospital night-shift workers. Ann. Nutr. Metab. 1997, 41, 291–298. [Google Scholar] [CrossRef]
- Johnston, C.S.; Day, C.S.; Swan, P.D. Postprandial Thermogenesis Is Increased 100% on a High-Protein, Low-Fat Dietversusa High-Carbohydrate, Low-Fat Diet in Healthy, Young Women. J. Am. Coll. Nutr. 2002, 21, 55–61. [Google Scholar] [CrossRef]
- Nehme, P.; Marqueze, E.C.; Ulhôa, M.; Moulatlet, E.; Codarin, M.A.; Moreno, C.R.C. Effects of a carbohydrate-enriched night meal on sleepiness and sleep duration in night workers: A double-blind intervention. Chronobiol. Int. 2014, 31, 453–460. [Google Scholar] [CrossRef]
- Bonham, M.; Bonnell, E.K.; Huggins, C.E. Energy intake of shift workers compared to fixed day workers: A systematic review and meta-analysis. Chronobiol. Int. 2016, 33, 1086–1100. [Google Scholar] [CrossRef] [PubMed]
- Moran-Ramos, S.; Baez-Ruiz, A.; Buijs, R.M.; Escobar, C. When to eat? The influence of circadian rhythms on metabolic health: Are animal studies providing the evidence? Nutr. Res. Rev. 2016, 29, 180–193. [Google Scholar] [CrossRef] [PubMed]
- Strzemecka, J.; Bojar, I.; Strzemecka, E.; Owoc, A. Dietary habits among persons hired on shift work. Ann. Agric. Environ. Med. 2014, 21, 128–131. [Google Scholar] [PubMed]
- Nyberg, M.; Wiklund, M. Impossible meals? The food and meal situation of flight attendants in Scandinavia–A qualitative interview study. Appetite 2017, 113, 162–171. [Google Scholar] [CrossRef]
- Jack, F.R.; Piacentini, M.; Schröder, M.J. Perception and Role of Fruit in the Workday Diets of Scottish Lorry Drivers. Appetite 1998, 30, 139–149. [Google Scholar] [CrossRef]
- Wong, H.; Wong, M.C.; Wong, S.Y.; Lee, A. The association between shift duty and abnormal eating behaviour among nurses working in a major hospital: A cross-sectional study. Int. J. Nurs. Stud. 2010, 47, 1021–1027. [Google Scholar] [CrossRef]
- De Assis, M.A.; Kupek, E.; Nahas, M.V.; Bellisle, F. Food intake and circadian rhythms in shift workers with a high workload. Appetite 2003, 40, 175–183. [Google Scholar] [CrossRef]
- Esquirol, Y.; Perret, B.; Ruidavets, J.-B.; Marquie, J.-C.; Dienne, E.; Niezborala, M.; Ferrières, J. Shift work and cardiovascular risk factors: New knowledge from the past decade. Arch. Cardiovasc. Dis. 2011, 104, 636–668. [Google Scholar] [CrossRef]
- Hemiö, K.; Puttonen, S.; Viitasalo, K.; Härmä, M.; Peltonen, M.; Lindstrom, J. Food and nutrient intake among workers with different shift systems. Occup. Environ. Med. 2015, 72, 513–520. [Google Scholar] [CrossRef]
- Tada, Y.; Kawano, Y.; Maeda, I.; Yoshizaki, T.; Sunami, A.; Yokoyama, Y.; Matsumoto, H.; Hida, A.; Komatsu, T.; Togo, F. Association of body mass index with lifestyle and rotating shift work in Japanese female nurses. Obesity 2014, 22, 2489–2493. [Google Scholar] [CrossRef]
- Balieiro, L.C.T.; Rossato, L.; Waterhouse, J.; Paim, S.L.; Mota, M.C.; Crispim, C.A. Nutritional status and eating habits of bus drivers during the day and night. Chronobiol. Int. 2014, 31, 1123–1129. [Google Scholar] [CrossRef]
- Turek, F.W.; Joshu, C.; Kohsaka, A.; Lin, E.; Ivanova, G.; McDearmon, E.; Laposky, A.; Losee-Olson, S.; Easton, A.; Jensen, D.R.; et al. Obesity and Metabolic Syndrome in Circadian Clock Mutant Mice. Science 2005, 308, 1043–1045. [Google Scholar] [CrossRef]
- Barnea, M.; Madar, Z.; Froy, O. High-Fat Diet Delays and Fasting Advances the Circadian Expression of Adiponectin Signaling Components in Mouse Liver. Endocrinology 2009, 150, 161–168. [Google Scholar] [CrossRef]
- Kohsaka, A.; Bass, J. A sense of time: How molecular clocks organize metabolism. Trends Endocrinol. Metab. 2007, 18, 4–11. [Google Scholar] [CrossRef]
- Panda, S.; Antoch, M.P.; Miller, B.H.; Su, A.I.; Schook, A.B.; Straume, M.; Schultz, P.G.; Kay, S.A.; Takahashi, J.S.; HogenEsch, J.B. Coordinated transcription of key pathways in the mouse by the circadian clock. Cell 2002, 109, 307–320. [Google Scholar] [CrossRef]
- Green, C.B.; Takahashi, J.S.; Bass, J. The Meter of Metabolism. Cell 2008, 134, 728–742. [Google Scholar] [CrossRef]
- Strickland, J.R.; Eyler, A.A.; Purnell, J.Q.; Kinghorn, A.M.; Herrick, C.; Evanoff, B.A. Enhancing Workplace Wellness Efforts to Reduce Obesity: A Qualitative Study of Low-Wage Workers in St Louis, Missouri, 2013–2014. Prev. Chronic Dis. 2015, 12, E67. [Google Scholar] [CrossRef]
- Allison, S. Biographic and Psychobehavioral Influences on Body Mass Index in a Nursing Sample. West. J. Nurs. Res. 2005, 27, 7–20. [Google Scholar] [CrossRef]
- Almajwal, A.M. Stress, shift duty, and eating behaviour among nurses in Central Saudi Arabia. Saudi Med. J. 2016, 37, 191–198. [Google Scholar] [CrossRef]
- Faugier, J.; Lancaster, J.; Pickles, D. Barriers to healthy eating in the nursing profession: Part 1 and part 2. Nurs. Stand. 2001, 15, 33–36. [Google Scholar] [PubMed]
- Burch, J.B.; Tom, J.; Zhai, Y. Shiftwork impacts and adaptation among health care workers. Occup. Med. (Lond.) 2009, 59, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Bonnell, E.K.; Huggins, C.E.; Huggins, C.T.; McCaffrey, T.A.; Palermo, C.; Bonham, M. Influences on Dietary Choices during Day versus Night Shift in Shift Workers: A Mixed Methods Study. Nutrients 2017, 9, 193. [Google Scholar] [CrossRef]
- Bass, J.; Takahashi, J.S. Circadian Integration of Metabolism and Energetics. Science 2010, 330, 1349–1354. [Google Scholar] [CrossRef]
- Habbal, O.A.; Al-Jabri, A.A. Circadian Rhythm and the Immune Response: A Review. Int. Rev. Immunol. 2009, 28, 93–108. [Google Scholar] [CrossRef]
- Hsieh, S.D.; Muto, T.; Murase, T.; Tsuji, H.; Arase, Y. Association of short sleep duration with obesity, diabetes, fatty liver and behavioral factors in Japanese men. Intern. Med. 2011, 50, 2499–2502. [Google Scholar] [CrossRef][Green Version]
- Colles, S.L.; Dixon, J.B.; O’Brien, P.E. Night eating syndrome and nocturnal snacking: Association with obesity, binge eating and psychological distress. Int. J. Obes. 2007, 31, 1722–1730. [Google Scholar] [CrossRef]
- Asher, G.; Sassone-Corsi, P. Time for Food: The Intimate Interplay between Nutrition, Metabolism, and the Circadian Clock. Cell 2015, 161, 84–92. [Google Scholar] [CrossRef]
- Eckel-Mahan, K.; Patel, V.R.; De Mateo, S.; Orozco-Solis, R.; Ceglia, N.J.; Sahar, S.; Dilag-Penilla, S.A.; Dyar, K.; Baldi, P.; Sassone-Corsi, P.; et al. Reprogramming of the circadian clock by nutritional challenge. Cell 2013, 155, 1464–1478. [Google Scholar] [CrossRef]
- Vogel, M.; Braungardt, T.; Meyer, W.; Schneider, W. The effects of shift work on physical and mental health. J. Neural Transm. 2012, 119, 1121–1132. [Google Scholar] [CrossRef]
- Hoogendoorn, W.E.; Van Poppel, M.N.M.; Bongers, P.M.; Koes, B.W.; Bouter, L. Systematic Review of Psychosocial Factors at Work and Private Life as Risk Factors for Back Pain. Spine 2000, 25, 2114–2125. [Google Scholar] [CrossRef] [PubMed]
- Goetz, K.; Berger, S.; Gavartina, A.; Zaroti, S.; Szecsenyi, J. How psychosocial factors affect well-being of practice assistants at work in general medical care?–A questionnaire survey. BMC Fam. Pract. 2015, 16, 166. [Google Scholar] [CrossRef] [PubMed]
- Shields, M. Shift work and health. Health Rep. 2002, 13, 11–33. [Google Scholar]
- Ohida, T.; Kamal, A.; Sone, T.; Ishii, T.; Uchiyama, M.; Minowa, M.; Nozaki, S. Night-shift work related problems in young female nurses in Japan. J. Occup. Health 2001, 43, 150–156. [Google Scholar] [CrossRef]
- Garde, A.H.; Hansen, A.M.; Hansen, J. Sleep length and quality, sleepiness and urinary melatonin among healthy Danish nurses with shift work during work and leisure time. Int. Arch. Occup. Environ. Health 2009, 82, 1219–1228. [Google Scholar] [CrossRef]
- Selvi, Y.; Güleç, M.; Agargun, M.Y.; Besiroglu, L. Mood changes after sleep deprivation in morningness?eveningness chronotypes in healthy individuals. J. Sleep Res. 2007, 16, 241–244. [Google Scholar] [CrossRef]
- Han, K.; Choi-Kwon, S.; Kim, K.S. Poor dietary behaviors among hospital nurses in Seoul, South Korea. Appl. Nurs. Res. 2016, 30, 38–44. [Google Scholar] [CrossRef]
- Torquati, L.; Kolbe-Alexander, T.; Pavey, T.; Perrsson, C.; Leveritt, M. Diet and physical activity behavior in nurses: A qualitative study. Int. J. Health Promot. Educ. 2016, 54, 268–282. [Google Scholar] [CrossRef]
- Anderson, J.W.; Patterson, K. Snack foods: Comparing nutrition values of excellent choices and “junk foods”. J. Am. Coll. Nutr. 2005, 24, 155–156. [Google Scholar] [CrossRef]
- Maillot, M.; Darmon, N.; Vieux, F.; Drewnowski, A. Low energy density and high nutritional quality are each associated with higher diet costs in French adults. Am. J. Clin. Nutr. 2007, 86, 690–696. [Google Scholar]
- Drewnowski, A. Concept of a nutritious food: Toward a nutrient density score. Am. J. Clin. Nutr. 2005, 82, 721–732. [Google Scholar] [CrossRef]
- Wells, A.S.; Read, N.W. Influences of fat, energy, and time of day on mood and performance. Physiol. Behav. 1996, 59, 1069–1076. [Google Scholar] [CrossRef]
- Adam, T.C.; Epel, E. Stress, eating and the reward system. Physiol. Behav. 2007, 91, 449–458. [Google Scholar] [CrossRef]
- Åkerstedt, T.; Knutsson, A.; Westerholm, P.; Theorell, T.; Alfredsson, L.; Kecklund, G. Sleep disturbances, work stress and work hours: A cross-sectional study. J. Psychosom. Res. 2002, 53, 741–748. [Google Scholar] [CrossRef]
- Cole, R.J.; Loving, R.T.; Kripke, D.F. Psychiatric aspects of shift work. Occup. Med. 1990, 5, 301–314. [Google Scholar]
- Black, J.E.; Hull, S.G.; Tiller, J.; Yang, R.; Harsh, J.R. The Long-Term Tolerability and Efficacy of Armodafinil in Patients with Excessive Sleepiness Associated with Treated Obstructive Sleep Apnea, Shift Work Disorder, or Narcolepsy: An Open-Label Extension Study. J. Clin. Sleep Med. 2010, 6, 458–466. [Google Scholar] [CrossRef]
- Schwartz, J.R.; Khan, A.; McCall, W.V.; Weintraub, J.; Tiller, J. Tolerability and Efficacy of Armodafinil in Naïve Patients with Excessive Sleepiness Associated with Obstructive Sleep Apnea, Shift Work Disorder, or Narcolepsy: A 12-Month, Open-Label, Flexible-Dose Study with an Extension Period. J. Clin. Sleep Med. 2010, 6, 450–457. [Google Scholar] [CrossRef]
- Boivin, D.B.; Boudreau, P. Impacts of shift work on sleep and circadian rhythms. Pathol. Boil. 2014, 62, 292–301. [Google Scholar] [CrossRef]
- Akerstedt, T.; Wright, K.P., Jr. Sleep Loss and Fatigue in Shift Work and Shift Work Disorder. Sleep Med. Clin. 2009, 4, 257–271. [Google Scholar] [CrossRef]
- Walker, J. Social problems of shift work. In Hours of Work–Temporal Factors in Work Scheduling; Folkard, S., Monk, T., Eds.; Wiley: New York, NY, USA, 1985; pp. 211–225. [Google Scholar]
- Stunkard, A.J.; Grace, W.J.; Wolff, H.G. The night-eating syndrome; a pattern of food intake among certain obese patients. Am. J. Med. 1955, 19, 78–86. [Google Scholar] [CrossRef]
- Kuldau, J.M.; Rand, C.S.W. The night eating syndrome and bulimia in the morbidly obese. Int. J. Eat. Disord. 1986, 5, 143–148. [Google Scholar] [CrossRef]
- Gluck, M.E.; Geliebter, A.; Satov, T. Night Eating Syndrome Is Associated with Depression, Low Self-Esteem, Reduced Daytime Hunger, and Less Weight Loss in Obese Outpatients. Obes. Res. 2001, 9, 264–267. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV, 4th ed.; American Psychiatric Association: Washington, DC, USA, 1994. [Google Scholar]
- Adami, G.F.; Campostano, A.; Marinari, G.M.; Ravera, G.; Scopinaro, N. Night eating in obesity: A descriptive study. Nutrition 2002, 18, 587–589. [Google Scholar] [CrossRef]
- Powers, P.S.; Perez, A.; Boyd, F.; Rosemurgy, A. Eating pathology before and after bariatric surgery: A prospective study. Int. J. Eat. Disord. 1999, 25, 293–300. [Google Scholar] [CrossRef]
- Greeno, C.G.; Wing, R.R.; Marcus, M.D. Nocturnal eating in binge eating disorder and matched-weight controls. Int. J. Eat. Disord. 1995, 18, 343–349. [Google Scholar] [CrossRef]
- Grilo, C.M.; Masheb, R.M. Night-time eating in men and women with binge eating disorder. Behav. Res. Ther. 2004, 42, 397–407. [Google Scholar] [CrossRef]
- Science News. Sleep Loss Linked to Night-Time Snacking, Junk Food Cravings, Obesity, Diabetes. 2018. Available online: https://www.sciencedaily.com/releases/2018/06/180601171900.htm (accessed on 25 November 2019).
- Bowman, S.A.; Vinyard, B.T. Fast food consumption of U.S. adults: Impact on energy and nutrient intakes and overweight status. J. Am. Coll. Nutr. 2004, 23, 163–168. [Google Scholar] [CrossRef]
- Zhao, I.; Bogossian, F.; Song, S.; Turner, C. The Association between Shift Work and Unhealthy Weight. J. Occup. Environ. Med. 2011, 53, 153–158. [Google Scholar] [CrossRef]
- Canuto, R.; Pattussi, M.P.; Macagnan, J.B.A.; Henn, R.L.; Olinto, M.T.A. Sleep deprivation and obesity in shift workers in southern Brazil. Public Health Nutr. 2014, 17, 2619–2623. [Google Scholar] [CrossRef]
- Kubo, T.; Oyama, I.; Nakamura, T.; Shirane, K.; Otsuka, H.; Kunimoto, M.; Kadowaki, K.; Maruyama, T.; Otomo, H.; Fujino, Y.; et al. Retrospective cohort study of the risk of obesity among shift workers: Findings from the Industry-based Shift Workers’ Health study, Japan. Occup. Environ. Med. 2010, 68, 327–331. [Google Scholar] [CrossRef]
- Jacobson, P.J.W.; Prawitz, A.D.; Lukaszuk, J.M. Long-Haul Truck Drivers Want Healthful Meal Options at Truck-Stop Restaurants. J. Am. Diet. Assoc. 2007, 107, 2125–2129. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Rong, Y.; Huang, X.; Lai, H.; Luo, X.; Zhang, Z.; Liu, Y.; He, M.; Wu, T.; Chen, W. Shift Work and the Relationship with Metabolic Syndrome in Chinese Aged Workers. PLoS ONE 2015, 10, e0120632. [Google Scholar] [CrossRef] [PubMed]
| Study & Country | Method | Sample Size (n) | Disease Related to Shift Works | Description on the Disease |
|---|---|---|---|---|
| Nikpour et al. [55] (Iran) | Cross-sectional study | 209 | Metabolic syndrome | Diagnostic criteria: simultaneously met three out of five criteria: (1) Hypertension, BP > 130/85 mmHg; (2) High serum TG level > 150 mg/dl; (3) High FBS > 110 mg/dl; (4) Low serum HDL level < 50 mg/dl; (5) Abdominal obesity, WC > 88 cm |
| Thomas et al. [22] (United Kingdom) | Large population-based cohort study | 7839 | Cardiovascular disease | Risk factors of cardiovascular disease such as adiposity, blood pressure, blood lipids, blood glucose, and level of inflammatory factors |
| Koh et al. [56] (Korea) | Cross-sectional study | 203 | Gastrointestinal disorders | Diseases include irritable bowel syndrome, functional dyspepsia |
| Knutsson et al. [57] (Sweden) | Longitudinal cohort study | 549 | Breast cancer | Increased risk for breast cancer among women who work in night shifts |
| Ferri et al. [24] (Italy) | Cross-sectional study | 213 | Psychological disorders | Job dissatisfaction, poor sleep quantity and quality, chronic fatigue, psychological stress |
| Study & Country | Sampling Frame | Method | Sample Size (n) | Criteria Used | Prevalence of Overweight/Obesity |
|---|---|---|---|---|---|
| Zhao et al. [149] (Australia) | Nurses and midwives | Cross-sectional study | 1235 | WHO | 32.9% overweight; 27.4% obesity |
| Canuto et al. [150] (Brazil) | Shift workers in poultry-processing plant | Cross-sectional study | 580 | WHO | 11.2% obesity |
| Kubo et al. [151] (Japan) | Shift workers manufacturing industry-based corporation | Retrospective cohort study | 920 | Obesity (BMI ≥ 25.0 kg/m2) | 21.1% obesity |
| Whitfield et al. [152] (United States) | Long-haul truck drivers | Cross-sectional study | 92 | WHO | 86% overweight; 66% obesity |
| Guo et al. [153] (China) | Shift workers in motor corporation | Cross-sectional study with retrospective assessment | 9088 | Obesity (BMI ≥ 28.0 kg/m2) | 13.5% obesity |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohd Azmi, N.A.S.; Juliana, N.; Mohd Fahmi Teng, N.I.; Azmani, S.; Das, S.; Effendy, N. Consequences of Circadian Disruption in Shift Workers on Chrononutrition and their Psychosocial Well-Being. Int. J. Environ. Res. Public Health 2020, 17, 2043. https://doi.org/10.3390/ijerph17062043
Mohd Azmi NAS, Juliana N, Mohd Fahmi Teng NI, Azmani S, Das S, Effendy N. Consequences of Circadian Disruption in Shift Workers on Chrononutrition and their Psychosocial Well-Being. International Journal of Environmental Research and Public Health. 2020; 17(6):2043. https://doi.org/10.3390/ijerph17062043
Chicago/Turabian StyleMohd Azmi, Nor Amira Syahira, Norsham Juliana, Nur Islami Mohd Fahmi Teng, Sahar Azmani, Srijit Das, and Nadia Effendy. 2020. "Consequences of Circadian Disruption in Shift Workers on Chrononutrition and their Psychosocial Well-Being" International Journal of Environmental Research and Public Health 17, no. 6: 2043. https://doi.org/10.3390/ijerph17062043
APA StyleMohd Azmi, N. A. S., Juliana, N., Mohd Fahmi Teng, N. I., Azmani, S., Das, S., & Effendy, N. (2020). Consequences of Circadian Disruption in Shift Workers on Chrononutrition and their Psychosocial Well-Being. International Journal of Environmental Research and Public Health, 17(6), 2043. https://doi.org/10.3390/ijerph17062043