Sexually Transmitted Diseases and Their Associated Factors in a Cohort in Da Nang City: An Alarming Trend in Syphilis Rates and Infection at Young Ages
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Considerations and Study Population
2.2. Participants
2.3. Microbiology Laboratory Assessment
2.4. Statistical Analysis
3. Results
3.1. Demographic Characteristics of Study Cohort
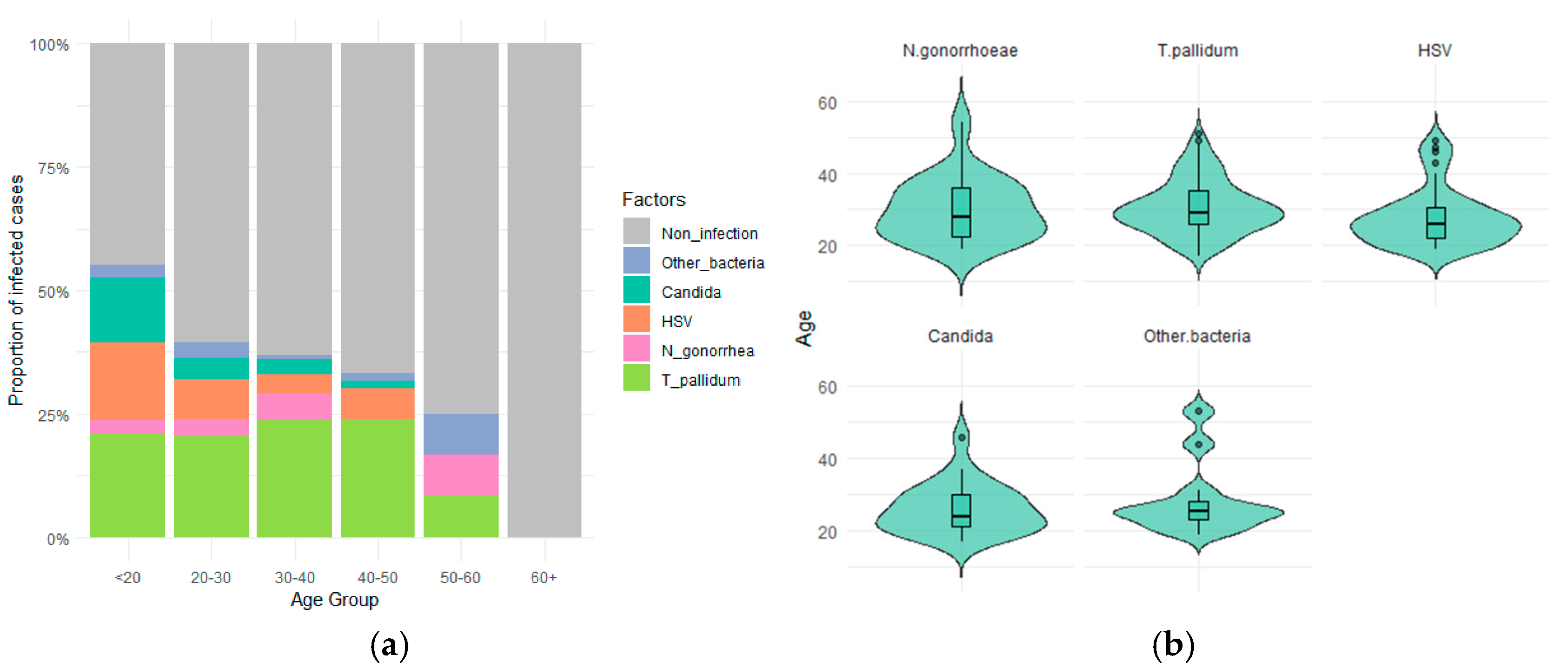
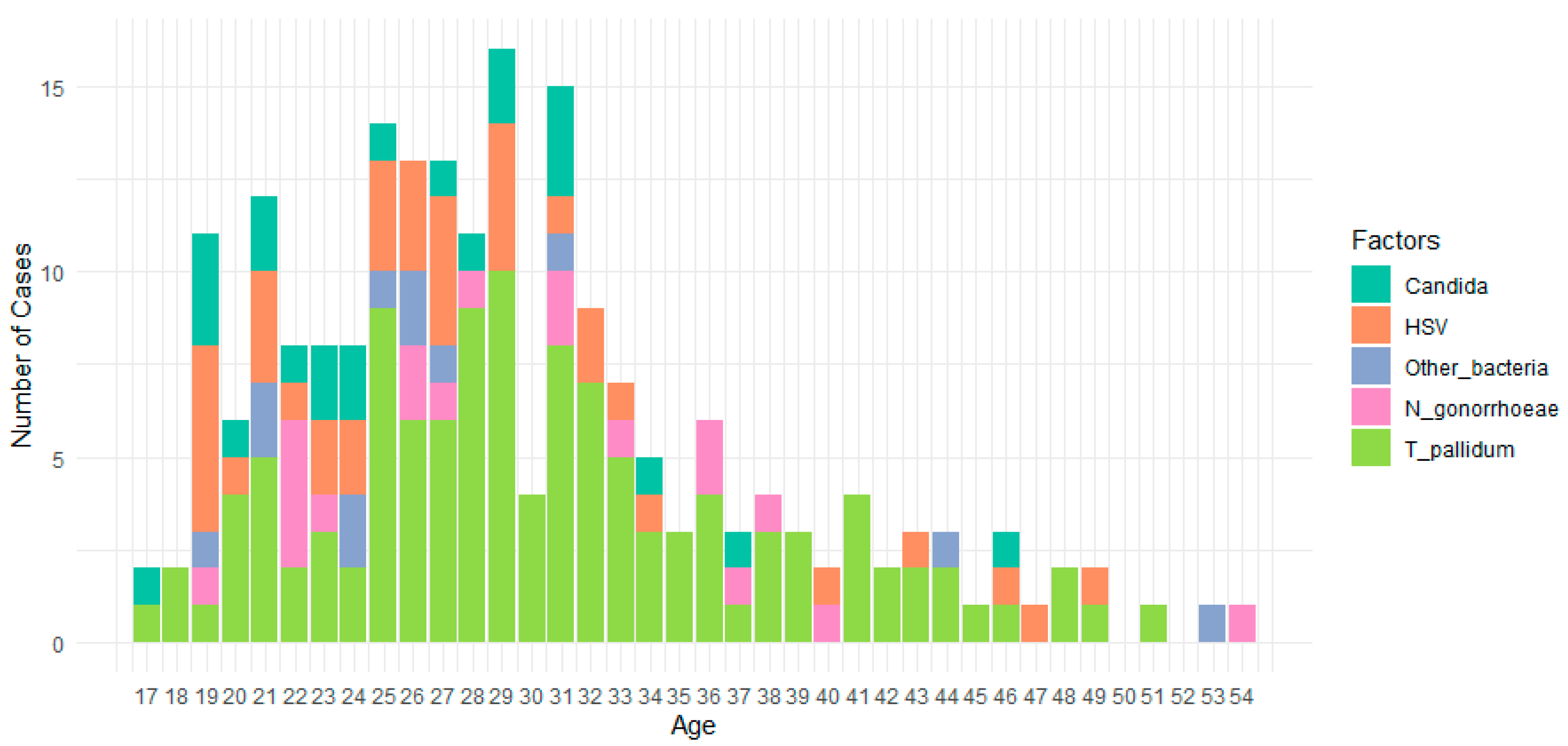
3.2. Prevalence of Pathogens in Target Infections over Different Age Groups
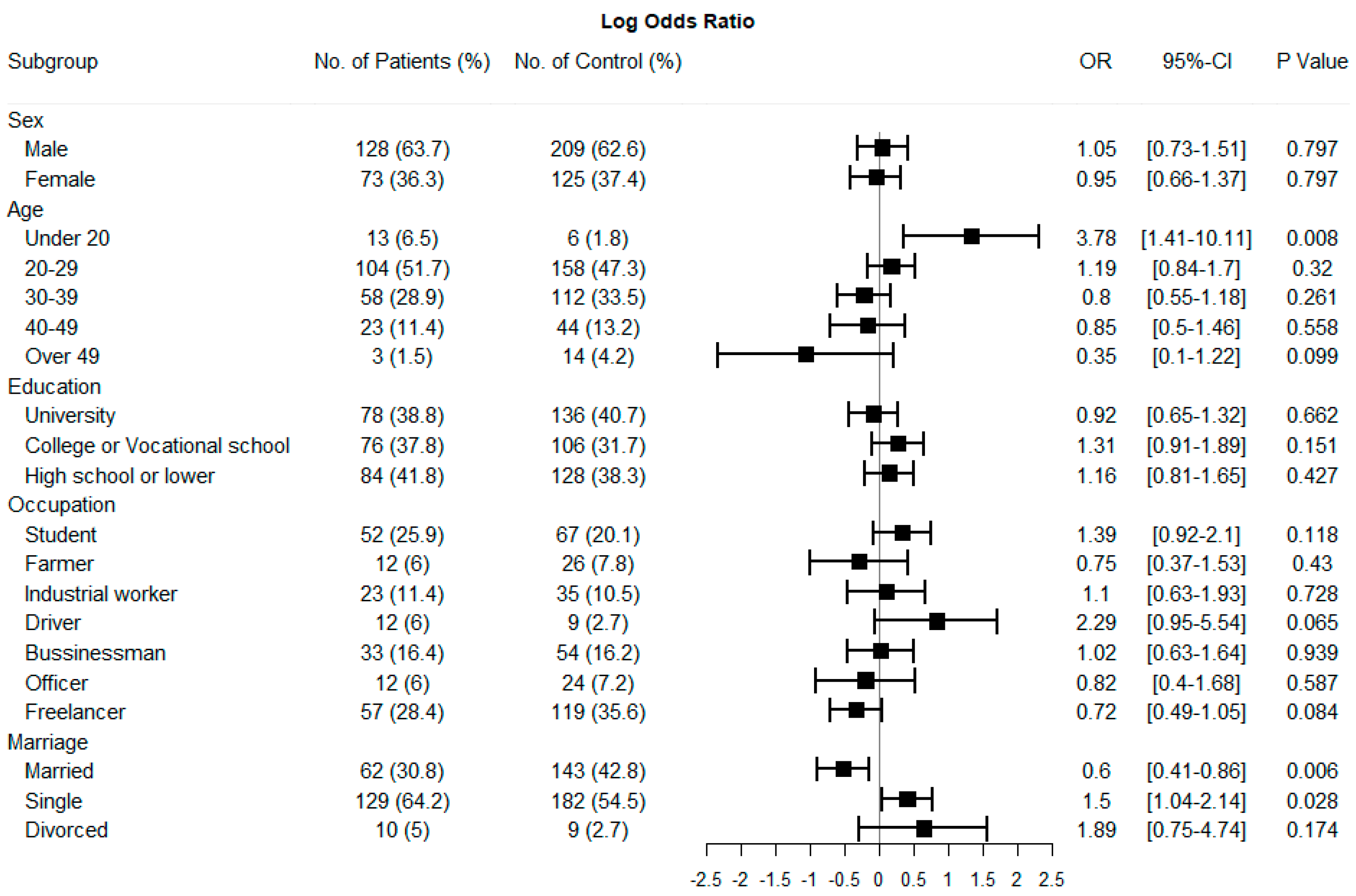
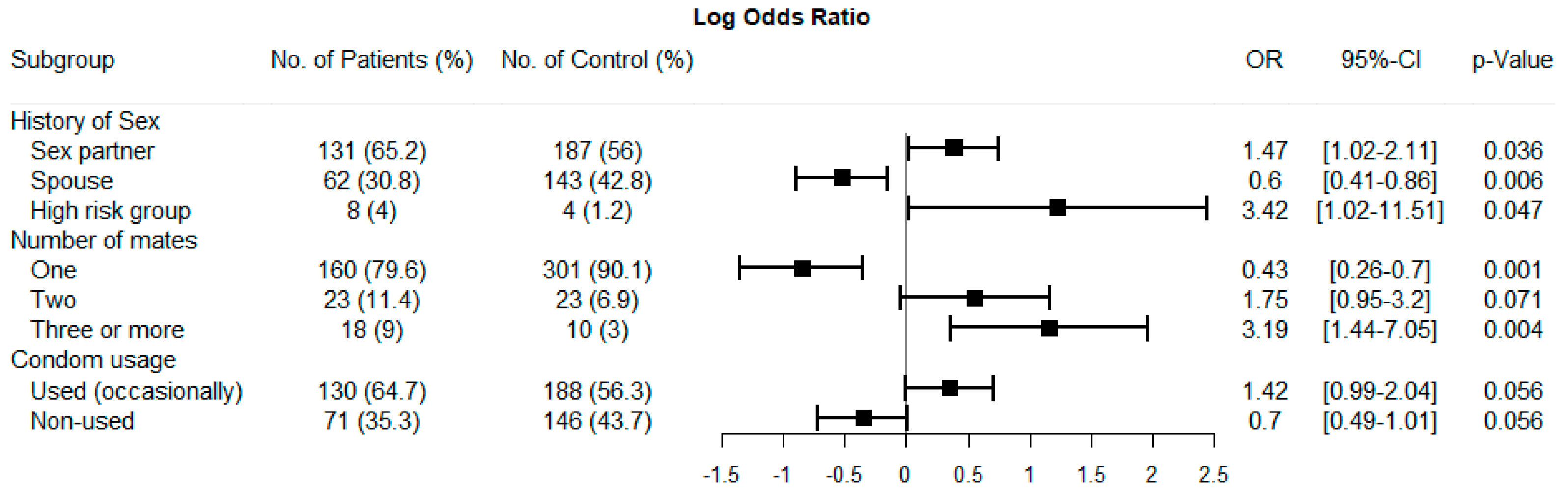
3.3. Correlation of Associated Risk Factors and Target Infections
4. Discussion
4.1. Scenario of Infection in Our Cohort
4.2. Factors Related to Infection Prevalence
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BV | Bacterial vaginosis |
| CIs | Confidence intervals |
| FSWs | Female sex workers |
| GTIs | Genital tract infections |
| HSV | Herpes Simplex Virus |
| LGTIs | Lower genital tract infections |
| MSM | Men who have sex with men |
| OR | Odds ratio |
| RPR | Rapid Plasma Reagin |
| STIs | Sexually transmitted infections |
| TPHA | Treponema pallidum hemagglutination assay |
References
- Brunham, R.C.; Paavonen, J. Reproductive system infections in women: Lower genital tract syndromes. Pathog. Dis. 2020, 78, ftaa022. [Google Scholar] [CrossRef] [PubMed]
- Soong, T.R.; Granter, S.R.; Haefner, H.K.; Laga, A.C. Chapter 4—Infectious Disorders of the Lower Genital Tract. In Diagnostic Gynecologic and Obstetric Pathology, 3rd ed.; ELSEVIER Inc.: Philadelphia, PA, USA, 2018; pp. 62–100. [Google Scholar] [CrossRef]
- De Seta, F.; Guaschino, S.; Larsen, B.; Donders, G.; Andabati, G. The infections of lower genital tract. Infect. Dis. Obstet. Gynecol. 2012, 2012, 926435. [Google Scholar] [CrossRef][Green Version]
- Errol, R.; Norwitz, M.D.; George, R.S.; Hugh, M.; Davidson, C.M. Lower Genital Tract Infection. In Obstetric Clinical Algorithms, 2nd ed.; Wiley Co.: Hoboken, NJ, USA, 2016. [Google Scholar]
- WHO. Consultancy/APW—Terms of Reference—Technical Assistance for Rapid Assessment of Sexually Transmitted Disease in Viet Nam; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Rowley, J.; Vander Hoorn, S.; Korenromp, E.; Low, N.; Unemo, M.; Abu-Raddad, L.J.; Chico, R.M.; Smolak, A.; Newman, L.; Gottlieb, S.; et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: Global prevalence and incidence estimates, 2016. Bull. World Health Organ. 2019, 97, 548–562. [Google Scholar] [CrossRef] [PubMed]
- Kojima, N.; Klausner, J.D. An update on the global epidemiology of syphilis. Curr. Epidemiol. Rep. 2018, 5, 24–38. [Google Scholar] [CrossRef]
- Spiteri, G.; Unemo, M.; Mårdh, O.; Amato-Gauci, A. The resurgence of syphilis in high-income countries in the 2000s: A focus on Europe. Epidemiol. Infect. 2019, 147, e143. [Google Scholar] [CrossRef]
- Chen, J.S.; Levintow, S.N.; Tran, H.V.; Sripaipan, T.; Nguyen, M.X.; Nguyen, S.M.; Miller, W.C.; Go, V.F.; Giang, L.M. HIV and STI prevalence and testing history among men who have sex with men in Hanoi, Vietnam. Int. J. STD AIDS 2022, 33, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Thanh Nguyen, H.T.; Nguyen, L.T.; Thanh Hoang, H.T.; Bui, D.H.; Thu Phan, H.T.; Van Khuu, N.; Hong Ngo, H.T.; Dang, D.A.; Mirzazadeh, A.; McFarland, W.; et al. Increase in human immunodeficiency virus and syphilis prevalence and incidence among men who have sex with men, vietnam 2015–2020. Int. J. STD AIDS 2024, 35, 197–205. [Google Scholar] [CrossRef]
- Nguyen, T.V.; Tran, H.P.; Khuu, N.V.; Nguyen, P.D.; Le, T.N.; Hoang, C.D.; Tran, T.; Le, T.Q.; Pham, Q.D.; Phan, L.T. Increases in both HIV and syphilis among men who have sex with men in Vietnam: Urgent need for comprehensive responses. Int. J. STD AIDS 2021, 32, 1298–1307. [Google Scholar] [CrossRef]
- Son, V.H.; Safarnejad, A.; Nga, N.T.; Linh, V.M.; Tu, L.T.C.; Manh, P.D.; Long, N.H.; Abdul-Quader, A. Estimation of the Population Size of Men Who Have Sex with Men in Vietnam: Social App Multiplier Method. JMIR Public Health Surveill. 2019, 5, e12451. [Google Scholar] [CrossRef]
- WHO. Guidelines for the Management of Symptomatic Sexually Transmitted Infections; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Vietnamese Ministry of Health. Decision on the Promulgation of Guidelines for the Diagnosis and Treatment of Sexually Transmitted Diseases; Vietnamese Ministry of Health: Hanoi, Vietnam, 2013. [Google Scholar]
- Hang, T.P.; Truc, P.T.N.; Loi, V.T. Prevalence of lower genital tract infections and associated factors among the women at medical centers, Ca Mau city in 2023–2024. Can Tho J. Med. Pharm. 2024, 77, 43–49. [Google Scholar] [CrossRef]
- Ginindza, T.G.; Stefan, C.D.; Tsoka-Gwegweni, J.M.; Dlamini, X.; Jolly, P.E.; Weiderpass, E.; Broutet, N.; Sartorius, B. Prevalence and risk factors associated with sexually transmitted infections (STIs) among women of reproductive age in Swaziland. Infect. Agents Cancer 2017, 12, 29. [Google Scholar] [CrossRef] [PubMed]
- An, N.V.; Luong, V.H.; Vinh, N.T.H.; Hoa, P.Q.; My, L.H.; Hoàng, L.H.; Viet, N.H.; Nam, N.T.; Hai, L.H.L. Antimicrobial resistance patterns of Neisseria gonorrheae at the National hospital of Dermatology and venereology in 2022. Vietnam Med. J. 2024, 538, 266–270. [Google Scholar] [CrossRef]
- Cannovo, N.; Bianchini, E.; Gironacci, L.; Garbati, E.; Di Prospero, F.; Cingolani, M.; Scendoni, R.; Fedeli, P. Sexually Transmitted Infections in Adolescents and Young Adults: A Cross Section of Public Health. Int. J. Environ. Res. Public Health 2024, 21, 501. [Google Scholar] [CrossRef] [PubMed]
- Whiting, C.; Schwartzman, G.; Khachemoune, A. Syphilis in dermatology: Recognition and management. Am. J. Clin. Dermatol. 2023, 24, 287–297. [Google Scholar] [CrossRef]
- Peeling, R.W.; Mabey, D.; Chen, X.S.; Garcia, P.J. Syphilis. Lancet 2023, 402, 336–346. [Google Scholar] [CrossRef]
- Mahmud, S.; Mohsin, M.; Muyeed, A.; Islam, M.M.; Hossain, S.; Islam, A. Prevalence of HIV and syphilis and their co-infection among men having sex with men in Asia: A systematic review and meta-analysis. Heliyon 2023, 9, e13947. [Google Scholar] [CrossRef]
- Tao, Y.T.; Gao, T.Y.; Li, H.Y.; Ma, Y.T.; Li, H.J.; Xian-Yu, C.Y.; Deng, N.J.; Zhang, C. Global, regional, and national trends of syphilis from 1990 to 2019: The 2019 global burden of disease study. BMC Public Health 2023, 23, 754. [Google Scholar] [CrossRef]
- Feng, Y.; Wu, Z.; Detels, R.; Qin, G.; Liu, L.; Wang, X.; Wang, J.; Zhang, L. HIV/STD prevalence among men who have sex with men in Chengdu, China and associated risk factors for HIV infection. J. Acquir. Immune Defic. Syndr. 2010, 53, S74–S80. [Google Scholar] [CrossRef]
- Regional Office for South-East Asia. Moving Ahead on Elimination of Sexually Transmitted Infections (STIs) in WHO South-East Asia Region—Progress and Challenges; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Sharma, M.; Rewari, B.B.; Aditama, T.Y.; Turlapati, P.; Dallabetta, G.; Steen, R. Control of sexually transmitted infections and global elimination targets, South-East Asia Region. Bull. World Health Organ. 2021, 99, 304–311. [Google Scholar] [CrossRef]
- Daiane de Peder, L.; Mesquita da Silva, C.; Nascimento, B.L.; Malizan, J.A.; Madeira, H.S.; Horvath, J.D.; Silva, E.S.; Vieira Teixeira, J.J. Prevalence of Sexually Transmitted Infections and Risk Factors Among Young People in a Public Health Center in Brazil: A Cross-Sectional Study. J. Pediatr. Adolesc. Gynecol. 2020, 33, 354–362. [Google Scholar] [CrossRef]
- Yamani, L.N.; Astutik, E.; Qurniyawati, E.; Lusida, M.I.; Getaneh, Y.; Kelly, M. Associations between socio-demographics, sexual knowledge and behaviour and sexually transmitted infections among reproductive-age women in Southeast Asia: Demographic Health Survey results. BMC Public Health 2025, 25, 738. [Google Scholar] [CrossRef] [PubMed]
- Son, D.T.; Oh, J.; Heo, J.; Van Huy, N.; Van Minh, H.; Choi, S.; Hoat, L.N. Early sexual initiation and multiple sexual partners among Vietnamese women: Analysis from the Multiple Indicator Cluster Survey, 2011. Glob. Health Action 2016, 9, 29575. [Google Scholar] [CrossRef] [PubMed]
- Alfonsi, G.A.; Shlay, J.C. The effectiveness of condoms for the prevention of sexually transmitted diseases. Curr. Women’s Health Rev. 2005, 1, 151–159. [Google Scholar] [CrossRef]
- Garnett, G.; White, P.; Ward, H. Fewer partners or more condoms? Modelling the effectiveness of STI prevention interventions. Sex. Transm. Infect. 2008, 84, ii4–ii11. [Google Scholar] [CrossRef]
| Factor | Group | No (%) |
|---|---|---|
| Sex | Male | 337 (63.0) |
| Female | 198 (37.0) | |
| Residence | Urban | 383 (71.6) |
| Rural | 152 (28.4) | |
| Age group | <20 | 19 (3.6) |
| 20–29 | 262 (48.9) | |
| 30–39 | 170 (31.8) | |
| 40–49 | 67 (12.5) | |
| >49 | 17 (3.2) | |
| Education | University | 214 (40.0) |
| College or vocational school | 109 (20.4) | |
| High school or lower | 212 (39.6) | |
| Occupation | Student | 119 (22.2) |
| Farmer | 38 (7.1) | |
| Industrial worker | 58 (10.8) | |
| Driver | 21 (3.9) | |
| Businessman | 87 (16.3) | |
| Officer | 36 (6.7) | |
| Freelancer | 176 (32.9) | |
| Marriage | Single | 311 (58.1) |
| Married | 205 (38.3) | |
| Divorced | 19 (3.6) | |
| Sexual history | Non-spousal partner | 318 (59.4) |
| Spouse | 205 (38.3) | |
| High-risk group | 12 (2.3) | |
| Number of sexual partners | 1 | 461 (86.2) |
| 2 | 46 (8.6) | |
| ≥3 | 28 (5.2) | |
| Used (regularly) | 0 (0) | |
| Condom usage | Used (occasionally) | 322 (60.2) |
| Not used | 213 (39.8) |
| Group | Number | Percent (%) |
|---|---|---|
| Negative | 334 | 62.4 |
| Positive | 201 | 37.6 |
| T. pallidum | 114 (95M, 19F) | 21.3 |
| N. gonorrhoeae | 17 (16M, 1F) | 3.2 |
| HSV | 32 (14M, 18F) | 6.0 |
| Other local vaginal bacteria | 9 (0M, 9F) | 1.7 |
| Candida sp. | 21 (0M, 21F) | 3.9 |
| Trichomonas vaginalis | 0 | 0.0 |
| T. pallidum + N. gonorrhoeae | 2 (2M, 0F) | 0.4 |
| T. pallidum + HSV | 1 (1M, 0F) | 0.2 |
| HSV + Candida sp. | 2 (0M, 2F) | 0.4 |
| HSV + Other local vaginal bacteria | 3 (0M, 3F) | 0.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Hellenic Society for Microbiology. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Le, T.T.; Nguyen, T.T.; Nguyen, N.D.; Nguyen, H.H.; Hoang, H.T.; Bui, L.T.; Nguyen, M.V.; Dang, C.P.; Cao, V. Sexually Transmitted Diseases and Their Associated Factors in a Cohort in Da Nang City: An Alarming Trend in Syphilis Rates and Infection at Young Ages. Acta Microbiol. Hell. 2025, 70, 23. https://doi.org/10.3390/amh70020023
Le TT, Nguyen TT, Nguyen ND, Nguyen HH, Hoang HT, Bui LT, Nguyen MV, Dang CP, Cao V. Sexually Transmitted Diseases and Their Associated Factors in a Cohort in Da Nang City: An Alarming Trend in Syphilis Rates and Infection at Young Ages. Acta Microbiologica Hellenica. 2025; 70(2):23. https://doi.org/10.3390/amh70020023
Chicago/Turabian StyleLe, Thuy Thi, Trinh ThiDoan Nguyen, Ngan DangThu Nguyen, Hoang Huy Nguyen, Hoa ThiMinh Hoang, Lam ThiKieu Bui, Minh Van Nguyen, Cong Phi Dang, and Van Cao. 2025. "Sexually Transmitted Diseases and Their Associated Factors in a Cohort in Da Nang City: An Alarming Trend in Syphilis Rates and Infection at Young Ages" Acta Microbiologica Hellenica 70, no. 2: 23. https://doi.org/10.3390/amh70020023
APA StyleLe, T. T., Nguyen, T. T., Nguyen, N. D., Nguyen, H. H., Hoang, H. T., Bui, L. T., Nguyen, M. V., Dang, C. P., & Cao, V. (2025). Sexually Transmitted Diseases and Their Associated Factors in a Cohort in Da Nang City: An Alarming Trend in Syphilis Rates and Infection at Young Ages. Acta Microbiologica Hellenica, 70(2), 23. https://doi.org/10.3390/amh70020023






