Cardiovascular Surgery in Conflict Zones: Insights from 2169 Cases in Wartime Yemen
Abstract
1. Introduction
2. Materials and Methods
Analyses
3. Results
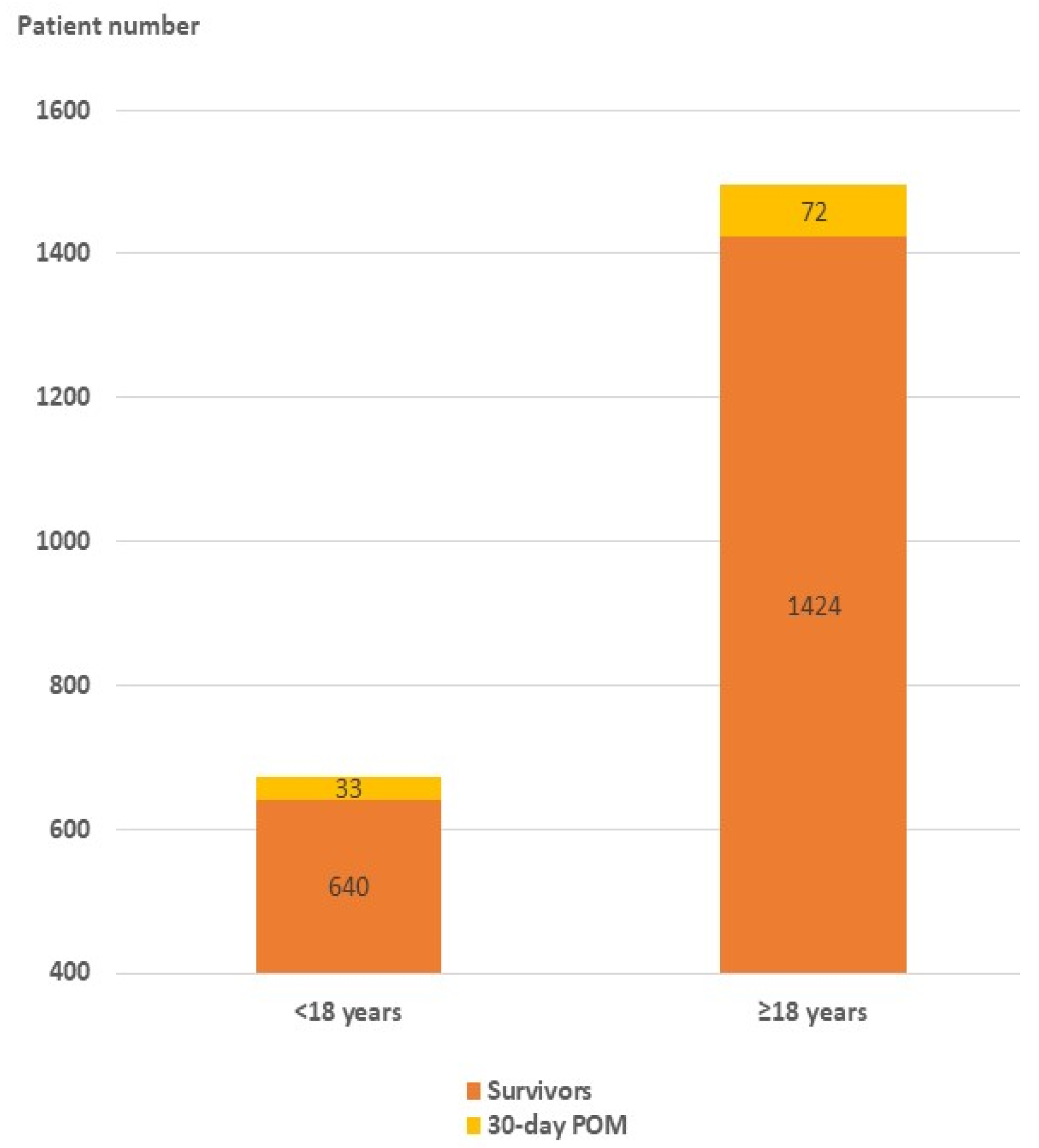
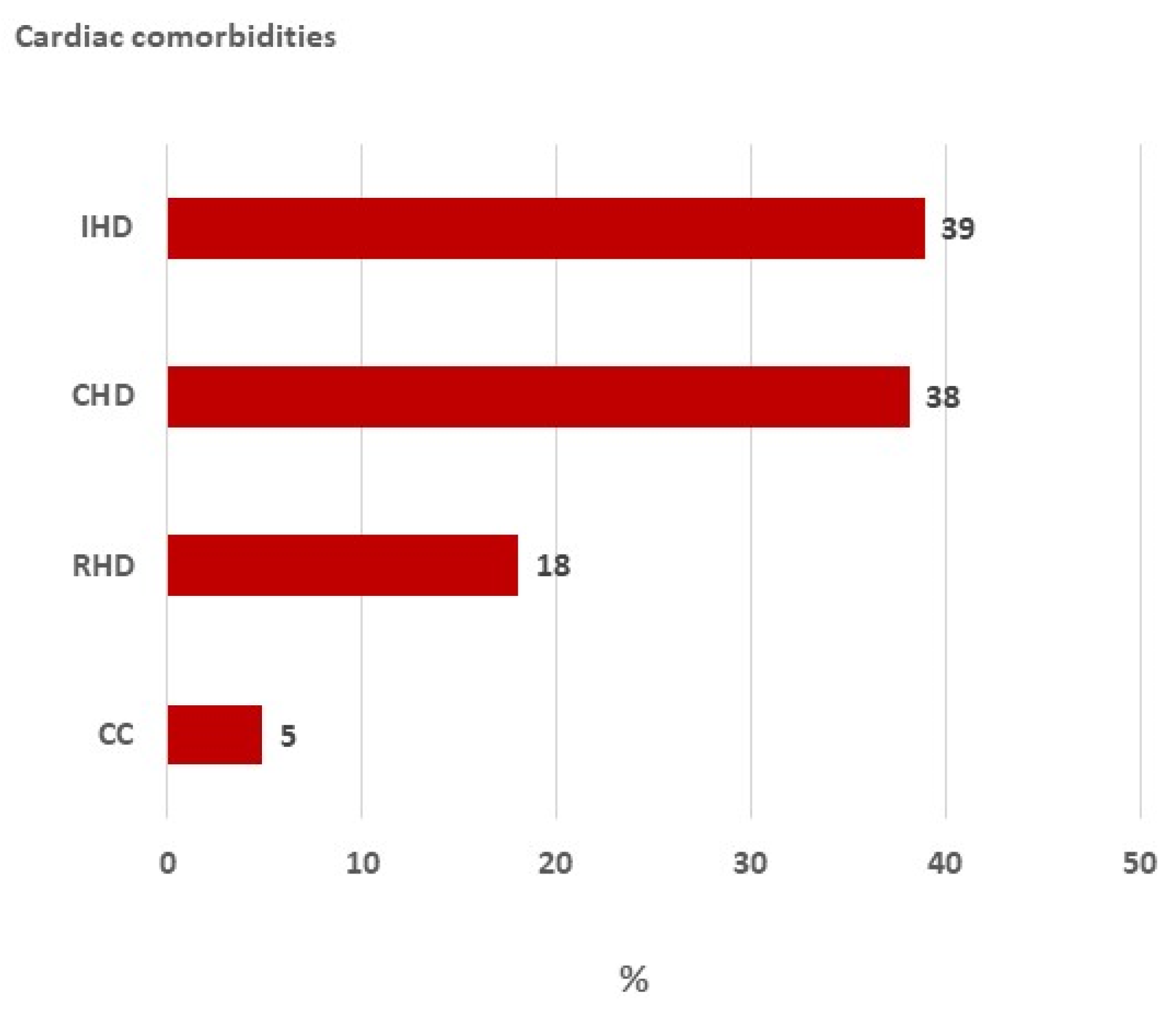
3.1. Demographic Data
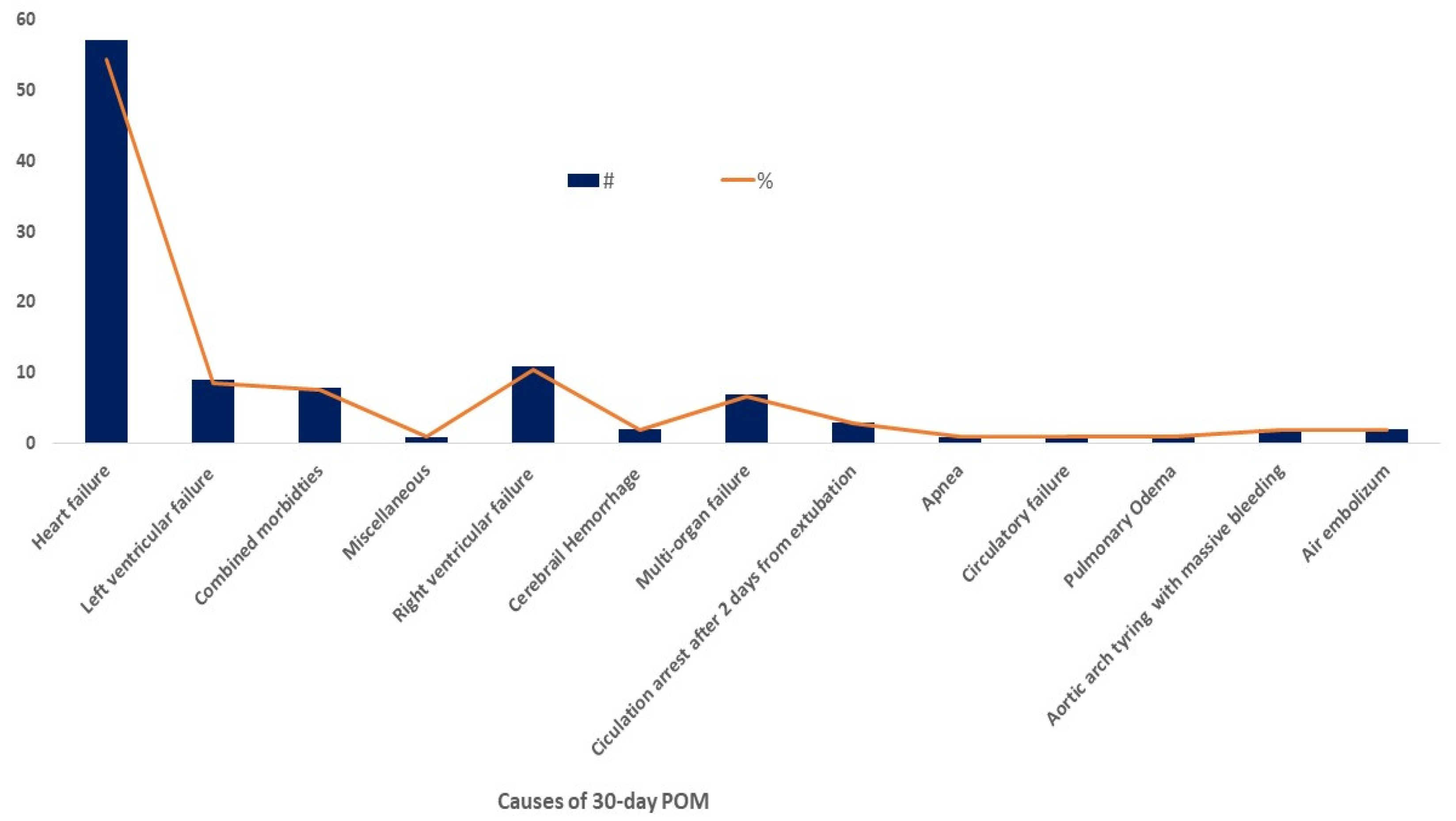
3.2. Causes of Mortality
3.3. Clinical and Intraoperative Variables Associated with Mortality
3.4. Clinical Variables Predicting Mortality in Post-Cardiovascular Surgical Patients
4. Discussion
5. Conclusions
Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jawad, M.; Vamos, E.P.; Najim, M.; Roberts, B.; Millett, C. Impact of Armed Conflict on Cardiovascular Disease Risk: A Systematic Review. Heart 2019, 105, 1388–1394. [Google Scholar] [CrossRef]
- Roth, G.A.; Johnson, C.; Abajobir, A.; Abd-Allah, F.; Abera, S.F.; Abyu, G.; Ahmed, M.; Aksut, B.; Alam, T.; Alam, K.; et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017, 70, 1–25. [Google Scholar] [CrossRef]
- Alsabri, M.; Alsakkaf, L.M.; Alhadheri, A.; Cole, J.; Burkle, F.M. Chronic Health Crises and Emergency Medicine in War-Torn Yemen, Exacerbated by the COVID-19 Pandemic. West. J. Emerg. Med. 2022, 23, 276–284. [Google Scholar] [CrossRef] [PubMed]
- Ripoll Gallardo, A.; Burkle, F.M.; Ragazzoni, L.; Della Corte, F. Yemen’s Unprecedented Humanitarian Crisis: Implications for International Humanitarian Law, the Geneva Convention, and the Future of Global Health Security. Disaster Med. Public Health Prep. 2016, 10, 701–703. [Google Scholar] [CrossRef] [PubMed]
- Salem, A.; Rosen, A.; Alharazi, I.; Gamallat, Y.; Aldbyani, A.; Amer, B.; Chimpandu, N. Healthcare Accessibility in Yemen’s Conflict Zones: Comprehensive Review Focused on Strategies and Solutions. Confl. Health 2025, 19, 42. [Google Scholar] [CrossRef]
- Jayed, D.; Al-Huthi, M.A.; Al-Zandani, A.; Al-Shuki, S.; Al-Dholae, M.; Al-Moqri, M. Spectrum of Heart Diseases in Sanaa, Capital of Yemen Republic. Open Access Libr. J. 2023, 10, 1–14. [Google Scholar] [CrossRef]
- Mohamed Ibrahim, M.I.; Alshakka, M.; Al-abd, N.; Bahattab, A.; Badulla, W. Availability of Essential Medicines in a Country in Conflict: A Quantitative Insight from Yemen. Int. J. Environ. Res. Public Health 2021, 18, 175. [Google Scholar] [CrossRef]
- Munibari, A.-N.; Alansi, A.K.; Al-Jaber, N.; Hidar, F.; Al-Kadi, A.-A. The Economic Burden of Cardiovascular Diseases in Yemen: An Example of Annual Direct Costs from the Cardiac Center–Althawra Teaching General Hospital- Sana’a. Hadhramout J. Med. Sci. 2014, 3, 253–258. [Google Scholar]
- Silva-Tejada, H.; Sisniegas-Razón, J.; Martínez-Ninanqui, F.; Díaz-Chávez, Z.; Ríos-Ortega, J.C. Perioperative morbidity and mortality of cardiac surgeries at the Instituto Nacional Cardiovascular, Lima, Peru, during the year 2023. Arch. Peru. Cardiol. Cir. Cardiovasc. 2025, 6, 36–43. [Google Scholar] [CrossRef]
- Siregar, S.; Groenwold, R.H.H.; de Mol, B.A.J.M.; Speekenbrink, R.G.H.; Versteegh, M.I.M.; Brandon Bravo Bruinsma, G.J.; Bots, M.L.; van der Graaf, Y.; van Herwerden, L.A. Evaluation of Cardiac Surgery Mortality Rates: 30-Day Mortality or Longer Follow-Up? Eur. J. Cardiothorac. Surg. 2013, 44, 875–883. [Google Scholar] [CrossRef] [PubMed]
- Vogt, A.; Grube, E.; Glunz, H.G.; Hauptmann, K.E.; Sechtem, U.; Mäurer, W.; Tebbe, U.; Heinrich, K.W.; Engel, H.J.; Kettner, W.; et al. Determinants of Mortality after Cardiac Surgery: Results of the Registry of the Arbeitsgemeinschaft Leitender Kardiologischer Krankenhausärzte (ALKK) on 10 525 Patients. Eur. Heart J. 2000, 21, 28–32. [Google Scholar] [CrossRef]
- Squiccimarro, E.; Stasi, A.; Lorusso, R.; Paparella, D. Narrative Review of the Systemic Inflammatory Reaction to Cardiac Surgery and Cardiopulmonary Bypass. Artif. Organs 2022, 46, 568–577. [Google Scholar] [CrossRef] [PubMed]
- Aladwan, H.; Alshoubaki, W.; Alqaisi, A.I.; Abuamereh, H.A.; Alatoum, L.M.; Mohd, A.F. Impact of Duration of Cardiopulmonary Bypass on Recovery after Open Heart Surgery. Int. J. Adv. Med. 2024, 11, 185–188. [Google Scholar] [CrossRef]
- Chan, J.; Oo, S.; Butt, S.; Benedetto, U.; Caputo, M.; Angelini, G.D.; Vohra, H.A. Network Meta-Analysis Comparing Blood Cardioplegia, Del Nido Cardioplegia and Custodiol Cardioplegia in Minimally Invasive Cardiac Surgery. Perfusion 2023, 38, 464–472. [Google Scholar] [CrossRef] [PubMed]
- Abah, U.; Roberts, P.G.; Ishaq, M.; De Silva, R. Is Cold or Warm Blood Cardioplegia Superior for Myocardial Protection? Interact. Cardiovasc. Thorac. Surg. 2012, 14, 848–855. [Google Scholar] [CrossRef]
- Kot, T.K.M.; Chan, J.S.K.; Froghi, S.; Lau, D.H.H.; Morgan, K.; Magni, F.; Harky, A. Warm versus Cold Cardioplegia in Cardiac Surgery: A Meta-Analysis with Trial Sequential Analysis. JTCVS Open 2021, 6, 161–190. [Google Scholar] [CrossRef] [PubMed]
- Mve Mvondo, C.; Giamberti, A.; Ngowe Ngowe, M.; Mbuoh, H.A.; Milocco, I.; Tsague Kengni, H.N.; Cirri, S.; Frigiola, A. Cardiac Surgery Development in Cameroon: Unexpected Challenges From a Socio-Political Crisis. Front. Cardiovasc. Med. 2022, 9, 778075. [Google Scholar] [CrossRef]
- Slusher, T.M.; Kiragu, A.W.; Day, L.T.; Bjorklund, A.R.; Shirk, A.; Johannsen, C.; Hagen, S.A. Pediatric Critical Care in Resource-Limited Settings-Overview and Lessons Learned. Front. Pediatr. 2018, 6, 49. [Google Scholar] [CrossRef]
- Salsano, A.; Giacobbe, D.R.; Sportelli, E.; Olivieri, G.M.; Natali, R.; Prevosto, M.; Del Bono, V.; Viscoli, C.; Santini, F. Aortic Cross-Clamp Time and Cardiopulmonary Bypass Time: Prognostic Implications in Patients Operated on for Infective Endocarditis. Interact. Cardiovasc. Thorac. Surg. 2018, 27, 328–335. [Google Scholar] [CrossRef]
- Zhang, Y.; Zheng, Q.; Dai, X.; Xu, X.; Ma, L. Overweight Is Associated with Better One-Year Survival in Elderly Patients after Cardiac Surgery: A Retrospective Analysis of the MIMIC-III Database. J. Thorac. Dis. 2021, 13, 562. [Google Scholar] [CrossRef]
- Koth, A.M.; Algaze, C.A.; Sakarovitch, C.; Long, J.; Kamra, K.; Wright, G.E.; Alexander-Banys, B.; Maeda, K.; Shin, A.Y. Younger Age Remains a Risk Factor for Prolonged Length of Stay after Bidirectional Cavopulmonary Anastomosis. Cardiol. Young 2019, 29, 369–374. [Google Scholar] [CrossRef] [PubMed]
- Mehmood, A.; Ismail, S.R.; Kabbani, M.S.; Abu-Sulaiman, R.M.; Najm, H.K. Outcome of Low Body Weight (<2.2 Kg) Infants Undergoing Cardiac Surgery. J. Saudi Heart Assoc. 2014, 26, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Potapov, E.V.; Loebe, M.; Anker, S.; Stein, J.; Bondy, S.; Nasseri, B.A.; Sodian, R.; Hausmann, H.; Hetzer, R. Impact of Body Mass Index on Outcome in Patients after Coronary Artery Bypass Grafting with and without Valve Surgery1. Eur. Heart J. 2003, 24, 1933–1941. [Google Scholar] [CrossRef] [PubMed]
| Variable | Mean ± SD |
|---|---|
| Age (years) | 35.3 ± 0.5 |
| Wt (Kg) | 47.2 ± 0.6 |
| BSA (m2) | 1.4 ± 0.1 |
| EF% | 67.38 ± 2.9 |
| Aortic X-Clamp (min) | 73.3 ± 0.9 |
| PO2 Pre-CPB Off (mmHg) | 332.4 ± 2.1 |
| Total Bypass Time (min) | 108.1 ± 1.6 |
| Reperfusion Time/min | 12.8 ± 0.3 |
| CP, Temp (°C) | 31.4 ± 0.5 |
| Variable | Survivors | 30-Day Postoperative Mortality | p-Value |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Age (years) | 36.2 ± 0.5 | 18.2 ± 2.4 | <0.001 |
| Wt (Kg) | 48.3 ± 0.6 | 25.2 ± 0.6 | <0.001 |
| BSA (m2) | 1.6 ± 0.1 | 0.8 ± 0.1 | <0.001 |
| EF% | 67.5 ± 3.1 | 66.2 ± 3.1 | 0.924 |
| Aortic X-Clamp (min) | 71.5 ± 0.9 | 107.6 ± 7.1 | <0.001 |
| PO2 Pre-CPB Off (mmHg) | 332.4 ± 2.1 | 332.8 ± 10.3 | 0.965 |
| Total Bypass Time (min) | 103.9 ± 1.1 | 190.3 ± 16.6 | <0.001 |
| Reperfusion Time/min | 12.2 ± 0.2 | 26.3 ± 0.2 | <0.001 |
| CP, Temp (°C) | 31.5 ± 0.1 | 30.0 ± 0.3 | <0.001 |
| n (%) | n (%) | ||
| Sex | 0.01 | ||
| Male | 1331 (62) | 59 (3) | |
| Female | 728 (33) | 51 (2) | |
| Types CP Temp | <0.001 | ||
| Warm | 1304 (60.1) | 43 (1.9) | |
| Cold | 753 (34.9) | 66 (3) | |
| No | 3 (0.1) | 0 | |
| CP Solution | <0.001 | ||
| MICS | 1242 (57) | 30 (1) | |
| MYOtherm | 398 (19) | 35 (1.6) | |
| Custodiol | 61 (3) | 18 (0.8) | |
| del Nido | 304 (14) | 18 (0.8) | |
| No | 56 (256) | 7 (0.3) |
| Risk Factor Variable | Odds Ratio (95% CI) | p-Value |
|---|---|---|
| Age (years) | 1.0 (0.9–1.1) | 0.05 |
| Wt (Kg) | 1.0 (1.00–1.1) | 0.01 |
| BSA (m2) | 0.008 (0.001–0.057) | <0.001 |
| EF% | 0.98 (0.93–1.04) | 0.64 |
| Aortic X-Clamp (min) | 0.98 (0.97–0.99) | 0.01 |
| PO2 Pre-CPB Off (mmHg) | 1.03 (1.02 -1.101) | <0.001 |
| Total Bypass Time (min) | 1.001 (0.999–1.004) | 0.22 |
| Reperfusion Time/min | 0.99 (0.97–1.01) | 0.48 |
| CP, Temp (°C) | 0.88 (0.78–1.01) | 0.07 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al Sayani, A.; Munibari, A.; Bafadhl, T.; Andragiri, E.; Elghoneimy, Y.; Al-Hariri, M. Cardiovascular Surgery in Conflict Zones: Insights from 2169 Cases in Wartime Yemen. Emerg. Care Med. 2025, 2, 54. https://doi.org/10.3390/ecm2040054
Al Sayani A, Munibari A, Bafadhl T, Andragiri E, Elghoneimy Y, Al-Hariri M. Cardiovascular Surgery in Conflict Zones: Insights from 2169 Cases in Wartime Yemen. Emergency Care and Medicine. 2025; 2(4):54. https://doi.org/10.3390/ecm2040054
Chicago/Turabian StyleAl Sayani, Anwar, Abdlnasser Munibari, Tayeb Bafadhl, Eiman Andragiri, Yasser Elghoneimy, and Mohammed Al-Hariri. 2025. "Cardiovascular Surgery in Conflict Zones: Insights from 2169 Cases in Wartime Yemen" Emergency Care and Medicine 2, no. 4: 54. https://doi.org/10.3390/ecm2040054
APA StyleAl Sayani, A., Munibari, A., Bafadhl, T., Andragiri, E., Elghoneimy, Y., & Al-Hariri, M. (2025). Cardiovascular Surgery in Conflict Zones: Insights from 2169 Cases in Wartime Yemen. Emergency Care and Medicine, 2(4), 54. https://doi.org/10.3390/ecm2040054







