Abstract
Background: Safe inter-hospital transport of critically ill patients is a complex procedure where nurses are integral to maintaining patient safety. A structured checklist is pivotal to ensuring the transfer process mitigates potential complications. Objective: The objective of this scoping review was to devise and implement a detailed checklist to enhance patient safety during the transfer of critically ill patients. Methods: A comprehensive literature review was conducted by Joanna Briggs Institute’s guidelines across several databases including MEDLINE, CINAHL Complete, LILACS, and Scopus. The search considered works published in Portuguese, English, or Spanish from 2008 onwards. A total of eight studies met our inclusion criteria and were selected for detailed analysis. Results: Our analysis delineated the critical clinical information necessary to compose an effective transfer checklist. This checklist was developed through iterative refinement, informed by the literature and appraised during a focus group meeting with experts. Subsequent to its development, the checklist was implemented in the emergency department of a Central Portuguese hospital. Conclusions: This scoping review emphasizes the significance of evidence-based protocols and clear communication in safeguarding patient welfare during critical transfers. The developed checklist is a tool that standardizes care processes, supports clinical decision-making, and is instrumental in minimizing adverse events during inter-hospital transfers.
1. Introduction
The inter-hospital transfer of critically ill patients is a vital link in the chain of critical care, ensuring that patients receive timely and specialized treatment that is essential for improving clinical outcomes. Emergency departments (EDs) in Portugal are at the forefront of initiating such critical care. Nevertheless, the variable presence of medical and surgical specialties necessitates the movement of patients to tertiary centers equipped to provide comprehensive care [1,2].
The concept of critical patient transport encompasses the movement of patients across healthcare facilities that offer different levels of care, a process that requires a meticulous risk assessment tailored to the patient’s clinical status and the intrinsic complexities of transport [3]. The undertaking of such transfers is a substantial decision, primarily resting on the shoulders of ED physicians. It demands rigorous preparation, including an assessment of the patient’s clinical history and ongoing monitoring, to pre-empt and manage any complications that may arise during the journey [1,3].
Despite careful planning, the transfer of critically ill patients is fraught with an increased risk of complications, highlighting the importance of developing and implementing standardized protocols, such as checklists, to ensure the safety of both patients and healthcare personnel [1,3,4]. The adoption of checklists—recommended by entities such as the Intensive Care Society—provides a structured approach to managing the multifaceted aspects of patient transport and is seen as instrumental in mitigating adverse events [5,6].
An effective transport checklist is predicated on the synthesis of evidence-based guidelines, incorporating scientifically vetted practices that resonate with the existing operational protocols of healthcare institutions. Designed to be both logical and practical, such a tool not only guides clinical practices during transfers but also serves to reduce error frequency, thereby enhancing patient care, reinforcing staff confidence, and lessening the dependence on memory in critical situations [5,7].
Standardized documentation throughout the transport process is equally critical, capturing essential data that facilitate real-time decision-making and post-transfer evaluations for quality improvement [1,3,5]. Clear and comprehensive records, spanning the patient’s clinical state before, during, and after transport, form the backbone of this effort, enabling healthcare providers to perform effective audits and drive continuous care enhancement [8].
Upon reaching the destination hospital, the seamless continuity of care relies heavily on the effective exchange of information between the transport and receiving teams. This exchange should encompass a complete dossier of the patient’s clinical journey, ensuring that all vital information is communicated without omission [1,5].
Despite the established benefits of checklists and meticulous recordkeeping in the realm of patient transport, there exists an identified gap: a systematic overview of clinical data and parameters that should populate an IHT checklist [8,9]. Given the last guideline’s obsolescence in 2008 [3] and its recent update in 2023 [4], there is a pressing need for a version tailored to the current state of EDs in Portugal, considering their unique infrastructural and resource challenges. Thus, this scoping review is poised to address two vital inquiries: (1) What clinical data are imperative for inclusion in an IHT checklist? and (2) What parameters require monitoring and documentation throughout the patient transfer? By resolving these questions, this study aims to enhance the robustness of guidelines and practices, elevating the safety and quality of care during critical transport of patients.
2. Materials and Methods
2.1. Study Design
A scoping review was conducted to devise a checklist for the inter-hospital transport of critically ill patients, informed by the latest Joanna Briggs Institute (JBI) guidelines. This review employed a systematic and exploratory approach suitable for mapping out the breadth of evidence on the subject and followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) guidelines. The protocol was registered with the Open Science Framework (registry at https://osf.io/hbmu6, accessed on 30 March 2023) to ensure transparency and replicability of research methods [10]. Through iterative refinement, involving both author review and peer input via focus group discussions, the emergent checklist was honed and subsequently applied in an emergency department in Central Portugal.
2.2. Inclusion Criteria
The scoping review followed the Joanna Briggs Institute (J.B.I.) recommendations and incorporated the mnemonic “P.C.C.” for the establishment of inclusion criteria. The criteria encompassed the following aspects: Participants: The review considered studies involving critically ill patients as the target population; Concept: Studies specifically focusing on inter-hospital transport were included to address the research question effectively; Context: The review included studies that investigated checklists, guidelines, and tools relevant to inter-hospital transport, irrespective of the country of origin or study setting.
Types of Sources: A broad spectrum of study designs, comprising quantitative, qualitative, mixed methods, and systematic reviews, were considered for inclusion in the scoping review.
Additionally, the proposed scoping review also incorporated all types of systematic reviews, ensuring comprehensive coverage of the relevant literature.
2.3. Exclusion Criteria
The literature search was scoped to enhance relevance by excluding studies involving pediatric populations or those predating the most recent Portuguese guidelines (2008), to align with the evolution of clinical practice since the inception of these guidelines.
2.4. Search Strategy and Study Selection
A comprehensive literature search was executed across key databases: MEDLINE (via PubMed), CINAHL Complete (EBSCOhost), LILACS, and Scopus. The search harnessed both text words in titles and abstracts and index terms to encapsulate the articles’ essence, focusing on works published in Portuguese, English, or Spanish from 2008 onwards [3].
The search yielded 88 records, from which 21 duplicates were removed. Screening by titles and abstracts excluded a further 44 articles, leaving 23 for full-text review. Subsequent assessment narrowed the selection to 8 studies for final inclusion. Additionally, a grey literature search via Google supplemented the database findings with nine further articles. The search was structured in both Medical Subject Headings (MeSH) and text words shown in the literature, as presented in Table 1. The terms were combined using truncation symbols and Boolean operators (“OR” and “AND”). Lastly, the reference lists of the articles included in the review were screened for supplementary papers.

Table 1.
Search strategy for MEDLINE (via PubMed) on 3 May 2022.
Two independent reviewers (C.C. and J.S.) undertook the selection process, guided by stringent inclusion criteria. The entire selection process was systematically documented and is presented in a PRISMA flow diagram (Figure 1), illustrating the article selection stages from identification to final inclusion.
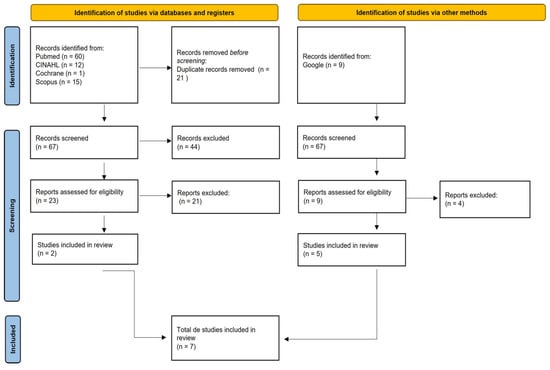
Figure 1.
PRISMA flowchart diagram of selected studies.
3. Results
3.1. Checklist Development
Drawing on the scoping review’s insights, we devised a comprehensive checklist to streamline the documentation required during the inter-hospital transport of critically ill patients. This checklist, structured around the ABCDE assessment framework from the National Institute of Medical Emergency’s (INEM) Advanced Life Support Manual, ensures a systematic approach to patient evaluation and care [11], in the following categories:
- Identification
This segment captures essential patient identifiers and contact details, facilitating accurate identification and communication throughout the transport process.
- Patient Assessment
This encompasses a thorough clinical assessment, recording vital signs and pertinent patient history at regular intervals to monitor and manage the patient’s condition effectively during transport.
This includes additional diagnostic and medical history information crucial for comprehensive patient care during the journey.
- Verification of Resources before Transportation
This focuses on confirming the availability and functionality of all necessary equipment and staffing resources before starting the transport, ensuring a prepared and responsive medical team.
Organized into these specific categories, the checklist serves as an essential tool for healthcare professionals, enabling meticulous patient care and documentation, as presented on Table 2.

Table 2.
Data to be included in the inter-hospital transport checklist.
3.2. Focus Group Feedback
To refine the checklist and ensure its relevance and applicability, a focus group comprising specialist nurses from the target ED in Central Portugal was convened. Selection criteria for the nurses included specialization in Medical–Surgical Nursing and current employment in the ED. Six out of seventy eligible nurses participated in this session, held via Zoom on 14 December 2022.
The focus group discussions, lasting ninety-four minutes, were instrumental in validating and enhancing the checklist’s content. The specialist nurses provided critical feedback based on their professional experience, ensuring the checklist’s practicality and effectiveness in real-world scenarios.
This collaborative effort not only aligned the checklist with evidence-based practices but also ensured it was tailored to the specific needs and conditions of the ED environment. The integration of frontline nursing insights underscores the checklist’s capacity to significantly elevate patient safety and care quality during inter-hospital transfers. The final checklist is available in Supplementary Materials.
4. Discussion
The scoping review, which scrutinized seven pivotal studies, revealed a significant concentration of research originating from the United Kingdom (n = 3), with additional contributions from Australia, New Zealand, the United States, India, and Portugal. The linguistic trend strongly favored English, with only a singular study presented in Portuguese, highlighting a potential linguistic bias in the dissemination of scientific knowledge.
All identified studies were systematic literature reviews, five of which specifically provided guidelines on the inter-hospital transport of critically ill patients, spanning publications from 2008 to 2021. This body of work collectively emphasizes the indispensable need for meticulous planning and comprehensive patient assessment prior to the commencement of inter-hospital transport [5]. The implementation of a standardized document that is to accompany the patient was highlighted, facilitating a detailed account of the patient’s clinical status at various stages of the transfer. Such documentation aids in the auditing process and fosters improvements in patient care during these critical transitions [5,6,8,11].
Moreover, the guidelines advocate for the clear documentation of all interventions and any complications arising during transport [1,8]. This documentation should meticulously record the patient’s condition, transfer rationale, and the identities of both the sending and receiving physicians, alongside vital signs and administered treatments [1,3,6,8,12]. Ensuring this information is conveyed both verbally and in writing upon arrival at the receiving facility is crucial for maintaining continuity of care [1,6].
An analysis from the reviewed literature also informed the checklist’s design, adopting the ABCDE approach for a holistic and standardized patient assessment, pivotal for identifying and managing emergent life-threatening conditions efficiently [13].
The review brought to light the prevalence of both medical and technical adverse events during inter-hospital transfers, which necessitate meticulous recording within the transport checklist [12]. Cardiovascular and respiratory complications were among the most frequently encountered medical issues, while equipment failures stood out as the predominant technical challenge, underscoring the necessity for rigorous equipment checks [1,8,12].
This comprehensive review underpins the checklist’s development, merging evidence-based guidelines with best practices to enhance the safety and efficiency of inter-hospital patient transport.
Ensuring the checklist’s applicability and relevance, a focus group comprising specialist nurses in Medical–Surgical Nursing from the target ED was convened. Their involvement was instrumental in validating the checklist’s content, drawing on their direct experience in critical patient transport. The nurses’ feedback during this session, which facilitated deep discussions on the checklist’s components, was vital for its refinement, ensuring it met the day-to-day operational demands of the ED and enhanced its practicality.
The active participation of these specialist nurses not only bolstered the checklist’s credibility among healthcare professionals but also contributed to a collective commitment to patient safety during transport. Their insights have significantly influenced the checklist’s design, making it user-friendly and reflective of the real-world challenges of inter-hospital transport.
Moreover, the collaborative development process highlighted the importance of a multidisciplinary approach in enhancing patient care and safety during transport, indicating the value of incorporating frontline nursing perspectives into healthcare tools and protocols.
The iterative review and validation process, enriched by expert feedback, ensured the checklist was comprehensive, coherent, and finely tuned to the unique needs of the ED, representing a significant stride toward improving patient outcomes and the quality of care during critical inter-hospital transfers.
5. Conclusions
This study has led to the creation of a meticulously designed checklist aimed at streamlining the inter-hospital transfer process for critically ill patients, emphasizing the secure and accurate conveyance of vital patient information to facilitate uninterrupted care upon arrival at the receiving facility. The genesis of the checklist was motivated by the critical need to bolster both safety and efficiency during these transfers, ensuring comprehensive documentation of patient data, verification of essential resources prior to transport, and meticulous recording of any emergent complications.
The adoption of this checklist within EDs stands to significantly bolster patient and nurse safety, mitigate adverse events, and thereby elevate the overall standard of care. It introduces a uniform protocol for inter-hospital transfers, guaranteeing the thorough documentation and effective communication of crucial patient information to the receiving care team.
A notable strength of the checklist is its potential to significantly improve patient safety. The ED staff, equipped with this tool, can more reliably manage patient care, minimizing the risk of errors. The structured capture of patient details and vital signs facilitates quick response to any critical changes during transport, allowing for timely medical interventions.
Furthermore, the checklist exemplifies the core tenets of patient-centered and evidence-based healthcare practices. Its structured format ensures the comprehensive capture of key clinical information, enhancing decision-making, streamlining communication, and ensuring a smooth transition of care. The capability to document transport-related complications and interventions offers a basis for ongoing monitoring and quality assessment, pinpointing opportunities for systemic improvements.
The introduction of this checklist promises to equip the ED more effectively to navigate the complexities of inter-hospital transfers, guaranteeing that critically ill patients are afforded consistent, high-caliber care throughout their transit between medical facilities. It is poised to cultivate a culture of safety and continual enhancement in patient care practices within the ED, championing a collaborative, patient-first healthcare paradigm.
In summation, the checklist developed through this study represents a significant advancement in the safety, efficacy, and quality of care for critically ill patients undergoing inter-hospital transport. By leveraging evidence-based practices and tapping into the insights of specialist nursing staff, this initiative stands as a meaningful contribution toward improving patient outcomes and enriching the healthcare experience for patients and their families in critical care contexts.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ecm1030023/s1, Table S1: Checklist for the follow-up of critical patients during inter-hospital transport.
Author Contributions
Conceptualization, C.C.; methodology, C.C. and J.P.S.; validation, C.C. and J.P.S.; formal analysis, C.C.; writing—original draft preparation, C.C.; writing—review and editing, C.C., C.R.B.C. and J.P.S.; supervision, J.P.S.; project administration, C.C., C.R.B.C. and J.P.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The original contributions presented in this study are included in this article/Supplementary Materials; further inquiries can be directed to the corresponding authors.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Intensive Care Society; Faculty of Intensive Care Medicine. Guidance On: The transfer of the Critically ill Adult. Intensive Care Soc. 2019, 1–20. Available online: https://www.ficm.ac.uk/sites/ficm/files/documents/2021-10/Transfer_of_Critically_Ill_Adult.pdf (accessed on 2 December 2022).
- National Health Service. Framework to Support Inter-Hospital Transfer of Critical Care Patients. 2021. Available online: https://www.england.nhs.uk/wp-content/uploads/2021/12/B1215-framework-to-support-inter-hospital-transfer-of-critical-care-patients.pdf (accessed on 2 December 2022).
- Ordem dos Médicos; Sociedade Portuguesa de Cuidados Intensivos. Transporte de Doentes Críticos—Recomendações. Sociedade Portuguesa de Cuidados Intensivos. 2008. Available online: https://www.spci.pt/media/documentos/15827260365e567b9411425.pdf (accessed on 2 December 2022).
- The Association of Anaesthetists of Great Britain and Ireland. AABGI Safety Guideline: Interhospital Transfer. Association of Anaesthetists. 2009, pp. 1–20. Available online: https://www.wyccn.org/uploads/6/5/1/9/65199375/interhospital09.pdf (accessed on 2 December 2022).
- Ordem dos Médicos; Sociedade Portuguesa de Cuidados Intensivos. Transporte de Doentes Críticos Adultos—Recomendações. Sociedade Portuguesa de Cuidados Intensivos. 2023. Available online: https://www.spci.pt/media/noticias/transporte-doente-critico-2023-versao-CEMI_OM_3.pdf (accessed on 2 December 2022).
- Comeau, Y.; Armendariz-Batiste, J.; Woodby, A. Safety first! Using a checklist for intrafacility transport of adult intensive care patients. Crit. Care Nurse 2015, 35, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Australasian College for Emergency Medicine; Australian and New Zealand College of Anaesthetists; College of Intensive Care Medicine of Australian and New Zealand. Guidelines for transport of critically ill patients. Aust. N. Z. Coll. Anaesth. Fac. Pain Med. 2015, 1–12. Available online: https://www.anzca.edu.au/getattachment/bd5938d2-d3ab-4546-a6b0-014b11b99b2f/PS52-Guideline-for-transport-of-critically-ill-patients (accessed on 2 December 2022).
- Kulshrestha, A.; Singh, J. Inter-hospital and intra-hospital patient transfer—Recent concepts. Indian J. Anaesth. 2016, 60, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Hales, B.; Terblanche, M.; Fowler, R.; Sibbald, W. Development of medical checklists for improved quality of patient care. Int. J. Qual. Health Care 2008, 20, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, C.; Pereira Sousa, J. Nursing Care at Critical Care Patient Inter-Hospital Transfer: A Scoping Review Protocol. Millenium 2022, 2, 71–76. [Google Scholar] [CrossRef]
- Whiteley, S.; Macartney, I.; Mark, J.; Barratt, H.; Binks, R. Guideline for the Transport of the Critically Ill Adult, 3rd ed.; Intensive Care Society: London, UK, 2011. [Google Scholar]
- Rali, P.; Sacher, D.; Rivera-Lebron, B.; Rosovsky, R.; Elwing, J.M.; Berkowitz, J.; Mina, B.; Dalal, B.; Davis, G.A.; Dudzinski, D.M.; et al. Interhospital Transfer of Patients with Acute Pulmonary Embolism. Chest 2021, 160, 1844–1852. [Google Scholar] [CrossRef] [PubMed]
- Instituto Nacional de Emergência Médica; Departamento de Formação em Emergência Médica. Manual de Suporte Avançado de Vida. Instituto Nacional de Emergência Médica. 2020. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).