Serum Urate as a Surrogate Outcome for Gout Flares: Where Do We Stand Today?
Abstract
:1. Introduction
2. Definitions
- Is there a strong, independent, consistent association between the biomarker (potential surrogate) and the clinical patient-important outcome (that the surrogate could potentially replace)?
- Is there evidence from randomized trials in the same drug class that improvement in the surrogate outcome has consistently led to improvement in the target outcome?
- Is there evidence from randomized trials in other drug classes that improvement in the surrogate outcome has consistently led to improvement in the target outcome?
3. Serum Urate as a Biomarker
4. The Gout Flare as an Important Patient-Centered Outcome in Gout
5. Unique Challenges in Showing Serum Urate Is a Surrogate Outcome for Gout Flares
5.1. SU Reporting
5.2. Gout Flare Reporting
5.3. Relationship between Change in Serum Urate, Gout Flares and Trial Design
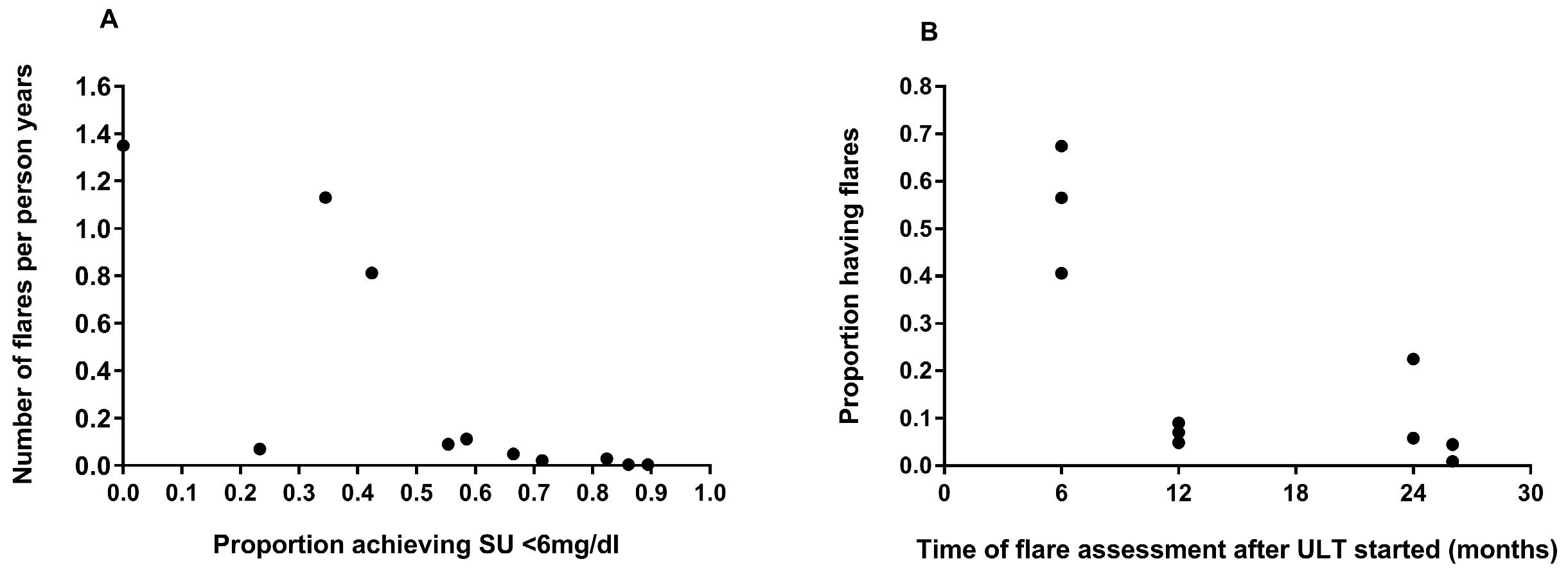
6. What Is the Current Evidence That SU Is a Valid Surrogate for Gout Flares?
7. Where Do We Stand Today?
8. What More Do We Need
Funding
Conflicts of Interest
References
- Doherty, M.; Jenkins, W.; Richardson, H.; Sarmanova, A.; Abhishek, A.; Ashton, D.; Barclay, C.; Doherty, S.; Duley, L.; Hatton, R.; et al. Efficacy and cost-effectiveness of nurse-led care involving education and engagement of patients and a treat-to-target urate-lowering strategy versus usual care for gout: A randomised controlled trial. Lancet 2018, 392, 1403–1412. [Google Scholar] [CrossRef] [PubMed]
- Stamp, L.K.; Chapman, P.T.; Barclay, M.L.; Horne, A.; Frampton, C.; Tan, P.; Drake, J.; Dalbeth, N. A randomised controlled trial of the efficacy and safety of allopurinol dose escalation to achieve target serum urate in people with gout. Ann. Rheum. Dis. 2017, 76, 1522–1528. [Google Scholar] [CrossRef] [PubMed]
- Ciani, O.; Manyara, A.M.; Chan, A.-W.; Taylor, R.S. Surrogate endpoints in trials: A call for better reporting. Trials 2022, 23, 991. [Google Scholar] [CrossRef]
- FitzGerald, J.D.; Dalbeth, N.; Mikuls, T.; Brignardello-Petersen, R.; Guyatt, G.; Abeles, A.M.; Gelber, A.C.; Harrold, L.R.; Khanna, D.; King, C.; et al. 2020 American College of Rheumatology Guideline for the Management of Gout. Arthritis Care Res. 2020, 72, 744–760. [Google Scholar] [CrossRef] [PubMed]
- Richette, P.; Doherty, M.; Pascual, E.; Barskova, V.; Becce, F.; Castañeda-Sanabria, J.; Coyfish, M.; Guillo, S.; Jansen, T.L.; Janssens, H.; et al. 2016 updated EULAR evidence-based recommendations for the management of gout. Ann. Rheum. Dis. 2017, 76, 29–42. [Google Scholar] [CrossRef]
- Stamp, L.; Morillon, M.B.; Taylor, W.J.; Dalbeth, N.; Singh, J.A.; Lassere, M.; Christensen, R. Serum urate as surrogate endpoint for flares in people with gout: A systematic review and meta-regression analysis. Semin. Arthritis Rheum. 2018, 48, 293–301. [Google Scholar] [CrossRef] [PubMed]
- Biomarkers In Risk Assessment: Validity and Validation. Available online: http://www.inchem.org/documents/ehc/ehc/ehc222.htm (accessed on 31 July 2023).
- Maksymowych, W.P.; Fitzgerald, O.; Wells, G.A.; Gladman, D.D.; Landewé, R.; Østergaard, M.; Taylor, W.J.; Christensen, R.; Tak, P.-P.; Boers, M.; et al. Proposal for Levels of Evidence Schema for Validation of a Soluble Biomarker Reflecting Damage Endpoints in Rheumatoid Arthritis, Psoriatic Arthritis, and Ankylosing Spondylitis, and Recommendations for Study Design. J. Rheumatol. 2009, 36, 1792–1799. [Google Scholar] [CrossRef]
- Maksymowych, W.P.; Landewé, R.; Tak, P.-P.; Ritchlin, C.J.; Østergaard, M.; Mease, P.J.; El-Gabalawy, H.; Garnero, P.; Gladman, D.D.; Fitzgerald, O.; et al. Reappraisal of OMERACT 8 Draft Validation Criteria for a Soluble Biomarker Reflecting Structural Damage Endpoints in Rheumatoid Arthritis, Psoriatic Arthritis, and Spondyloarthritis: The OMERACT 9 v2 Criteria. J. Rheumatol. 2009, 36, 1785–1791. [Google Scholar] [CrossRef]
- Stamp, L.K.; Zhu, X.; Dalbeth, N.; Jordan, S.; Edwards, N.L.; Taylor, W. Serum Urate as a Soluble Biomarker in Chronic Gout—Evidence that Serum Urate Fulfills the OMERACT Validation Criteria for Soluble Biomarkers. Semin. Arthritis Rheum. 2011, 40, 483–500. [Google Scholar] [CrossRef]
- Taylor, W.J.; Schumacher, H.R.; Baraf, H.S.B.; Chapman, P.; Stamp, L.; Doherty, M.; McQueen, F.; Dalbeth, N.; Schlesinger, N.; E Furst, D.; et al. A modified Delphi exercise to determine the extent of consensus with OMERACT outcome domains for studies of acute and chronic gout. Ann. Rheum. Dis. 2008, 67, 888–891. [Google Scholar] [CrossRef]
- Temple, R. Clinical Measurement in Drug Evaluation. In A Regulatory Authority’s Opinion about Surrogate Endpoints; Nimmo, W., Tucker, G., Eds.; John Wiley & Sons Ltd.: Hoboken, NJ, USA, 1995; pp. 3–22. [Google Scholar]
- Bucher, H.C.; Guyatt, G.H.; Cook, D.J.; Holbrook, A.; McAlister, F.A. Users’ Guides to the Medical Literature: XIX. Applying Clinical Trial Results A. How to Use an Article Measuring the Effect of an Intervention on Surrogate End Points. JAMA 1999, 282, 771–778. [Google Scholar] [CrossRef] [PubMed]
- Lassere, M.N.; Johnson, K.R.; Boers, M.; Tugwell, P.; Brooks, P.; Simon, L.; Strand, V.; Conaghan, P.G.; Ostergaard, M.; Maksymowych, W.P.; et al. Definitions and validation criteria for biomarkers and surrogate endpoints: Development and testing of a quantitative hierarchical levels of evidence schema. J. Rheumatol. 2007, 34, 607–615. [Google Scholar]
- Lassere, M.N.; Johnson, K.R.; Schiff, M.; Rees, D. Is blood pressure reduction a valid surrogate endpoint for stroke prevention? An analysis incorporating a systematic review of randomised controlled trials, a by-trial weighted errors-in-variables regression, the surrogate threshold effect (STE) and the biomarker-surrogacy (BioSurrogate) evaluation schema (BSES). BMC Med Res. Methodol. 2012, 12, 1–21. [Google Scholar] [CrossRef]
- Dalbeth, N.; Merriman, T.; Stamp, L. Gout. Lancet 2016, 388, 2039–2052. [Google Scholar] [CrossRef] [PubMed]
- Tatlock, S.; Rüdell, K.; Panter, C.; Arbuckle, R.; Harrold, L.R.; Taylor, W.J.; Symonds, T. What Outcomes are Important for Gout Patients? In-Depth Qualitative Research into the Gout Patient Experience to Determine Optimal Endpoints for Evaluating Therapeutic Interventions. Patient-Patient-Centered Outcomes Res. 2017, 10, 65–79. [Google Scholar] [CrossRef] [PubMed]
- Stewart, S.; Guillen, A.G.; Taylor, W.J.; Gaffo, A.; Slark, J.; Gott, M.; Dalbeth, N. The experience of a gout flare: A meta-synthesis of qualitative studies. Semin. Arthritis Rheum. 2020, 50, 805–811. [Google Scholar] [CrossRef]
- Schumacher, H.R.; Taylor, W.; Edwards, L.; Grainger, R.; Schlesinger, N.; Dalbeth, N.; Sivera, F.; Singh, J.; Evans, R.; Waltrip, R.W.; et al. Outcome Domains for Studies of Acute and Chronic Gout. J. Rheumatol. 2009, 36, 2342–2345. [Google Scholar] [CrossRef]
- Stamp, L.K.; Morillon, M.B.; Taylor, W.J.; Dalbeth, N.; Singh, J.A.; Lassere, M.; Christensen, R. Variability in the reporting of serum urate and flares in gout clinical trials: Need for minimal reporting requirements. J. Rheumatol. 2018, 45, 419–424. [Google Scholar] [CrossRef]
- Morillon, M.B.; Nørup, A.; Singh, J.A.; Dalbeth, N.; Taylor, W.J.; Kennedy, M.A.; Pedersen, B.M.; Grainger, R.; Tugwell, P.; Perez-Ruiz, F.; et al. Outcome reporting in randomized trials in gout: A systematic scoping review from the OMERACT gout working group assessing the uptake of the core outcome set. Semin. Arthritis Rheum. 2023, 60, 152191. [Google Scholar] [CrossRef]
- Stewart, S.; Tallon, A.; Taylor, W.J.; Gaffo, A.; Dalbeth, N. How flare prevention outcomes are reported in gout studies: A systematic review and content analysis of randomized controlled trials. Semin. Arthritis Rheum. 2020, 50, 303–313. [Google Scholar] [CrossRef]
- Gaffo, A.L.; Dalbeth, N.; Saag, K.G.; Singh, J.A.; Rahn, E.J.; Mudano, A.S.; Chen, Y.; Lin, C.; Bourke, S.; Louthrenoo, W.; et al. Brief Report: Validation of a Definition of Flare in Patients with Established Gout. Arthritis Rheumatol. 2018, 70, 462–467. [Google Scholar] [CrossRef]
- Gaffo, A.L.; Schumacher, H.R.; Saag, K.G.; Taylor, W.J.; Dinnella, J.; Outman, R.; Chen, L.; Dalbeth, N.; Sivera, F.; Vázquez-Mellado, J.; et al. Developing a provisional definition of flare in patients with established gout. Arthritis Rheum. 2012, 64, 1508–1517. [Google Scholar] [CrossRef]
- Stamp, L.; Frampton, C.; Morillon, M.; Taylor, W.J.; Dalbeth, N.; Singh, J.A.; Doherty, M.; Zhang, W.; Richardson, H.; Sarmanova, A.; et al. Association between serum urate and flares in people with gout and evidence for surrogate status: A secondary analysis of two randomised controlled trials. Lancet Rheumatol. 2022, 4, e53–e60. [Google Scholar] [CrossRef]
- Manyara, A.M.; Davies, P.; Stewart, D.; Weir, C.J.; Young, A.; Butcher, N.J.; Bujkiewicz, S.; Chan, A.-W.; Collins, G.S.; Dawoud, D.; et al. Protocol for the development of SPIRIT and CONSORT extensions for randomised controlled trials with surrogate primary endpoints: SPIRIT-SURROGATE and CONSORT-SURROGATE. BMJ Open 2022, 12, e064304. [Google Scholar] [CrossRef]

| Essential Criteria | |
|---|---|
| Truth and Discrimination |
|
| Feasibility |
|
| Biomarker-Surrogate Domains | Score | Explanation |
|---|---|---|
| Study design | 0 | Biological plausibility and lower quality clinical studies, e.g., cross-sectional observational studies |
| 1 | Rank 0 and at least 2 good quality prospective observational cohort studies measuring S and T | |
| 2 | Rank 1 and at least 2 high quality adequately powered RCTs measuring S and T | |
| 3 | Rank 1 and all, and at least 5 high quality adequately powered, RCTs measuring S and T | |
| Target outcome | 0 | Target is reversible disease-centered biomarker of harm |
| 1 | Target is irreversible disease-centered biomarker of harm | |
| 2 | Target is patient-centered endpoint of reversible organ morbidity or clinical burden of disease or clinical harm | |
| 3 | Target is patient-centered endpoint of irreversible organ morbidity or clinical burden of disease or severe irreversible clinical harm or death | |
| Statistical Evaluation of biosurrogate—Target (B-T) domain | 0 | Poor: Does not meet the criteria for Rank 1 |
| 1 | Fair: RCT R2trial ≥ 0.2 AND STEP ≥ 0.1 AND R2ind ≥ 0.2 OR cohort data R2ind ≥ 0.4 | |
| 2 | Good: RCT R2trial ≥ 0.4 AND STEP ≥ 0.2 AND R2ind ≥ 0.4 | |
| 3 | Excellent: RCT R2trial ≥ 0.6 AND STEP ≥ 0.3 AND R2ind is ≥0.6 (without data subdivision) | |
| Generalizability | 0 | No clinical or pharmacologic evidence |
| 1 | Clinical OR pharmacologic evidence | |
| 2 | Clinical AND pharmacologic evidence | |
| 3 | Consistent Clinical RCT AND pharmacologic RCT evidence |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stamp, L.K.; Christensen, R.; Morillon, M.B. Serum Urate as a Surrogate Outcome for Gout Flares: Where Do We Stand Today? Gout Urate Cryst. Depos. Dis. 2024, 2, 70-76. https://doi.org/10.3390/gucdd2010007
Stamp LK, Christensen R, Morillon MB. Serum Urate as a Surrogate Outcome for Gout Flares: Where Do We Stand Today? Gout, Urate, and Crystal Deposition Disease. 2024; 2(1):70-76. https://doi.org/10.3390/gucdd2010007
Chicago/Turabian StyleStamp, Lisa K., Robin Christensen, and Melanie B. Morillon. 2024. "Serum Urate as a Surrogate Outcome for Gout Flares: Where Do We Stand Today?" Gout, Urate, and Crystal Deposition Disease 2, no. 1: 70-76. https://doi.org/10.3390/gucdd2010007





