Abstract
Introduction: Chronic neck pain is a prevalent condition that challenges physical therapists (PTs) due to its multifactorial etiology. Differential diagnosis is crucial for identifying the underlying causes and providing appropriate interventions. However, the extent to which PTs apply and understand differential diagnostic criteria remains unclear. This study aimed to evaluate the knowledge, attitudes, and behaviors of PTs in France regarding the differential diagnosis of chronic neck pain. Materials and Methods: An online questionnaire was designed to assess PTs’ beliefs, attitudes, knowledge, and clinical application of differential diagnostic criteria in chronic neck pain. The survey was distributed nationwide and included questions regarding demographic data, theoretical knowledge, practical application, and perceived barriers. A total of 80 responses were collected and analyzed using descriptive and inferential statistics. Results: The results revealed moderate levels of theoretical knowledge among participants, with 62% correctly identifying key criteria for differential diagnosis. However, only 45% reported consistently applying these criteria in clinical practice. Common barriers included time constraints (70%), lack of access to advanced diagnostic tools (55%), and insufficient training (40%). Attitudes towards the importance of differential diagnosis were predominantly positive, with 85% recognizing its relevance for improving patient outcomes. Conclusions: This study highlights a gap between PTs’ knowledge and the practical application of differential diagnosis criteria in chronic neck pain. Addressing barriers such as training and resource availability could enhance clinical practices. Future efforts should focus on integrating these competencies into professional development programs to improve diagnostic accuracy and patient care.
1. Introduction
Chronic neck pain (CNP) is one of the most common and disabling musculoskeletal conditions affecting individuals worldwide [1]. It is a complex condition that can significantly impair a person’s quality of life, leading to difficulties with daily activities, work, and social participation [2]. With an estimated lifetime prevalence ranging from 30% to 50%, chronic neck pain is a widespread issue that places considerable burdens on healthcare systems [3], including the profession of physical therapy (PT). Given the chronic nature of the condition and the multifactorial issues that contribute to its onset and persistence, physical therapists are frequently called upon to assess and treat individuals suffering from this affliction [4]. However, the complexity of CNP—due to its diverse etiologies—presents a significant challenge in clinical practice, especially in terms of differential diagnosis and management [5].
The cervical spine is a highly dynamic and intricate anatomical structure composed of the bones, muscles, ligaments, nerves, and surrounding tissues [6]. Consequently, CNP can arise from a broad range of sources, including musculoskeletal, neurological, and psychosocial factors. Common causes of CNP include cervical spine pathologies such as degenerative disc disease, herniated discs, facet joint dysfunction, and myofascial pain [7]. However, the involvement of neurological factors such as radiculopathy or cervical myelopathy, as well as referred pain from the thoracic spine, shoulder, or even the temporomandibular joint, can complicate diagnosis and treatment [8].
Given the vast array of potential contributing factors, an accurate and timely differential diagnosis is critical for physical therapists to identify the root causes of chronic neck pain and determine the appropriate course of treatment. For physical therapists, differential diagnosis is a vital skill, as it not only informs treatment decisions but also helps to identify cases that may require referral to other healthcare professionals [9].
However, research [10] into the diagnostic practices of PTs has revealed that while they are skilled at assessing musculoskeletal conditions, their ability to recognize and differentiate between the wide range of potential causes of neck pain, including neurological and systemic disorders, remains unclear. This raises concerns about whether physical therapists possess sufficient knowledge and awareness of the full spectrum of conditions contributing to chronic neck pain and whether they consistently apply differential diagnostic criteria in their clinical decision-making processes.
In this context, diagnostic imaging techniques, such as magnetic resonance imaging (MRI) and computed tomography (CT) [11,12], have become increasingly relevant in identifying structural and neurological alterations associated with chronic neck pain, particularly when used under medical referral. Additionally, artificial intelligence-based tools are emerging as promising aids in the diagnostic process [13], enhancing accuracy and efficiency in assessing musculoskeletal and neurological conditions. As these technological advancements continue to evolve, their integration into clinical practice may play a crucial role in improving the diagnostic capabilities of physical therapists.
Given the growing body of research [14,15] emphasizing the importance of early diagnosis and intervention in the management of chronic pain, it is essential to explore how physical therapists perceive their role in the diagnostic process. While technological advancements provide valuable support, the behaviors and decision-making processes of physical therapists remain central to effective diagnosis and treatment. This study will examine the use of standardized clinical guidelines, screening tools, and decision-making frameworks to determine the extent to which evidence-based practices inform their diagnostic processes. By identifying the behaviors that characterize the diagnostic process, this study will provide insight into how physical therapists apply their clinical knowledge and skills in practice, highlighting any gaps or areas where further education may be needed.
2. Materials and Methods
A cross-sectional study was carried out to examine the beliefs, attitudes, knowledge, and behaviors of physical therapists towards differential diagnosis in chronic neck pain etiology in France. The study was performed according to the ethical principles of the Declaration of Helsinki. It was carried out between July and December 2024.
2.1. Participants
The study design consisted of an online questionnaire for physiotherapy professionals (≥18 years) with clinical experience in treating patients with chronic neck pain. Additionally, undergraduate physical therapy students, trainees, and individuals without experience in this field were excluded from participating.
2.2. The Questionnaire
The questionnaire was designed according to the CHERRIES guidelines (Checklist for Reporting Results of Internet E-Surveys) [16]. The survey was open and anonymous. All subjects participated voluntarily. Participants gave their consent before the start of the questionnaire, after reading the informed consent statement. The survey was conducted in compliance with France’s personal data protection law, which adapts the GDPR legal framework and guarantees the anonymity and confidentiality of the participants.
The questionnaire is made up of 33 questions, organized into five different sections: (1) demographic data (age, gender, location of their professional practice, etc.); (2) profile of the training of the professionals; (3) their knowledge of differential diagnosis; (4) their clinical practice and experience as physical therapists in the application of differential diagnosis of chronic neck pain; (5) the perceptions and opinions of physical therapists regarding differential diagnoses.
It was developed for this specific study and was constructed after a detailed review of the literature concerning the physiotherapeutic management of patients with chronic neck pain [17,18,19].
A pilot test of the questionnaire was conducted prior to the main study. Physiotherapy students took a pretest of the questionnaire, which was timed. Once the survey time had elapsed, the students were asked to raise doubts and make appropriate observations. This made it possible to verify that the questions were interpreted in the same way by all of the participants. The questionnaire was then modified, and some questions were reformulated.
The distribution of the questionnaire was carried out through several channels, such as the National Council of the Order of Physiotherapists (CNOMK, Paris, France), the Institute of Manual Therapy and Physiotherapy (ITMP, Paris, France), the Physiotherapy Training Institute (IFMK, Paris, France), and social media (Facebook® and Instagram®, Menlo Park, CA, USA), to maximize participation from private practice physiotherapists in France.
2.3. Statical Analysis
Data collection was carried out using Google Forms. All responses to the questionnaire were collected directly through this application. Subsequently, the data were exported to Microsoft Excel to analyze the data more efficiently.
Data were transferred and analyzed with SPSS Version 23.0 statistical software (SPSS Inc., Chicago, IL, USA). Summary descriptive statistics (mean values with 95% confidence intervals) were calculated for the socio-demographic data of the respondents. A descriptive analysis of the study variables was performed using absolute and relative frequencies (%). For categorical variables, frequencies and proportions were calculated to describe the distribution of the main characteristics of the study population. The results are presented in tables. The Chi-squared test of independence was applied to assess associations between categorical variables.
3. Results
In total, 80 surveys were completed by physiotherapists. The demographic data and the specialization profile of the professionals are presented in Table 1.

Table 1.
Sociodemographic and training profile of participants.
A total of 55% of respondents were men. The participants’ ages were distributed as follows: 15% were under 25 years old, 56.3% were between 25 and 40 years old, 23.8% were between 40 and 60 years old, and 5% were over 60 years old. The mean work experience was 10.9 ± 8.7 years.
A total of 65% of physiotherapists reported having completed postgraduate studies. Specific training on neck pain was completed by 16.3% of respondents in the last year and by 35% in the past five years. Specific training on differential diagnostic techniques was completed by 17.7% in the last year and by 35.4% in the past five years. Most respondents engaged in self-training, with 43.8% doing so occasionally and 42.5% regularly.
Table 2 shows the clinical practice and experience as physical therapists in the application of differential diagnosis of chronic neck pain.

Table 2.
Clinical practice and experience as physical therapists in the application of differential diagnosis of chronic neck pain.
Among physiotherapists, 43.8% reported that 11–20% of their patients were diagnosed with chronic neck pain (CNP), 28.8% reported 0–10%, 20% reported 21–30%, 6.3% reported 31–40%, and 1.3% reported more than 50% of their patients being diagnosed with CNP. Regarding familiarity with CNP red flags, 61.3% were moderately familiar, and the frequency of identifying red flags in clinical practice was most commonly once a month (53.8%).
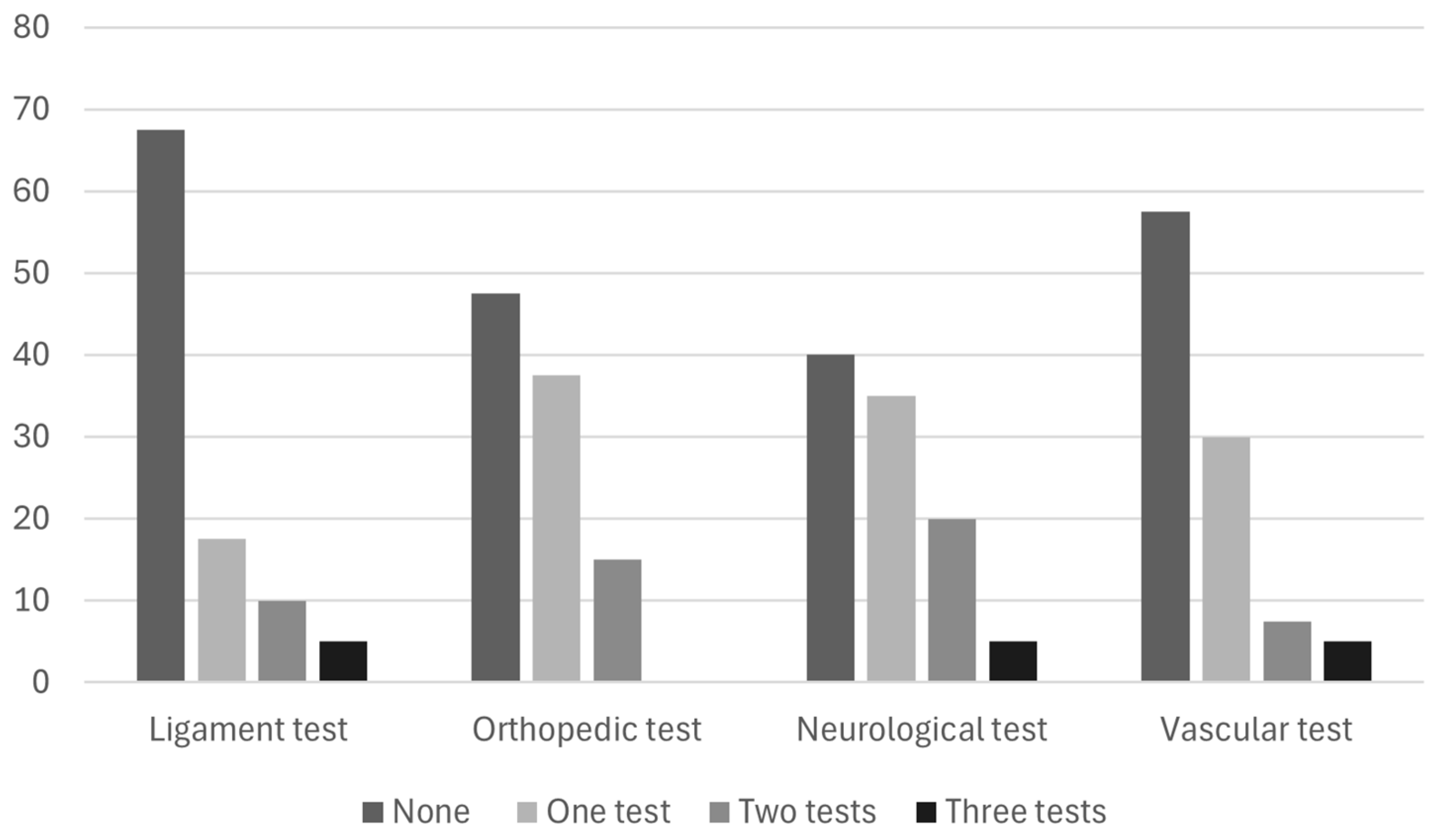
To evaluate the specific exclusion criteria of red flags, 37.5% used one or two types of assessments, and 25% used three types of assessments. Concerning specific tests, 67.5% did not use ligament tests, 47.5% did not use orthopedic tests, 40% did not use neurological tests, and 57.7% did not use vascular tests (Figure 1).
Figure 1.
Use of specific exclusion tests for red flags (%).
A total of 50% of physiotherapy professionals were familiar with the factors contributing to CNP; 67.5% identified these factors more than three times per month. However, only 6.5% used specific tests to assess CNP factors.
The majority of physiotherapist professionals were confident (56.3%) in the use of differential diagnosis of CNP and always (30%) performed specific tests for the differential diagnosis of CNP.
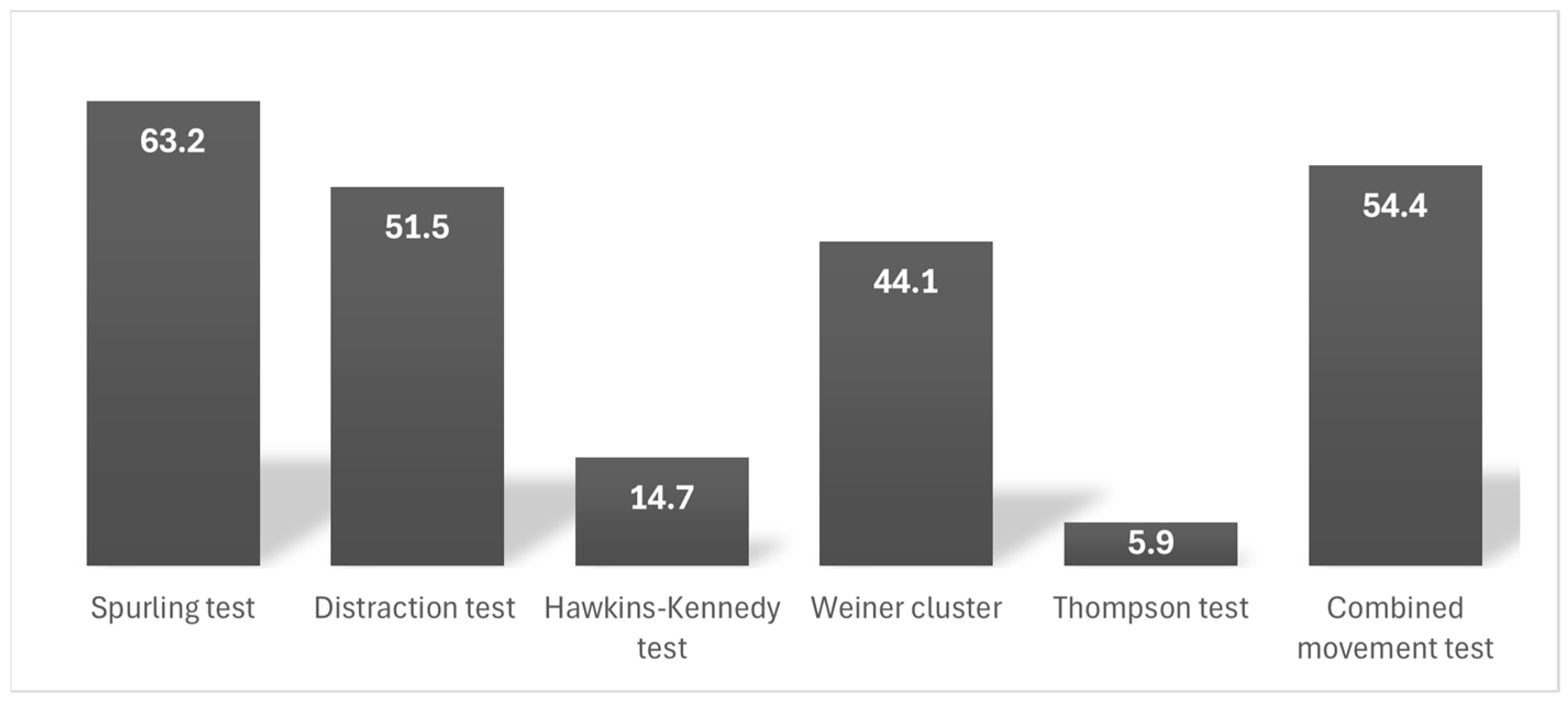
Among physiotherapists, 29.4% used one test specific for CNP, with the most commonly used tests being the Spurling test (63.2%), the combined movement test (54.4%), the distraction test (51.5%), the Weiner cluster (44.1%), the Hawkins–Kennedy test (14.7%), and the Thompson test (5.9%) (Figure 2).

Figure 2.
Specific chronic neck pain tests used (%).
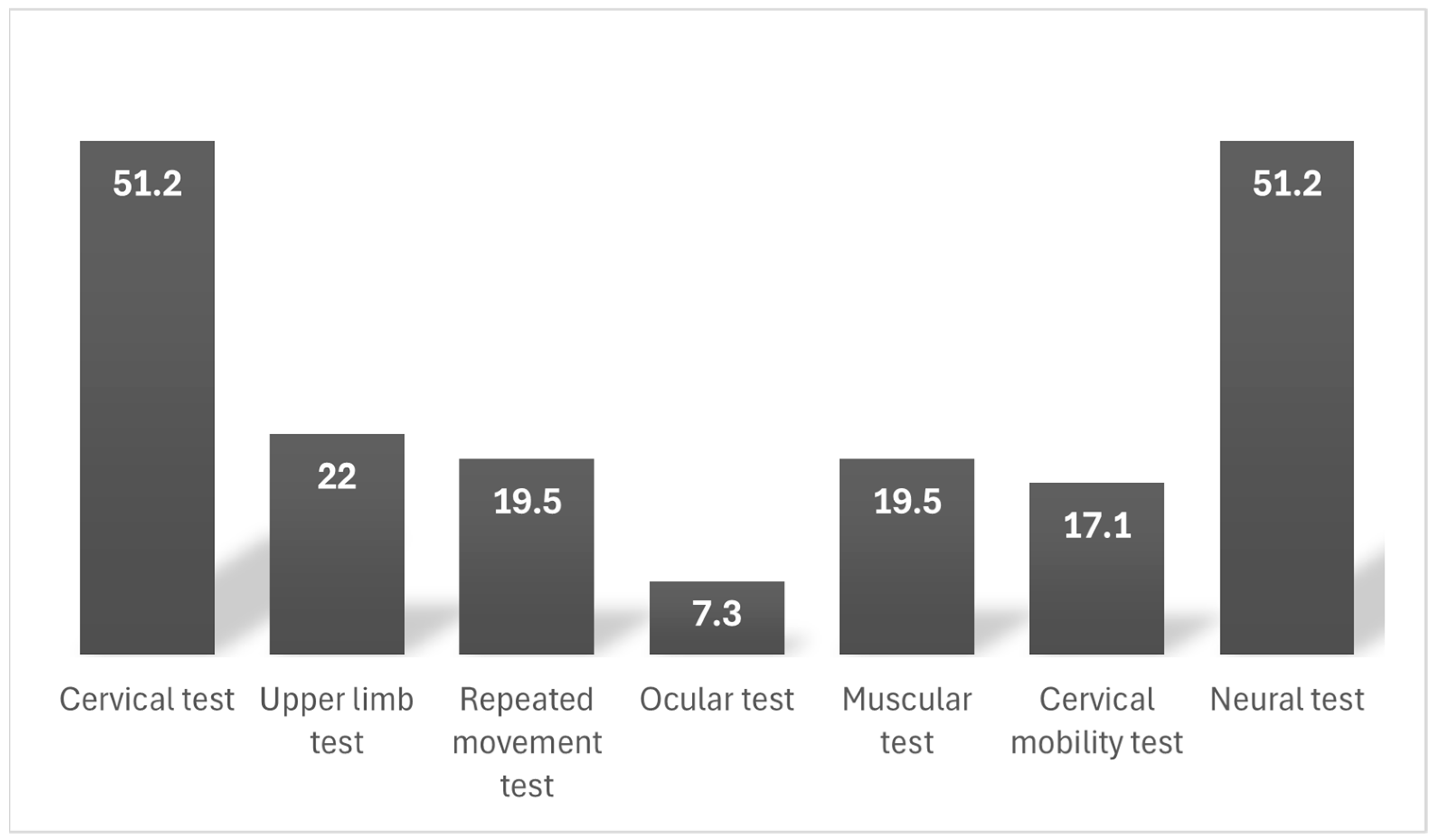
In addition to these tests, the majority of professionals (65.9%) incorporated at least one additional test for differential diagnosis. The most frequently used test was the neural and cervical test (51.2%), followed by the upper limb test (22%), the repeated movement test and muscular test (19.5%), the cervical mobility test (17.1%), and the ocular test (7.3%) (Figure 3). Only 7.5% of physiotherapist professionals reported using a specific classification system for CNP.

Figure 3.
Additional tests for differential diagnosis of chronic neck pain (%).
Participants’ knowledge, perceptions, and opinions regarding the differential diagnosis of chronic neck pain are presented in Table 3.

Table 3.
Participants’ knowledge, perceptions, and opinions regarding the differential diagnosis of chronic neck pain.
A total of 80% of professionals reported following a process to define the differential diagnosis. Among the items included in the differential diagnosis, the exclusion of red flags was the most frequent (92.5%), followed by the identification of elements involved in the patient’s symptoms (87.5%), identification of the factors contributing to pain (77.5%), and the use of a classification (36.3%). The most frequently identified underlying dysfunction pattern was sensor and motor control dysfunction (61.3%). Half of the professionals considered differential diagnosis important in the choice of treatment, and 47.5% deemed it important for CNP recovery.
4. Discussion
The results of this study provide a comprehensive overview of the current practices, knowledge, and approaches of physiotherapists in the differential diagnosis of chronic neck pain. The data revealed several key trends related to the demographic profile, clinical experience, and diagnostic methods employed by physiotherapists.
Considering the need for a systematic approach to differential diagnosis in the management of chronic pain pathologies [20,21], our study highlights the characteristics of differential diagnosis for chronic neck pain to further enhance the consistency and applicability of future management.
The sample was predominantly male, with a majority of participants falling within the 25–40 age range. The mean years of work experience suggest that the respondents are relatively experienced, although there is a notable variation in the years of experience among them. Other studies focused on physical therapist clinical practices have explored a similar age range but with more work experience, considering similar sample sizes as adequate [22,23]. A significant proportion reported having completed postgraduate courses, which indicates a solid foundation of advanced knowledge among the participants. This is relevant given the complexities involved in diagnosing chronic neck pain, which often requires specialized knowledge and expertise [24,25]. Additionally, the high percentage of physiotherapists who have undergone specialization training on CNP or differential diagnostic techniques within the last five years reflects a strong commitment to professional development. In this line, the questionnaire of Morales-Osorio et al. [26] regarding clinical practice in physical therapists in Latin America found that clinical experience and educational background may behave as facilitators or barriers for clinical decision making. A study observed that factors such as individual knowledge and experience, personal routines and habits, the sense of powerlessness to modify patients’ external factors, and patients’ reluctance to adopt a biopsychosocial approach influenced physiotherapists’ clinical decisions regarding the cause and prognosis of neck pain [27].
Regarding clinical practice, a substantial proportion of physiotherapists reported that 11–20% of their patients were diagnosed with CNP. That prevalence is similar to published data stating that CNP is a common condition encountered in physiotherapy practice [28]. However, the variation in the prevalence of CNP among patients reported in different studies [29,30] highlights the diversity in clinical caseloads and the potential influence of factors such as specialization or practice setting.
One of the most notable findings from this study is the moderate familiarity of physiotherapists with the red flags associated with CNP, with 61.3% reporting a moderate level of familiarity. The frequency of identifying red flags, typically once a month, further highlights the importance of maintaining vigilance in recognizing these signs during clinical assessment [31]. However, there appears to be a gap in the utilization of specific exclusion criteria and diagnostic tests for red flags. A significant portion of physiotherapists did not employ specific ligament, orthopedic, neurological, or vascular tests, suggesting potential limitations in the diagnostic rigor applied by some practitioners [32].
The use of specific tests for the differential diagnosis of CNP also varied widely. The lack of standardized testing practices raises concerns about the variability in the accuracy and consistency of diagnoses across different practitioners [33]. Furthermore, while 50% of physiotherapists were familiar with factors contributing to CNP, only a small percentage used specific tests to assess these contributing factors, highlighting a gap in the application of evidence-based diagnostic tools.
Importantly, the study identified that the exclusion of red flags, the identification of symptomatic elements, and the understanding of factors contributing to pain were considered key components in the differential diagnosis process. These findings also have important implications for physiotherapy training programs and patient care strategies to ensure the safety of patients with chronic neck pain. By addressing these gaps, we can improve both the quality of education for physiotherapy professionals and the outcomes for patients.
While the majority of physiotherapists acknowledged the importance of differential diagnosis in selecting treatment strategies and promoting recovery, there is a need for further emphasis on developing and integrating systematic diagnostic approaches into everyday clinical practice.
Several limitations of this study must be taken into consideration. The online questionnaire used was not previously validated; therefore, this represents an important limitation of our study, and we suggest that the results be interpreted with caution. In addition, this study relies on self-reported data, as participants’ responses were based on self-assessment. Future research should include the validation of the questionnaire and consider alternative methods, such as direct observation or case-based assessments, to minimize response bias and provide more objective results.
In conclusion, while the findings suggest that physiotherapists generally follow a structured approach to diagnosing CNP, there are notable gaps in the use of specific diagnostic tests, classification systems, and the comprehensive assessment of red flags and contributing factors. Given the complexity of chronic neck pain and its potential to be influenced by multiple factors, enhancing the consistency and depth of diagnostic practices among physiotherapists could significantly improve patient outcomes. Future research should focus on exploring the barriers to implementing more standardized diagnostic protocols and developing targeted interventions to address these gaps. Future research should focus on assessing the effectiveness of standardized diagnostic protocols and their impact on clinical decision making among physical therapists. Additionally, studies should explore the barriers to implementing evidence-based differential diagnosis techniques, including time constraints, access to diagnostic tools, and specific training. Longitudinal research is also needed to determine whether improved diagnostic accuracy translates into better patient outcomes.
Author Contributions
Conceptualization, C.S.V.-F. and M.C.V.; methodology, J.R.-B. and C.S.V.-F.; formal analysis, M.C.V.; investigation, C.S.V.-F. and M.G.-S.; resources, J.Z.-T.; data curation, M.G.-S. and A.H.-C.; writing—original draft preparation, J.R.-B., M.G.-S. and J.Z.-T.; writing—review and editing, M.C.V. and A.H.-C.; supervision, M.C.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
According to the General Data Protection Regulation (GDPR) and French data protection laws, research projects using non-sensitive data may proceed without ethics committee approval, provided they adhere to data protection principles and respect individuals’ rights. Informed consent was obtained from all subjects involved in this study, which was conducted in accordance with the Declaration of Helsinki. No personal or sensitive participant data were collected, and all applicable ethical principles were upheld throughout the research.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are unavailable due to privacy and ethical restrictions.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Kazeminasab, S.; Nejadghaderi, S.A.; Amiri, P.; Pourfathi, H.; Araj-Khodaei, M.; Sullman, M.J.; Kolahi, A.A.; Safiri, S. Neck pain: Global epidemiology, trends and risk factors. BMC Musculoskelet. Disord. 2022, 23, 26. [Google Scholar] [CrossRef]
- Maistrello, L.F.; Zanconato, L.; Palese, A.; Geri, T.; Turolla, A.; Gianola, S.; Dell’isola, A.; Rossettini, G. Perceptions and experiences of individuals with neck pain: A systematic critical review of qualitative studies with meta-summary and meta-synthesis. Phys. Ther. 2002, 102, pzac080. [Google Scholar] [CrossRef] [PubMed]
- Turk, D.C.; Patel, K.V. Epidemiology and economics of chronic and recurrent pain. In Clinical Pain Management: A Practical Guide, 2nd ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2022; pp. 6–24. [Google Scholar]
- Prablek, M.; Gadot, R.; Xu, D.S.; Ropper, A.E. Neck pain: Differential diagnosis and management. Neurol. Clin. 2023, 41, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Devecchi, V.; Alalawi, A.; Liew, B.; Falla, D. A network analysis reveals the interaction between fear and physical features in people with neck pain. Sci. Rep. 2022, 12, 11304. [Google Scholar] [CrossRef] [PubMed]
- Peng, B.; Yang, L.; Li, Y.; Liu, T.; Liu, Y. Cervical proprioception impairment in neck pain-pathophysiology, clinical evaluation, and management: A narrative review. Pain Ther. 2021, 10, 143–164. [Google Scholar] [CrossRef]
- Sterling, M.; de Zoete, R.M.; Coppieters, I.; Farrell, S.F. Best evidence rehabilitation for chronic pain part 4: Neck pain. J. Clin. Med. 2019, 8, 1219. [Google Scholar] [CrossRef]
- Rampazo, É.P.; da Silva, V.R.; de Andrade, A.L.M.; Back, C.G.N.; Madeleine, P.; Arendt-Nielsen, L.; Liebano, R.E. Sensory, motor, and psychosocial characteristics of individuals with chronic neck pain: A case control study. Phys. Ther. 2021, 101, pzab104. [Google Scholar] [CrossRef]
- Childress, M.A.; Stuek, S.J. Neck pain: Initial evaluation and management. Am. Fam. Physician 2020, 102, 150–156. [Google Scholar]
- Freynhagen, R.; Parada, H.A.; Calderon-Ospina, C.A.; Chen, J.; Emril, D.R.; Fernández-Villacorta, F.J.; Franco, H.; Ho, K.-Y.; Lara-Solares, A.; Li, C.C.-F.; et al. Current understanding of the mixed pain concept: A brief narrative review. Curr. Med. Res. Opin. 2019, 35, 1011–1018. [Google Scholar] [CrossRef]
- Cutaia, G.; Gargano, R.; Cannella, R.; Feo, N.; Greco, A.; Merennino, G.; Nicastro, N.; Comelli, A.; Benfante, V.; Salvaggio, G.; et al. Radiomics analyses of schwannomas in the head and neck: A preliminary analysis. Lect. Notes Comput. Sci. 2022, 13373, 317–325. [Google Scholar]
- Comelli, A.; Stefano, A.; Russo, G.; Sabini, M.G.; Ippolito, M.; Bignardi, S.; Petrucci, G.; Yezzi, A. A smart and operator independent system to delineate tumours in Positron Emission Tomography scans. Comput. Biol. Med. 2018, 102, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.; Cui, L.; Huang, X.; Xiang, Y.; Xiao, J. EasiCSDeep: A deep learning model for Cervical Spondylosis Identification using surface electromyography signal. arXiv 2018, arXiv:1812.04912. [Google Scholar]
- Treede, R.-D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. Chronic pain as a symptom or a disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain 2019, 160, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Fujii, K.; Yamazaki, M.; Kang, J.D.; Risbud, M.V.; Cho, S.K.; Qureshi, S.A.; Hecht, A.C.; Iatridis, J.C. Discogenic back pain: Literature review of definition, diagnosis, and treatment. J. Bone Miner. Res. Plus 2019, 3, e10180. [Google Scholar] [CrossRef]
- Eysenbach, G. Improving the quality of web surveys: The checklist for reporting results of internet E-surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef]
- Damgaard, P.; Bartels, E.M.; Ris, I.; Christensen, R.; Juul-Kristensen, B. Evidence of Physiotherapy Interventions for Patients with Chronic Neck Pain: A Systematic Review of Randomised Controlled Trials. ISRN Pain 2013, 2013, 567175. [Google Scholar] [CrossRef]
- Verhagen, A.P. Physiotherapy management of neck pain. J. Physiother. 2021, 67, 5–11. [Google Scholar] [CrossRef]
- Simoni, G.; Bozzolan, M.; Bonnini, S.; Grassi, A.; Zucchini, A.; Mazzanti, C.; Oliva, D.; Caterino, F.; Gallo, A.; Da Roit, M. Effectiveness of standard cervical physiotherapy plus diaphragm manual therapy on pain in patients with chronic neck pain: A randomized controlled trial. J. Bodyw. Mov. Ther. 2021, 26, 481–491. [Google Scholar] [CrossRef]
- Mathers, J.J. Differential diagnosis of a patient referred to physical therapy with neck pain: A case study of a patient with an atypical presentation of angina. J. Man. Manip. Ther. 2012, 20, 214–218. [Google Scholar] [CrossRef]
- Slaven, E.J.; Mathers, J. Differential diagnosis of shoulder and cervical pain: A case report. J. Man. Manip. Ther. 2010, 18, 191–196. [Google Scholar] [CrossRef]
- Sangoseni, O.; Hellman, M.; Hill, C. Development and validation of a questionnaire to assess the effect of online learning on behaviors, attitudes, and clinical practices of physical therapists in the United States regarding evidenced-based clinical practice. Internet J. Allied Health Sci. Pract. 2013, 11, 7. [Google Scholar] [CrossRef]
- Jette, D.U.; Bacon, K.; Batty, C.; Carlson, M.; Ferland, A.; Hemingway, R.D.; Hill, J.C.; Ogilvie, L.; Volk, D. Evidence-based practice: Beliefs, attitudes, knowledge, and behaviors of physical therapists. Phys. Ther. 2003, 83, 786–805. [Google Scholar] [CrossRef] [PubMed]
- Devonshire, E.; Nicholas, M.K. Continuing education in pain management: Using a competency framework to guide professional development. Pain Rep. 2018, 3, e688. [Google Scholar] [CrossRef]
- Munneke, W.; Demoulin, C.; Nijs, J. Development of an interdisciplinary training program about chronic pain management with a cognitive behavioural approach for healthcare professionals: Part of a hybrid effectiveness-implementation study. BMC Med. Educ. 2024, 24, 331. [Google Scholar] [CrossRef]
- Morales-Osorio, M.A.; Ordoñez-Mora, L.T.; Gutiérrez-Espinoza, H.; Araya-Quintanilla, F.; Bays-Moneo, A.; Ramírez-Vélez, R. A survey of beliefs, attitudes, knowledge, and behaviors about evidence-based practice in physical therapists of Latin America: A cross-sectional study. Sci. Rep. 2024, 14, 27404. [Google Scholar] [CrossRef]
- Verwoerd, M.J.; Wittink, H.; Goossens, M.E.J.B.; Maissan, F.; Smeets, R.J.E.M. Physiotherapists’ knowledge, attitude and practice behavior to prevent chronification in patients with non-specific, non-traumatic, acute- and subacute neck pain: A qualitative study. Musculoskelet Sci. Pract. 2022, 57, 102493. [Google Scholar] [CrossRef]
- Carlesso, L.C.; MacDermid, J.C.; Gross, A.R.; Walton, D.M.; Santaguida, P.L. Treatment preferences amongst physical therapists and chiropractors for the management of neck pain: Results of an international survey. Chiropr. Man. Ther. 2024, 22, 11. [Google Scholar] [CrossRef]
- Genebra, C.V.D.S.; Maciel, N.M.; Bento, T.P.F.; Simeão, S.F.A.P.; De Vitta, A. Prevalence and factors associated with neck pain: A population-based study. Braz. J. Phys. Ther. 2017, 21, 274–280. [Google Scholar] [CrossRef]
- Karels, C.H.; Polling, W.; Bierma-Zeinstra, S.M.A.; Burdorf, A.; Verhagen, A.P.; Koes, B.W. Treatment of arm, neck, and/or shoulder complaints in physical therapy practice. Spine 2006, 31, E584–E589. [Google Scholar] [CrossRef]
- Sizer, P.S., Jr.; Brismée, J.M.; Cook, C. Medical screening for red flags in the diagnosis and management of musculoskeletal spine pain. Pain Pract. 2007, 7, 53–71. [Google Scholar] [CrossRef]
- Feller, D.; Chiarotto, A.; Koes, B.; Maselli, F.; Mourad, F. Red flags for potential serious pathologies in people with neck pain: A systematic review of clinical practice guidelines. Arch. Physiother. 2024, 14, 105. [Google Scholar] [CrossRef]
- Bier, J.D.; Scholten-Peeters, W.G.; Staal, J.B.; Pool, J.; van Tulder, M.W.; Beekman, E.; Knoop, J.; Meerhoff, G.; Verhagen, A.P. Clinical practice guideline for physical therapy assessment and treatment in patients with nonspecific neck pain. Phys. Ther. 2018, 98, 162–171. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).