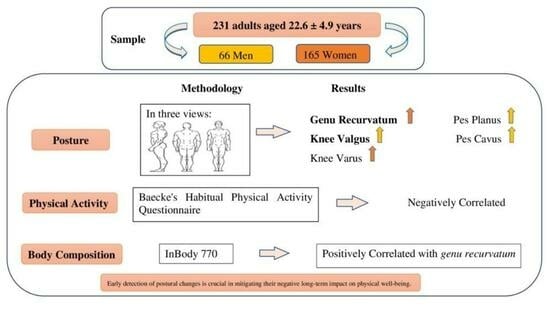
Association between Body Composition, Physical Activity Profile, and Occurrence of Knee and Foot Postural Alterations among Young Healthy Adults
Abstract
1. Introduction
2. Methodology
2.1. Sample
2.2. General Procedure
2.2.1. Postural Evaluation
- (a)
- In the Anterior View
- (b)
- In the Side View
- (c)
- In the Posterior View
2.2.2. Body Composition
2.2.3. Physical Activity
- (a)
- Formal PA
- (b)
- Informal PA
- (c)
- Total Practical History
- (d)
- Frequency of PA
2.3. Statistical Analysis
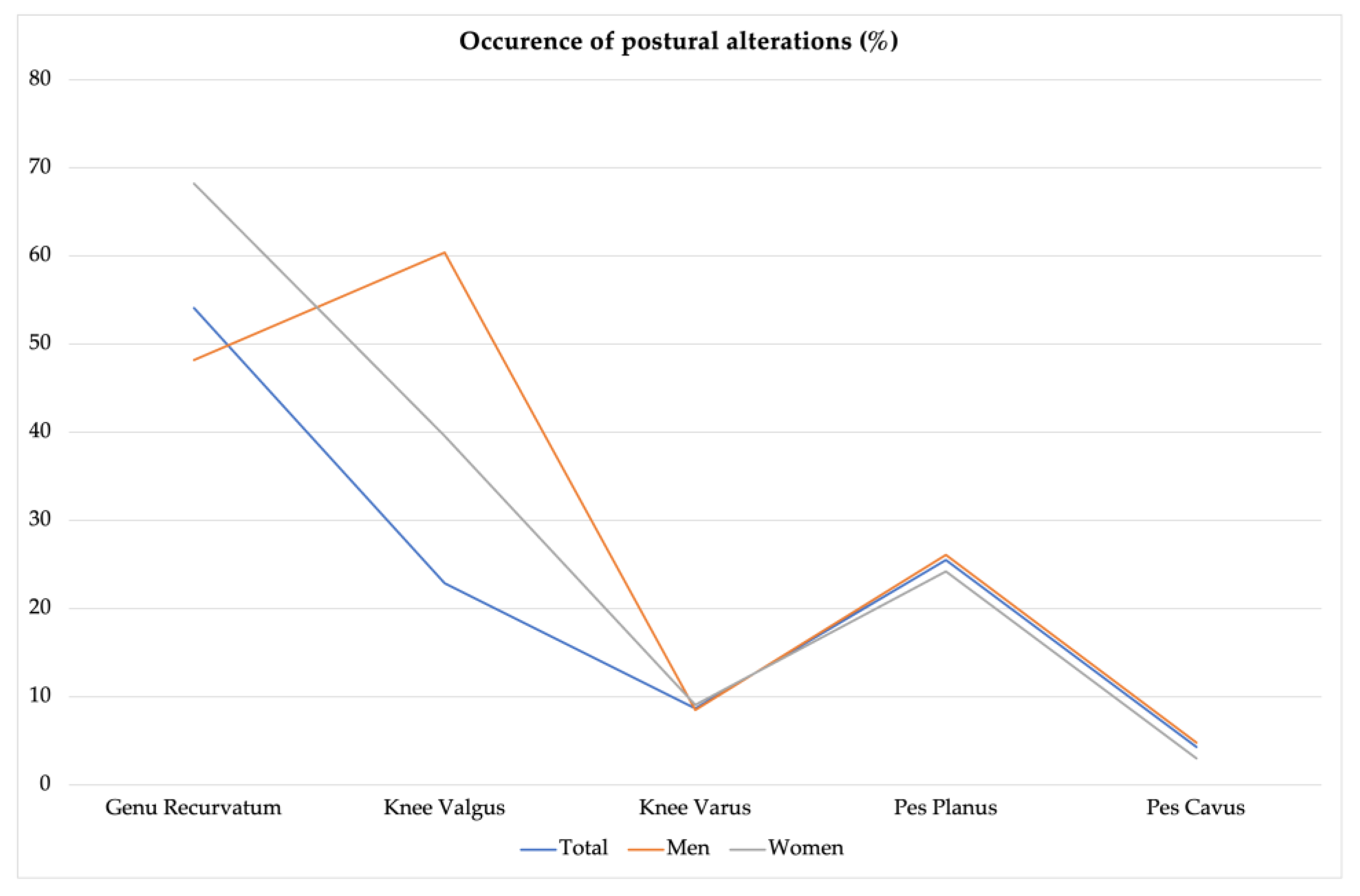
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Smith, L.K.; Weiss, L.; Lehmkuhl, L.D. Brunnstrom’s Clinical Kinesiology; FA Davis: Philadelphia, PA, USA, 1996. [Google Scholar]
- Barker, V. Postura, Posizione, Movimento per Potenziare le Prestazioni Sessuali, Rimodellare il Corpo, Ritardare L’invecchiamento, Ridurre L’obesità, Sviluppare le Capacità; Edizioni Mediterranee: Roma, Italy, 1998. [Google Scholar]
- Teixeira, L. Importância do Movimento Humano na Relação Homem/Trabalho: Aspectos Posturais; Cepeusp: São Paulo, Brazil, 1996. [Google Scholar]
- Bernard, P.; Geraci, M.; Hue, O.; Amato, M.; Seynnes, O.; Lantieri, D. Influence of obesity on postural capacities of teenagers. Preliminary study. Ann. Readapt. Med. Phys. 2003, 46, 184–190. [Google Scholar]
- Detsch, C.; Luz, A.M.H.; Candotti, C.T.; Oliveira, D.S.D.; Lazaron, F.; Guimarães, L.K.; Schimanoski, P. Prevalência de alterações posturais em escolares do ensino médio em uma cidade no Sul do Brasil. Rev. Panam. De Salud Publica 2007, 21, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Andrews, D.M.; Fiedler, K.M.; Weir, P.L.; Callaghan, J.P. The effect of posture category salience on decision times and errors when using observation-based posture assessment methods. Ergonomics 2012, 55, 1548–1558. [Google Scholar] [CrossRef] [PubMed]
- Iedynak, G.; Galamandjuk, L.; Kyselytsia, O.; Nakonechnyi, I.; Hakman, A.; Chopik, O. Special aspects of changes in physical readiness indicators of young men with different somatotypes between 15 and 17 years of age. J. Phys. Educ. Sport 2017, 17, 2690–2696. [Google Scholar]
- Kashuba, V.; Dudko, M. Sovremennye podkhody, metodiki i tekhnologii k formirovaniiu zdorovogo obraza zhizni studentov v processe fizicheskogo vospitaniia [Modern approaches to, methodic and technologies of students’ healthy life style formation in process of physical education]. Fiz. Vikhovannia Sport I Kul’tura Zdorov’ia U Suchasnomu Suspil’stvi 2015, 1, 52–57. [Google Scholar]
- Torlakovic, A.; Muftic, M.; Radjo, I.; Talovic, M.; Mahmutovic, I. Evolution of sports-medical team management in the program of posture correction in children. Mater. Socio-Medica 2014, 26, 104. [Google Scholar] [CrossRef] [PubMed]
- Dahle, L.K.; Mueller, M.; Delitto, A.; Diamond, J.E. Visual assessment of foot type and relationship of foot type to lower extremity injury. J. Orthop. Sports Phys. Ther. 1991, 14, 70–74. [Google Scholar] [CrossRef] [PubMed]
- Nigg, B.M.; Cole, G.K.; Nachbauer, W. Effects of arch height of the foot on angular motion of the lower extremities in running. J. Biomech. 1993, 26, 909–916. [Google Scholar] [CrossRef]
- Mølgaard, C.; Lundbye-Christensen, S.; Simonsen, O. High prevalence of foot problems in the Danish population: A survey of causes and associations. Foot 2010, 20, 7–11. [Google Scholar] [CrossRef]
- Chandler, J.T.; Moskal, J.T. Evaluation of knee and hindfoot alignment before and after total knee arthroplasty: A prospective analysis. J. Arthroplast. 2004, 19, 211–216. [Google Scholar] [CrossRef]
- Abourazzak, F.; Kadi, N.; Azzouzi, H.; Lazrak, F.; Najdi, A.; Nejjari, C.; Harzy, T. A positive association between foot posture index and medial compartment knee osteoarthritis in moroccan people. Open Rheumatol. J. 2014, 8, 96. [Google Scholar]
- Sheng, B.; Li, X.; Nussler, A.K.; Zhu, S. The relationship between healthy lifestyles and bone health: A narrative review. Medicine 2021, 100, e24684. [Google Scholar] [CrossRef] [PubMed]
- Browning, R.C. Locomotion mechanics in obese adults and children. Curr. Obes. Rep. 2012, 1, 152–159. [Google Scholar] [CrossRef]
- Kim, D.; Lewis, C.L.; Gill, S.V. Effects of obesity and foot arch height on gait mechanics: A cross-sectional study. PLoS ONE 2021, 16, e0260398. [Google Scholar] [CrossRef] [PubMed]
- Butterworth, P.A.; Urquhart, D.M.; Landorf, K.B.; Wluka, A.E.; Cicuttini, F.M.; Menz, H.B. Foot posture, range of motion and plantar pressure characteristics in obese and non-obese individuals. Gait Posture 2015, 41, 465–469. [Google Scholar] [CrossRef]
- Brownstein, B.; Noyes, F.R.; Mangine, R.E.; Kryger, S. Physical Therapy of the Knee: Anatomy and Biomechanics; Mangine, R.E., Ed.; Churchill Livingstone: New York, NY, USA, 1988. [Google Scholar]
- Jalalvand, H.; Fatahi, A.; Entezari Khorasani, Z. Comparison of the Kinematic Pattern of Knee Joint Flexion in Healthy and Genu Valgum and Genu Varum Children During Jumping. J. Sport Biomech. 2021, 7, 270–279. [Google Scholar] [CrossRef]
- Franco, A.H. Pes cavus and pes planus: Analyses and treatment. Phys. Ther. 1987, 67, 688–694. [Google Scholar] [CrossRef]
- Oatis, C.A. Kinesiology the Mechanics and Pathomechanics of Human Movement; Wolters Kluwer: Alphen aan den Rijn, The Netherlands, 2009. [Google Scholar]
- Berrigan, F.; Simoneau, M.; Tremblay, A.; Hue, O.; Teasdale, N. Influence of obesity on accurate and rapid arm movement performed from a standing posture. Int. J. Obes. 2006, 30, 1750–1757. [Google Scholar] [CrossRef]
- Hue, O.; Simoneau, M.; Marcotte, J.; Berrigan, F.; Doré, J.; Marceau, P.; Marceau, S.; Tremblay, A.; Teasdale, N. Body weight is a strong predictor of postural stability. Gait Posture 2007, 26, 32–38. [Google Scholar] [CrossRef]
- Maffiuletti, N.; Agosti, F.; Proietti, M.; Riva, D.; Resnik, M.; Lafortuna, C.; Sartorio, A. Postural instability of extremely obese individuals improves after a body weight reduction program entailing specific balance training. J. Endocrinol. Investig. 2005, 28, 2–7. [Google Scholar] [CrossRef]
- Ghandi, A.R.; Hadi, H.A.; Behruzi, A.R.; Holakooie, A.R. The prevalence of genu-varum in students aged 7–16 in Arak city. J. Arak Univ. Med. Sci. 2012, 15, 63–68. [Google Scholar]
- Bray, G.A. Medical consequences of obesity. J. Clin. Endocrinol. Metab. 2004, 89, 2583–2589. [Google Scholar] [CrossRef] [PubMed]
- Janssen, I.; Katzmarzyk, P.T.; Ross, R. Body mass index, waist circumference, and health risk: Evidence in support of current National Institutes of Health guidelines. Arch. Intern. Med. 2002, 162, 2074–2079. [Google Scholar] [CrossRef] [PubMed]
- Kopelman, P.G. Obesity as a medical problem. Nature 2000, 404, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Tomaszewska, A.; Pawlicka-Lisowska, A. Evaluation of an influence of systematic motor activity on the body posture of young people. Pol. Merkur. Lek. Organ Pol. Tow. Lek. 2014, 36, 336–340. [Google Scholar]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Radaš, J.; Bobić, T.T. Posture in top-level Croatian rhythmic gymnasts and non-trainees. Kinesiology 2011, 43, 64–73. [Google Scholar]
- Florindo, A.A.; Latorre, M.D.R.D.D.O.; Santos, E.C.M.D.; Negrão, C.E.; Azevedo, L.F.; Segurado, A.A.C. Validity and reliability of the Baecke questionnaire for the evaluation of habitual physical activity among people living with HIV/AIDS. Cad. De Saúde Pública 2006, 22, 535–541. [Google Scholar] [CrossRef]
- Loudon, J.K.; Jenkins, W.; Loudon, K.L. The relationship between static posture and ACL injury in female athletes. J. Orthop. Sports Phys. Ther. 1996, 24, 91–97. [Google Scholar] [CrossRef]
- Nguyen, A.-D.; Shultz, S.J. Sex differences in clinical measures of lower extremity alignment. J. Orthop. Sports Phys. Ther. 2007, 37, 389–398. [Google Scholar] [CrossRef]
- Stanley, H. Physical Examination of the Spine and Extremities; Appleton-Century-Crofts: New York, NY, USA, 1976. [Google Scholar]
- Penha, P.J.; João, S.M.A.; Casarotto, R.A.; Amino, C.J.; Penteado, D.C. Postural assessment of girls between 7 and 10 years of age. Clinics 2005, 60, 9–16. [Google Scholar] [CrossRef]
- Gh, M.E.; Alilou, A.; Ghafurinia, S.; Fereydounnia, S. Prevalence of faulty posture in children and youth from a rural region in Iran. Biomed. Hum. Kinet. 2012, 4, 121–126. [Google Scholar] [CrossRef]
- Hutchinson, M.R.; Ireland, M.L. Knee injuries in female athletes. Sports Med. 1995, 19, 288–302. [Google Scholar] [CrossRef] [PubMed]
- Kendall, F. Kendall-McCreary, and Provance PG. Muscles Testing and Function; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 1993. [Google Scholar]
- Stauffer, R.N.; Chao, E.Y.; Györy, A.N. Biomechanical gait analysis of the diseased knee joint. Clin. Orthop. Relat. Res. 1977, 126, 246–255. [Google Scholar] [CrossRef]
- Scerpella, T.A.; Stayer, T.J.; Makhuli, B.Z. Ligamentous laxity and non-contact anterior cruciate ligament tears: A gender-based comparison. Orthopedics 2005, 28, 656–660. [Google Scholar] [CrossRef] [PubMed]
- Shultz, S.J.; Schmitz, R.J.; Nguyen, A.-D.; Chaudhari, A.M.; Padua, D.A.; McLean, S.G.; Sigward, S.M. ACL Research Retreat V: An update on ACL injury risk and prevention, March 25–27, 2010, Greensboro, NC. J. Athl. Train. 2010, 45, 499–508. [Google Scholar] [CrossRef]
- Anderson, A.F.; Dome, D.C.; Gautam, S.; Awh, M.H.; Rennirt, G.W. Correlation of anthropometric measurements, strength, anterior cruciate ligament size, and intercondylar notch characteristics to sex differences in anterior cruciate ligament tear rates. Am. J. Sports Med. 2001, 29, 58–66. [Google Scholar] [CrossRef]
- Chandrashekar, N.; Mansouri, H.; Slauterbeck, J.; Hashemi, J. Sex-based differences in the tensile properties of the human anterior cruciate ligament. J. Biomech. 2006, 39, 2943–2950. [Google Scholar] [CrossRef]
- Maciałczyk-Paprocka, K.; Stawińska-Witoszyńska, B.; Kotwicki, T.; Sowińska, A.; Krzyżaniak, A.; Walkowiak, J.; Krzywińska-Wiewiorowska, M. Prevalence of incorrect body posture in children and adolescents with overweight and obesity. Eur. J. Pediatr. 2017, 176, 563–572. [Google Scholar] [CrossRef]
- Odding, E.; Valkenburg, H.; Algra, D.; Vandenouweland, F.; Grobbee, D.; Hofman, A. The association of abnormalities on physical examination of the hip and knee with locomotor disability in the Rotterdam Study. Rheumatology 1996, 35, 884–890. [Google Scholar] [CrossRef]
- Sanchis, G.J.B.; Lopes, J.M.; de Assis, S.J.C.; Catão, R.L.A.; Santos, T.R.T.; Roncalli, A.G.D.C.O. Dynamic knee valgus prevalence in children and its association with pain intensity, foot mobility, and sex—A cross-sectional study. Heliyon 2022, 8, e10984. [Google Scholar] [CrossRef]
- Ganeb, S.S.; Egaila, S.E.-S.; Younis, A.A.; El-Aziz, A.M.A.; Hashaad, N.I. Prevalence of lower limb deformities among primary school students. Egypt. Rheumatol. Rehabil. 2021, 48, 1–7. [Google Scholar] [CrossRef]
- Azhagiri, R.; Malar, A.; Hemapriya, J.; Sumathi, G. The cause and frequency of PES Planus (Flat Foot) problems among young adults. Asian J. Med. Sci. 2021, 12, 107. [Google Scholar]
- Kharbuja, R.; Dhungel, S. Prevalence of Pes Cavus and Pes Planus Among School Going Children of Bhaktapur District, Nepal. Nepal. Med. Coll. J. 2017, 19, 9–12. [Google Scholar]
- Bafor, A.; Chibuzom, C. Foot and ankle abnormalities among a cohort of Nigerian school children: An epidemiological study. Int. Orthop. 2020, 44, 1169–1175. [Google Scholar] [CrossRef] [PubMed]
- Chou, L.-W.; Chen, F.-F.; Lo, S.-F.; Yang, P.-Y.; Meng, N.-H.; Lin, C.-L.; Liao, F.-Y.; Kao, M.-J. The prevalence of four common pathomechanical foot deformities in primary school students in Taichung county. Mid Taiwan J. Med. 2009, 14, 1–9. [Google Scholar]
- Kordi, Y.A. The evaluation and prevalence of foot problems among iranian students using “alfoot” company scanner. Health Sci. J. 2014, 8, 393. [Google Scholar]
- St-Onge, M.-P. Relationship between body composition changes and changes in physical function and metabolic risk factors in aging. Curr. Opin. Clin. Nutr. Metab. Care 2005, 8, 523–528. [Google Scholar] [CrossRef]
- Loudon, J.K.; Goist, H.L.; Loudon, K.L. Genu recurvatum syndrome. J. Orthop. Sports Phys. Ther. 1998, 27, 361–367. [Google Scholar] [CrossRef]
- Ahn, S.-H.; Kwon, O.-Y.; Hwang, U.-J.; Jung, S.-H.; Kim, H.-A.; Kim, J.-H. The association between genu recurvatum angle and the strength of the hip and knee muscles in standing workers. Work 2020, 66, 173–181. [Google Scholar] [CrossRef]
- Lasjouri, G.; Mirzaei, B. The prevalence of postural deformities in pupils aged 11–13 and their relationship with age, height and weight factors. Res. Sport Sci. 2005, 3, 123–133. [Google Scholar]
- Soheilipour, F.; Pazouki, A.; Mazaherinezhad, A.; Yagoubzadeh, K.; Dadgostar, H.; Rouhani, F. The prevalence of genu varum and genu valgum in overweight and obese patients: Assessing the relationship between body mass index and knee angular deformities. Acta Bio Medica Atenei Parm. 2020, 91, e2020121. [Google Scholar]
- Ciaccia, M.C.C.; Pinto, C.N.; Golfieri, F.d.C.; Machado, T.F.; Lozano, L.L.; Silva, J.M.S.; Rullo, V.E.V. Prevalence of genu valgum in public elementary schools in the city of Santos (SP), Brazil. Rev. Paul. De Pediatr. 2017, 35, 443–447. [Google Scholar] [CrossRef] [PubMed]
- Shapouri, J.; Aghaali, M.; Aghaei, M.; Iranikhah, A.; Ahmadi, R.; Hovsepian, S. Prevalence of lower extremities’ postural deformities in overweight and normal weight school children. Iran. J. Pediatr. 2019, 29, 6. [Google Scholar] [CrossRef]
- Taylor, E.D.; Theim, K.R.; Mirch, M.C.; Ghorbani, S.; Tanofsky-Kraff, M.; Adler-Wailes, D.C.; Brady, S.; Reynolds, J.C.; Calis, K.A.; Yanovski, J.A. Orthopedic complications of overweight in children and adolescents. Pediatrics 2006, 117, 2167–2174. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.-P.; Chung, M.-J.; Wang, M.-J. Flatfoot prevalence and foot dimensions of 5- to 13-year-old children in Taiwan. Foot Ankle Int. 2009, 30, 326–332. [Google Scholar] [CrossRef] [PubMed]
- Suciati, T.; Adnindya, M.R.; Septadina, I.S.; Pratiwi, P.P. Correlation between flat feet and body mass index in primary school students. In Journal of Physics: Conference Series; IOP Publishing: Bristol, UK, 2019; p. 012063. [Google Scholar]
- Lee, J. Comparisons of incidence of spinal and lower extremity deformities according to the physical characteristics between sports major and nonmajor college students. J. Exerc. Rehabil. 2017, 13, 240. [Google Scholar] [CrossRef] [PubMed]
- Gribble, P.A.; Hertel, J. Effect of lower-extremity muscle fatigue on postural control. Arch. Phys. Med. Rehabil. 2004, 85, 589–592. [Google Scholar] [CrossRef] [PubMed]
- Cetin, N.; Bayramoglu, M.; Aytar, A.; Surenkok, O.; Yemisci, O.U. Effects of lower-extremity and trunk muscle fatigue on balance. Open Sports Med. J. 2008, 2, 16–22. [Google Scholar] [CrossRef]
- Susco, T.M.; McLeod, T.C.V.; Gansneder, B.M.; Shultz, S.J. Balance recovers within 20 minutes after exertion as measured by the balance error scoring system. J. Athl. Train. 2004, 39, 241. [Google Scholar]
- Zemková, E.; Hamar, D. Postural Sway Response to Exercise: The Effect of Intensity and Duration. Int. J. Appl. Sports Sci. 2005, 17, 1. [Google Scholar]
- Simoneau, M.; Bégin, F.; Teasdale, N. The effects of moderate fatigue on dynamic balance control and attentional demands. J. Neuroeng. Rehabil. 2006, 3, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Vuillerme, N.; Anziani, B.; Rougier, P. Trunk extensor muscles fatigue affects undisturbed postural control in young healthy adults. Clin. Biomech. 2007, 22, 489–494. [Google Scholar] [CrossRef] [PubMed]
- Yaggie, J.; Armstrong, W.J. Effects of lower extremity fatigue on indices of balance. J. Sport Rehabil. 2004, 13, 312–322. [Google Scholar] [CrossRef]
- Deland, J.T. The adult acquired flatfoot and spring ligament complex: Pathology and implications for treatment. Foot Ankle Clin. 2001, 6, 129–135. [Google Scholar] [CrossRef]
- Kızılcı, H.; Erbahçeci, F. Pes planus olan ve olmayan erkeklerde fiziksel uygunluğun değerlendirilmesi. Fiz. Rehabil. 2016, 27, 25–33. [Google Scholar] [CrossRef]
- Aleander, I.J.; Johnson, K.A. Assessment and management of pes cavus in Charcot-Marie-tooth disease. Clin. Orthop. Relat. Res. 1989, 246, 273–281. [Google Scholar]
- Sabir, M.; Lyttle, D. Pathogenesis of pes cavus in Charcot-Marie-Tooth disease. Clin. Orthop. Relat. Res. 1983, 175, 173–178. [Google Scholar] [CrossRef]
- Babu, D.; Bordoni, B. Anatomy, bony pelvis and lower limb, medial longitudinal arch of the foot. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Şahin, F.N.; Ceylan, L.; Küçük, H.; Ceylan, T.; Arıkan, G.; Yiğit, S.; Sarşık, D.Ç.; Güler, Ö. Examining the Relationship between Pes Planus Degree, Balance and Jump Performances in Athletes. Int. J. Environ. Res. Public Health 2022, 19, 11602. [Google Scholar] [CrossRef]
- Zhao, X.; Tsujimoto, T.; Kim, B.; Tanaka, K. Association of arch height with ankle muscle strength and physical performance in adult men. Biol. Sport 2017, 34, 119–126. [Google Scholar] [CrossRef]
- Neal, B.S.; Griffiths, I.B.; Dowling, G.J.; Murley, G.S.; Munteanu, S.E.; Franettovich Smith, M.M.; Collins, N.J.; Barton, C.J. Foot posture as a risk factor for lower limb overuse injury: A systematic review and meta-analysis. J. Foot Ankle Res. 2014, 7, 1–13. [Google Scholar] [CrossRef]

| Genu Recurvatum | Knee Valgus | Knee Varus | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | With | Without | Comparison | With | Without | Comparison | With | Without | Comparison | |||
| Mean ± SD | Mean ± SD | t | p | Mean ± SD | Mean ± SD | t | p | Mean ± SD | Mean ± SD | t | p | |
| Stature (cm) | 171.21 ± 9.79 | 174.31 ± 8.44 | 2.497 | 0.013 * | 171.35 ± 9.97 | 172.93 ± 9.12 | 1.052 | 0.294 | 172.57± 9.50 | 172.95 ± 7.56 | −0.167 | 0.867 |
| Body Mass (kg) | 68.64 ± 12.23 | 70.68 ± 11.72 | 1.222 | 0.218 | 68.89 ± 11.53 | 69.72 ± 12.21 | 0.679 | 0.670 | 67.43 ± 7.84 | 69.64 ± 12.31 | 0.168 | 0.279 |
| BMI (kg/m2) | 23.27 ± 3.15 | 23.35 ± 2.64 | −0.293 | 0.769 | 23.43 ± 3.40 | 23.41 ± 2.79 | −0.030 | 0.976 | 2340 ± 2.91 | 23.09 ± 2.16 | 0.468 | 0.640 |
| TBW (L) | 40.48 ± 8.37 | 45.18 ± 7.67 | 2.897 | 0.005 ** | 40.21 ± 8.43 | 43.76 ± 8.14 | 1.907 | 0.060 | 42.71 ± 8.34 | 45.07 ± 9.47 | −0.481 | 0.632 |
| Intracellular Water (L) | 25.56 ± 5.41 | 28.61 ± 4.96 | 2.909 | 0.005 ** | 25.39 ± 5.43 | 27.69 ± 5.28 | 1.911 | 0.059 | 27.01 ± 5.40 | 28.60 ± 6.16 | −0.491 | 0.624 |
| Extracellular Water (L) | 14.92 ± 2.91 | 16.57 ± 2.72 | 2.863 | 0.005 ** | 14.82 ± 3.01 | 16.07 ± 2.87 | 1.892 | 0.062 | 16.50 ± 3.31 | 15.71 ± 2.96 | −0.459 | 0.647 |
| Protein (kg) | 11.05 ± 2.37 | 12.37 ± 2.14 | 2.911 | 0.004 ** | 10.97 ± 2.32 | 11.97 ± 2.29 | 1.909 | 0.059 | 11.67 ± 2.33 | 12.30 ± 2.64 | −0.457 | 0.649 |
| Minerals (kg) | 3.92 ± 0.80 | 4.34 ± 0.76 | 2.704 | 0.008 ** | 4.22 ± 0.79 | 3.87 ± 0.79 | 1.984 | 0.050 * | 4.48 ± 0.99 | 4.12 ± 0.80 | −0.773 | 0.441 |
| FM (%) | 20.78 ± 10.12 | 14.92 ± 7.01 | −3.333 | 0.001 ** | 17.05 ± 8.46 | 20.16 ± 10.75 | −1.502 | 0.136 | 17.77 ± 5.95 | 17.91 ± 9.31 | 0.027 | 0.979 |
| SMM (kg) | 31.32 ± 7.05 | 35.32 ± 6.47 | 2.918 | 0.004 ** | 31.09 ± 7.07 | 34.11 ± 6.89 | 1.921 | 0.058 | 33.22 ± 7.04 | 35.27 ± 8.01 | −0.495 | 0.622 |
| WHR (cm) | 0.86 ± 0.07 | 0.82 ± 0.04 | −3.045 | 0.003 ** | 0.85 ± 0.06 | 0.84 ± 0.06 | −0.665 | 0.507 | 0.85 ± 0.06 | 0.84 ± 0.06 | −0.213 | 0.832 |
| Pes Planus | Pes Cavus | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | With | Without | Comparison | With | Without | Comparison | ||
| Mean ± SD | Mean ± SD | t | p | Mean ± SD | Mean ± SD | t | p | |
| Stature (cm) | 171.47 ± 9.20 | 172.94 ± 9.39 | 1.019 | 0.309 | 176.50 ± 5.10 | 172.36 ± 9.46 | −2.372 | 0.035 * |
| Body Mass (kg) | 69.56 ± 12.27 | 69.51 ±11.98 | −0.022 | 0.982 | 72.37 ± 6.55 | 69.38 ± 12.23 | −0.765 | 0.445 |
| BMI (kg/m2) | 23.96 ± 3.31 | 23.22 ±2.76 | 0.093 | 0.108 | 23.35 ± 1.77 | 23.42 ± 2.96 | −1.613 | 0.945 |
| TBW (L) | 42.99 ± 8.27 | 42.99 ± 8.27 | 0.479 | 0.633 | 42.65 ± 8.36 | 45.83 ± 8.08 | 0.479 | 0.458 |
| Intracellular Water (L) | 26.54 ± 5.58 | 27.19 ± 5.37 | 0.488 | 0.627 | 26.96 ± 5.41 | 29.05 ± 5.22 | 0.488 | 0.453 |
| Extracellular Water (L) | 15.56 ± 3.13 | 15.80 ± 2.91 | 0.460 | 0.647 | 15.68 ± 2.96 | 16.78 ± 2.87 | 0.460 | 0.471 |
| Protein (kg) | 11.76 ± 2.32 | 11.46 ± 2.39 | 0.511 | 0.611 | 11.65 ± 2.34 | 12.53 ± 2.25 | 0.511 | 0.469 |
| Minerals (kg) | 4.15 ± 0.801 | 4.03 ± 0.82 | 0.587 | 0.558 | 4.11 ± 0.80 | 4.54 ± 0.84 | 0.587 | 0.301 |
| FM (%) | 17.53 ± 8.61 | 19.29 ± 11.25 | −0.776 | 0.439 | 17.98 ± 9.37 | 16.25 ± 3.49 | −0.776 | 0.715 |
| SMM (kg) | 33.46 ± 7.01 | 32.61 ± 7.27 | 0.590 | 0.627 | 33.17 ± 7.06 | 35.90 ± 6.81 | 0.487 | 0.450 |
| WHR (cm) | 0.85 ± 0.06 | 0.84 ± 0.06 | −0.423 | 0.673 | 0.84 ± 0.03 | 0.84 ± 0.06 | −0.423 | 0.863 |
| Genu Recurvatum | Knee Valgus | Knee Varus | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | With | Without | Comparison | With | Without | Comparison | With | Without | Comparison | |||
| Mean ± SD | Mean ± SD | t | p | Mean ± SD | Mean ± SD | t | p | Mean ± SD | Mean ± SD | t | p | |
| Score Formal PA | 11.93 ± 2.91 | 12.06 ± 3.10 | 0.292 | 0.770 | 12.70 ± 3.11 | 11.72 ± 2.91 | −1.989 | 0.048 * | 13.62 ± 1.66 | 11.85 ± 3.03 | −3.427 | 0.003 ** |
| Score Informal PA | 2.78 ± 0.58 | 2.81 ± 0.52 | 0.283 | 0.778 | 2.76 ± 0.57 | 2.81 ± 0.55 | 0.582 | 0.561 | 2.78 ± 0.67 | 2.79 ± 0.54 | 0.132 | 0.895 |
| Score Total | 14.89 ± 3.28 | 14.73 ± 3.10 | 0.339 | 0.735 | 15.46 ± 3.22 | 14.54 ± 3.13 | −1.730 | 0.085 | 16.57 ± 1.93 | 14.64 ± 3.21 | −3.279 | 0.004 ** |
| Practical History | 9.90 ± 5.64 | 9.34 ± 5.44 | −0.656 | 0.513 | 10.39 ± 5.11 | 9.38 ± 5.69 | −1.054 | 0.293 | 9.13 ± 4.68 | 9.75 ± 5.66 | 0.457 | 0.648 |
| Frequency of PA | 8.42 ± 4.57 | 7.91 ± 3.61 | −0.696 | 0.488 | 8.89 ± 5.10 | 7.94 ± 3.79 | −1.152 | 0.251 | 8.77 ± 4.66 | 8.16 ± 4.18 | −0.494 | 0.622 |
| Pes Planus | Pes Cavus | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | With | Without | Comparison | With | Without | Comparison | ||
| Mean ± SD | Mean ± SD | t | p | Mean ± SD | Mean ± SD | t | p | |
| Score Formal PA | 11.32 ± 2.57 | 12.24 ± 3.10 | 1.869 | 0.063 | 11.44 ± 2.01 | 12.08 ± 3.03 | 0.560 | 0.576 |
| Score Informal PA | 2.82 ± 0.55 | 2.79 ± 0.56 | −0.316 | 0.752 | 2.79 ± 0.56 | 2.79 ± 0.38 | −0.685 | 0.494 |
| Score Total | 14.13 ± 2.86 | 15.05 ± 3.26 | 1.738 | 0.068 | 14.36 ± 2.22 | 14.82 ± 3.21 | 0.421 | 0.674 |
| Practical History | 7.42 ± 4.47 | 10.52 ± 5.69 | 3.393 | 0.001 * | 12.17 ± 5.98 | 9.52 ± 5.51 | −1.401 | 0.163 |
| Frequency of PA | 6.78 ± 3.12 | 8.69 ± 4.41 | 2.130 | 0.035 * | 8.64 ± 2.78 | 8.19 ± 4.29 | −0.272 | 0.786 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ashraf, S.; Viveiros, R.; França, C.; Ornelas, R.T.; Rodrigues, A. Association between Body Composition, Physical Activity Profile, and Occurrence of Knee and Foot Postural Alterations among Young Healthy Adults. Future 2024, 2, 16-29. https://doi.org/10.3390/future2010002
Ashraf S, Viveiros R, França C, Ornelas RT, Rodrigues A. Association between Body Composition, Physical Activity Profile, and Occurrence of Knee and Foot Postural Alterations among Young Healthy Adults. Future. 2024; 2(1):16-29. https://doi.org/10.3390/future2010002
Chicago/Turabian StyleAshraf, Sadaf, Roberto Viveiros, Cíntia França, Rui Trindade Ornelas, and Ana Rodrigues. 2024. "Association between Body Composition, Physical Activity Profile, and Occurrence of Knee and Foot Postural Alterations among Young Healthy Adults" Future 2, no. 1: 16-29. https://doi.org/10.3390/future2010002
APA StyleAshraf, S., Viveiros, R., França, C., Ornelas, R. T., & Rodrigues, A. (2024). Association between Body Composition, Physical Activity Profile, and Occurrence of Knee and Foot Postural Alterations among Young Healthy Adults. Future, 2(1), 16-29. https://doi.org/10.3390/future2010002