Characteristics and Demographics of Patients Younger than 50 with Atherosclerotic Cardiovascular Disease
Abstract
1. Introduction
2. Methods
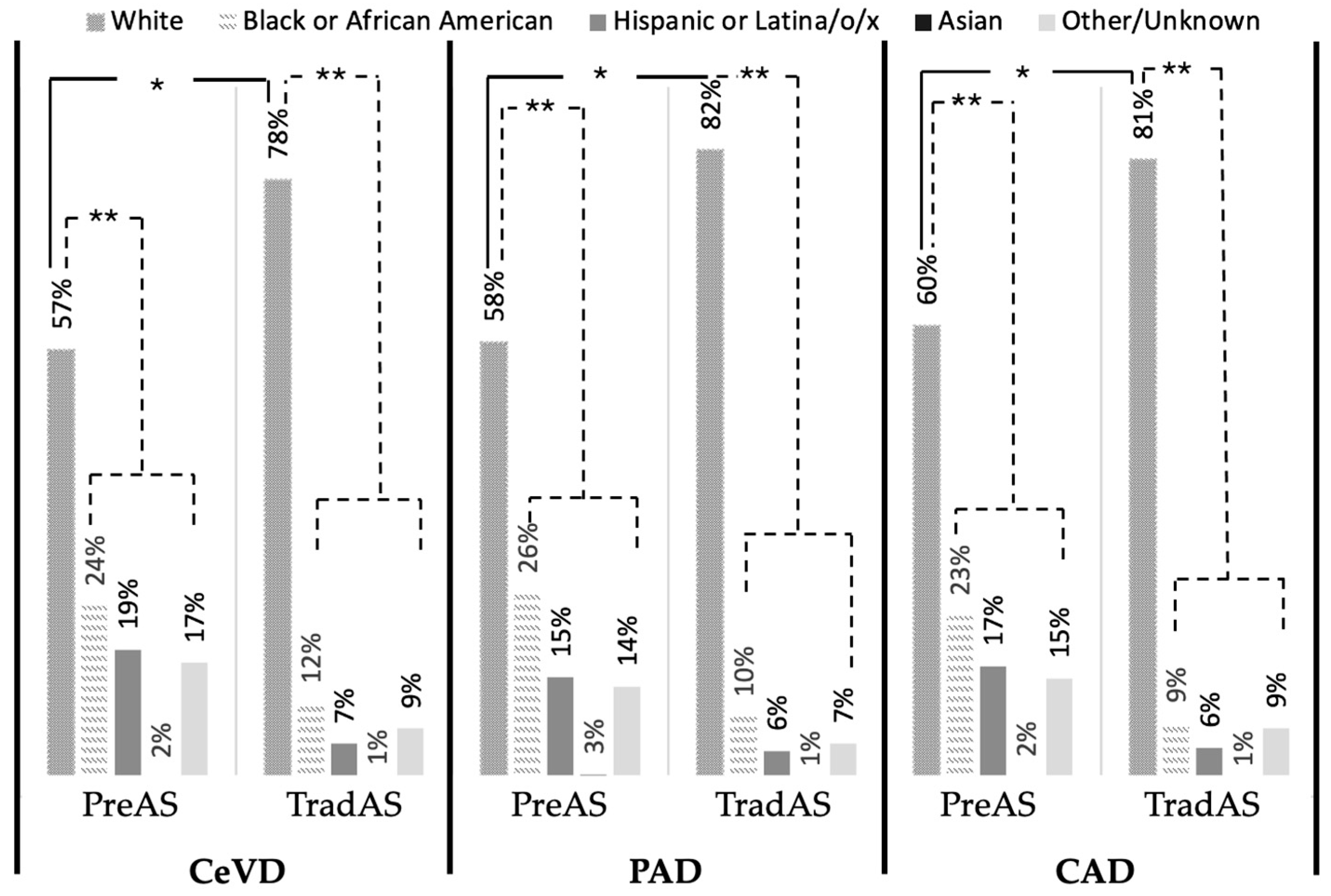
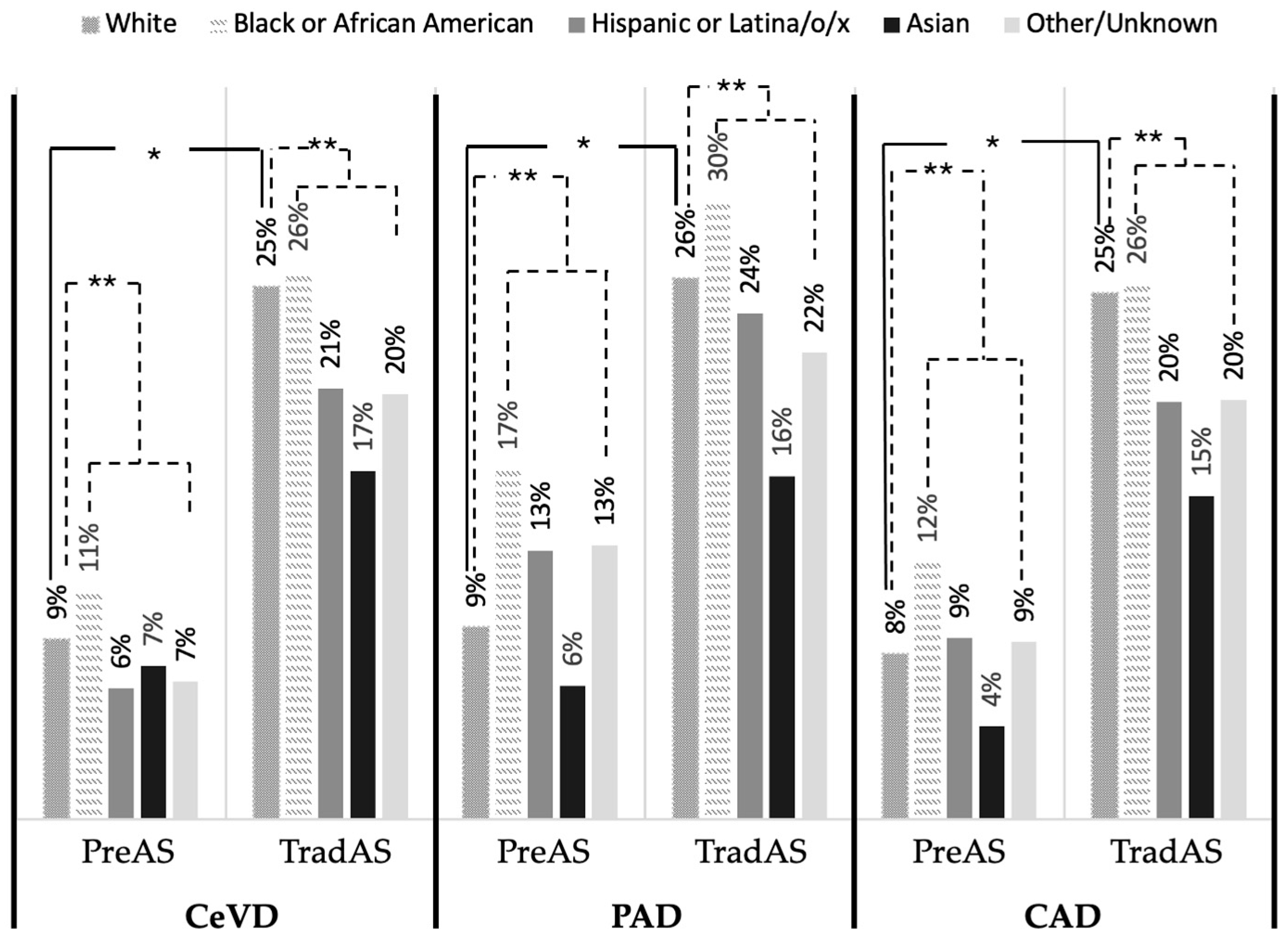
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jovin, D.G.; Sumpio, B.E.; Greif, D.M. Manifestations of human atherosclerosis across vascular beds. JVS Vasc. Insights 2024, 2, 100089. [Google Scholar] [CrossRef]
- Neifert, A.R.; Su, D.; Chaar, C.I.O.; Sumpio, B.E. Premature atherosclerosis: A review of current literature. JVS-Vasc. Insights Open Access Publ. Soc. Vasc. Surg. 2023, 1, 100013. [Google Scholar] [CrossRef]
- Libby, P. The changing landscape of atherosclerosis. Nature 2021, 592, 524–533. [Google Scholar] [CrossRef]
- Beller, J.; Bauersachs, J.; Schafer, A.; Schwettmann, L.; Heier, M.; Peters, A.; Meisinger, C.; Geyer, S. Diverging Trends in Age at First Myocardial Infarction: Evidence from Two German Population-Based Studies. Sci. Rep. 2020, 10, 9610. [Google Scholar] [CrossRef] [PubMed]
- Kim, I.; Kim, M.C.; Sim, D.S.; Hong, Y.J.; Kim, J.H.; Jeong, M.H.; Cho, J.G.; Park, J.C.; Seung, K.B.; Chang, K.; et al. Effect of the Metabolic Syndrome on Outcomes in Patients Aged <50 Years Versus >50 Years with Acute Myocardial Infarction. Am. J. Cardiol. 2018, 122, 192–198. [Google Scholar] [CrossRef] [PubMed]
- Arora, S.; Stouffer, G.A.; Kucharska-Newton, A.M.; Qamar, A.; Vaduganathan, M.; Pandey, A.; Porterfield, D.; Blankstein, R.; Rosamond, W.D.; Bhatt, D.L.; et al. Twenty Year Trends and Sex Differences in Young Adults Hospitalized With Acute Myocardial Infarction. Circulation 2019, 139, 1047–1056. [Google Scholar] [CrossRef]
- Gao, H.; Wang, Y.; Shen, A.; Chen, H.; Li, H. Acute Myocardial Infarction in Young Men Under 50 Years of Age: Clinical Characteristics, Treatment, and Long-Term Prognosis. Int. J. Gen. Med. 2021, 14, 9321–9331. [Google Scholar] [CrossRef]
- Vikulova, D.N.; Grubisic, M.; Zhao, Y.; Lynch, K.; Humphries, K.H.; Pimstone, S.N.; Brunham, L.R. Premature Atherosclerotic Cardiovascular Disease: Trends in Incidence, Risk Factors, and Sex-Related Differences, 2000 to 2016. J. Am. Heart Assoc. 2019, 8, e012178. [Google Scholar] [CrossRef]
- Mehta, A.; Dhindsa, D.S.; Hooda, A.; Nayak, A.; Massad, C.S.; Rao, B.; Makue, L.F.; Rajani, R.R.; Alabi, O.; Quyyumi, A.A.; et al. Premature atherosclerotic peripheral artery disease: An underrecognized and undertreated disorder with a rising global prevalence. Trends Cardiovasc. Med. 2021, 31, 351–358. [Google Scholar] [CrossRef]
- Allison, M.A.; Ho, E.; Denenberg, J.O.; Langer, R.D.; Newman, A.B.; Fabsitz, R.R.; Criqui, M.H. Ethnic-specific prevalence of peripheral arterial disease in the United States. Am. J. Prev. Med. 2007, 32, 328–333. [Google Scholar] [CrossRef]
- Wojcik-Cichy, K.; Koslinska-Berkan, E.; Piekarska, A. The influence of NAFLD on the risk of atherosclerosis and cardiovascular diseases. Clin. Exp. Hepatol. 2018, 4, 1–6. [Google Scholar] [CrossRef]
- Finney, A.C.; Das, S.; Kumar, D.; McKinney, M.P.; Cai, B.; Yurdagul, A., Jr.; Rom, O. The interplay between nonalcoholic fatty liver disease and atherosclerotic cardiovascular disease. Front. Cardiovasc. Med. 2023, 10, 1116861. [Google Scholar] [CrossRef]
- Arai, T.; Atsukawa, M.; Tsubota, A.; Kato, K.; Abe, H.; Ono, H.; Kawano, T.; Yoshida, Y.; Tanabe, T.; Okubo, T.; et al. Liver fibrosis is associated with carotid atherosclerosis in patients with liver biopsy-proven nonalcoholic fatty liver disease. Sci. Rep. 2021, 11, 15938. [Google Scholar] [CrossRef]
- Beckman, J.A.; Duncan, M.S.; Alcorn, C.W.; So-Armah, K.; Butt, A.A.; Goetz, M.B.; Tindle, H.A.; Sico, J.J.; Tracy, R.P.; Justice, A.C.; et al. Association of Human Immunodeficiency Virus Infection and Risk of Peripheral Artery Disease. Circulation 2018, 138, 255–265. [Google Scholar] [CrossRef]
- Haser, G.C.; Sumpio, B. Systemic and cell-specific mechanisms of vasculopathy induced by human immunodeficiency virus and highly active antiretroviral therapy. J. Vasc. Surg. 2017, 65, 849–859. [Google Scholar] [CrossRef]
- He, J.; Zhu, Z.; Bundy, J.D.; Dorans, K.S.; Chen, J.; Hamm, L.L. Trends in Cardiovascular Risk Factors in US Adults by Race and Ethnicity and Socioeconomic Status, 1999-2018. JAMA 2021, 326, 1286–1298. [Google Scholar] [CrossRef] [PubMed]
- Sidhu, G.S.; Ward, C.; Ferdinand, K.C. Racial disparity in atherosclerotic cardiovascular disease in hospitalized patients with diabetes 2005-2015: Potential warning signs for future U.S. public health. Am. J. Prev. Cardiol. 2020, 4, 100095. [Google Scholar] [CrossRef]
- Shah, N.S.; Ning, H.; Petito, L.C.; Kershaw, K.N.; Bancks, M.P.; Reis, J.P.; Rana, J.S.; Sidney, S.; Jacobs, D.R., Jr.; Kiefe, C.I.; et al. Associations of Clinical and Social Risk Factors With Racial Differences in Premature Cardiovascular Disease. Circulation 2022, 146, 201–210. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.U.; Lone, A.N.; Yedlapati, S.H.; Dani, S.S.; Khan, M.Z.; Watson, K.E.; Parwani, P.; Rodriguez, F.; Cainzos-Achirica, M.; Michos, E.D. Cardiovascular Disease Mortality Among Hispanic Versus Non-Hispanic White Adults in the United States, 1999 to 2018. J. Am. Heart Assoc. 2022, 11, e022857. [Google Scholar] [CrossRef]
- Volgman, A.S.; Palaniappan, L.S.; Aggarwal, N.T.; Gupta, M.; Khandelwal, A.; Krishnan, A.V.; Lichtman, J.H.; Mehta, L.S.; Patel, H.N.; Shah, K.S.; et al. Atherosclerotic Cardiovascular Disease in South Asians in the United States: Epidemiology, Risk Factors, and Treatments: A Scientific Statement From the American Heart Association. Circulation 2018, 138, e1–e34. [Google Scholar] [CrossRef] [PubMed]
- Curtin, S.C.; Arias, E. Mortality Trends by Race and Ethnicity Among Adults Aged 25 and over: United States, 2000–2017. NCHS Data Brief. 2019, 342, 1–8. [Google Scholar]
- Song, P.; Rudan, D.; Zhu, Y.; Fowkes, F.J.I.; Rahimi, K.; Fowkes, F.G.R.; Rudan, I. Global, regional, and national prevalence and risk factors for peripheral artery disease in 2015: An updated systematic review and analysis. Lancet Glob. Health 2019, 7, e1020–e1030. [Google Scholar] [CrossRef]
- Mendez, D.; Le, T.T.T.; Warner, K.E. Monitoring the Increase in the U.S. Smoking Cessation Rate and Its Implication for Future Smoking Prevalence. Nicotine Tob. Res. 2022, 24, 1727–1731. [Google Scholar] [CrossRef]
- Lee, Y.H.; Woods, C.; Shelley, M.; Arndt, S.; Liu, C.T.; Chang, Y.C. Racial and Ethnic Disparities and Prevalence in Prescription Drug Misuse, Illicit Drug Use, and Combination of Both Behaviors in the United States. Int. J. Ment. Health Addict. 2023, 22, 3818–3834. [Google Scholar] [CrossRef]
- Scott, M.L.; Murnane, K.S.; Orr, A.W. Young at heart? Drugs of abuse cause early-onset cardiovascular disease in the young. Heart 2021, 107, 604–606. [Google Scholar] [CrossRef] [PubMed]
- Gan, W.Q.; Buxton, J.A.; Scheuermeyer, F.X.; Palis, H.; Zhao, B.; Desai, R.; Janjua, N.Z.; Slaunwhite, A.K. Risk of cardiovascular diseases in relation to substance use disorders. Drug Alcohol Depend. 2021, 229 Pt A, 109132. [Google Scholar] [CrossRef] [PubMed]
- 2020 Census Data Products. Demographic and Housing Characteristics File. In Proceedings of the Workshop; The National Academies Press: Washington, DC, USA, 2020. [Google Scholar]
- Laurent, S.; Pierre, B.; Pedro, G.; Lacolley, P.; Nilsson, P.M. Concept of Extremes in Vascular Aging: From Early Vascular Aging to Supernormal Vascular Aging. Hypertension 2019, 74, 218–228. [Google Scholar] [CrossRef] [PubMed]

| Total | PreAS (≤50 y/o) | TradAS (>50 y/o) | Cohen’s h-Value | |
|---|---|---|---|---|
| Demographics | ||||
| Total number of patients | 136,328 | 17,008 | 119,320 | |
| Percent of total patients * | 100% | 12.5% | 87.5% | −1.70 |
| Male * | 54.1% | 50.8% | 54.6% | −0.08 |
| Female * | 45.9% | 49.2% | 45.4% | 0.08 |
| Mortality Rate * | 21.0% | 8.2% | 22.8% | −0.41 |
| Age at Diag Mean/Median | 67/68 | 40/42 | 70/70 | |
| Age Std Dev/Interq Range | 13.7/58–76 | 8.0/35–47 | 11.2/62–79 | |
| Comorbidities | ||||
| CAD * | 61.0% | 42.4% | 63.6% | −0.43 |
| PAD * | 38.4% | 27.6% | 39.9% | −0.26 |
| CeVD * | 45.2% | 46.6% | 45.0% | 0.03 |
| Atrial fibrillation * | 26.3% | 9.1% | 28.7% | −0.52 |
| Chronic Heart Failure * | 34.8% | 22.5% | 36.6% | −0.31 |
| Chronic Kidney Disease * | 24.9% | 15.4% | 26.3% | −0.27 |
| Dementia * | 12.8% | 1.4% | 14.4% | −0.54 |
| Diabetes * | 33.9% | 28.5% | 34.7% | −0.13 |
| HIV * | 1.0% | 1.7% | 0.9% | 0.07 |
| Hyperlipidemia * | 65.1% | 45.4% | 67.9% | −0.46 |
| Hypertension * | 83.2% | 63.4% | 86.0% | −0.53 |
| Liver Disease * | 16.3% | 19.0% | 15.9% | 0.08 |
| MI * | 27.4% | 24.9% | 27.8% | −0.07 |
| Malignancy * | 30.1% | 11.9% | 32.7% | −0.51 |
| Pulmonary Disease * | 36.8% | 32.2% | 37.4% | −0.11 |
| Rheumatological Disease + | 6.9% | 6.5% | 7.0% | −0.02 |
| Race and Ethnicity | PreAS | TradAS | Cohen’s h-Value |
|---|---|---|---|
| White *# | 59.0% | 79.9% | 1.26 |
| Black or African American *# | 22.4% | 9.5% | −0.11 |
| Hispanic or Latina/o/x *# | 17.2% | 6.2% | −0.17 |
| Asian *# | 2.8% | 1.5% | 0.02 |
| Race Other *# | 15.3% | 8.9% | 0.09 |
| Tobacco Use | Substance Use | |||||
|---|---|---|---|---|---|---|
| PreAs | TradAS | Cohen’s h-Value | PreAS | TradAS | Cohen’s h-Value | |
| Total | 50.2% | 58.2% | −0.16 * | 14.8% | 4.3% | 0.37 * |
| Male | 55.2% | 63.9% | −0.18 * | 17.8% | 5.4% | 0.40 * |
| Female | 45.1% | 51.3% | −0.12 * | 11.6% | 3.1% | 0.34 * |
| White | 50.7% | 59.6% | −0.18 * | 13.2% | 3.9% | 0.35 * |
| Black or African American | 53.7% | 59.2% | −0.11 * | 22.7% | 9.6% | 0.36 * |
| Hispanic or Latina/o/x | 49.8% | 50.7% | −0.02 * | 14.1% | 4.7% | 0.33 * |
| Asian | 29.9% | 31.3% | −0.03 * | 2.4% | 0.6% | 0.16 * |
| Race other | 47.2% | 50.3% | −0.06 * | 11.7% | 3.7% | 0.31 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neifert, A.R.; Su, D.; Sumpio, B.E. Characteristics and Demographics of Patients Younger than 50 with Atherosclerotic Cardiovascular Disease. J. Vasc. Dis. 2025, 4, 31. https://doi.org/10.3390/jvd4030031
Neifert AR, Su D, Sumpio BE. Characteristics and Demographics of Patients Younger than 50 with Atherosclerotic Cardiovascular Disease. Journal of Vascular Diseases. 2025; 4(3):31. https://doi.org/10.3390/jvd4030031
Chicago/Turabian StyleNeifert, Alexander R., David Su, and Bauer E. Sumpio. 2025. "Characteristics and Demographics of Patients Younger than 50 with Atherosclerotic Cardiovascular Disease" Journal of Vascular Diseases 4, no. 3: 31. https://doi.org/10.3390/jvd4030031
APA StyleNeifert, A. R., Su, D., & Sumpio, B. E. (2025). Characteristics and Demographics of Patients Younger than 50 with Atherosclerotic Cardiovascular Disease. Journal of Vascular Diseases, 4(3), 31. https://doi.org/10.3390/jvd4030031






