Abstract
The purpose of this study is to compare IVC Celect and ALN filters in regard to their efficacy, retrievability, and one-year follow-up after retrieval. Materials and Methods: This is a prospective randomized study, conducted in three centers between April 2020 and May 2021. A total of 115 participants were randomized, of which 15 participants were excluded for various reasons. Each group of 50 participants was finally assigned a type of filter (Celect n = 50 and ALN = 50). Tilt angles at placement and retrieval, rates of overall filter retrieval, complications, complex retrieval, and clinical follow-up at 12 months were compared. Results: One hundred participants (59 men and 41 women) were included. The mean age was 62.4 ± 13.3, with no significant differences between both groups (p 0.503). The mean of dwelling time was 44.7 ± 93 days. (p 0.520) Filter retrieval was successful in all participants (100%). The main complication in CT prior to removal was tilt >15° (31%) and filter tip embedment (16%). No significant differences were observed in the type of retrieval (standard or complex) between both filters (p 0.24); however, fluoroscopy time was significantly longer in the complex removal of the Celect filter: 29.1 ± 12 min vs. 17.5 ± 10.3 (p 0.005). After one year, no recurrent pulmonary embolism was observed in both types of filters. Conclusions: The ALN filter had a significantly lower rate of tip and filter tip embedding, with no differences in complexity or removal success rate. There were significant differences in the fluoroscopy time consumed for standard and complex retrievals between both filters, with less time for the ALN filter.
1. Introduction
Venous thromboembolic disease (VTD) includes deep vein thrombosis (DVP) and pulmonary embolism (PE). VTE is a serious disease that affects 1–2 per 1000 European citizens [1]. The treatment of choice in VTD is systemic anticoagulant therapy that includes: heparin, low-weight heparins, warfarin, acenocoumarin, and the new oral anticoagulants [2]. When anticoagulation fails, resulting in complications such as bleeding, or where it is contraindicated, most clinical guidelines recommend implanting an inferior vena cava filter (IVCF) [3,4,5].
Inferior vena cava filters can be permanent or temporary and recoverable. Currently, temporary and retrievable filter devices placed in the inferior vena cava are generally used [6,7,8].
It has been found that the vast majority of existing filters on the market have a similar efficiency. However, there are no comparative studies between different filters that provide this clinical evidence. All types of filters can cause complications: IVC stenosis and obstruction, recurrent DVT, filter fracture, migration, and penetration of the struts or hooks into the wall [9]. Due to these complications reported in the MAUDE (Manufacturer and User Facility Device Experience of the FDA), since 2010 the FDA [10,11] has warned of the need to withdraw IVCFs between 29 and 54 days after implantation once they are no longer clinically necessary.
There are few controlled prospective studies with limited clinical evidence regarding the efficacy and safety of retrievable filters [9].
There are several models of recoverable filters on the market that are supposed to have the same safety in handling and similar recoverability; however, there are few studies that compare the main characteristics of IVCFs [12,13].
The main objective of this study was to compare two IVCFs available in our centers. For this purpose, a randomized study of the Celect and ALN filters was carried out in relation to efficacy at twelve months, safety (major complications), and filter recoverability.
2. Materials and Methods
2.1. IVCF Indication
According to the inclusion and exclusion criteria, following the recommendations of the guidelines (SIR and SIDI), all the indications were grouped into three main types of indication [14]: 1. Contraindication for anticoagulation. 2. Prevention of high risk of pulmonary embolism. 3. Recurrence of PE despite correct anticoagulation.
2.2. Study Design
This is a prospective randomized study carried out in three centers center between April 2020 and May 2021. The study was approved by the Research Ethics Committee of Aragon (CEICA (EC21/012). All participants signed the corresponding informed consent. The inclusion criteria were patients over 18 years of age with an indication for IVCF, in accordance with the guidelines approved by the following societies: Society of Interventional Radiology (SIR), Spanish Society of Vascular and Interventional Radiology (SERVEI) and Ibero-American Society of Interventionism (SIDI) [4,5]. Both the inclusion and exclusion criteria can be seen in Table 1. The study participants were followed up in the interventional outpatient clinic and the device was scheduled to be withdrawn 30 days after implantation [15].

Table 1.
Baseline participant characteristics and filter release. BMI: body mass index, IVC: inferior vena cava, PE: pulmonary embolism, AC: anticoagulation.
2.3. Randomization and Blinding
The patients were enrolled in the study when they had a temporary filter indication accepted by our group, following the SIDI-SERVEI and SIR guidelines. The team epidemiologist generated a random allocation sequence using Research Randomizer version 4.0 [16] and a research collaborator assigned eligible patients to the ALN or Celect group.
All patients were blinded to the device used. The performing radiologists were not blinded, but the interventional radiologists performing the clinical follow-up were blinded to group allocation. The Consolidated Standards of Reporting Trials (CONSORT) flow diagram shows the randomization and flow of participant evaluations throughout the trial, given in Figure 1.
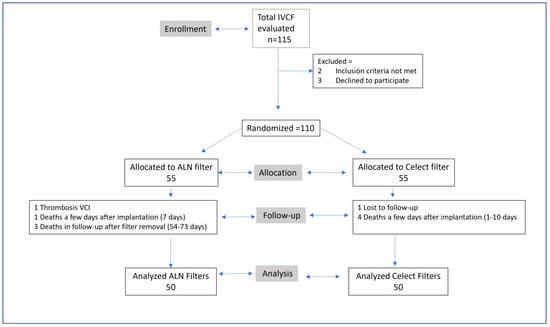
Figure 1.
Consolidated standards of reporting trials diagram.
2.4. Sample Size
Assuming that both filters are equally effective in preventing thrombus embolization and based on the experience of the research [14,17], the primary outcome (i.e., clinical success) was not used to calculate the sample size. Instead, sample size was determined by computer software [18] (G*Power 3.1; Universität Kiel, Kiel, Germany) using fluoroscopy time regarding filter retrieval for ALN filters [18] and Celect filters [19], comparing the mean total procedure time for both methods (16 min ± 9 min vs. 4.25 min ± 13.38). To detect the above-mentioned differences with an α error of 0.05 and 80% power using a 2-sided test, a total of 27 patients were considered in each group.
2.5. Filter Placement
All filters were implanted with right jugular access. Once in the jugular vein, through a 5 Fr and 10 cm introducer sheath (Radiofocus Introducer II Standard Terumo, Japan) a 0.035″ Teflon-coated guidewire was passed. A pig-tail catheter with distal holes of 5 Fr and 90 cm long (UHF Merit USA) was passed through this. A cavograph was performed to determine its permeability and the height of the renal veins. The filter was implanted 2–4 cm below the renal veins. Two types of filters were used.
The Celect IVC is constructed of cobalt alloy with platinum markings; it measures 30 × 49 mm and passes through a 7 Fr catheter. It is a modification of the Gunther Tulip filter (Cook IN Medical Bloomington USA), compatible with MR, that was introduced for potentially retrievable use in March 2008 and has a conical shape with four primary struts and eight short secondary struts. It is manufactured by Cook Medical (Bloomington, IN, USA). The ALN filter is made of stainless steel and is non-ferromagnetic. It was approved by the FDA for use as a retrievable filter in 2008, it has 6 anchoring struts and 3 stabilization struts. It measures 59 × 30 mm. It passes through a 7 Fr catheter. It is manufactured by ALN Implants, Chirurgicaux Borme les Mimosas, France; imaged in Figure 2 and Figure 3.
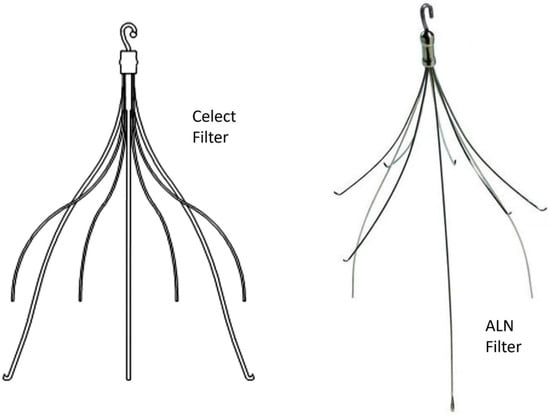
Figure 2.
Types of filters compared in the trial.
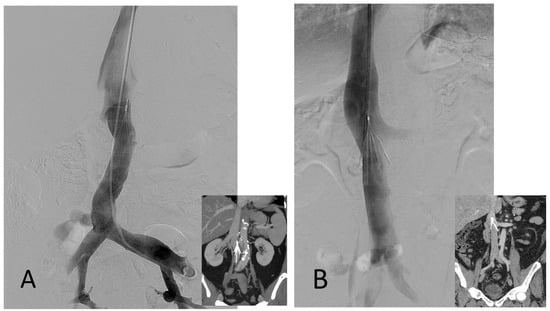
Figure 3.
(A) ALN filter, cavography with the filter and CT coronal view. (B) Celect filter cavography and CT coronal view.
2.6. Filter Retrieval
In all cases, prior to IVCF retrieval, a CT angiography of the chest and abdomen was performed to assess the evolution of the pulmonary embolism and the location, morphology, and possible thrombosis of the filter or in the IVC.
IVCF recovery was performed in the interventional operating room, using aseptic measures, and always through the right jugular vein. Through a 5 Fr introducer, cavography was performed with a 5 Fr pig-tail catheter (UHF Merit USA).
Attempts were made to initially remove all IVCF with the same type of recovery system (filter removal set, Cook Medical, Bloomington, IN, USA). For this purpose, the 11 Fr sheath included in the standard removal set (Cook Medical) was passed over the guide and the retrieval loop was passed coaxially to the sheath. In cases where it was impossible to remove the IVCF, the attempt was repeated with a new device or a different strategy (e.g., using simultaneous jugular and femoral access, balloons, loops, or forceps). After 3 failed attempts, it was left as a permanent IVCF and the patient was kept anticoagulated.
2.7. Outcome Measures
The complexity of filter recovery was the primary endpoint of the study. Complex recovery was defined as that in which a technique or device other than the standard had to be used (11 Fr loop and sheath). Other secondary endpoints were the complications observed in the imaging studies: filter tilt, migration, filter fracture, and significant intrafilter thrombosis. The recurrence of PE during the filter indwelling time and the IVCF indwelling time were studied. According to Kleedehn M et al. [20], we do not consider the penetration of the legs (>3 mm into the wall), an inclination of less than 15°, nor migration as a cause of complexity to remove the IVCF. However, it is considered as a cause of increased complexity when there is an inclination >15° with fixation of the hook to the wall of the IVC, as well as the time of permanence of the IVCF.
In cases of large intrafilter thrombus or vein thrombosis, both the guidelines and various authors recommend thrombolysis [15,16]. Subjective difficulty felt by the operator was assessed and classified into five grades based on the time of inverted fluoroscopy or filter removal: No difficulty (IVCF removed in less than 10 min); Medium difficulty (IVCF withdrawn between 10 and 25 min); Quite difficult (recovered between 25 and 50 min using special maneuvers); Difficult (IVCF removed in more than 50 min with special maneuvers); Impossible (IVCF Could not be recovered).
2.8. Statistical Analysis
Statistical analysis was performed using SPSS software (version 28; IBM, Armonk, NY, USA). Continuous variables were described as mean ± standard deviation and compared using the Student’s t-test. Categorical variables were described as frequencies and percentages, and were compared using chi-square or Fisher’s exact tests. All analyses were by intention to treat; p values < 0.05 indicated statistical significance.
3. Results
Of the 115 recruited patients, 15 were excluded for various reasons (See Figure 1). Of these, 69 (59%) were men and 41 (41%) were women (See Table 2).

Table 2.
Inclusion and exclusion criteria. VTD: venous thrombosis disease, AC: anticoagulation, PE: pulmonary embolism, IVCF: inferior vena cava filter.
Of the 115 participants initially recruited, five were excluded, two did not meet the inclusion criteria, and three refused to participate in the trial. One hundred and ten participants were randomized, 55 to each filter arm (55 to the Celect filter arm and 55 to the ALN filter arm). In the Celect filter arm, one participant, a 71-year-old man with metastatic neoplasm, without anticoagulation, presented with thrombosis of the inferior vena cava and both iliac veins 20 days after implantation and refused recanalization treatment. One patient died a few days after filter implantation by respiratory insufficiency (seven days) and three died of their underlying disease (two COVID and one neoplasm) between 54 and 74 days. In the ALN filter arm, five participants were also excluded: one was lost to follow-up after filter implantation, and four died of complications of their pulmonary embolism early on (between days 1 and 10 after filter implantation). A total of one hundred participants (59 men and 41 women) with a mean BMI of 27.6 ± 5.2 (range 21.3–39.2) were definitively included in the trial. The mean age was 62.4 ± 13.3 (range: 29–87 years old), with no significant differences between both groups (p 0.503). The indications for IVCF implantation were: 1. Contraindication for anticoagulation (recent bleeding, recent surgery, recent stroke). 2. Prevention of high risk of pulmonary embolism (patients with poor respiratory reserve and massive pulmonary embolism, large floating thrombus in iliac vein or vena cava). 3. Recurrence of pulmonary embolism despite correct anticoagulation. Table 2 shows the percentages of each of the indications for both filters. No significant differences were observed. The areas of the vena cava were similar in the filter types (433 ± 190 mm2 and 377.9 ± 150 mm2, respectively (p 0.945)). There were also no significant differences in IVC pressures after IVCF implantation, both at baseline and with the Valsalva maneuver.
Deep vein thrombosis of one of the lower extremity segments was found in 83% of all patients. There were no significant differences in both arms of the study (p 0.599).
Fluoroscopy performed immediately after IVCF implantation did not show significant differences in centering and tilting of the filters (p 0.538 (see Table 3). Filter repositioning was necessary in the same intervention on nine (18%) occasions with the Celect filter and seven (14%) with the ALN (p 0.424). There were no significant differences in fluoroscopy time in the implantation of both filters (Celect filter 9.9 ± 1.1 min vs. ALN filter 7.8 ± 4.3 min) (p 0.380).

Table 3.
Filter retrieval data and some results.
Filter recovery was generally scheduled for 30–35 days after implantation [15]. However, there were cases in which the recovery of the filter was delayed for medical or patient reasons. There was no significant difference in filter recovery time between both groups. Whenever possible, when there was no contraindication for anticoagulation, the patients remained anticoagulated with low molecular weight heparin or dicumarin at therapeutic doses. Ninety six percent of all patients were on anticoagulation at the time of filter removal, with no significant difference between both groups (37.4 ± 11 vs. 34.4 ± 5.2) (p 0.453).
All patients underwent abdominal and chest CT to assess the filter and the evolution of PE. There were significant differences between both groups in the inclination of the filter, 42% vs. 24% (p 0.05), in the apposition of the hook-tip to the wall of the CV, 24% vs. 8% (p 0.02), but there were no significant differences in the penetration of the struts into the wall of the IVC, 14% vs. 8% (p 0.338).
Small intrafilter thrombi were seen in three participants and were adhered to the IVC wall in two cases. In all cases, they were resolved with aspiration prior to filter removal using a 14–16 Fr sheath introducer without complications.
There was no significant difference in the type of filter retrieval, standard and complex, 82% vs. 18% and 90% vs. 14%, respectively (p 0.249). Regarding fluoroscopy time, there were very significant differences when the standard technique was used (p 0.006), but they were not as significant with the complex technique (p 0.095).
In all cases, it was possible to recover the filter. There were significant differences in the subjective degree of difficulty in recovery; a simpler result was found with the ALN filter (p 0.047).
In the Celect filter group, a re-embolism was found that occurred at seven months. There was no re-embolism in the ALN group. Regarding post-thrombotic syndrome, the incidence was similar in both groups, being mild or moderate in all cases (p 0.836).
4. Discussion
Despite the FDA recommendation [11] to remove IVC filters as soon as possible in patients who no longer clinically need them, few IVC filters are removed. In a systematic review of 103 articles [7] from 1984 to 2016, 10 different IVCF models were identified in 20,319 patients. The authors found that two-thirds of implanted retrievable filters were not removed, despite the fact that more than 85% of them were initially implanted with intent to remove. Different reasons for remaining permanent were observed: primary indication as permanent, deaths, need for protection in ongoing PE, and technical impossibility of recovering the filter. In a total of 7820 IVCFs (38.4%), withdrawal was attempted, achieving technical success in 7095 patients (90.7%). In a study of 725 patients (9.2%) with IVCFs, the filter could not be removed due to technical difficulties. Technical success in IVCF withdrawal is estimated to be 84–100% [14,19,20]. In general, IVCF recovery is simple [6,17,21,22]. he main reasons that make filter removal difficult are tilting >15° of the filter at the time of removal and apposition of the removal hook to the IVC wall [23]. Some authors also stated IVCF dwelling time as a cause of recovery difficulty. However, there are studies, such as Desai KR et al. [24], comparing the technical success of removal in patients with more than or less than six months of filter permanence that have not observed significant differences (94% versus 97% technical success, respectively) based on these difficulties. Kleedehn M et al. [21] established two types of IVC filter removal: standard and complex. In the present series, in 84 participants (84%) recovery of IVCF was standard; while the remaining 16%, despite differences in degree of difficulty, fluoroscopy time, radiation dose, and device cost (between standard and complex recovery types), the procedure’s technical success rate in recovery is similar in the two types of recovery [21,25]. There are no significant differences published between the different types of filters in terms of their recoverability. In the systematic review by Liu J et al. [26], conducted on 80 original studies (11,413 patients) between 2003 and 2019, no significant differences were observed in the six types of IVCF compared (ALN, Celect, Gunther Tulip, Denali, Crux, and Option). The authors observed an overall recoverability of 98.4–100%, with less than 2% occurrence of complications. Another non-randomized study [27] has compared the Denali, Option, and Gunther Tulip filters in a single center, concluding that the Denali and Gunther Tulip filters are easier to remove than the Option. In this study, removal of the Denali filter required less fluoroscopy time and less complex techniques than the other two filters. However, there are few prospective randomized studies comparing particular filters [12,13]. There are two randomized studies comparing two filters (Denali and Option with Celect). The reason for selecting the Celect filter may be that this filter is the most used and for which there are more bibliographic references [6,8,14,17].
There is agreement that the degree of tilt of the filter (>15°) and the penetration of the hook of the tip into the wall of the inferior vena cava are the most important factors when considering the complexity of IVCF recovery. In the present series, both filters (Celect and ALN) presented a tilt greater than 15° at the time of recovery in 38% and 24% of cases, respectively. The tilt of the filter is an important factor, since the tilt can lead to the contact of the tip with the wall of the IVC more easily with the consequence of a greater risk of embedment of the tip in the wall.
While the filter tip embedment was 24% with the Celect filter, it was 4% with the ALN. The presence of the two findings (tilt and embedment) in the CT prior to removal determined that 76% of both filters required complex removal when there was only one complication (tilt or embedment). Removal was complex for 35% (tilt) and 41% (embedment). The subjective sensation of difficulty did not present significant differences in the two filters, with no difficulty in 77% and 86%, respectively. However, despite the differences in the findings of complications on CT, and the degree of complexity in the removal of both types of filters, technical success was 100%.
Kuo WT [28] et al., have reported 500 patients with embedded vena cava filters in which classical removal methods had failed and the filters were removed using laser assistance.
Based on our experience [15] in this study, it was established that without contraindication the IVCF was removed between days 30 and 40 post implantation
During the dwelling time of filter, no re-embolism was observed in any case. This coincides with results published in the literature (>2.5%) [9,17]. Once the filter was removed, one case of re-embolism was observed in the Celect arm at 7 months. Mild or moderate post-thrombotic syndrome was observed in both arms (Celect and ALN)
The main limitations of the study are that it is from a single center and the number of participants is not very large, although it is sufficient to establish clinical significance.
The conclusions of the study are that the ALN filter presented in our study shows a significantly lower rate of inclination and filter tip embedment, without differences in the complexity or in the rate of success in the removal of the filter. There were significant differences in the fluoroscopy time consumed for standard and complex removals between both filters, with less time for the ALN filter.
Author Contributions
Conception and design: M.A.D.G., S.M. and J.A.G., Analysis and interpretation: M.A.D.G., J.A.G., J.J.C.-D., S.M., J.M.A., J.U., C.B. and J.R., Data collection: J.R., C.S.-C., R.B. and A.F. Writing the article: M.A.D.G. and R.B., Critical revision of the article: J.A.G., J.J.C.-D., J.U., J.M.A., S.M. and J.R., Final approval of the article: M.A.D.G. and J.A.G., Statistical analysis: J.A.G., R.B. and S.R. Overall responsibility: M.A.D.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical Committee of the Government of Aragon approved C.P.—I.C. EC21/012.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The authors of this research declare that the data supporting this investigation are available in the database of the Interventional Radiology Service of the hospitals involved.
Conflicts of Interest
The authors of this research declare that they have no conflict of interest and do not receive help from any commercial company.
Abbreviations
| IVC | Inferior vena cava |
| VTD | Venous thromboembolic disease |
| DVT | Deep vein thrombosis |
| PE | Pulmonary embolism |
| AC | Anticoagulants |
| IVCF | Inferior vena cava filter |
| SIR | Society of Interventional Radiology |
| SIDI | Ibero-American Society of Interventionism |
| SERVEI | Spanish Society of Vascular and Interventional Radiology |
References
- Monreal, M.; Mahé, I.; Bura-Riviere, A.; Prandoni, P.; Verhamme, P.; Brenner, B.; Wells, P.S.; Di Micco, P.; Bertoletti, L. Pulmonary embolism: Epidemiology and registries. Presse Med. 2015, 44, e377–e383. [Google Scholar] [CrossRef] [PubMed]
- Pattullo, C.S.; Barras, M.; Tai, B.; Mckean, M.; Donovan, P. New oral anticoagulants: Appropriateness of prescribing in real-world setting. Intern. Med. J. 2016, 46, 812–818. [Google Scholar] [CrossRef] [PubMed]
- Konstantinides, S.V.; Meyer, G. The 2019 ESC Guidelines on the Diagnosis and Management of Acute Pulmonary Embolism. Eur. Heart J. 2019, 40, 3453–3455. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, J.A.; Barnes, G.D.; Chaer, R.A.; Cuschieri, J.; Eberhardt, R.T.; Johnson, M.S.; Kuo, W.T.; Murin, S.; Patel, S.; Rajasekhar, A.; et al. Society of Interventional Radiology Clinical Practice Guideline for Inferior Vena Cava Filters in the Treatment of Patients with Venous Thromboembolic Disease: Developed in collaboration with the American College of Cardiology, American College of Chest Phy-sicians, American College of Surgeons Committee on Trauma, American Heart Association, Society for Vascular Surgery, and Society for Vascular Medicine. J. Vasc. Interv. Radiol. 2020, 31, 1529–1544. [Google Scholar]
- De Gregorio, M.A.; Guirola, J.A.; Sierre, S.; Urbano, J.; Ciampi-Dopazo, J.J.; Abadal, J.M.; Pulido, J.; Eyheremendy, E.; Lonjedo, E.; Guerrero, G.; et al. Ibero-American Society of Interventionism (SIDI) and the Spanish Society of Vascular and Interventional Radiology (SERVEI) Standard of Practice (SOP) for the Management of Inferior Vena Cava Filters in the Treatment of Acute Venous Thromboembolism. J. Clin. Med. 2021, 11, 77. [Google Scholar] [CrossRef]
- Lee, M.J.; Valenti, D.; De Gregorio, M.A.; Minocha, J.; Rimon, U.; Pellerin, O. The CIRSE Retrievable IVC Filter Registry: Retrieval Success Rates in Practice. Cardiovasc. Interv. Radiol. 2015, 38, 1502–1507. [Google Scholar] [CrossRef]
- Jia, Z.; Fuller, T.A.; McKinney, J.M.; Paz-Fumagalli, R.; Frey, G.T.; Sella, D.M.; Van Ha, T.; Wang, W. Utility of Re-trievable Inferior Vena Cava Filters: A Systematic Literature Review and Analysis of the Reasons for Nonretrieval of Filters with Temporary Indications. Cardiovasc. Interv. Radiol. 2018, 41, 675–682. [Google Scholar]
- Uberoi, R.; Tapping, C.R.; Chalmers, N.; Allgar, V. British Society of Interventional Radiology (BSIR) Inferior Vena Cava (IVC) Filter Registry. Cardiovasc. Interv. Radiol. 2013, 36, 1548–1561. [Google Scholar] [CrossRef]
- Bikdeli, B.; Jiménez, D.; Kirtane, A.J.; Bracken, M.B.; Spencer, F.A.; Monreal, M.; Krumholz, H.M. Systematic re-view of efficacy and safety of retrievable inferior vena caval filters. Thromb. Res. 2018, 165, 79–82. [Google Scholar] [CrossRef]
- Morales, J.P.; Li, X.; Irony, T.Z.; Ibrahim, N.G.; Moynahan, M.; Cavanaugh, K.J. Decision analysis of retrievable inferior vena cava filters in patients without pulmonary embolism. J. Vasc. Surg. Venous Lymphat. Disord. 2013, 1, 376–384. [Google Scholar] [CrossRef]
- United States Food and Drug Administration. Alerts and Notices (Medical Devices) Removing Retrieva-Ble Inferior Vena Cava Filters: Initial Communication. Available online: http://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm221676.htm (accessed on 24 August 2022).
- Ryu, R.K.; Desai, K.; Karp, J.; Gupta, R.; Evans, A.E.; Rajeswaran, S.; Salem, R.; Lewandowski, R.J. A comparison of retrievability: Celect versus Option filter. J. Vasc. Interv. Radiol. 2015, 26, 865–869. [Google Scholar] [CrossRef] [PubMed]
- Han, K.; Kim, M.-D.; Kim, G.M.; Kwon, J.H.; Lee, J.; Won, J.Y.; Moon, S.; An, H. Comparison of Retrievability and Indwelling Complications of Celect and Denali Infrarenal Vena Cava Filters: A Randomized, Controlled Trial. Cardiovasc. Interv. Radiol. 2021, 44, 1536–1542. [Google Scholar] [CrossRef]
- De Gregorio, M.A.; Guirola, J.A.; Serrano, C.; Figueredo, A.; Kuo, W.T.; Quezada, C.A.; Jimenez, D. Success in Optional Vena Cava Filter Retrieval. An Analysis of 246 Patients. Arch. Bronconeumol. 2018, 54, 371–377. [Google Scholar] [CrossRef]
- De Gregorio, M.A.; Gamboa, P.; Bonilla, D.L.; Sanchez, M.; Higuera, M.T.; Medrano, J.; Mainar, A.; Lostalé, F.; Laborda, A. Retrieval of Gunther Tulip optional vena cava filters 30 days after implantation: A prospective clinical study. J. Vasc. Interv. Radiol. 2006, 17, 1781–1789. [Google Scholar] [CrossRef]
- Urbaniak, G.C.; Plous, S. Research Randomizer (Version 4.0). 2013. Available online: http://www.randomizer.org/ (accessed on 21 September 2021).
- De Gregorio, M.A.; Guirola, J.A.; Urbano, J.; Díaz-Lorenzo, I.; Muñoz, J.J.; Villacastin, E.; Lopez-Medina, A.; Fi-gueredo, A.L.; Guerrero, J.; Sierre, S.; et al. Spanish multicenter real—Life registry of retrievable vena cava filters (REFiVeC). CVIR Endovasc. 2020, 3, 26. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Pellerin, O.; Barral, F.G.; Lions, C.; Novelli, L.; Beregi, J.P.; Sapoval, M. Early and late retrieval of the ALN re-movable vena cava filter: Results from a multicenter study. Cardiovasc. Interv. Radiol. 2008, 31, 889–896. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.E.; Van Allan, R.J.; Friedman, M.L.; Lipshutz, H.G. Complications and retrieval characteristics of Celect Platinum inferior vena cava filters. J. Vasc. Surg. Venous Lymphat. Disord. 2018, 6, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Kleedehn, M.; Moore, K.; Longo, K.; Woo, K.; Laeseke, P. An analysis of factors associated with increased fluoroscopy time or the need for complex techniques at IVC filter retrieval. Eur. Radiol. 2019, 29, 1931–1938. [Google Scholar] [CrossRef]
- Dinglasan, L.A.V.; Oh, J.C.; Schmitt, J.; Trerotola, S.O.; Shlansky-Goldberg, R.; Stavropoulos, S.W. Complicated Inferior Vena Cava Filter Retrievals: Associated Factors Identified at Preretrieval CT. Radiology 2013, 266, 347–354. [Google Scholar] [CrossRef]
- Kuyumcu, G.; Walker, T.G. Inferior vena cava filter retrievals, standard and novel techniques. Cardiovasc. Diagn. Ther. 2016, 6, 642–650. [Google Scholar] [CrossRef] [PubMed]
- Desai, K.R.; Lewandowski, R.J.; Salem, R.; Mouli, S.K.; Karp, J.K.; Laws, J.L.; Ryu, R.K. Retrieval of Inferior Vena Cava Filters With Prolonged Dwell Time: A Single-Center Experience in 648 Retrieval Procedures. JAMA Intern. Med. 2015, 175, 1572–1574. [Google Scholar] [CrossRef]
- Merritt, T.; Powell, C.; Hansmann, J. Safety and Effectiveness of Advanced Retrieval Techniques for Inferior Vena Cava Filters Compared with Standard Retrieval Techniques: A Systematic Review of the Literature and Meta-Analysis. J. Vasc. Interv. Radiol. 2022, 33, 564–571.e4. [Google Scholar] [CrossRef]
- Liu, J.; Jiang, P.; Tian, X.; Jia, W.; Huang, N.-L.; Zhan, H.; Chen, W. Clinical outcomes of retrievable inferior vena cava filters for venous thromboembolic diseases. J. Comp. Eff. Res. 2022, 11, 437–449. [Google Scholar] [CrossRef]
- Ramaswamy, R.S.; Jun, E.; van Beek, D.; Mani, N.; Salter, A.; Kim, S.K.; Akinwande, O. Denali, Tulip, and Option Inferior Vena Cava Filter Retrieval: A Single Center Experience. Cardiovasc. Interv. Radiol. 2018, 41, 572–577. [Google Scholar] [CrossRef]
- Kuo, W.T.; Doshi, A.A.; Ponting, J.M.; Rosenberg, J.K.; Liang, T.; Hofmann, L.V. Laser-Assisted Removal of Embedded Vena Cava Filters: A First-In-Human Escalation Trial in 500 Patients Refractory to High-Force Retrieval. J. Am. Heart Assoc. 2020, 9, e017916. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).