Abstract
Background: Pulse pressure (PP), a marker of arterial stiffening, is closely related to adverse outcomes in hypertensive patients. Correspondingly, less attention has been paid to the value of PP in the population with normal blood pressure. Methods: The study included normotensive elders aged over 60 years from the 1999–2014 National Health and Nutrition Examination Survey (NHANES). All included participants were followed up until the date of death or 31 December 2015. Restricted cubic spline analyses were used to explore the associations of PP with cardiovascular mortality and all-cause mortality. The population was categorized into two groups according to the optimal cut-off of PP for all-cause mortality by X-tile software. Propensity matching score analysis was further performed to reduce confounding bias. The Kaplan–Meier curves and Cox proportional hazard models were applied to estimate the associations of widening PP cardiovascular mortality and all-cause mortality. Subgroup analyses were also conducted. Results: A total of 6309 participants were included (52.9% men and median age 69 (63, 75) years). The median follow-up duration was 74 (42, 114) months. The restricted cubic spline analyses revealed that continuous PP was linearly related to cardiovascular mortality (p for linearity < 0.001; p for nonlinearity = 0.284) and nonlinearly related to all-cause mortality (p for nonlinearity = 0.001). After propensity score matching, 1855 subjects with widening PP and 1855 matched counterparts were included (50.2% men and average age 72 (66, 78) years, 50.9% men and average age 72 (66, 78) years, respectively), of which 966 (26.0%) died during a median follow-up duration of 71 (39, 105) months. In the Cox proportional hazards model, widening PP was associated with increased cardiovascular mortality Hazard Ratio (HR) 1.47; 95% Confidence Interval (CI) 1.07–2.00, p < 0.05] and all-cause mortality (HR 1.15; 95% CI 1.01–1.31, p < 0.05). After adjusting for other traditional risk factors, the association of widening PP with cardiovascular mortality (HR 1.44; 95%CI 1.05–1.98, p < 0.05) remained, and the association of widening PP with all-cause mortality was not statistically significant (p > 0.05). Conclusion: In the normotensive elder population, a low-risk population without traditional coronary risk factors, PP is an independent risk factor for cardiovascular mortality.
1. Introduction
Blood pressure (BP) has been increasingly recognized as an important risk factor for cardiovascular events by the public for half a century. However, there is uncertainty about the relative importance of various BP components in predicting cardiovascular risk [1,2]. Widening pulse pressure (PP), as a marker of vascular aging and arterial stiffening, is considered to be probably the best predictor of the subject being elderly out of all other BP components [3,4,5]. However, previous evidence of the relationship between PP and cardiovascular or all-cause mortality was mainly collected from studies enrolling patients with hypertension, at least partly [6,7,8,9]. It has not yet been elucidated which components of blood pressure are superior for predicting the risk for cardiovascular and all-cause mortality in the normotensive elder population.
BP usually refers to two traditional components, i.e., systolic blood pressure (SBP) and diastolic blood pressure (DBP). From the perspective of the hemodynamic alterations, however, BP can be more clearly assessed by a model that consists of PP and mean artery pressure (MAP), regarded as a pulsatile component and a steady component, respectively [10]. PP is determined by both left ventricular ejection and total arterial compliance, while MAP is influenced mainly by cardiac output and systemic vascular resistance. Under the circumstances of similar left ventricular systolic function, PP tends to represent the properties of large elastic arteries, whereas MAP tends to reflect the properties of muscular arteries and arterioles.
The efficiency of MAP and PP in predicting cardiovascular risk is debated. For clinicians, PP could be a crude but valuable, easy-to-measure marker of arterial stiffening, especially suitable to health screening in the community-based population [4]. This study attempted to explore whether a widening PP is associated with increasing risk of cardiovascular mortality or all-cause mortality in a population with normal or controlled BP.
In this large-scale elderly population, including subjects without hypertension and hypertensive patients with controlled BP, the relationship between PP and cardiovascular mortality or all-cause mortality was investigated, and propensity score matching (PSM) analysis was performed to control confounding factors and to ensure the reliability of the analysis.
2. Materials and Methods
2.1. Study Participants and Data Collection
The National Health and Nutrition Examination Survey (NHANES) is a series of large-scale surveys sponsored by the National Center for Health Statistics for analyzing the health status of civilians and presenting the corresponding measures to promote national physical quality. Data from the 1999–2014 NHANES cycle were extracted and used in this analysis. The relevant data were obtained by questionnaire and medical examination with informed consent. The survey protocol was approved by the Ethics Review Board of the National Center for Health Statistics (https://www.cdc.gov/nchs/nhanes/irba98.htm, accessed on 1 August 2021), and the methods and procedure of data extraction complied with NHANES relevant guidelines.
Methods of data collection, including collection of BP measurements, have been described previously [11]. The mean measured BP of the first three measurements was used for this analysis. Elevated BP was defined as mean SBP ≥ 140 mmHg and/or mean DBP ≥ 90 mmHg. Participants aged 60–85 years with complete basic information and BP lower than 140/90 mmHg at enrollment were included in this study. They were divided into two groups with or without widening PP according to the cut-off value of 62 mmHg that was calculated by X-tile software. The diagnosis criterion of diabetes mellitus (DM) was glycosylated hemoglobin ≥ 6.5%. Hypercholesterolemia was defined as total cholesterol (TC) above 240 mg/dL, and low high-density lipoprotein cholesterolemia was defined as lower than 40 mg/dL in males and 50 mg/dL in females. Smoking was defined if the participant had smoked more than 100 cigarettes for a lifetime. The outcome of cardiovascular mortality and all-cause mortality was collected on 31 December 2015.
2.2. Statistical Analysis
All continuous variables were identified as non-normally distributed by the Kolmogorov–Smirnov test. Continuous variables were summarized as medians and interquartile ranges and compared using the Mann–Whitney test. Categorical variables were presented by counts and percentages and compared using Pearson’s c2 test. A restricted cubic spline was performed to explore the potential dose–response pattern in PP with mortality. The population was segmented into two groups according to the optimal cut-off value of PP for all-cause mortality calculated by X-tile software (Yale University, New Haven, CT, USA). PSM analysis was applied using a 1:1 nearest neighbor matching method with a caliper width value equal to 0.02 in this study to explore the association between widening PP and cardiovascular or all-cause mortality. The propensity score was calculated by the logistic regression model, in which the covariates included age, gender, body mass index (BMI), DM, TC, high-density lipoprotein cholesterol (HDL-C), and smoking status. The Kaplan–Meier analysis was used to depict and compare by log-rank tests. Unadjusted and adjusted Cox proportional hazard models were used to assess the association of widening PP and cardiovascular or all-cause mortality, described as hazard ratio (HR) and 95% confidence interval (CI). Multivariable Cox regression analysis adjusted for all variables with p < 0.1 in univariate Cox regression analysis. We further assessed the relationship between widening PP and cardiovascular mortality using subgroup analysis and interaction analysis. All analyses were performed in R version 4.0.3, and a two-sided p-value < 0.05 was considered significant.
3. Results
3.1. The Baseline Characteristics of All Subjects
There were 6309 subjects (52.9% men and average age 69 (63, 75) years) included in this study, and the median follow-up duration was 74 (42, 114) months. The baseline characteristics of all subjects in groups with normal PP or widening PP are shown in Table 1. There were 4294 subjects (54.8% men and average age 67 (63,73) years) with normal PP and 2015 subjects (48.9% men and average age 73 (66, 80) years) with widening PP; the median follow-up duration was 77 (44, 120) months and 69 (39, 101) months, respectively. Subjects with widening PP were commonly elderly and female, with a higher prevalence of DM and frequently higher TC and lower MAP (p < 0.001). Compared to subjects with normal PP, subjects with widening PP had higher cardiovascular mortality and all-cause mortality (p < 0.001).

Table 1.
The baseline characteristics of all subjects with normal PP and widening PP.
3.2. Associations between PP and Mortality in All Subjects
As shown in Figure 1, higher PP was linearly associated with higher cardiovascular mortality (p for linearity < 0.001; p for nonlinearity = 0.284) and nonlinearly associated with all-cause mortality (p for nonlinearity = 0.001).
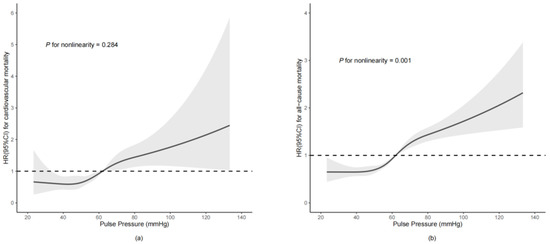
Figure 1.
HRs for cardiovascular mortality (a) and all-cause mortality (b) according to PP (continuous variable). This model was adjusted by age, body mass index, diabetes mellitus, total cholesterol, high-density lipoprotein cholesterol, and mean artery pressure.
3.3. The Baseline Characteristics of the Study Subjects after PSM
After PSM, a total of 1855 subjects with widening PP (50.9% men and average age 72 (66, 78) years) were matched with 1855 subjects with normal PP (50.2% men and average age 72 (66, 78) years) (Table 2). The differences between groups were mostly unremarkable except for differences relating to MAP (p > 0.05). A similar, significant difference in cardiovascular mortality (p < 0.05) was found, while all-cause mortality (p > 0.05) was not significantly different between the two groups.

Table 2.
The baseline characteristics of subjects after PSM with normal PP and widening PP.
3.4. Survival Analysis before and after PSM
As shown in Figure 2, the association between widening PP and cardiovascular or all-cause mortality was evaluated by Kaplan–Meier curves. The cumulative incidence of cardiovascular mortality in subjects with widening PP was higher than that in subjects without widening PP both before PSM (log-rank test: p < 0.001) and after PSM (log-rank test: p = 0.016). Subjects with widening PP had higher all-cause mortality before PSM (log-rank test: p < 0.001) and after PSM (log-rank test: p = 0.029).
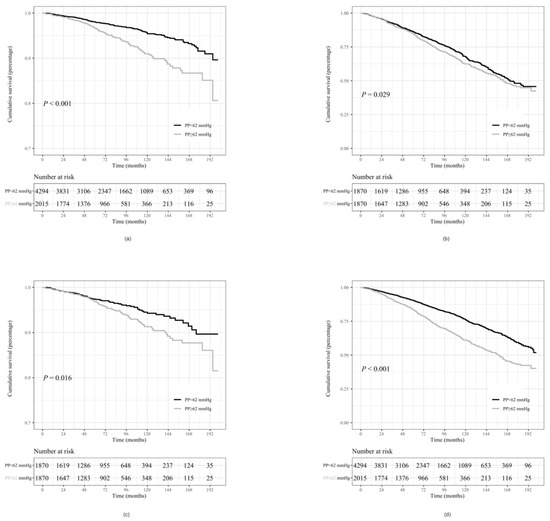
Figure 2.
Kaplan–Meier curves for cardiovascular mortality and all-cause mortality in widening PP subjects vs. normal PP subjects. (a): cardiovascular mortality in widening PP subjects vs. normal PP subjects before PSM, (b): all-cause mortality in widening PP subjects vs. normal PP subjects before PSM, (c): cardiovascular mortality in widening PP subjects vs. normal PP subjects after PSM, (d): all-cause mortality in widening PP subjects vs. normal PP subjects after PSM. PSM: propensity score match, PP: pulse pressure.
The Cox regression analysis is shown in Table 3. In the unadjusted Cox regression models, compared to subjects with normal PP, subjects with widening PP had a significant higher risk of cardiovascular (HR 1.96; 95% CI 1.52–2.52, p < 0.001) and all-cause mortality (HR 1.74; 95% CI 1.57–1.94, p < 0.001). After adjusting the variables with p < 0.1 in the multivariate Cox regression models, widening PP was considered an independent risk factor of cardiovascular mortality (HR 1.32; 95% CI 1.01–1.74, p = 0.045), while no difference was found for all-cause mortality (HR 1.11; 95% CI 0.99–1.24, p = 0.080). After further analysis of the matched cohort, subjects with widening PP still had higher risk of cardiovascular mortality (univariate: HR 1.47; 95% CI 1.07–2.00, p = 0.016; multivariate: HR 1.44; 95% CI 1.05–1.98, p = 0.024). Subjects with widening PP had higher risk of all-cause mortality in the univariate model (HR 1.15; 95% CI 1.01–1.31, p = 0.029), but the difference was not significant in the multivariate model (HR 1.10; 95% CI 0.91–1.33, p = 0.309).

Table 3.
The univariate and multivariate Cox regression analyses for cardiovascular mortality and all-cause mortality before PSM and after PSM.
3.5. Subgroup Analysis Stratified by Traditional Cardiovascular Risk Factors
As shown in Figure 3, there were significant differences in cardiovascular mortality between subjects with and without widening PP in most subgroups, except for the subgroup of subjects who were under 70 years old (HR 1.53, 95% CI 0.96–2.46; p = 0.075) with DM (HR 1.31; 95% CI 0.79–2.16, p = 0.296) and with hypercholesterolemia (HR 1.62; 95% CI 0.82–3.18, p = 0.163). Widening PP was associated with a 3.30-fold (95% CI, 2.04–5.33) increase in the risk of cardiovascular mortality in the subgroup who was female, whereas the association was weaker in the subgroup who was male (HR 1.69; 95% CI 1.24–2.31, p < 0.001). The association was stronger in the subgroups of non-smokers (HR 2.05; 95% CI 1.33–3.16, p < 0.001), participants with normal HDL-C (HR 2.14; 95% CI 1.55–2.94, p < 0.001), and participants without hypertension (HR 2.28; 95% CI 1.58–3.30, p < 0.001) compared to in the subgroups of smokers (HR 1.98; 95% CI 1.45–2.71, p < 0.001), participants with low HDL-C (HR 1.64; 95% CI 1.08–2.49, p = 0.021), and participants with well-controlled hypertension (HR 1.61; 95% CI 1.13–2.29, p < 0.001), respectively. Significant interaction was found between PP and gender (p for interaction = 0.023).
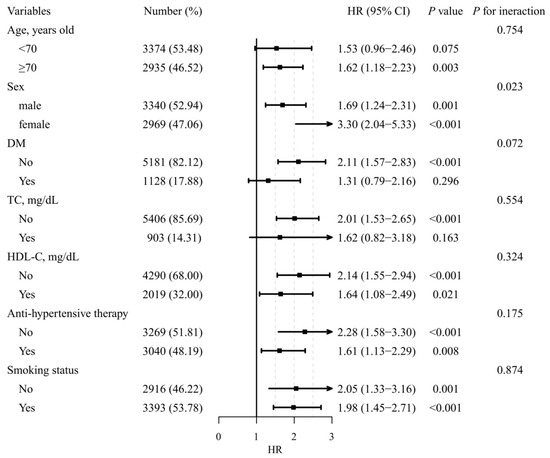
Figure 3.
Forest plots of cardiovascular survival according to stratified traditional cardiovascular risk factors during follow up. DM: diabetes mellitus, TC: total cholesterol, HDL-C: high-density lipoprotein cholesterol, PP: pulse pressure, MAP: mean artery pressure.
4. Discussion
In the large cohort survey of the non-institutionalized, normotensive elderly population of the United States, we found that PP was positively associated with cardiovascular mortality within about 6 years of follow up. Furthermore, there was a linear relationship between PP and cardiovascular mortality and a nonlinear relationship between PP and all-cause mortality. The subjects with widening PP had higher cardiovascular and all-cause mortality than those with normal PP. The optimal cut-off value of widening PP in this population was almost identical to the recommended value of PP as a marker of arterial stiffening in the 2018 European Society of Cardiology/European Society of Hypertension Guidelines for the management of arterial hypertension [4].
Arterial stiffening is a common pathogenesis mechanism in almost all age-related diseases [12]. Both PP ≥ 60 mmHg and pulse wave velocity (PWV) > 10 m/s are considered as the indication of arterial stiffening [8]. In recent years, a large amount of evidence has demonstrated that a widening PP is capable of predicting adverse cardiovascular outcomes, independent of traditional risk factors, in specific populations, especially in hypertensive patients [6,7,8,9]. Additionally, PP has unique advantages over PWV, i.e., availability and low cost, especially for health screening in primary hospitals and large-scale populations, while PWV measurement is still not publicly available.
Considering that hypertension and arterial stiffening usually coexist in elders, hypertension superimposes the cardiovascular risk on the basis of arterial stiffening, so the cardiovascular risk predicted by PP is hardly ever attributed to arterial stiffening in hypertensive patients [13,14]. Consequently, the cardiovascular risk originating from widening PP per se has not been convincingly differentiated from the influence of arterial stiffening. In this study, in order to filter out the impact of elevated BP on the outcome, we excluded the population with elevated BP and selected a normotensive population with relatively-low-to-moderate cardiovascular risk, including subjects without hypertension and hypertensive patients with controlled BP. Furthermore, we applied PSM and adjusted other traditional risk factors in the multivariate model to minimize their impact on the outcome. After PSM, the group of participants with normal PP had even higher MAP than the counterparts. We supposed that individuals with lower PP were less likely to suffer from arterial stiffening and, therefore, were more likely to have a higher DBP.
PP seems simple, but it has a complex physiological background. A study found that there is a U-shaped relationship between PP and mortality in acute coronary syndrome patients undergoing percutaneous coronary intervention [7]. This U-shaped relationship was not found in our study, possibly because our study population was a community population with normal cardiac function.
Widening PP raises the risk of cardiovascular death by increasing left ventricular afterload and wall stress, affecting ventricular remodeling and myocardial fibrosis and reducing diastolic coronary perfusion [12]. All of the above pathophysiological alterations contribute to the development of heart failure, ischemic heart disease, and other cardiovascular diseases. Widening PP is also related to cerebrovascular events and accelerates the progression of chronic kidney diseases, thereby increasing the risk of all-cause death [15,16]. Results from the the Meta-analysis Global Group in Chronic Heart Failure (MAGGIC) study showed that higher PP is associated with crude mortality but loses its predictive value after adjustment for covariates [17]. In our study, after strict adjustment of traditional cardiovascular risk factors, widening PP was still significantly associated with cardiovascular mortality, but the association of widening PP with all-cause mortality was not statistically significant.
Of interest, SBP, which is mainly determined by stroke volume, was unrelated to mortality in our study. This finding may also drop a hint that arterial stiffening, reflected by PP, may be the key point related to mortality in normotensive elders.
SBP is the most widely used BP component in current cardiovascular diseases risk estimation systems, which mainly focus on the middle-age group of those aged from 40 to 65 years old, so the accuracy of various assessment systems is equivocal when applied to the elderly population. Our study found that PP rather than SBP is an independent risk factor of cardiovascular mortality in the normotensive elders. It may be possible to consider using PP rather than SBP in cardiovascular risk estimation systems for elders.
A clinically useful cut-off value for PP may be difficult to derive from the current study, as the cut-off values of the widening PP differed among the various study subgroups. As mentioned above, 60mmHg of PP is an acceptable critical value and has been used in many studies [4,7]. The cut-off value of widening PP in our study was determined by X-tile software according to the best differentiation of all-cause mortality in this population, and that of cardiovascular mortality was 63mmHg. Both were approximately equal to 60mmHg, indicating that this could be a reliable cut-off value even in the elderly without elevated BP.
The subgroup analysis suggested that the effect of widening PP on the risk of cardiovascular mortality was more obvious in the participants without DM and hypercholesterolemia than in their counterparts. DM and hypercholesterolemia are major risk factors for both arterial stiffening and cardiovascular diseases, so the role of PP in diabetic and hyperlipidemic patients is confounding and not independent. Similarly, in the non-smoking population or the population without hypertension, widening PP was correlated with a higher risk of cardiovascular mortality. This finding suggests that widening PP has more important prognostic significance in populations with fewer risk factors. In individuals who were female or aged over 70 years, widening PP was associated with a higher risk for cardiovascular mortality, which indicates the more significant role of arterial stiffness in cardiovascular health in these special populations.
The limitations of our research are as follows: Firstly, 55% of participants were on anti-hypertensive treatment at baseline. Although anti-hypertensive treatment could influence PP and mortality, we did not adjust for anti-hypertensive medication when correcting for confounders, as the information was derived from self-report, and the classes of drugs were not reported in the database. However, the participants were divided into two subgroups based on the history of anti-hypertensive medication in the subgroup analysis. Secondly, due to the limited self-report information, it was impossible to exclude all peripheral vascular disease, arteriovenous fistulas, hyperthyroidism, and other diseases that would affect PP. We reasonably presumed that a small number of patients with mild diseases would not affect the conclusions, because this was a community-based population, and the sample size was large. Thirdly, central PP may provide more physiologically relevant information, but it is difficult to obtain for individuals in the community. Furthermore, the prognostic value of central PP over branchial PP is controversial, and studies showed that central PP does not offer significant additional predictive ability compared to branchial PP [3,18]. Fourthly, the characteristics of this study population showed that participants were mostly white Americans aged 60 to 85 years old, so the conclusion may not be extrapolated to other races or very elderly people.
5. Conclusions
In normotensive elder population, a low-risk population without traditional coronary risk factors, PP is an independent risk factor for cardiovascular mortality.
Author Contributions
Conceptualization, Y.J., H.Z. and W.T.; Data curation, H.Z. and Y.Y.; Formal analysis, Y.J. and H.Z.; Methodology, H.Z.; Project administration, Y.S. and W.T.; Supervision, W.T.; Validation, Y.J., Y.Y. and Y.S.; Visualization, H.Z.; Writing—original draft, Y.J.; Writing—review and editing, W.T. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by grants from the ‘Thirteenth Five-Year’ program funds (the National Key Research and Development Program of China, grant no. 2018YFC2000301).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data are included in the NHANES database (https://wwwn.cdc.gov/nchs/nhanes/Default.aspx, accessed on 1 August 2021).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Warren, J.; Nanayakkara, S.; Andrianopoulos, N.; Brennan, A.; Dinh, D.; Yudi, M.; Clark, D.; Ajani, A.E.; Reid, C.M.; Selkrig, L.; et al. Impact of Pre-Procedural Blood Pressure on Long-Term Outcomes Following Percutaneous Coronary Intervention. J. Am. Coll. Cardiol. 2019, 73, 2846–2855. [Google Scholar] [CrossRef] [PubMed]
- Georgakis, M.K.; Gill, D.; Malik, R.; Protogerou, A.D.; Webb, A.J.S.; Dichgans, M. Genetically Predicted Blood Pressure across the Lifespan: Differential Effects of Mean and Pulse Pressure on Stroke Risk. Hypertension 2020, 76, 953–961. [Google Scholar] [CrossRef] [PubMed]
- Vlachopoulos, C.; Aznaouridis, K.; O’Rourke, M.F.; Safar, M.E.; Baou, K.; Stefanadis, C. Prediction of cardiovascular events and all-cause mortality with central haemodynamics: A systematic review and meta-analysis. Eur. Heart J. 2010, 31, 1865–1871. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Melgarejo, J.D.; Thijs, L.; Wei, D.-M.; Bursztyn, M.; Yang, W.-Y.; Li, Y.; Asayama, K.; Hansen, T.W.; Kikuya, M.; Ohkubo, T.; et al. Relative and Absolute Risk to Guide the Management of Pulse Pressure, an Age-Related Cardiovascular Risk Factor. Am. J. Hypertens. 2021, 34, 929–938. [Google Scholar] [CrossRef] [PubMed]
- Pareek, M.; Vaduganathan, M.; Biering-Sørensen, T.; Byrne, C.; Qamar, A.; Almarzooq, Z.; Pandey, A.; Olsen, M.H.; Bhatt, D.L. Pulse Pressure, Cardiovascular Events, and Intensive Blood-Pressure Lowering in the Systolic Blood Pressure Intervention Trial (SPRINT). Am. J. Med. 2019, 132, 733–739. [Google Scholar] [CrossRef] [PubMed]
- Wei, H.; Hongwei, L.; Ying, S.; Dai, Z.; Man, W. The U-shape relationship between pulse pressure level on inpatient ad-mission and long-term mortality in acute coronary syndrome patients undergoing percutaneous coronary intervention. J. Clin. Hypertens. 2021, 24, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Wei, F.-F.; Wu, Y.; Xue, R.; Liu, X.; He, X.; Dong, B.; Zhen, Z.; Chen, X.; Liang, W.; Zhao, J.; et al. Clinical Significance of Mean and Pulse Pressure in Patients with Heart Failure with Preserved Ejection Fraction. Hypertension 2022, 79, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Selvaraj, S.; Steg, P.G.; Elbez, Y.; Sorbets, E.; Feldman, L.J.; Eagle, K.A.; Ohman, E.M.; Blacher, J.; Bhatt, D.L.; on behalf of the REACH Registry Investigators. Pulse Pressure and Risk for Cardiovascular Events in Patients with Atherothrombosis: From the REACH Registry. J. Am. Coll. Cardiol. 2016, 67, 392–403. [Google Scholar] [CrossRef] [PubMed]
- Darne, B.; Girerd, X.; Safar, M.; Cambien, F.; Guize, L. Pulsatile versus steady component of blood pressure: A cross-sectional analysis and a prospective analysis on cardiovascular mortality. Hypertension 1989, 13, 392–400. [Google Scholar] [CrossRef] [PubMed]
- Burt, V.L.; Whelton, P.; Roccella, E.J.; Brown, C.; Cutler, J.A.; Higgins, M.; Horan, M.J.; Labarthe, D. Prevalence of hypertension in the US adult population. Results from the Third National Health and Nutrition Examination Survey, 1988–1991. Hypertension 1995, 25, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Chirinos, J.A.; Segers, P.; Hughes, T.; Townsend, R. Large-Artery Stiffness in Health and Disease: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2019, 74, 1237–1263. [Google Scholar] [CrossRef] [PubMed]
- Laurent, S.; Boutouyrie, P. Arterial Stiffness and Hypertension in the Elderly. Front. Cardiovasc. Med. 2020, 7, 544302. [Google Scholar] [CrossRef] [PubMed]
- Niiranen, T.J.; Kalesan, B.; Hamburg, N.M.; Benjamin, E.J.; Mitchell, G.F.; Vasan, R.S. Relative Contributions of Arterial Stiffness and Hypertension to Cardiovascular Disease: The Framingham Heart Study. J. Am. Heart Assoc. 2016, 5, e004271. [Google Scholar] [CrossRef] [PubMed]
- Webb, A.J.; Lawson, A.; Wartolowska, K.; Mazzucco, S.; Rothwell, P.M.; on behalf of the OXVASC Study Cohort. Aortic Stiffness, Pulse Pressure, and Cerebral Pulsatility Progress despite Best Medical Management: The OXVASC Cohort. Stroke 2022, 53, 1310–1317. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.-Y.; Meng, Q.; Yang, C.; Wang, Y.; Kong, G.; Zhao, Y.; Wang, F.; Zhang, L. Association between pulse pressure, systolic blood pressure and the risk of rapid decline of kidney function among general population without hypertension: Results from the China health and retirement longitudinal study (CHARLS). J. Transl. Med. 2021, 19, 512. [Google Scholar] [CrossRef] [PubMed]
- Jackson, C.E.; Castagno, D.; Maggioni, A.P.; Køber, L.; Squire, I.B.; Swedberg, K.; Andersson, B.; Richards, A.M.; Bayes-Genis, A.; Tribouilloy, C.; et al. Differing prognostic value of pulse pressure in patients with heart failure with reduced or preserved ejection fraction: Results from the MAGGIC individual patient meta-analysis. Eur. Heart J. 2015, 36, 1106–1114. [Google Scholar] [CrossRef] [PubMed]
- Laugesen, E.; Knudsen, S.T.; Hansen, K.W.; Rossen, N.B.; Jensen, L.O.; Hansen, M.S.; Andersen, L.K.; Thomsen, K.K.; Søndergaard, H.; Böttcher, M.; et al. Invasive aortic purvival Analysis Before and Afterflse pressure is not superior to cuff pulse pressure in cardiovascular risk prediction. J. Hypertens. 2020, 39, 607–613. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).