Management of Malpositioned Double-Lumen Tubes: A Simulation-Based Training Exercise for Anesthesiology Residents
Abstract
:1. Introduction
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Rothkrug, A.; Mahboobi, S.K. Simulation training and skill assessment in anesthesiology. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Nestel, D.; Groom, J.; Eikeland-Husebø, S.; O’Donnell, J.M. Simulation for learning and teaching procedural skills: The state of the science. Simul. Healthc. 2011, 6, S10–S13. [Google Scholar] [CrossRef] [PubMed]
- Bora, V.; Kritzmire, S.M.; Arthur, M.E. Double Lumen Endobronchial Tubes. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Smith, S.; Arthur, M.E. Lung Isolation Anesthesia. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Inoue, S.; Nishimine, N.; Kitaguchi, K.; Furuya, H.; Taniguchi, S. Double lumen tube location predicts tube malposition and hypoxaemia during one lung ventilation. Br. J. Anaesth. 2004, 92, 195–201. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klein, U.; Karzai, W.; Bloos, F.; Wohlfarth, M.; Gottschall, R.; Fritz, H.; Gugel, M.; Seifert, A. Role of fiberoptic bronchoscopy in conjunction with the use of double-lumen tubes for thoracic anesthesia: A prospective study. Anesthesiology 1998, 88, 346–350. [Google Scholar] [CrossRef] [PubMed]
- Brodsky, J.B.; Shulman, M.S.; Mark, J.B. Malposition of left-sided double-lumen endobronchial tubes. Anesthesiology 1985, 62, 667–669. [Google Scholar] [CrossRef] [PubMed]
- Campos, J.H.; Hallam, E.A.; Van Natta, T.; Kernstine, K.H. Devices for lung isolation used by anesthesiologists with limited thoracic experience: Comparison of double-lumen endotracheal tube, Univent torque control blocker, and Arndt wire-guided endobronchial blocker. Anesthesiology 2006, 104, 261-5A. [Google Scholar] [CrossRef] [PubMed]
- Campos, J.H.; Hallam, E.A.; Ueda, K. Training in placement of the left-sided double-lumen tube among non-thoracic anaesthesiologists: Intubation model simulator versus computer-based digital video disc, a randomised controlled trial. Eur. J. Anaesthesiol. 2011, 28, 169–174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Failor, E.; Bowdle, A.; Jelacic, S.; Togashi, K. High-fidelity simulation of lung isolation with double-lumen endotracheal tubes and bronchial blockers in anesthesiology resident training. J. Cardiothorac. Vasc. Anesth. 2014, 28, 865–869. [Google Scholar] [CrossRef] [PubMed]
- Jelačić, S.; Ghioni, V.; Bowdle, A. Airway anatomy of AirSim high-fidelity simulator. Anesthesiology 2013, 118, 228–229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hierlmeier, B.; Levesque, V.; Vale, H. Lung Isolation. In Anesthesiology; Decker Medicine: Toronto, ON, Canada, December 2018. [Google Scholar] [CrossRef]


| Steps to Assess DLT Position |
|---|
| Assess the tube length at the teeth: Is it too deep or too shallow? |
| Fiberoptic scope down the tracheal lumen to identify position; if unsure, go to step 3. |
| Fiberoptic scope down the bronchial lumen; if unsure, go to step 4. |
| With the scope through the bronchial lumen, deflate both the tracheal and bronchial cuffs and start withdrawing the DLT until you can confirm carina with left and right mainstem along with right-upper lobe for confirmation. |
| Once carina is accurately identified, (then) with the scope still through the bronchial lumen, advance the DLT into the correct position over the scope. |
| Confirm correct position of the fiberoptic scope through the tracheal lumen and visualize the bronchial lumen going into the left mainstem along with RUL identification. Inflate the tracheal, then the bronchial cuffs. |
| Simulation Position | First Attempt (Seconds) | Repeat Weeks Later (Seconds) | Difference (Seconds) |
|---|---|---|---|
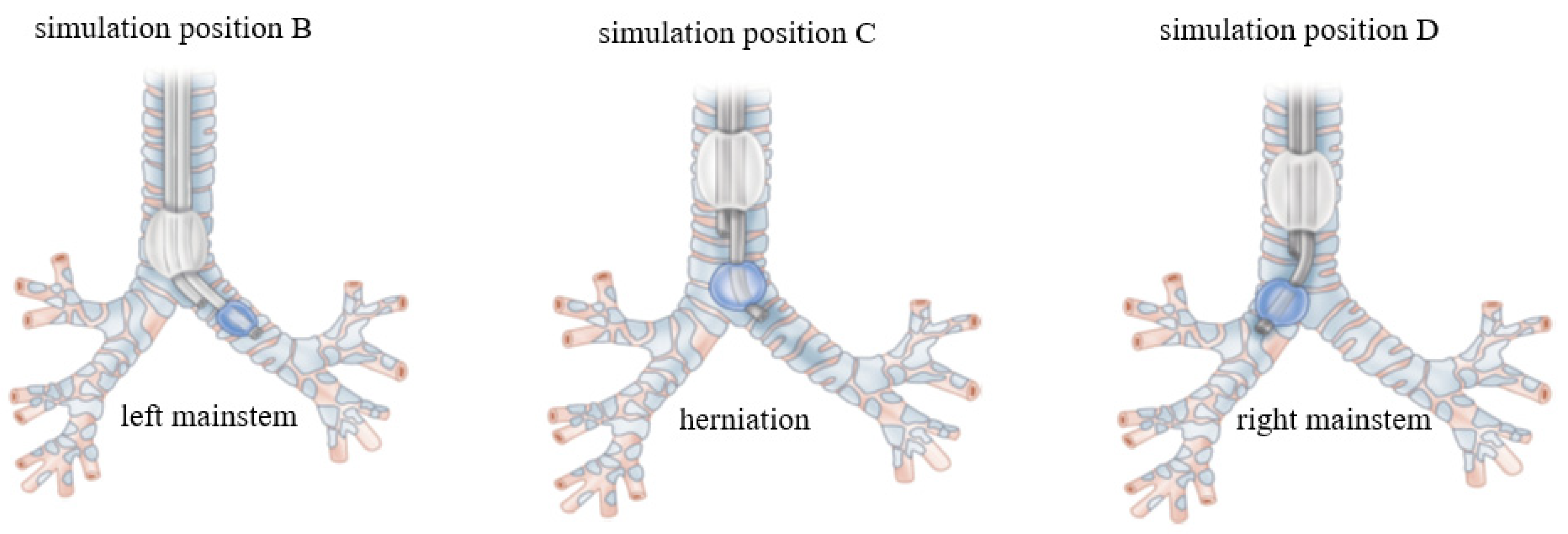
| B | 134 | 34 | 99 |
| C | 126 | 56 | 70 |
| D | 156 | 76 | 80 |
| Average | 139 | 56 | 83 |
| Questionnaire Item | After First Assessment | After Curriculum + Simulation Training |
|---|---|---|
| Extremely comfortable | 0% | 10% |
| Very comfortable | 0% | 40% |
| Comfortable | 10% | 50% |
| Not comfortable | 70% | 0% |
| Very uncomfortable | 20% | 0% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hierlmeier, B.; Prem, A.; Anand, S.; Lerant, A.; Ostrovsky, G. Management of Malpositioned Double-Lumen Tubes: A Simulation-Based Training Exercise for Anesthesiology Residents. Int. Med. Educ. 2022, 1, 4-10. https://doi.org/10.3390/ime1010003
Hierlmeier B, Prem A, Anand S, Lerant A, Ostrovsky G. Management of Malpositioned Double-Lumen Tubes: A Simulation-Based Training Exercise for Anesthesiology Residents. International Medical Education. 2022; 1(1):4-10. https://doi.org/10.3390/ime1010003
Chicago/Turabian StyleHierlmeier, Bryan, Anand Prem, Suwarna Anand, Anna Lerant, and Galina Ostrovsky. 2022. "Management of Malpositioned Double-Lumen Tubes: A Simulation-Based Training Exercise for Anesthesiology Residents" International Medical Education 1, no. 1: 4-10. https://doi.org/10.3390/ime1010003
APA StyleHierlmeier, B., Prem, A., Anand, S., Lerant, A., & Ostrovsky, G. (2022). Management of Malpositioned Double-Lumen Tubes: A Simulation-Based Training Exercise for Anesthesiology Residents. International Medical Education, 1(1), 4-10. https://doi.org/10.3390/ime1010003






