Feeding and Gastrointestinal Symptomatology: Comparing Infants Without Oral Restriction to Those with Treated and Untreated Tethered Oral Tissues
Abstract
INTRODUCTION
METHODS
Design
Settings
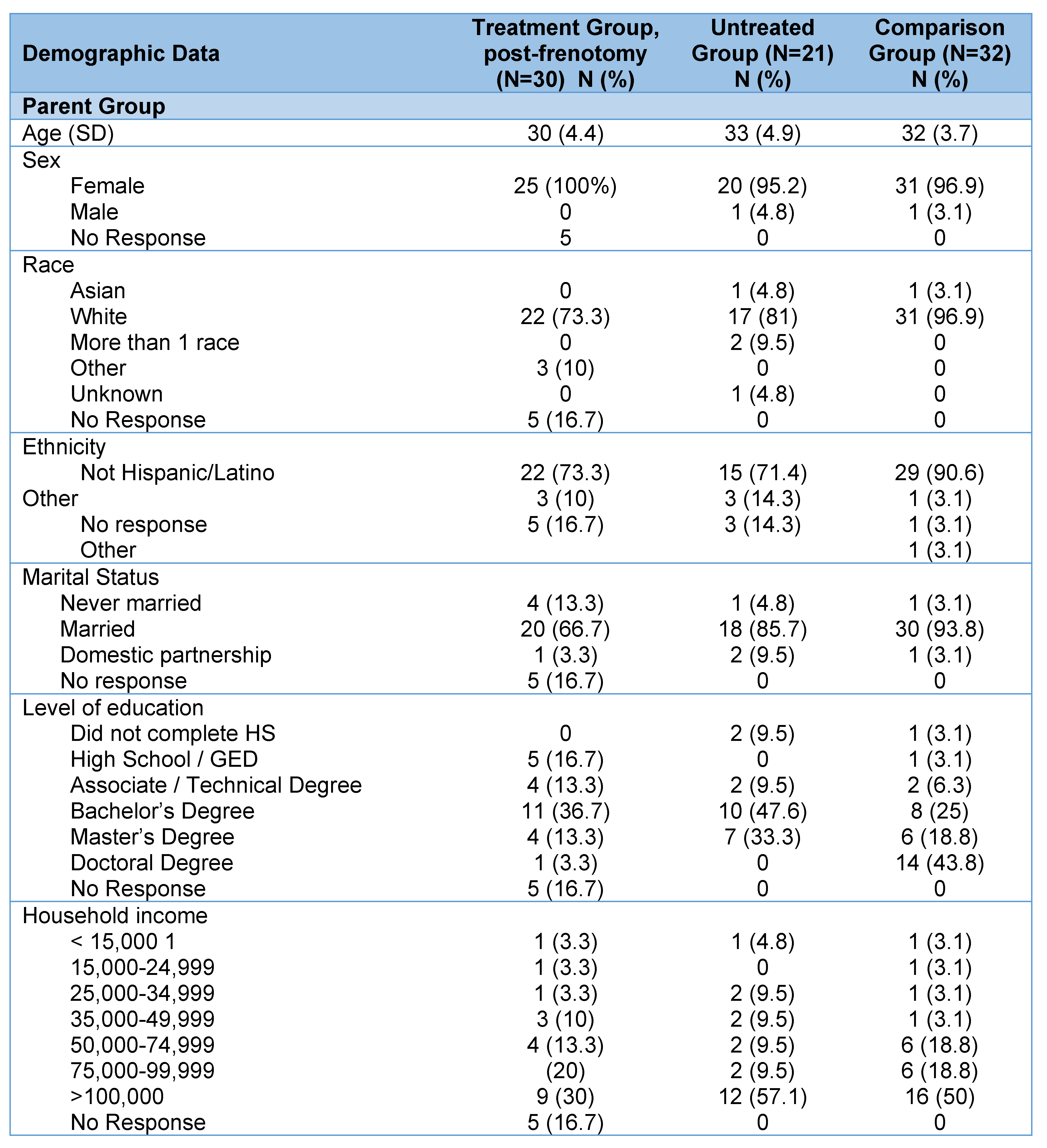
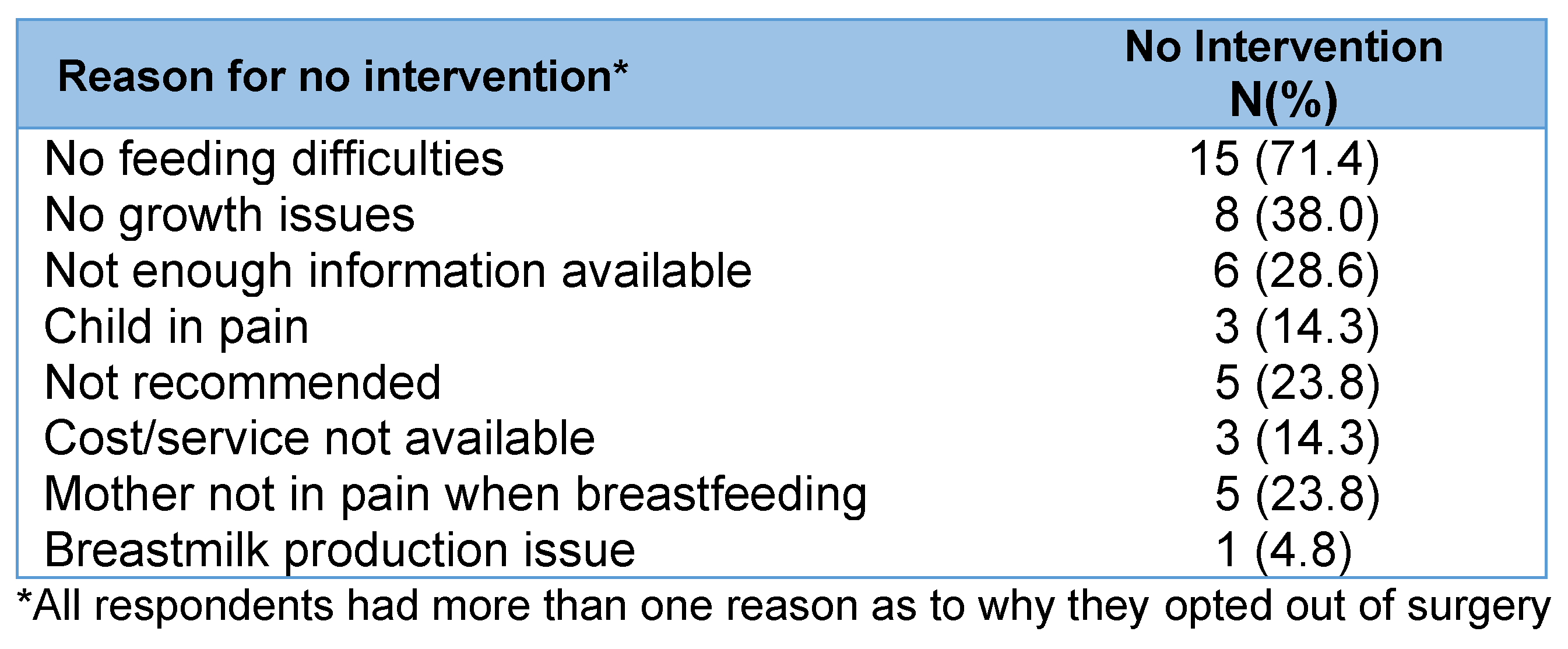
Sample
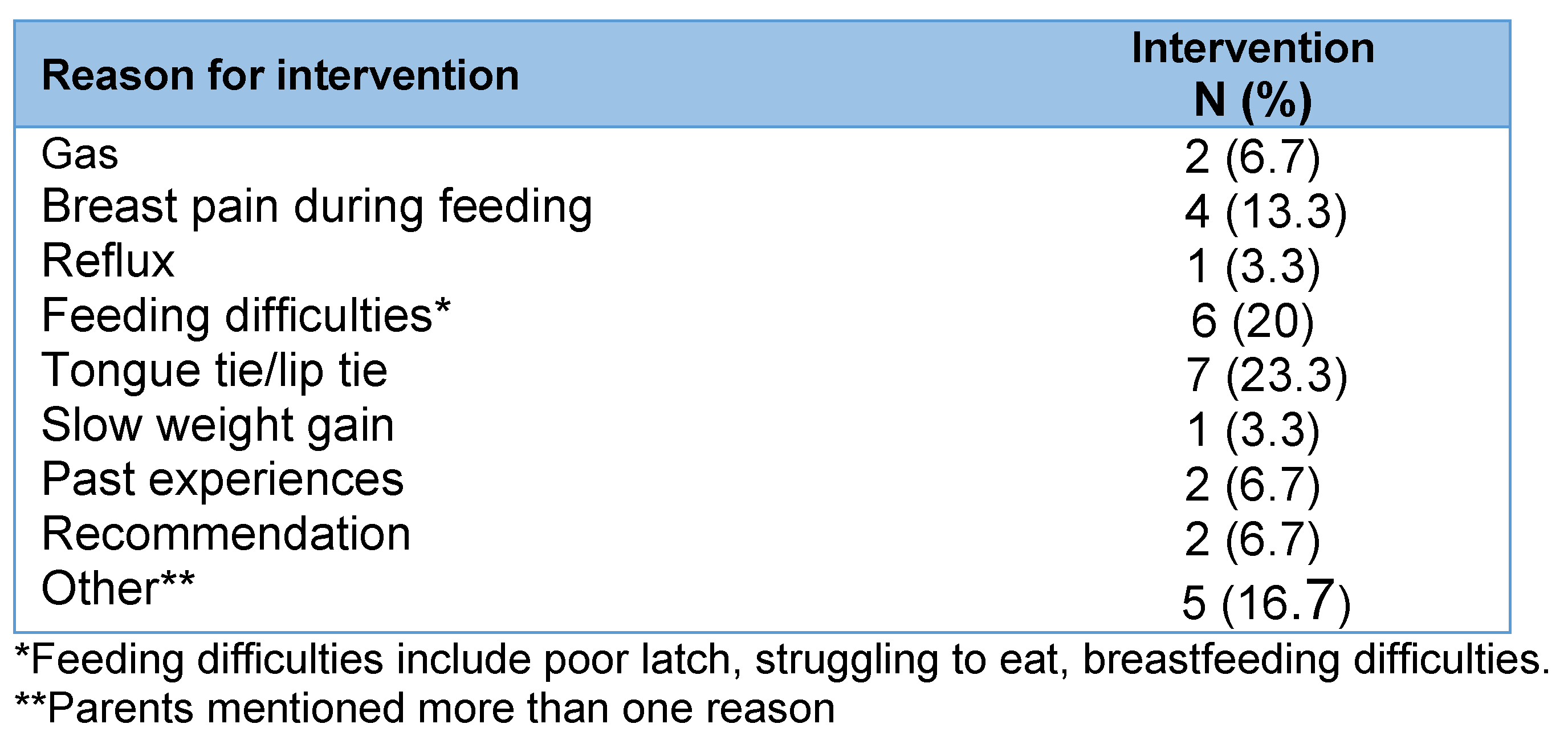
Frenotomy Intervention
Data Collection
Measures
Analysis
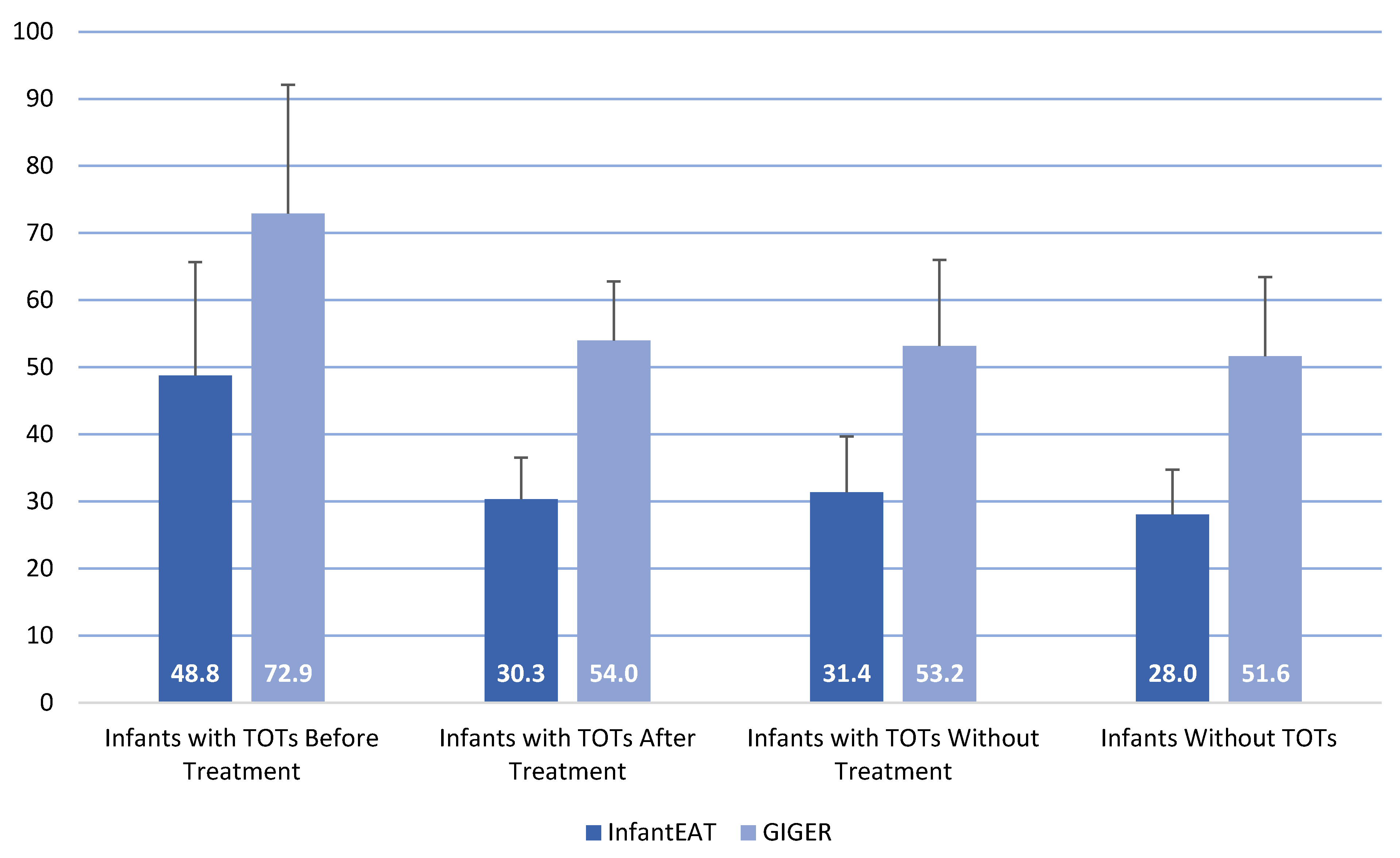
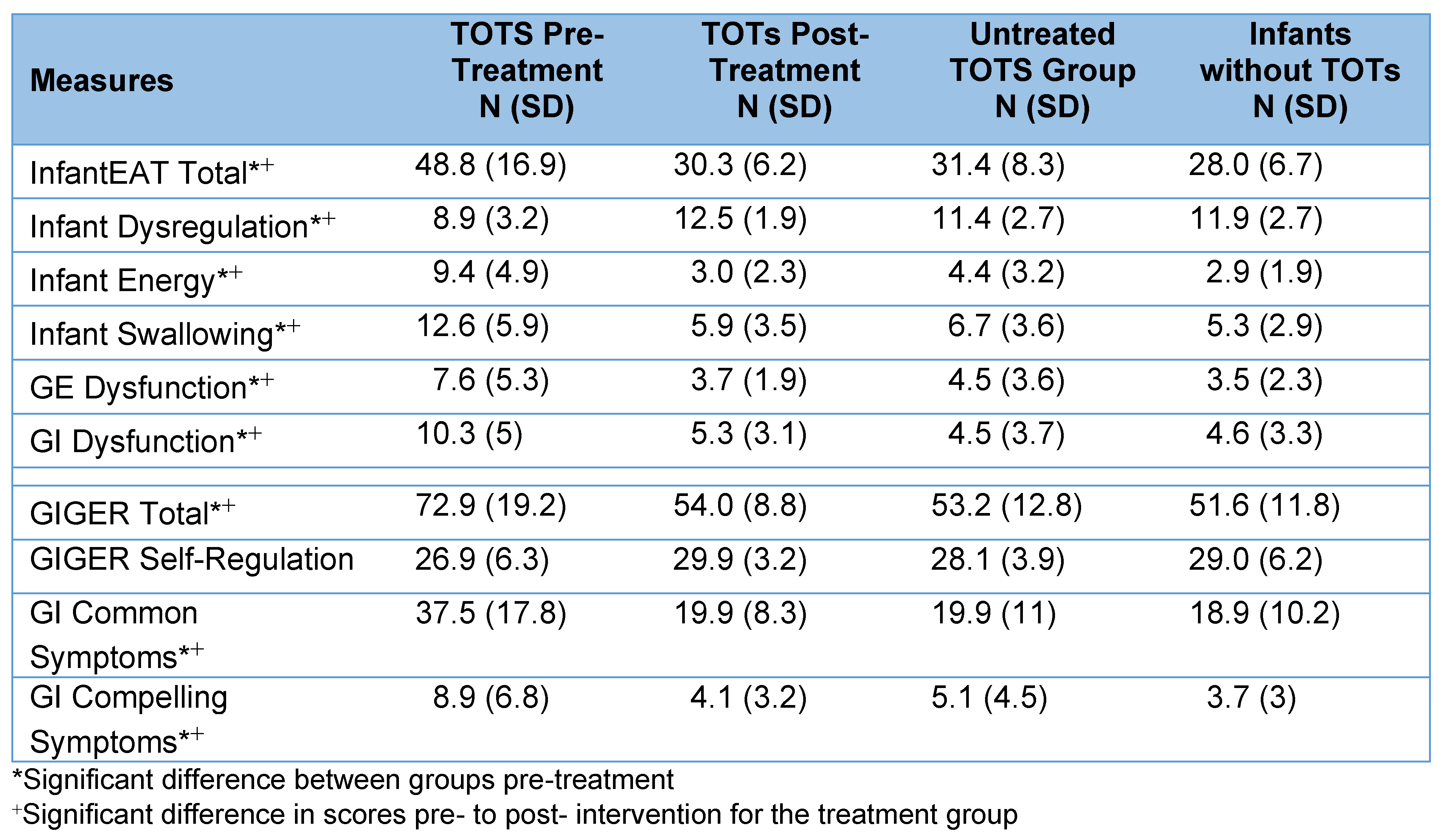
Results
DISCUSSION
CONCLUSION
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix
References
- Becker, S., and M. D. Mendez. 2022. Ankyloglossia. In StatPearls. StatPearls Publishing: Available online: http://www.ncbi.nlm.nih.gov/books/NBK482295/.
- Brookes, A.F., and D. Bowley. 2014. Tongue tie: The evidence for frenotomy. Early Human Development 90: 765–768. [Google Scholar] [CrossRef] [PubMed]
- Corvaglia, L., and S. Martini. 2015. Feeding difficulties during the neonatal period. Italian Journal of Pediatrics 41, S2: A21, 1824-7288-41 S2-A21. [Google Scholar] [CrossRef]
- Freeman, C.G., J.F. Ohlstein, N.A. Rossi, and et al. 2022. Labial frenectomy for symptomatic isolated upper lip tie. Cureus 14, 12: e32755. [Google Scholar] [CrossRef]
- Frenectomy for the Correction of Ankyloglossia: A Review of Clinical Effectiveness and Guidelines (2016). Canadian Agency for Drugs and Technologies in Health. Available online: https://www.ncbi.nlm.nih.gov/books/NBK373454.
- Hand, P., G. Olivi, C. Lajolo, and et al. Short lingual frenum in infants, children, and adolescents. Part 1: Breastfeeding and gastroesophageal reflux disease improvement after tethered oral tissues release. European Journal of Pediatric Dentistry 21, 4: 309–317. [CrossRef] [PubMed]
- Harris, P.A., R. Taylor, R. Thielke, J. Payne, N. Gonzalez, and J.G. Conde. 2009. Research electronic data capture (REDCap)-a-metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics 42, 2: 377–381. [Google Scholar] [CrossRef]
- Harris, P.A., R. Taylor, B. L. Minor, and et al. 2019. The REDCap consortium: Building an international community of software platform partners. Journal of Biomedical Informatics 95: 1–10. [Google Scholar] [CrossRef] [PubMed]
- Hill, R.R., M. Hines, A. Martens, B.F. Pados, and E. Zimmerman. 2022. A pilot study of non-nutritive suck measures immediately pre-and post-frenotomy in full term infants with problematic feeding. Journal of Neonatal Nursing 28: 413–419. [Google Scholar] [CrossRef]
- Hill, R.R., K.S. Lyons, S. Kelly-Weeder, and B.F. Pados. 2023. Improvement in problematic feeding symptoms for infants with tethered oral tissues after frenotomy. Journal of Neonatal Nursing. Online ahead of print. [Google Scholar] [CrossRef]
- Hill, R.R., and B.F. Pados. 2020. Symptoms of problematic feeding in infants under 1 year of age undergoing frenotomy: A review article. Acta Paediatrica 109: 2502–2514. [Google Scholar] [CrossRef]
- Hill, R.R., and B.F. Pados. 2023. Gastrointestinal symptom improvement for infants following tongue-tie correction. Clinical Pediatrics 62, 2: 136–142. [Google Scholar] [CrossRef]
- Hill, R.R., M.A. Richard, and B.F. Pados. Breastfeeding symptoms with tongue-and lip-tie. MCN: The American Journal of Maternal Child Nursing 48, 1: 17–23. [CrossRef]
- Kotlow, L. 2015. TOTS-Tethered oral tissues. The assessment and diagnosis of the tongue and upper lip ties in breastfeeding. Oral Health: Available online: https://www.oralhealthgroup.com/features/tots- (accessed on 8 March 2023).
- Messner, A.H., J. Walsh, R. M. Rosenfeld, S. R. Schwartz, S. L. Ishman, C. Baldassari, and et al. 2020. Clinical Consensus Statement: Ankyloglossia in Children. Otolaryngology-Head and Neck Surgery (United States) 162, 5: 597–611. [Google Scholar] [CrossRef]
- Mills, N., S. M. Pransky, D. T. Geddes, and S. A. Mirjalili. 2019. What is a tongue tie? Defining the anatomy of the in-situ lingual frenulum. Clinical Anatomy 32, 6: 749–761. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, M.E., A.M. Gilliland, and Y. LeFort. 2022. Complications and misdiagnoses associated with infant frenotomy: Results of a healthcare professional survey. International Breastfeeding Journal 17, 1: 39. [Google Scholar] [CrossRef] [PubMed]
- O’Shea, J.E., J.P. Foster, C.P. O’Donnell, D. Breathnach, S.E. Jacobs, D.A. Todd, and P.G. Davis. 2017. Frenotomy for tongue-tie in newborn infants. The Cochrane Database of Systematic Reviews 3, 3: CD011065. [Google Scholar] [CrossRef] [PubMed]
- Pados, B.F., and R.R. Hill. 2024. Development, psychometric testing, and reference values of the Infant Eating Assessment Tool (InfantEAT). Advances in Neonatal Care 24, 1: E2–E10. [Google Scholar] [CrossRef]
- Pados, B.F., and R.R. Hill. 2024. Reference values for the Gastrointestinal and Gastroesophageal Reflux (GIGER) Scale for Infants and Toddlers. MCN: The American Journal of Maternal/Child Nursing. [Google Scholar] [CrossRef]
- Pados, B.F., J. Johnson, and M. Nelson. 2021. Neonatal Eating Assessment Tool–Mixed Breastfeeding and Bottle-Feeding: Reference values and factors associated with problematic feeding symptoms in healthy, full-term infants. Journal of the American Association of Nurse Practitioners 33, 11: 938–946. [Google Scholar] [CrossRef]
- Pados, B.F., J. Park, and S.M. Thoyre. 2019. Neonatal Eating Assessment Tool—breastfeeding: Reference values for infants less than 7 months old. Journal of Human Lactation 36, 2: 236–244. [Google Scholar] [CrossRef]
- Pados, B.F., J. Park, and S.M. Thoyre. 2019. Neonatal Eating Assessment Tool–Bottle-Feeding: Norm-reference values for infants less than 7 months old. Clinical Pediatrics 58, 8: 857–863. [Google Scholar] [CrossRef]
- Pados, B.F., C. Repsha, and R.R. Hill. 2021. The gastrointestinal and gastroesophageal reflux (GIGER) scale for infants and toddlers. Global Pediatric Health 8: 1–8. [Google Scholar] [CrossRef]
- Pados, B.F., S.M. Thoyre, H. H. Estrem, J. Park, and C. McCormish. 2018. Factor structure and psychometric properties of the Neonatal Eating Assessment Tool-Breastfeeding (NeoEAT-Breastfeeding). Journal of Obstetric, Gynecologic & Neonatal Nursing 47, 3: 396–414. [Google Scholar] [CrossRef]
- Pados, B.F., S.M. Thoyre, H.H. Estrem, J. Park, and C. McComish. 2018. Factor structure and psychometric properties of the Neonatal Eating Assessment Tool-Bottle Feeding (NeoEAT-Bottle feeding). Advances in Neonatal Care 18, 3: 232–242. [Google Scholar] [CrossRef] [PubMed]
- Pados, B.F., S.M. Thoyre, and K. Galer. 2019. Neonatal Eating Assessment Tool-Mixed Breastfeeding and Bottle-Feeding (NeoEAT-Mixed Feeding): Factor analysis and psychometric properties. Matern Heal Neonatol Perinatol 5, 1: 1–15. [Google Scholar] [CrossRef]
- Pransky, S.M., D. Lago, and P. Hong. 2015. Breastfeeding difficulties and oral cavity anomalies: The influence of posterior ankyloglossia and upper-lip ties. International Journal of Pediatric Otorhinolaryngology 79, 10: 1714–1717. [Google Scholar] [CrossRef]
- Shah, S., P. Allen, R. Walker, C. Rosen-Carole, and M.K. Mckenna Benoit. 2021. Upper lip tie: Anatomy, effect on breastfeeding, and correlation with ankyloglossia. The Laryngoscope 131: E1701–E1706. [Google Scholar] [CrossRef] [PubMed]
- Shekher, R., L. Lin, R. Zhang, and et al. 2021. How to treat tongue-tie: An evidence-based algorithm of care. Plastic and Reconstructive Surgery–Global Open 9, 1: e3336. [Google Scholar] [CrossRef]
- Siegel, S.A. 2016. Aerophagia induced reflux in breastfeeding infants with ankyloglossia and shortened maxillary labial frenula (tongue and lip tie). International Journal of Clinical Pediatrics 16, 1: 1369. [Google Scholar]
- Slagter, K.W., G.M. Raghoebar, I. Hamming, J. Meijer, and A. Wissink. 2021. Effect of frenotomy on breastfeeding and reflux: results from the BRIEF prospective longitudinal cohort study. Clinical Oral Investigation 25, 6: 3431–3439. [Google Scholar] [CrossRef]
- Smart, S.J., A. Kittrell, R. Merkel-Walsh, and R.J. Tseng. 2024. International Consortium of oral Ankylofrenula Professionals (ICAP): Practice guidelines for ankylofrenula management. International Journal of Orofacial Myology and Myofunctional Therapy 50, 2: 1–11. [Google Scholar] [CrossRef]
- Talmor, G., and C.L. Caloway. 2022. Ankyloglossia and tethered oral tissue: An evidence-based review. Pediatric Clinics of North America 69, 2: 235–245. [Google Scholar] [CrossRef] [PubMed]
- Tancredi, S., P. De Angelis, M. Marra, and et al. 2022. Clinical comparison of diode laser assisted “v-shape frenectomy” and conventional surgical method as treatment of ankyloglossia. Healthcare (10): 1. [Google Scholar] [CrossRef] [PubMed]
- Walsh, J., and D. Tunkel. 2017. Diagnosis and Treatment of Ankyloglossia in Newborns and Infants: A Review. JAMA Otolaryngology--Head & Neck Surgery 143, 10: 1032–1039. [Google Scholar] [CrossRef]
  |
 |
 |
 |
© 2024 by the author. 2024 Rebecca R. Hill.
Share and Cite
Hill, R.R. Feeding and Gastrointestinal Symptomatology: Comparing Infants Without Oral Restriction to Those with Treated and Untreated Tethered Oral Tissues. Int. J. Orofac. Myol. Myofunct. Ther. 2024, 50, 1-11. https://doi.org/10.52010/ijom.2024.50.2.5
Hill RR. Feeding and Gastrointestinal Symptomatology: Comparing Infants Without Oral Restriction to Those with Treated and Untreated Tethered Oral Tissues. International Journal of Orofacial Myology and Myofunctional Therapy. 2024; 50(2):1-11. https://doi.org/10.52010/ijom.2024.50.2.5
Chicago/Turabian StyleHill, Rebecca R. 2024. "Feeding and Gastrointestinal Symptomatology: Comparing Infants Without Oral Restriction to Those with Treated and Untreated Tethered Oral Tissues" International Journal of Orofacial Myology and Myofunctional Therapy 50, no. 2: 1-11. https://doi.org/10.52010/ijom.2024.50.2.5
APA StyleHill, R. R. (2024). Feeding and Gastrointestinal Symptomatology: Comparing Infants Without Oral Restriction to Those with Treated and Untreated Tethered Oral Tissues. International Journal of Orofacial Myology and Myofunctional Therapy, 50(2), 1-11. https://doi.org/10.52010/ijom.2024.50.2.5




