Abstract
Objective: This project aimed to develop and update a dynamic three-dimensional (3D) graphic video learning object demonstrating a current knowledge of the anatomy and physiology of sucking and swallowing in newborns during breastfeeding. Method: To build and update the 3D computer graphics iconographies of the “Virtual Baby,” we defined objectives for the learning object, created a literature review-based script, and organized a guide for structural (static) and functional (dynamic) graphical modeling for the designer. Results: Using 3D computer graphics, we produced a video with static images (anatomical structural) and dynamic sequences (most significant physiological and functional aspects and application of transparency to visualize the anatomical correlations between both). The video showed the anatomy and physiology of sucking and swallowing during breastfeeding. Its updates reflected additional scientific evidence as studies were published. Conclusion: Creation of the Virtual Baby provides a learning tool for visualizing the anatomy and physiology of sucking and swallowing in full-term newborns. The tool addresses the significant morphofunctional aspects of the breastfeeding process, supported by scientific literature, and can be used for student or professional training and in primary health care.
INTRODUCTION
Breastfeeding is a complex process that requires effective coordination between sucking, swallowing, and breathing (Geddes & Sakalidis, 2016). Such complexity has led several researchers to conduct studies to understand its dynamics. Furthermore, technological advances supporting current research allow for a better understanding of the breastfeeding process better and provide an opportunity to shift paradigms regarding the subject (Elad et al., 2014; Geddes & Sakalidis, 2016; Geddes et al., 2012; Mills et al., 2020; Sakalidis et al., 2013).
Previous understanding of breastfeeding was that milk was extracted through peristaltic tongue movements that would press the nipple against the palate (Adran; Kemp; Lind, 1958; Hayashi; Hoashi; Nara, 1997; Herbst, 1983; Palmer, 1998; Neiva, 2000). However, more recent studies using ultrasonography to analyze the biomechanics of breastfeeding reported that milk secretion happens due to the intraoral vacuum from sucking. This generates negative pressure and is aided by tongue movements, enabling milk to flow out of milk ducts. Then, the tongue’s anterior and middle portions move like a rigid body, and the ensuing vacuum increases as the tongue moves down, expanding the nipple and allowing the milk to flow out. Pressure then normalizes when the tongue returns to the superior position and closer to the palate (Elad et al., 2014; Geddes & Sakalidis, 2016; Geddes et al., 2012; Sakalidis et al., 2013).
For sucking efficiency, the oral cavity is sealed, and the tongue fills most of that space with its sides touching the palate and its center surrounding the nipple (Elad et al., 2014; Geddes et al., 2012; Mills et al., 2020; Sakalidis et al., 2013).
Health organizations recommend that infants be exclusively breastfed until they are approximately six months old; breastfeeding with complementary feeding may continue for up to 2 years or longer (Brazil, 2015; World Health Organization, 2017). There are several benefits for both baby’s and mother’s health, including reduced risk of infant death, protection against infections, allergies, respiratory diseases, diarrhea, necessary nutritional support, and mother and baby bonding. In addition, it is considered an essential factor for the stomatognathic system and orofacial function development (Brazil, 2015; Geddes et al., 2019; Victoria et al., 2016).
Despite the many advantages, studies point to the occurrence of early weaning, which is justified by multiple factors, such as the low level of breastfeeding self-efficacy, the mother’s insecurity, her lack of intention to breastfeed, breastfeeding problems, sociodemographic factors, and the lack of support from health care professionals (Kronborg & Foverskov, 2020; Mangrio et al., 2018; Vargas et al., 2016).
Health professionals’ guidance and counseling on breastfeeding are essential for successful breastfeeding and its increased duration. Performing these effectively favors the mother’s sense of security and increases her effort to overcome difficulties and breastfeed successfully (Alves et al., 2018; Kronborg & Foverskov, 2020).
Academically trained professionals and community health care agents have developed different studies to educate people, especially pregnant and postpartum women, on the benefits of natural breastfeeding for babies’ health and development (Coutinho et al., 2014; Shafaei et al., 2020). In addition, other studies have been performed to train those professionals regarding counseling and health promotion-related actions toward breastfeeding (Buskens e Jaffe, 2008; O’Sullivan et al., 2019; Wallace et al., 2018).
Technological advances enabled many audiovisual resources and educational technologies to support health care guidelines, promotion, and therapies. These serve as strategies to improve patients’ and health care providers’ knowledge and make them agents to empower adherence to recommendations (Adhisivam et al., 2017; Oriá et al., 2018; Silva et al., 2019). Consequently, three-dimensional (3D) computer graphics is one of the fastest-growing technologies in the health sciences, especially when teaching anatomy and physiology (Cemenasco et al., 2004; Petersson et al., 2009; Temkin et al., 2006). Different studies have used models and simulators with that type of resource. (Lara et al., 2020; Vieira et al. 2009). However, none contemplates dynamic 3D computer graphics iconography for breastfeeding-related anatomy and physiology of the baby’s sucking and swallowing.
Recent literature also addresses technological resources to offer health promotion and counseling for families with newborns regarding breastfeeding and newborns’ first care. The resources include video and web conferences, e-learning programs, and email or text message exchanges between families and health care professionals (Chaves et al., 2019; Friesen et al., 2015; Lau et al., 2021; Oriá et al., 2018). However, no study used 3D computer graphics iconography regarding the theme of breastfeeding.
Considering how important it is to understand the breastfeeding process using audiovisual resources to improve the training of health care professionals, students, mothers, and caregivers, this study aimed to develop and update a dynamic 3D graphic video learning object showing newborns’ anatomy and physiology of sucking and swallowing during breastfeeding. It also aims to analyze 3D graphic material content and appearance in the current scientific literature.
METHODS
We developed this research as a multi-disciplinary project to build a learning object called “Virtual Baby.” It was a partnership between the University of São Paulo’s Bauru School of Dentistry’s Department of Speech Therapy (FOB USP) and the University of São Paulo’s Medical School’s Telemedicine class (FMUSP). The first version of the learning object was developed in 2010 and received an update in 2021 to improve content and image. The methodology follows the Virtual Man Project’s precepts, which are three-dimensional modeling of the structures of the human body based on scientific details using 3D computer graphics resources and its conversion into directed and objective knowledge units https://homemvirtual.org.br/projeto/.
We organized a transdisciplinary team with anatomy, speech therapy, medicine, communication, and digital design professionals to develop this project. The team defined a theme to build the educational material in a 3D computer graphics realistic simulator format: the anatomy and physiology of the orofacial myofunctional system of the full-term newborn during breastfeeding. This choice considered the theme’s relevance to primary health care, health education, and public health care.
To guide the digital designer’s structural (static) and functional (dynamic) graphic modeling, we defined the objectives of the learning object, and created a script based on academic bibliographic references. The script focused on describing the anatomy of the newborn’s face, skull, oral cavity, pharynx and esophagus, the mechanisms related to sucking, and the oral and pharyngeal phases of swallowing.
To support the scientific development roadmap of the first Virtual Baby version, we performed a literature review in the Lilacs and MedLine databases and selected scientific works with information on the anatomical and physiological of the sucking and swallowing processes. The keywords were suction, swallowing, breastfeeding, infant, and anatomy.
Additionally, we studied anatomy, physiology, speech therapy, and pediatric dentistry books, anatomy atlases, photos, skeletons of newborns and fetuses in different gestational periods preserved in vitro, as well as videofluoroscopy videos (swallowing dynamics assessment via radiological imaging), and dynamic ultrasound images of the oral cavity during suction and swallowing. Finally, we examined computed tomography scans for morphofunctional details of the orofacial myofunctional system.
To prepare for the updated version of the Virtual Baby, we conducted a second bibliographical review to update and improve its content and image, covering the MedLine, Lilacs, and PubMed databases. In addition, we paired the following Portuguese and English descriptors/ keywords to check for representativeness of all items: anatomy, physiology, sucking behavior, swallowing, newborn, and breastfeeding.
Studies selected for informational content included full-term and healthy babies with no neurological changes or craniofacial anomalies. Excluded studies involved preterm babies with ankyloglossia, patients with neurological diseases, chromosomal syndromes, craniofacial anomalies, or any anatomical changes that could interfere with breastfeeding.
Article analysis considered casuistry, evaluation procedures, methodology, and results related to the anatomical and physiological aspects of sucking and swallowing during breastfeeding in full-term newborns. The selected studies were classified according to their level of scientific evidence, as follows: evidence resulting from the meta-analysis of multiple randomized controlled clinical trials (Level 1); evidence from individual studies with experimental design (Level 2); evidence from quasi-experimental studies (Level 3); evidence of descriptive (non-experimental) studies or with a qualitative approach (Level 4); evidence from case reports or experience (Level 5); evidence based on specialist’s opinions (Level 6) (Souza et al., 2010).
Script development allowed the designer to build scientific evidence-based iconographies in 3D computer graphics, whose production was divided into modeling, animation, texturing, lighting, rendering, composition, and post-production. The programs used were 3DS Max 2010, ZBrush 3.5, Photoshop CS4, and After Effects CS4. Regarding the technological infrastructure, the following resources were available: Core 2 Quad Q8200 Processor (Speed: 2.33 GHz / FSB: 1333 Mhz / L2 Cache: 4 Mb / Technology: 45 NM); 4 GB DDR2 800 Kingston Memory (two 2 GB DDR800 Kingston PC 6400 Dual Channel models); Geforce 9500 GT 1GB Video Card (1024Mb/128Bit GDDR2 PCI-Ex 16X/DVI TV OUT/DX10 - Shader 4.0); 500GB 7200 RPM SATA 2 hard drive; two LCD widescreen 18.5-inch 933sn Samsung monitors; Wacom Bamboo Pen Ctl-460 tablet.
RESULTS
The script that guided the preparation of the 3D iconographies was created based on the literature review, which included a survey that included 14 publications with six scientific articles and eight book chapters (Table 1). These materials helped guide our representation of the breastfeeding process into two sections: the first contains descriptions and information about the anatomy of the newborns’ face, skull, oral cavity, pharynx and esophagus; and the second addresses the description of the physiological mechanisms related to sucking and swallowing during breastfeeding.

Table 1.
Literature review regarding the anatomophysiological aspects of sucking and swallowing in full-term newborns.
Upon completing the academic bibliographic reference-based script, the designer created the 3D iconographies for the Virtual Baby’s anatomy and physiology of sucking and swallowing. This stage included interactions between health care professionals and digital designers so they could discuss the script information, analyze and revise image details, and confirm the accuracy of the final product regarding newborns anatomy.
The Virtual Baby was updated in 2021 to ensure improved content and more detailed images and content. The update included a new bibliographic review with 11 updated articles that relied on the use of technologies to educate on the breastfeeding process (Table 2 and Table 3). As indicated in Table 2, the studies’ levels of evidence ranged from 2 to 4; level 3 was the most frequent. Updating the computer graphics involved meetings between health professionals and digital designers to ensure material quality and reliability.

Table 2.
Bibliographic references on the anatomical and physiological aspects of sucking and swallowing in full-term newborns.

Table 3.
Selected articles that used technological tests for the baby’s virtual suitability.
Considering the selected theoretical framework, sucking and swallowing adjustment for the Virtual Baby was performed in five steps described in Table 4. This progression allowed the educational 3D model to come closer to the reality indicated by the current literature.

Table 4.
Adjustments in sucking and swallowing for the Virtual Baby.
Figure 1 and Figure 2 correspond to the images of the first version of Virtual Baby. Figure 3, Figure 4 and Figure 5 show the current model during breastfeeding. In addition, a video clip of the Virtual Baby model as an embedded and downloadable link is available on this article’s homepage (https://ijom.iaom.com/journal/vol48/iss1/4/).
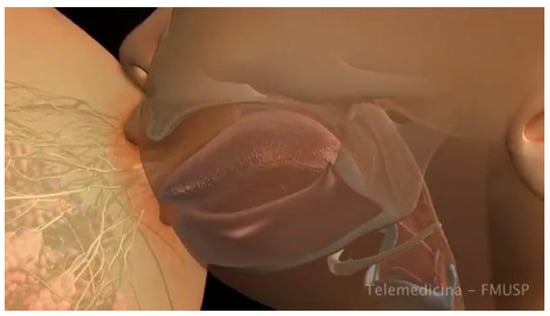
Figure 1.
Image of nipple attachment in the first version of Virtual Baby.

Figure 2.
Image of sucking movement in the first version of Virtual Baby.

Figure 3.
Image of nipple attachment and early sucking movement in the Virtual Baby.

Figure 4.
Tongue lowers and nipple diameter increases while sucking in the Virtual Baby.
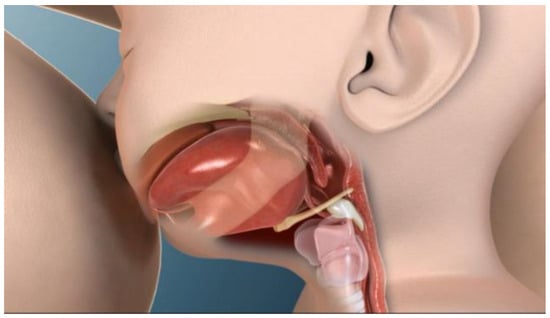
Figure 5.
Swallowing pharyngeal phase in the Virtual Baby.
DISCUSSION
This project developed both the content and appearance of a learning object that shows the mechanisms involved in breastfeeding. An interdisciplinary team created and modeled the Virtual Baby’s breastfeeding 3D computer graphics based on reviewing and analyzing studies published in scientific journals and anatomy and physiology books. The analysis of this theoretical framework showed that the first studies on sucking during breastfeeding were performed using cineradiography (Adran et al., 1958). In addition, the authors reported that the tongue performs peristaltic movements during sucking (Adran et al., 1958), and these findings were later reproduced in other studies (Hayashi et al., 1997; Herbst, 1983; Neiva, 2000; Palmer, 1998) over many years.
Technological evolution enabled current studies to show that the tongue, composed of striated skeletal musculature, does not perform peristaltic movements (Elad et al., 2014; Geddes et al., 2012) since such movement can only be performed by smooth musculature and undulatory movements similar to peristaltic waves.
Milk is not secreted when the tongue is pressing the nipple but rather by the vacuum created in the oral cavity as a result of tongue movements (Elad et al., 2014; Geddes & Sakalidis, 2016; Geddes et al., 2012; Mills et al., 2020; Sakalidis et al., 2013a). The baby’s grip needed for anterior sealing helps create a vacuum and prevents milk from escaping through the mouth (Tamilla et al., 2014). A vacuum begins to form when the middle portion of the tongue rises and comes into contact with the hard palate. When the tongue descends, the vacuum and nipple diameter increase, and milk flows into the oral cavity (Geddes & Sakalidis, 2016; Geddes et al., 2012; Sakalidis et al., 2013). During sucking, the nipple moves towards the junction of the hard and soft palates but does not extend to this junction, remaining a few millimeters away (Elad et al., 2014; Geddes & Sakalidis, 2016; Geddes et al., 2012; Sakalidis et al., 2013a).
Once milk is expressed from the nipple, it is directed from the oral cavity to the pharynx, initiating the pharyngeal phase of swallowing. At this point, the velopharynx closes to ensure that the milk does not enter the nasopharynx; finally, the larynx elevates. The fluid is then transferred to the esophagus with the aid of constricting movements of the pharyngeal muscles. The esophageal phase begins when food passes through the upper esophageal sphincter on its way to the stomach (Lau, 2015; Mills et al., 2020).
Current studies performed based on instrumental methods served to create the Virtual Baby’s 3D computer graphics. In addition, they allowed us to develop a learning object based on up-to-date scientific evidence.
Initially, the Virtual Baby’s first version had a sequence of dynamic 3D iconographies picturing the baby latching on. Then the forward tongue movement was associated with the forward mandibular movement for milk extraction. Lastly, the swallowing movement occurred along with laryngeal elevation and velopharyngeal closure.
We changed the sequence in the second version after updating the studies on the newborns’ anatomy and physiology of sucking and swallowing. As a result, there were adjustments in the synchronization between sucking, swallowing, and breathing, improved sliding of mandibular movement during suction, increased video speed for more realistic results, synchronized tongue movements with peak vacuum and increased nipple expansion and larynx elevation during swallowing. The update also included a video demonstrating improved nipple latching.
Future work is needed to validate the developed material. In addition, we recommend developing additional tools for babies with or at risk for developing orofacial myofunctional disorders, such as those with a cleft lip or cleft palate, those born prematurely, babies with Down syndrome, and those with ankyloglossia.
The Virtual Baby learning object can be applied in education and health promotion strategies, both for formal education and interactive tele-education. It has the potential to contribute to the training of students and health professionals and to benefit patients’ health.
CONCLUSION
This original and innovative project produced both the content and appearance of a dynamic 3-dimensional graphical learning object created to demonstrate the anatomy and physiology of sucking and swallowing in full-term newborns. In addition, the tool addresses the significant morphofunctional aspects of the breastfeeding process, which are consistent with current scientific literature and can be used for professional training or in primary health care.
Author Contributions
Conceptualization: C.L.W.; Study design: F.R.P., A.d.C.R., S.R.-M., R.L.d.C.M. and G.B.-F.; Interpretation: F.R.P., M.G. and S.R.-M.; Drafting: F.R.P., M.G. and S.R.-M.; Critical revision: A.d.C.R., C.L.W., R.L.d.C.M. and G.B.-F.
References
- Adhisivam, B., B. Vishnu Bhat, R. Poorna, M. Thulasingam, F. Pournami, and R. Joy. 2017. Postnatal counseling on exclusive breastfeeding using video—Experience from a tertiary care teaching hospital, South India. The Journal of Maternal-Fetal & Neonatal Medicine: The Official Journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians 30, 7: 834–838. [Google Scholar] [CrossRef]
- Alves, J. S., M. I. C. Oliveira, and R. V. V. F. Rito. 2018. Orientações sobre amamentação na atenção básica de saúde e associação com o aleitamento materno exclusivo. Revista Ciência & Saúde Coletiva 23, 4: 1077–1088. [Google Scholar] [CrossRef]
- Ardran, G. M., F. H. Kemp, and J. Lind. 1958. A cineradiographic study of bottle feeding. The British Journal of Radiology 31, 361: 11–22. [Google Scholar] [CrossRef]
- Behlau, M., R. Azevedo, and G. Madazio. 2001. Edited by M. Behlau. Anatomia da laringe e fisiologia da produção vocal. In Voz: O livro do especialista vol. I. Rio de Janeiro: Revinter. [Google Scholar]
- Brasil. 2015. Saúde da criança: Aleitamento materno e alimentação complementar. Brasília: Ministério da Saúde. [Google Scholar]
- Burton, P., J. Deng, D. McDonald, and M. S. Fewtrell. 2013. Real-time 3D ultrasound imaging of infant tongue movements during breast-feeding. Early Human Development 89, 9: 635–641. [Google Scholar] [CrossRef]
- Buskens, I., and A. Jaffe. 2008. Demotivating infant feeding counselling encounters in southern Africa: Do counsellors need more or different training? AIDS Care 20, 3: 337–345. [Google Scholar] [CrossRef] [PubMed]
- Cannon, A. M., V. S. Sakalidis, C. T. Lai, S. L. Perrella, and D. T. Geddes. 2016. Vacuum characteristics of the sucking cycle and relationships with milk removal from the breast in term infants. Early Human Development 96: 1–6. [Google Scholar] [CrossRef]
- Cemenasco, A. F., C. C. Bianchi, S. Tornincasa, and S. D. Bianchi. 2004. The WEBD project: A research of new methodologies for a distant-learning 3D system prototype. Dento Maxillo Facial Radiology 33, 6: 403–408. [Google Scholar] [CrossRef]
- Chaves, A., L. B. Ximenes, D. P. Rodrigues, C. Vasconcelos, J. Monteiro, and M. Oriá. 2019. Telephone intervention in the promotion of self-efficacy, duration and exclusivity of breastfeeding: Randomized controlled trial. Intervenção telefônica na promoção da autoeficácia, duração e exclusividade do aleitamento materno: Estudo experimental randomizado controlado. Revista Latino-americana de Enfermagem 27: e3140. [Google Scholar] [CrossRef]
- Costas, M., S. Santos, C. Godoy, and M. Martell. 2006. Patrones de succión en el recién nacido de término y pretérmino. Revista Chilena de Pediatría 77, 2: 198–212. [Google Scholar] [CrossRef]
- Coutinho, S. B., P. I. Lira, M. C. Lima, P. G. Frias, S. H. Eickmann, and A. Ashworth. 2014. Promotion of exclusive breast-feeding at scale within routine health services: Impact of breast-feeding counselling training for community health workers in Recife, Brazil. Public Health Nutrition 17, 4: 948–955. [Google Scholar] [CrossRef]
- da Costa, S. P., C. P. van der Schans, S. R. Boelema, E. van der Meij, M. A. Boerman, and A. F. Bos. 2010. Sucking patterns in full term infants between birth and 10 weeks of age. Infant Behavior & Development 33, 1: 61–67. [Google Scholar] [CrossRef]
- Derkay, C. S., and G. L. Schechter. 1998. Anatomy and physiology of pediatric swallowing disorders. Otolaryngologic Clinics of North America 31, 3: 397–404. [Google Scholar] [CrossRef] [PubMed]
- Douglas, C. R. 2006. Fisiologia aplicada à Fonoaudiologia. Guanabara. [Google Scholar]
- Elad, D., P. Kozlovsky, O. Blum, A. F. Laine, M. J. Po, E. Botzer, S. Dollberg, M. Zelicovich, and L. Ben Sira. 2014. Biomechanics of milk extraction during breast-feeding. Proceedings of the National Academy of Sciences of the United States of America 111, 14: 5230–5235. [Google Scholar] [CrossRef] [PubMed]
- Friesen, C. A., L. J. Hormuth, D. Petersen, and T. Babbitt. 2015. Using Videoconferencing Technology to Provide Breastfeeding Support to Low-Income Women: Connecting Hospital-Based Lactation Consultants with Clients Receiving Care at a Community Health Center. Journal of human lactation: Official journal of International Lactation Consultant Association 31, 4: 595–599. [Google Scholar] [CrossRef]
- Geddes, D. T., L. M. Chadwick, J. C. Kent, C. P. Garbin, and P. E. Hartmann. 2010. Ultrasound imaging of infant swallowing during breast-feeding. Dysphagia 25, 3: 183–191. [Google Scholar] [CrossRef]
- Geddes, D. T., J. C. Kent, L. R. Mitoulas, and P. E. Hartmann. 2008. Tongue movement and intra-oral vacuum in breastfeeding infants. Early Human Development 84, 7: 471–477. [Google Scholar] [CrossRef]
- Geddes, D., and S. Perrella. 2019. Breastfeeding and Human Lactation. Nutrients 11, 4: 802. [Google Scholar] [CrossRef]
- Geddes, D. T., and V. S. Sakalidis. 2016. Ultrasound Imaging of Breastfeeding--A Window to the Inside: Methodology, Normal Appearances, and Application. Journal of Human Lactation: Official Journal of International Lactation Consultant Association 32, 2: 340–349. [Google Scholar] [CrossRef]
- Geddes, D. T., V. S. Sakalidis, A. R. Hepworth, H. L. McClellan, J. C. Kent, C. T. Lai, and P. E. Hartmann. 2012. Tongue movement and intra-oral vacuum of term infants during breastfeeding and feeding from an experimental teat that released milk under vacuum only. Early Human Development 88, 6: 443–449. [Google Scholar] [CrossRef]
- World Health Organization. 2017. Guideline: Protecting, Promoting and Supporting Breastfeeding in Facilities Providing Maternity and Newborn Services. World Health Organization. [Google Scholar]
- Hayashi, Y., E. Hoashi, and T. Nara. 1997. Ultrasonographic analysis of sucking behavior of newborn infants: The driving force of sucking pressure. Early Human Development 49, 1: 33–38. [Google Scholar] [CrossRef]
- Herbst, J. J. 1983. Development of suck and swallow. Journal of Pediatric Gastroenterology and Nutrition 2 Suppl. S1: S131–S135. [Google Scholar] [CrossRef]
- Kronborg, H., and E. Foverskov. 2020. Multifactorial influence on duration of exclusive breastfeeding; a Danish cohort study. PLoS ONE 15, 9: e0238363. [Google Scholar] [CrossRef] [PubMed]
- Lang, W. C., N. R. Buist, A. Geary, S. Buckley, E. Adams, A. C. Jones, S. Gorsek, S. C. Winter, H. Tran, and B. R. Rogers. 2011. Quantification of intraoral pressures during nutritive sucking: Methods with normal infants. Dysphagia 26, 3: 277–286. [Google Scholar] [CrossRef] [PubMed]
- Lara, J. S., M. M. Braga, C. G. Zagatto, C. L. Wen, F. M. Mendes, P. U. Murisi, and A. E. Haddad. 2020. A Virtual 3D Dynamic Model of Caries Lesion Progression as a Learning Object for Caries Detection Training and Teaching: Video Development Study. JMIR Medical Education 6, 1: e14140. [Google Scholar] [CrossRef] [PubMed]
- Lau, C. 2015. Development of Suck and Swallow Mechanisms in Infants. Annals of Nutrition & Metabolism 66, Suppl. S505: 7–14. [Google Scholar] [CrossRef]
- Lau, J. D., Y. Zhu, and S. Vora. 2021. An Evaluation of a Perinatal Education and Support Program to Increase Breastfeeding in a Chinese American Community. Maternal and Child Health Journal 25, 2: 214–220. [Google Scholar] [CrossRef]
- Madeira, M. C. 2008. Anatomia da face, 2nd ed. São Paulo: Sarvier. [Google Scholar]
- Mangrio, E., K. Persson, and A. C. Bramhagen. 2018. Sociodemographic, physical, mental and social factors in the cessation of breastfeeding before 6 months: A systematic review. Scandinavian Journal of Caring Sciences 32, 2: 451–465. [Google Scholar] [CrossRef]
- Marchesan, I. Q. 1998. Edited by I. Q. Marchesan. Avaliação e terapia dos problemas da respiração. In Fundamentos em fonoaudiologia: Aspectos clínicos da motricidade oral. Rio de Janeiro: Guanabara Koogan, pp. 23–36. [Google Scholar]
- McClellan, H. L., A. R. Hepworth, J. C. Kent, C. P. Garbin, T. M. Williams, P. E. Hartmann, and D. T. Geddes. 2012. Breastfeeding frequency, milk volume, and duration in mother-infant dyads with persistent nipple pain. Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine 7: 275–281. [Google Scholar] [CrossRef]
- McClellan, H. L., V. S. Sakalidis, A. R. Hepworth, P. E. Hartmann, and D. T. Geddes. 2010. Validation of nipple diameter and tongue movement measurements with B-mode ultrasound during breastfeeding. Ultrasound in Medicine & Biology 36, 11: 1797–1807. [Google Scholar] [CrossRef]
- Mills, N., A. M. Lydon, D. Davies-Payne, M. Keesing, D. T. Geddes, and S. A. Mirjalili. 2020. Imaging the breastfeeding swallow: Pilot study utilizing real-time MRI. Laryngoscope Investigative Otolaryngology 5, 3: 572–579. [Google Scholar] [CrossRef]
- Moreira, M. A. 1999. A pesquisa em educaçao em Ciencias a formaçao permanente do professor de Ciencias. In Educación Científica: Conferencias, Mesas de Debate Y Secciones. Editorial Universidad de Alcalá: pp. 71–80. [Google Scholar]
- Moreira, A. D. S. 2003. Cultura midiática e educação infantil. Educação & Sociedade 24, 85: 1203–1235. [Google Scholar]
- Morris, S. E. 1998. Issues in the Anatomy and Physiology of Swallowing: Impact on the Assessment and Treatment of Children with Dysphagia. Retrieved from https://www.new-vis.com/.
- Neiva, F. C. B. 2000. Sucção em recém-nascidos: Algumas contribuições da fonoaudiologia. Pediatria (São Paulo) 22, 3: 264–70. [Google Scholar]
- Oriá, M., H. D. Dodou, A. Chaves, L. Santos, L. B. Ximenes, and C. Vasconcelos. 2018. Effectiveness of educational interventions conducted by telephone to promote breastfeeding: A systematic review of the literature. Eficácia de intervenções educativas realizadas por telefone para promoção do aleitamento materno: Revisão sistemática da literatura. Revista da Escola de Enfermagem da U S P 52, e03333. [Google Scholar] [CrossRef]
- O’Sullivan, T. A., J. Cooke, C. McCafferty, and R. Giglia. 2019. Online Video Instruction on Hand Expression of Colostrum in Pregnancy is an Effective Educational Tool. Nutrients 11, 4: 883. [Google Scholar] [CrossRef]
- Palmer, B. 1998. The influence of breastfeeding on the development of the oral cavity: A commentary. Journal of human lactation: Official journal of International Lactation Consultant Association 14, 2: 93–98. [Google Scholar] [CrossRef] [PubMed]
- Pérez Navarro, N., and M. López. 2002. Anquiloglosia en niños de 5 a 11 años de edad: Diagnóstico y tratamiento. Revista Cubana de Estomatología 39, 3: 282–301. [Google Scholar]
- Petersson, H., D. Sinkvist, C. Wang, and O. Smedby. 2009. Web-based interactive 3D visualization as a tool for improved anatomy learning. Anatomical Sciences Education 2, 2: 61–68. [Google Scholar] [CrossRef]
- Shafaei, F. S., M. Mirghafourvand, and S. Havizari. 2020. The effect of prenatal counseling on breastfeeding self-efficacy and frequency of breastfeeding problems in mothers with previous unsuccessful breastfeeding: A randomized controlled clinical trial. BMC Women’s Health 20, 1: 94. [Google Scholar] [CrossRef]
- Sakalidis, V. S., T. M. Williams, C. P. Garbin, A. R. Hepworth, P. E. Hartmann, M. J. Paech, and D. T. Geddes. 2013. Ultrasound imaging of infant sucking dynamics during the establishment of lactation. Journal of Human Lactation: Official Journal of International Lactation Consultant Association 29, 2: 205–213. [Google Scholar] [CrossRef]
- Sakalidis, V. S., T. M. Williams, A. R. Hepworth, C. P. Garbin, P. E. Hartmann, M. J. Paech, Y. Al-Tamimi, and D. T. Geddes. 2013. A comparison of early sucking dynamics during breastfeeding after cesarean section and vaginal birth. Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine 8, 1: 79–85. [Google Scholar] [CrossRef]
- Sanches, M. T. 2004. Manejo clínico das disfunções orais na amamentação [Clinical management of oral disorders in breastfeeding]. Jornal de Pediatria 80 Suppl. S5: S155–S162. [Google Scholar] [CrossRef] [PubMed]
- Silva, N. V. N., C. M. Pontes, N. F. C. Sousa, and M. G. L. Vasconcelos. 2019. Tecnologias em saúde e suas contribuições para a promoção do aleitamento materno: Revisão integrativa da literatura. Revista Ciência & Saúde Coletiva 24, 2: 589–602. [Google Scholar] [CrossRef]
- Souza, M. T., M. D. Silva, and R. d. Carvalho. 2010. Integrative review: What is it? How to do it? Sao Paulo, Brazil) 8, 1: 102–106. [Google Scholar] [CrossRef]
- Tamilia, E., F. Taffoni, D. Formica, L. Ricci, E. Schena, F. Keller, and E. Guglielmelli. 2014. Technological solutions and main indices for the assessment of newborns’ nutritive sucking: A review. Sensors (Basel, Switzerland) 14, 1: 634–658. [Google Scholar] [CrossRef]
- Tavano, P. T. 2008. Anatomia do recém nascido e da criança: Características gerais. Ensaios e Ciência: Ciências Biológicas, Agrárias e da Saúde 12, 1: 63–75. [Google Scholar]
- Temkin, B., E. Acosta, A. Malvankar, and S. Vaidyanath. 2006. An interactive three-dimensional virtual body structures system for anatomical training over the internet. Clinical anatomy (New York, N.Y.) 19, 3: 267–274. [Google Scholar] [CrossRef]
- Vargas, G. S. A., V. H. Alves, D. P. Rodrigues, M. B. L. R. Branco, R. de M. P. de Souza, and J. V. V. Guerra. 2016. Atuação dos profissionais de saúde da estratégia saúde da família: Promoção da prática do aleitamento materno. Revista Baiana de Enfermagem 30, 2: 1–9. [Google Scholar] [CrossRef]
- Victora, C. G., R. Bahl, A. J. Barros, G. V. França, S. Horton, J. Krasevec, S. Murch, M. J. Sankar, N. Walker, N. C. Rollins, and Lancet Breastfeeding Series Group. 2016. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet (London, England) 387, 10017: 475–490. [Google Scholar] [CrossRef]
- Vieira, M. M. R. M., G. Berretin-Felix, and A. G. Brasolotto. 2009. The Virtual Man Project’s CD-ROM” Voice assessment: Speech-Language Pathology and Audiology & Medicine”, Vol. 1. Journal of Applied Oral Science 17, SPE: 43–49. [Google Scholar] [CrossRef]
- Villena, R. S., and M. S. N. P. Corrêa. 1998. Edited by M. S. N. P. Corrêa. Flúor: Aplicação tópica na primeira infância. In Odontopediatria na primeira infância. São Paulo: Santos, pp. 316–342. [Google Scholar]
- Wallace, L. M., Y. Ma, L. Q. Qiu, and O. M. Dunn. 2018. Educational videos for practitioners attending Baby Friendly Hospital Initiative workshops supporting breastfeeding positioning, attachment and hand expression skills: Effects on knowledge and confidence. Nurse Education in Practice 31: 7–13. [Google Scholar] [CrossRef]
Notes and Disclosures: This study was conducted at Bauru School of Dentistry, University of São Paulo - FOB/USP, Bauru (São Paulo), Brazil. No authors have relevant declarations of interest or financial disclosures. |
© 2022 by the authors. 2022 Flávia Rebelo Puccini, Marina Gatti, Antônio de Castro Rodrigues, Silmara Rondon-Melo, Chao Lung Wen, Roberta Lopes de Castro Martinelli, Giédre Berretin-Felix.