Orofacial Myofunctional Assessments in Adults with Malocclusion: A Scoping Review
Abstract
:INTRODUCTION
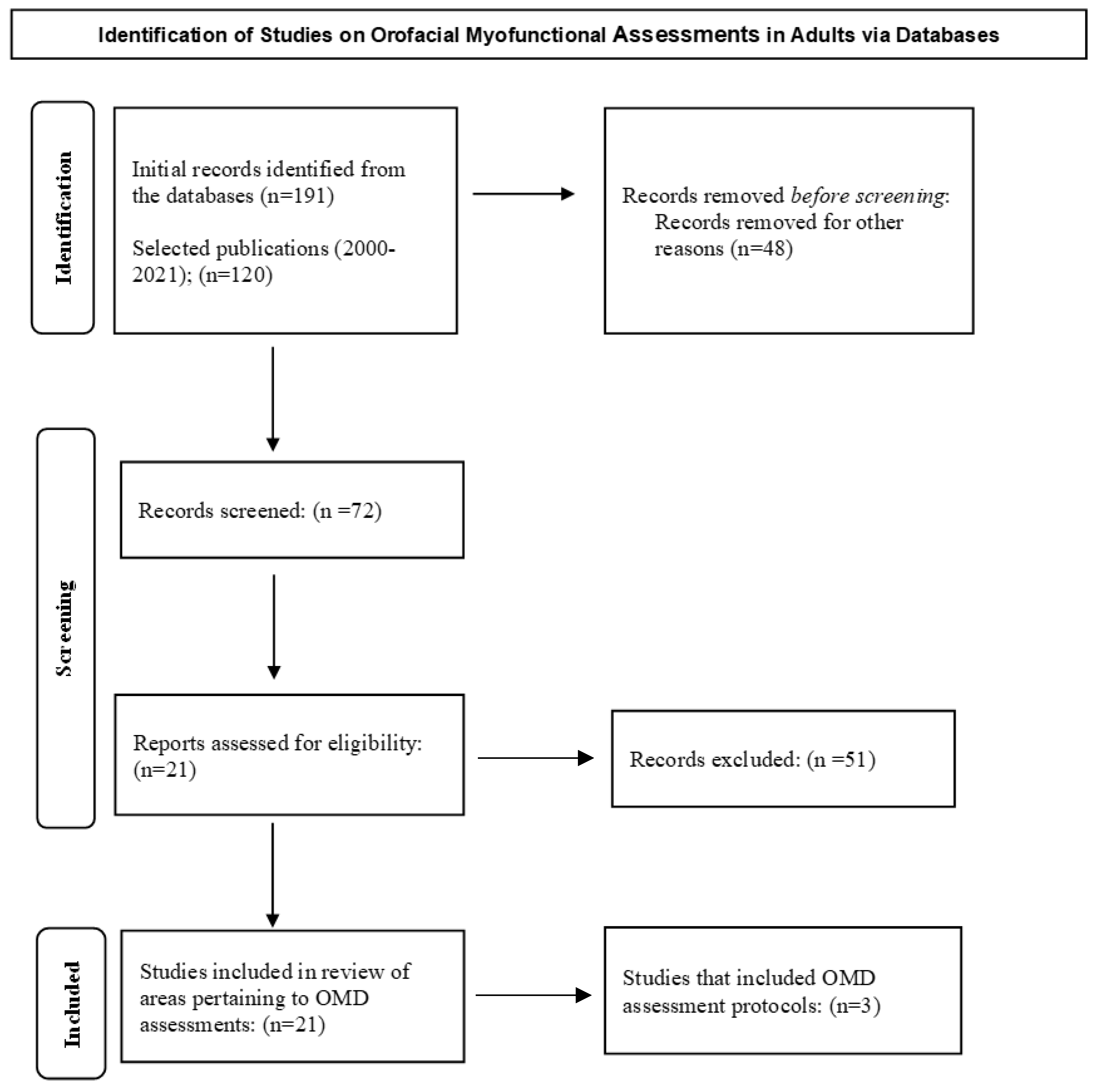
METHODS
Inclusionary and Exclusionary Criteria
RESULTS AND DISCUSSION
Non-Instrumental Assessment Protocols for Adults
Target Areas of Noninstrumental Assessment of OMD in Adults with Malocclusion
Case History
Oral habits
Visualization of Hard and Soft Tissues
Mandible and Chewing Functions
Sleep Patterns
Airway Functions
Dental Status
Tongue Functions
Articulation Problems
CONCLUSIONS, LIMITATIONS, AND FUTURE RESEARCH
References
- American Speech-Language-Hearing Association. 2021. Orofacial Myofunctional Disorders. Retrieved from https://www.asha.org/practice-portal/clinical-topics/orofacial-myofunctional-disorders/.
- Angle, E. 1907. Malocclusion of the Teeth, 7th ed. The S.S. White Dental Manufacturing Co. [Google Scholar]
- Bakke, M., B. Bergendal, A. McAllister, L. Sjögreen, and P. Asten. 2007. Development and evaluation of a comprehensive screening for orofacial dysfunction. Swedish Dental Journal 31, 2: 75–84. [Google Scholar] [PubMed]
- Banabihl, S. M. 2017. Orthodontic view in the diagnoses of obstructive sleep apnea. Journal of Orthodontic Science 6, 3: 81–85. [Google Scholar] [CrossRef]
- Benkert, K. K. 1997. The effectiveness of orofacial myofunctional therapy in improving dental occlusion. International Journal of Orofacial Myology 23: 35–46. [Google Scholar] [CrossRef] [PubMed]
- Bergendal, B., M. Bakke, A. McAllister, L. Sjögreen, and P. Åsten. 2014. Profiles of orofacial dysfunction in different diagnostic groups using the Nordic Orofacial Test (NOT-S): A review. Acta Odontology Scandinavia 72, 8: 578–584. [Google Scholar] [CrossRef]
- Campbell, S., and G. Goldstein. 2021. Angle’s Classification-A prosthodontic consideration: Best evidence consensus statement. Journal of Prosthodontics 30, S1: 67–71. [Google Scholar] [CrossRef] [PubMed]
- D’Onofrio, L. 2019. Oral dysfunction as a cause of malocclusion. Orthodontics & Craniofacial Research 22 Suppl. 1: 43–48. [Google Scholar] [CrossRef]
- de Felício, C. M., and C. L. Ferreira. 2008. Protocol of orofacial myofunctional evaluation with scores. International Journal of Pediatric Otorhinolaryngology 72, 3: 367–375. [Google Scholar] [CrossRef]
- de Felicio, C.M., A.P. Medeiros, and M. M. de Oliveira. 2012. Validity of the protocol of orofacial myofunctional evaluation with scores for young and adult subjects. Journal of Oral Rehabilitation 39, 10: 744–753. [Google Scholar] [CrossRef]
- Dellepiane, E., F. Pera, P. Zunino, M.G. Mugno, P. Pesce, and M. Menini. 2020. Oral health-related quality of life and full-arch immediate loading rehabilitation: An evaluation of preoperative, intermediate, and posttreatment assessments of patients using a modification of the OHIP questionnaire. Journal of Oral Implantology 46, 6: 540–549. [Google Scholar] [CrossRef]
- Elfseyie, M., M. Hassan, N. Mohammed, and A. Al-Jaf. 2020. Prevalence of malocclusion and occlusal traits of Malay adults (18–23 years) in Shah Alam, Malaysia. International Journal of Dentistry Research, 81–86. [Google Scholar] [CrossRef]
- Ferreira, C. L., M. A. Da Silva, and C. M. de Felício. 2009. Orofacial myofunctional disorder in subjects with temporomandibular disorder. Cranio 27, 4: 268–274. [Google Scholar] [CrossRef] [PubMed]
- Grandi, D. 2012. The “Interdisciplinary Orofacial Examination Protocol for Children and Adolescents”: A resource for the interdisciplinary assessment of the stomatognathic system. International Journal of Orofacial Myology 38: 15–26. [Google Scholar] [CrossRef] [PubMed]
- Hale, S. T., G. D. Kellum, V. M. Nason, and M. A. Johnson. 1988. Analysis of orofacial myofunctional factors in kindergarten subjects. International Journal of Orofacial Myology 14, 3: 12–15. [Google Scholar] [CrossRef]
- Hitos, S. F., R. Arakaki, D. Solé, and L. L. Weckx. 2013. Oral breathing and speech disorders in children. Journal of Pediatrics 89, 4: 361–365. [Google Scholar] [CrossRef]
- Ihan Hren, N., and U. Barbič. 2016. Tongue volume in adults with skeletal Class III dentofacial deformities. Head & Face Medicine 12: 12. [Google Scholar] [CrossRef]
- Indriksone, I., and G. Jakobsone. 2014. The upper airway dimensions in different sagittal craniofacial patterns: A systematic review. Stomatologija 16, 3: 109–117. [Google Scholar] [PubMed]
- Junqueira, P., I. Q. Marchesan, L. R. de Oliveira, E. Ciccone, L. Haddad, and M. C. Rizzo. 2010. Speech-language pathology findings in patients with mouth breathing: Multidisciplinary diagnosis according to etiology. International Journal of Orofacial Myology 36: 27–32. [Google Scholar] [CrossRef]
- Kamdar, R. J., and I. Al-Shahrani. 2015. Damaging oral habits. Journal of International Oral Health 7, 4: 85–87. [Google Scholar] [PubMed]
- Kondo, E., and T. J. Aoba. 1999. Case report of malocclusion with abnormal head posture and TMJ symptoms. American Journal of Orthodontics and Dentofacial Orthopedics 116, 5: 481–493. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-S., J. Ryu, S.-H. Baek, W. H. Lim, I.-H. Yang, T.-W. Kim, and S.-K. Jung. 2021. Comparative analysis of the differences in dentofacial morphology according to the tongue and lip pressure. Diagnostics 11, 3: 503. [Google Scholar] [CrossRef]
- Lichnowska, A., and M. Kozakiewicz. 2021a. The effectiveness of frenotomy on speech in adults. Applied Science 11: 2727. [Google Scholar] [CrossRef]
- Lichnowska, A., and M. Kozakiewicz. 2021b. The logopedic evaluation of adult patients after orthognathic surgery. Applied Science 11: 5732. [Google Scholar] [CrossRef]
- Lopatiene, K., M. Borisovaite, and E. Lapenaite. 2016. Prevention and treatment of white spot lesions during and after treatment with fixed orthodontic appliances: A systematic literature review. Journal of Oral & Maxillofacial Research 7, 2. [Google Scholar] [CrossRef]
- Macedo, P. F., and E. M. Bianchini. 2014. Myofunctional orofacial examination: Comparative analysis in young adults with and without complaints. Codas 26, 6: 464–470. [Google Scholar] [CrossRef]
- Marchesan, I. Q., G. Berretin-Felix, and K. F. Genaro. 2012. MBGR Protocol of orofacial myofunctional evaluation with scores. International Journal of Orofacial Myology 38, 1: 38–77. [Google Scholar] [CrossRef]
- Menezes, L. F., A. M. da Rocha, C. E. B. Paulino, J. R. Laureano, and L. M. Studart-Pereira. 2018. Tongue pressure and endurance in patients with Class II and Class III malocclusion. Revista CEFAC 20, 2: 166–174. [Google Scholar] [CrossRef]
- Mokhtar, K. I., N. A. Bakar, and A. H. M. A. Tahir. 2020. Genetics of malocclusion: A review. IIUM Journal of Orofacial and Health Sciences 1, 1: 1–6. [Google Scholar] [CrossRef]
- Moyers, R. 1988. Handbook of orthodontics. Yearbook Medical Publisher. [Google Scholar]
- Page, M. J., J. E. McKenzie, P. M. Bossuyt, I. Boutron, T. C. Hoffmann, C. D. Mulrow, L. Shamseer, J. M. Tetzlaff, E. A. Akl, S. E. Brennan, R. Chou, J. Glanville, J. M. Grimshaw, A. Hróbjartsson, M. M. Lalu, T. Li, E. W. Loder, E. Mayo-Wilson, S. McDonald, L. A. McGuinness, and D. Moher. 2021. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ (Clinical Research ed.) 372: n71. [Google Scholar] [CrossRef]
- Paskay, L. C. 2012. A one-page orofacial myofunctional assessment form: A proposal. International Journal of Orofacial Myology 38, 1: 27–37. [Google Scholar] [CrossRef]
- Prado, D. G. A., H. N. Filho, G. Berretin-Felix, and A. G. Brasalotto. 2014. Breathing characteristics of individuals with dentofacial deformity. Revista CEFAC 16, 4: 1194–1200. [Google Scholar] [CrossRef]
- Rapeepattana, S., A. Thearmontree, and S. Suntornlohanakul. 2019. Etiology of malocclusion and dominant orthodontic problems in mixed dentition: A cross-sectional study in a group of Thai children aged 8–9 years. Journal of International Society of Preventive & Community Dentistry 9, 4: 383–389. [Google Scholar] [CrossRef]
- Ruf, S., P. Proff, and J. Lisson. 2021. Tooth and jaw misalignments-health relevance and treatment. Federal Health Gazette, Health Research, Health Protection 64, 8: 918–923. [Google Scholar] [CrossRef]
- Scarponi, L., C. M. de Felicio, C. Sforza, C. L. Pimenta Ferreira, D. Ginocchio, N. Pizzorni, S. Barozzi, F. Mozzanica, and A. Schindler. 2018. Reliability and validity of the Italian version of the protocol of Orofacial Myofunctional Evaluation with Scores (I-OMES). Folia Phoniatrica et Logopaedica 70, 1: 8–12. [Google Scholar] [CrossRef]
- Shortland, H. L., S. Hewat, A. Vertigan, and G. Webb. 2020. Orofacial myofunctional therapy and myofunctional devices used in speech pathology treatment: A systematic quantitative review of the literature. American Journal of Speech-Language Pathology 30: 301–317. [Google Scholar] [CrossRef]
- Trench, J. A., and R. P. de Araújo. 2015. Dentofacial deformities: Orofacial myofunctional character-istics. Review CEFAC 17, 4: 1202–1214. [Google Scholar]
- Tricco, A. C., E. Lillie, W. Zarin, K.K. O’Brien, H. Colquhoun, D. Levac, D. Moher, M. D. Peters, T. Horsley, L. Weeks, S. Hempel, E. A. Akl, C. Chang, J. McGowan, L. Stewart, L. Hartling, A. Aldcroft, M. G. Wilson, C. Garritty, S. Lewin, C. M. Godfrey, M. T. Macdonald, E. V. Langlois, K. Soares-Weiser, J. Moriarty, T. Clifford, Ö. Tunçalp, and S.E. Straus. 2018. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine 169, 7: 467–473. [Google Scholar] [CrossRef] [PubMed]
- Van Lierde, K., H. Browaeys, P. Corthals, P. Mussche, E. Van Kerkhoven, and H. De Bruyn. 2012. Comparison of speech intelligibility, articulation and oromyofunctional behaviour in subjects with single-tooth implants, fixed implant prosthetics or conventional removable prostheses. Journal of Oral Rehabilitation 39: 285–293. [Google Scholar] [CrossRef]
- Vaz, A. C., and P. M. Bai. 2015. Lingual frenulum and malocclusion: An overlooked tissue or a minor issue. Indian Journal of Dental Research 26, 5: 488. [Google Scholar] [CrossRef]
- Yoon, A., C. Guilleminault, S. Zaghi, and S. Y. Liu. 2020. Distraction Osteogenesis Maxillary Expansion (DOME) for adult obstructive sleep apnea patients with narrow maxilla and nasal floor. Sleep Medicine 65: 172–176. [Google Scholar] [CrossRef]
- Zaghi, S., S. Shamtoob, C. Peterson, L. Christianson, S. Valcu-Pinkerton, Z. Peeran, B. Fung, D. Kwok-Keung Ng, T. Jagomagi, N. Archambault, B. O’Connor, K. Winslow, M. Lano, J. Murdock, L. Morrissey, and A. Yoon. 2021. Assessment of posterior tongue mobility using lingual-palatal suction: Progress towards a functional definition of ankyloglossia. Journal of Oral Rehabilitation 48, 6: 692–700. [Google Scholar] [CrossRef]
- Zere, E., P. K. Chaudhari, J. Sharan, K. Dhingra, and N. Tiwari. 2018. Developing Class III malocclusions: Challenges and solutions. Clinical, Cosmetic and Investigational Dentistry 10: 99–116. [Google Scholar] [CrossRef] [PubMed]
- Zou, J., M. Meng, C. S. Law, Y. Rao, and X. Zhou. 2018. Common dental diseases in children and malocclusion. International Journal of Oral Science 10, 1: 1–7. [Google Scholar] [CrossRef]
| Nordic Orofacial Test -Screening (Bakke et al., 2007) |
| Protocol used by professionals: dentist, speech therapist, physician, physiotherapist |
| Interview sections: sensory function, breathing, habits, chewing and swallowing, drooling, and dryness of the mouth |
| Six sections for examination: face at rest, nose breathing, facial expression, masticatory muscle and jaw function, oral motor function, and speech |
| Scoring: yes = 1; no = 0; not assessed = --; total range of scores: 0–12 |
| The MBGR [Marchesan, Berrentin-Felix, Genaro, and Rehder protocol] (Marchesan et al., 2012) |
| Protocol used by professionals: speech-language pathologist/speech therapist |
| Case history section: general health problems; breathing; sleep; previous treatments; feeding; chewing; swallowing; oral and postural habits; communication; education; speech; hearing; and voice. |
| Clinical examination section: body posture; the face, mandibular and occlusion measurements; extra-oral and intra-oral examinations; mobility of lips, tongue, velum, and jaw; pain; tone of lips, mentum, tongue and cheeks; orofacial functions including breathing, chewing, swallowing, speech, and voice |
| Scoring: Higher score = deficient results; 0 = best or normal performance |
| A One-Page Oromyofunctional Assessment Form (Paskay, 2012) |
| Protocol used by professionals: speech-language pathologist/speech therapist; orofacial myologists with a speech-language pathology background; dental professionals, cranio-osteopathic physicians, occupational therapists, and others |
| Clinical examination section: body posture, sitting, walking, breathing, sleep disorders, orofacial symmetry, temporomandibular joint functions, dental status, malocclusion, palatal structures, tongue tie, swallowing, speech, voice, and hearing functions. |
| Scoring: Notes are collected at the time of evaluation; no available scoring criteria |
| Professionals | Major Areas of Assessment |
| Dentist/Orthodontist | Skeletal (maxilla and mandible) and dental anomalies |
| Otorhinolaryngologist | Oral/nasal airway; allergies; tonsils |
| Primary care physician | General health conditions secondary to OMDs related to malocclusion |
| Sleep specialist | Sleep patterns; sleep apnea/dyspnea |
| Speech-language pathologist | Articulation of speech sounds; chewing; swallowing; tongue functioning; hard and soft palatal tissues; lips |
| Certified orofacial myologist | Tongue thrust; atypical swallows; oral habits; lingual frenulum |
| Dental hygienist | Tongue thrust; atypical swallows; oral habits; lingual frenulum |
| Neurologist | Cranial nerve disorders; jaw/facial pain |
| Physical therapist | Body posture and alignment |
© 2021 by the authors. 2021 Samantha C. Washington, Jayanti Ray.
Share and Cite
Washington, S.C.; Ray, J. Orofacial Myofunctional Assessments in Adults with Malocclusion: A Scoping Review. Int. J. Orofac. Myol. Myofunct. Ther. 2021, 47, 22-31. https://doi.org/10.52010/ijom.2021.47.1.4
Washington SC, Ray J. Orofacial Myofunctional Assessments in Adults with Malocclusion: A Scoping Review. International Journal of Orofacial Myology and Myofunctional Therapy. 2021; 47(1):22-31. https://doi.org/10.52010/ijom.2021.47.1.4
Chicago/Turabian StyleWashington, Samantha C., and Jayanti Ray. 2021. "Orofacial Myofunctional Assessments in Adults with Malocclusion: A Scoping Review" International Journal of Orofacial Myology and Myofunctional Therapy 47, no. 1: 22-31. https://doi.org/10.52010/ijom.2021.47.1.4
APA StyleWashington, S. C., & Ray, J. (2021). Orofacial Myofunctional Assessments in Adults with Malocclusion: A Scoping Review. International Journal of Orofacial Myology and Myofunctional Therapy, 47(1), 22-31. https://doi.org/10.52010/ijom.2021.47.1.4





