INTRODUCTION
Tongue strength and endurance are commonly assessed to identify orofacial neuromuscular impairments that may impact function (
Keskool et al., 2018;
Paris-Alemany et al., 2021;
Park et al., 2015;
Pitts et al., 2018;
Villa et al., 2017). The Iowa Oral Performance Instrument (IOPI) is a common device used to measure tongue strength and endurance (
Adams et al., 2013;
IOPI, 2020a;
Solomon et al., 2008;
VanRavenhorst-Bell et al., 2017,
2018), and offers the ability to assess the anterior and posterior regions of the oral tongue separately (
Adams et al., 2013;
IOPI, 2020a;
VanRavenhorst-Bell et al., 2017,
2018).
Some reports contend that the IOPI bulb can become slippery, causing tongue-to-bulb contact to slide or slip during assessment procedures (
Adams et al., 2013;
Hewitt et al., 2008;
Liu et al., 2021;
Neel et al., 2008;
Solomon & Clark, 2020;
Solomon et al., 2000,
2008;
Yoshikawa et al., 2011). Due to the smooth texture of the bulb as well as saliva production by the participant, slippage of the tongue on the bulb’s surface is a concern. Slippage may occur during both tongue strength and endurance measures; previous research has shown notably greater test-retest variability in endurance measures (
Adams et al., 2014;
Hewitt et al., 2008). Although such variability may be due to numerous underlying factors, slippage of the tongue-to-bulb connection may be a consideration due to the extended duration of time the client is asked to hold the bulb in a set tongue position. Regardless, slippage may cast doubt on the reliability of the lingual measures obtained. In addition, consequential misdiagnosis is a risk as well as general distrust in the IOPI system from both clinicians and clients.
Recognizing such concerns, IOPI Medical has taken steps to address such complaints by providing quality informational instructions (e.g., white paper instruction, web-based information, video) on proper bulb placement and practice (
IOPI, 2020a); however, a persistent opinion of bulb movement remains.
Solomon and Clark (
2020) recently investigated a potential solution by wrapping a single layer of gauze around the IOPI bulb to minimize slippage. Whether the gauze helped the bulb remain in place is unknown because pre-post placement measures were not recorded, however, participants reported improved IOPI bulb stabilization. Seeking a different solution,
Liu and colleagues (
2021) developed a new lingual pressure device with a disposable bulb that is custom fit to the oral cavity of each patient. The bulb shape was also altered in comparison to the IOPI bulb; it offers an exaggerated bump at the anterior end to increase stability of the bulb within the oral cavity while offering bite grooves on the extender tube to further assist with maintaining bulb placement. Recent testing against the Japan Medical Supply (JMS) tongue pressure measurement device confirmed its reliability and precision in performing tongue strength training (
r = .72 – .91); however, it is not readily available in market and has yet to be tested against the IOPI system.
The purpose of this study was to evaluate an individual’s overall perception of IOPI bulb stabilization and comfort across three IOPI bulb conditions while performing tongue strength and endurance assessments. Furthermore, the study sought to identify whether tongue muscle performance measures (strength, endurance) differed across the three IOPI bulb conditions.
METHODS
Participants
Forty healthy adults (11 male, 29 female), ages 18 – 49 years (M = 22.13, SD = 5.31) volunteered for this study. An a priori analysis was conducted using G*Power software (Heinrich Heine Universität Dusseldorf) to identify appropriate sample size. To achieve a power of .80 with an error of probability set at an α = .05 and a medium effect size, a sample size of 28 participants was suggested. Volunteers were recruited through a promotional flyer distributed around the university campus, the surrounding community and by word of mouth. The study was approved by the Wichita State University Institutional Review Board and informed consent was obtained from all volunteers prior to participation. An oral health history questionnaire was administered to screen each participant for presences of an oral fixture (e.g., dentures, bridge, permanent retainer), history of lingual or oral surgery, and/or a known neurological condition of the oral cavity. Reporting “yes” on any one of the screening questions resulted in exclusion to participate because it indicated a known presence of a condition that may negatively affect tongue function.
All 40 volunteers qualified and participated in the study. Participants were randomly assigned to one of two groups: anterior tongue region (n = 22; age M = 20.86 yr, SD = .83) and posterior tongue region (n = 18; age M = 23.66 yr, SD = 7.70).
Instrumentation and Materials
The IOPI 2.3 system (IOPI Medical, Carnation, WA), a standardized orofacial-bulbar device, was used to assess tongue strength and tongue endurance. The IOPI is a hand-held device with a silicone connecting tube ending with an air-filled silicone bulb. The device measures pressure difference against a known volume of air when lingual force is exerted on the bulb and digitally displays the intra-bulb pressure in kilopascals (kPa). A scaled line of LED lights provides visual feedback during tongue endurance measures. The scaled LED light system emits red (lower than 20% of the targeted lingual pressure) and scales up to amber (warning zone) when underperforming and then displays green at the top when the desired pressure is reached and maintained. A manually controlled timer within the device measures the duration of acceptable pressure held in seconds. The IOPI was calibrated monthly, as recommended by the manufacturer. Participants were instructed by a trained research administrator on how to engage the tongue during the lingual assessment to maintain relaxed lips and prevent the front teeth from clenching down on the IOPI silicon connector tube.
The IOPI bulb was presented under three conditions as shown in
Figure 1. Condition 1 presented the standard bulb with no modifications. In Condition 2 (Patch1), an oral-safe non-latex, flexible fabric patch, and in Condition 3 (Patch2), an oral-safe non-latex, hypoallergenic, micropore fabric patch were customized to fit (2.7 cm long, 1.8 cm wide, thickness < 0.10 cm) and adhere to one flat-surfaced side of the IOPI bulb with a biosafe adhesive.
Procedures
A trained research administrator provided instruction and administered the assessments in the Wichita State University Human Performance Laboratory in Wichita, Kansas. A random identification number was assigned to each participant’s data to protect confidentiality. The administrator measured and recorded participants’ height and weight. Participants self-reported sex (at birth) and age.
Comfort Level and Preference Survey
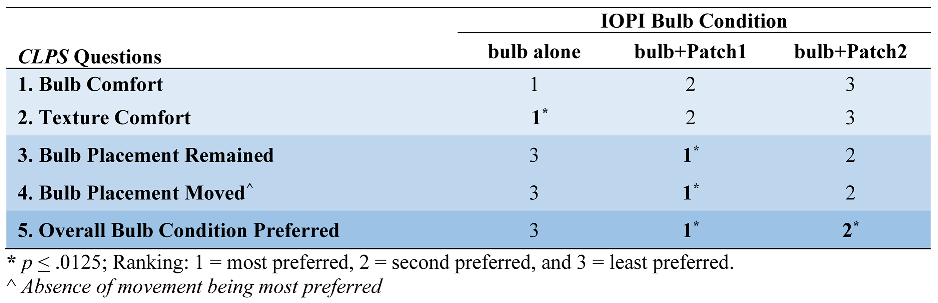
After completion of all tongue muscle performance measures for each bulb condition, a custom-designed Comfort Level and Preference Survey (
CLPS) was administered to each participant. The
CLPS is a Likert-scaled survey comprising a total of five questions, as shown in
Table 1. Questions 1 and 2 of the
CLPS focused on comfort by asking the participant which bulb condition and which texture between each condition were most comfortable. The 4-point Likert scale for these questions ranged from
comfortable to
uncomfortable. Questions 3 and 4 addressed movement of the bulb using a 3-point Likert scale ranging from
always to
never. Questions 3 and 4 intentionally sought to ask the same question in a transposed manner. Question 5 culminated a participant’s perception and overall preference among the three bulb conditions in a ranking order, from
most to
least preferred. In addition to the
CLPS, an administrator recorded a tick mark beside the corresponding bulb condition each time a participant verbally indicated tongue-to-bulb slippage during the assessment.
Internal consistency of the CLPS survey. A Cronbach’s Alpha analysis was conducted to determine internal consistency of the questions administered on the
CLPS. Questions 1, 2, 3, and 4, as grouped and shown in
Table 1, were analyzed by category at a 95% confidence level. Overall Preference (Question 5) was not analyzed because two or more items grouped is required for analysis. The Comfort category (Questions 1 and 2) indicated a moderate level of internal consistency, α = .68. The Movement Perception category of the survey (Questions 3 and 4) was shown to have a very high internal consistency, α = .93. These findings support the overall inclusion of the
CLPS survey.
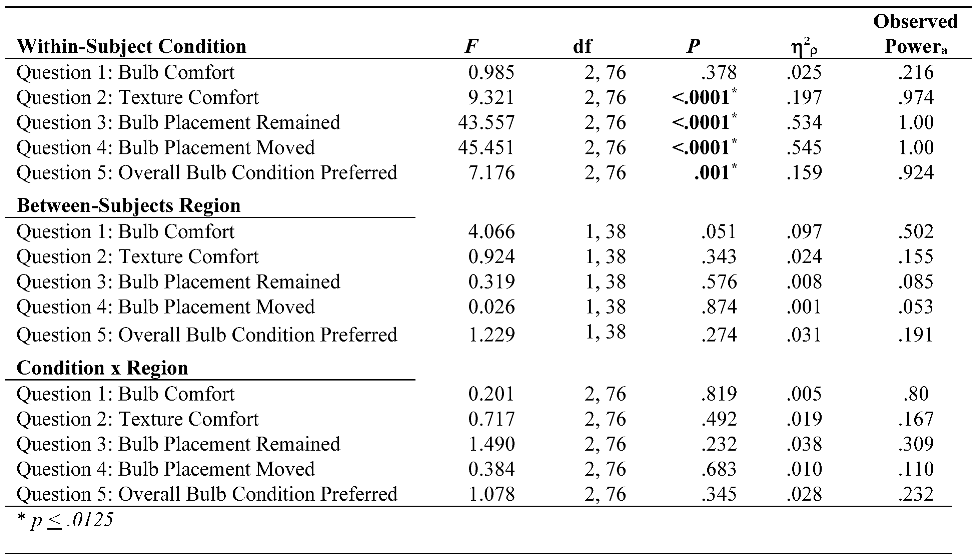
Statistical Analysis
To objectively test the first research question, a 3 x 2 [IOPI bulb condition (bulb alone, bulb+Patch1, bulb+Patch2) x tongue region (anterior, posterior)] mixed-design repeated-measures ANOVA was administered for the five items of the CLPS. Between-subjects differences were included to examine whether the group of participants who performed anterior-tongue tasks differed from those in the posterior-tongue group. Pairwise comparisons (t-tests) were completed if a significant bulb condition x tongue region interaction was found.
To test the second research question, four separate one-way within-subjects ANOVAs were conducted across bulb conditions for each measure: anterior tongue strength, anterior tongue endurance, posterior tongue strength, and posterior tongue endurance. Paired sample t-tests were completed if a significant tongue measure x bulb condition interaction was found.
All analyses were administered using IBM SPSS Statistics software version 27. Analyses followed a family-wise error adjustment of
p ≤ .05/4 for an adjusted critical alpha level set at
p ≤ .0125 for all statistical analysis. Partial eta squared (η
2ρ) values were referenced based on small = .01, medium = .06, and large = .14 effect sizes (
Green & Salkind, 2017).
DISCUSSION
Overall, the findings of this study showed that by adding an anti-slip patch to an IOPI bulb’s surface, one’s perception of bulb stability improved in comparison to the IOPI bulb alone. Although placement and movement measures of the tongue in relation to the bulb were not investigated, participants rated their perceptions of IOPI bulb stability and movement while performing lingual assessment measures. As shown in
Table 3, one’s perceptions of a stable and well-controlled bulb appeared to outweigh the role of comfort and texture. Specifically, participants preferred the non-latex, flexible fabric anti-slip patch (Patch1) and its perceived stability over the notable comfort of the IOPI bulb alone.
Solomon and Clark (
2020) reported similar findings stating that the IOPI bulb was perceived to be more stable on the tongue when applying a thin layer of gauze over the IOPI bulb during lingual assessments. These findings suggest that applying a textured material to the IOPI bulb may serve as a viable solution for bulb slippage. Relatedly, participants in the current study reported slippage of the bulb 38 times when the bulb was used in its original manufactured state compared to 15 times with Patch2 and only one time with Patch1. Proper lingual placement of the IOPI bulb across all conditions followed instructional guidelines provided by IOPI Medical (
IOPI, 2020b); however, the perception of bulb slippage was prevalent in the absence of an anti-slip patch.
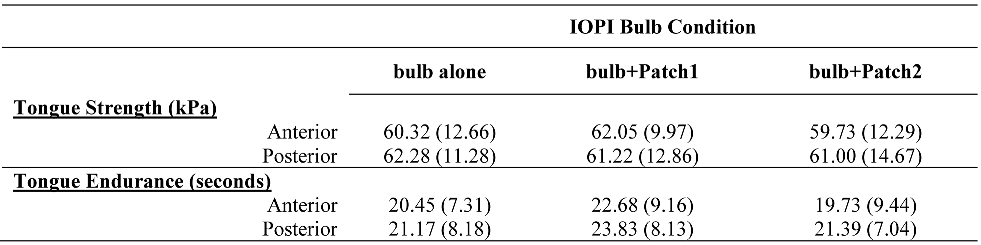
In addition to investigating an individual’s perception of bulb slippage with and without an anti-slip patch, the current study found that tongue strength and tongue endurance measures (anterior, posterior) did not differ significantly regardless of bulb condition (
Table 4). To date, the only other known study to report tongue muscle performance, specifically tongue strength, in respect to applying a textured material to the IOPI bulb was by
Solomon and Clark (
2020). They reported no significant difference in anterior tongue strength measures (
p= .2096) before and after applying a layer of gauze to the IOPI bulb which is in agreement with current findings; the difference for posterior tongue strength measures was just shy of the conservative level of significance (α = .01) set for their study (
p = .0115). Tongue strength measures in the lateral and protrusive directions were significantly improved with the use of gauze, but these are not conventional assessment procedures with the IOPI. The current study is the first known study to investigate tongue-endurance performance with and without a modified IOPI bulb.
Liu et al. (
2021) used an entirely different device and bulb to investigate maximal tongue pressure and fatigue testing of the bulb itself which may not be a suitable comparison.
The findings of this study invite consideration of a study by
Sura and colleagues (
2012) that reported more effective improvements in lingual performance with the implementation of preferred lingual exercise(s) compared to minimally exertive compensatory strategies. The presence of tongue-to-bulb slippage during an assessment or treatment may negatively alter one’s psychological investment. An anti-slip patch added to the IOPI bulb may benefit the patient’s and clinician’s overall psychological investment in the therapy exercise and confidence in the effectiveness of the assessment tool.
In general, the findings of the current study suggest that the addition of a textured material to minimize tongue-to-bulb slippage does not alter overall lingual performance and offers the perception of stability when administering standard tongue strength and endurance assessments. These findings also offer support for current tongue strength and endurance normative values generalized for healthy adults when assessed using the IOPI system (
Adams et al., 2013;
Hewitt et al., 2008;
IOPI, 2020b;
Keskool et al., 2018;
Solomon et al., 2000). As shown in
Table 4, the self-reported healthy adults in the current study delivered anterior and posterior tongue strength and endurance measures that fell within healthy normative values across all three IOPI bulb conditions.
Limitations and Future Directions
This study introduced and investigated anti-slip patches and their perceived ability to maintain IOPI bulb placement on the lingual surface, as well as how tongue strength and endurance measures may be affected. Due to a relatively small sample size, findings should be interpreted with caution and continued validation is needed. Additionally, direct comparison of tongue muscle performance measures (strength, endurance) by tongue region (anterior, posterior) across all IOPI bulb conditions was not possible because participants only performed tongue strength and endurance measures in one tongue region, either anterior or posterior, in an effort to mitigate lingual fatigue. Based on the current findings, Patch2 can be removed from future studies. Fewer bulb conditions would reduce the total number of trials which may be more favorable for performing both anterior and posterior tongue strength and endurance measures for a direct comparison by tongue region.
In addition, caution should be considered when generalizing the findings of this study across populations. Future research should investigate the use of the IOPI bulb with the flexible fabric anti-slip patch in individuals with orofacial impairments and from different age groups. Finally, the CLPS was custom developed for this study and appeared to have acceptable internal consistency for assessing bulb comfort and movement (α = .68, .93), respectively; however, future studies should examine it for additional indicators of validity and reliability.
Conclusion
The findings of this study revealed that healthy adults prefer the IOPI bulb with a flexible fabric anti-slip patch during lingual assessments due to perceived tongue-to-bulb stability compared to the noted comfort of the IOPI bulb alone. Additionally, tongue strength and endurance measures did not differ across IOPI bulb conditions. These preliminary findings are promising and support further testing and validation of the flexible fabric anti-slip patch for use with the IOPI bulb.