An Introduction to Clinical Simulation (CS) for Orofacial Myologists: COVID-19’s Impact on Clinical Education
Abstract
:INTRODUCTION
TYPES OF CS-BASED LEARNING AND OMD-RELATED EXPERIENCES
ADVANTAGES AND DISADVANTAGES OF CS
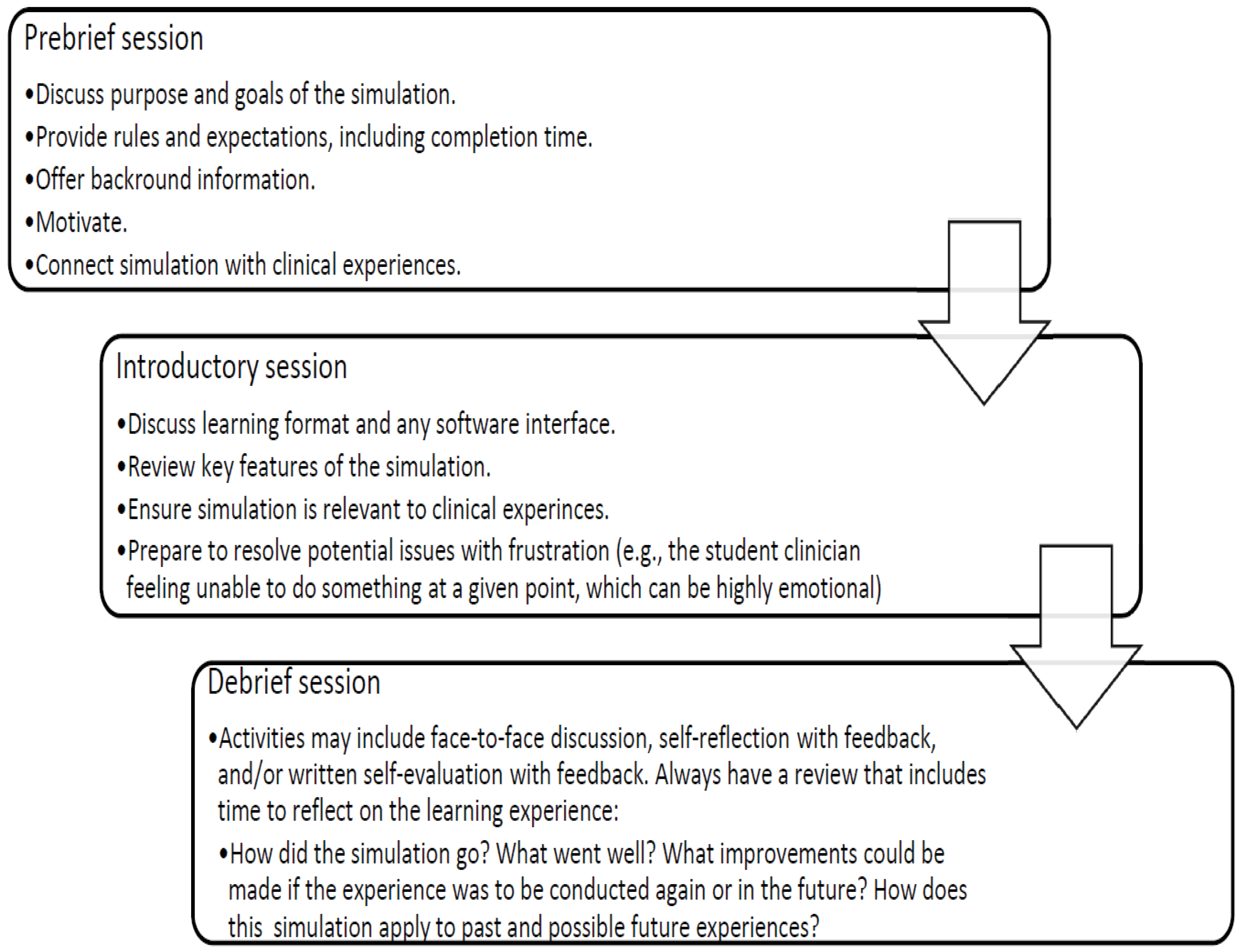
EVIDENCE AND BEST PRACTICES RELATED TO CS
CONCLUSION
References
- Alanazi, A. A., N. Nicholson, S. R. Atcherson, C. Franklin, M. Anders, N. K. Nagaraj, and P. Highley. 2016. Use of baby isao simulator and standardized parents in hearing screening and parent counseling education. American Journal of Audiology 25: 211–223. [Google Scholar] [CrossRef] [PubMed]
- Alanazi, A. A., N. Nicholson, S. R. Atcherson, C. Franklin, N. K. Nagaraj, M. Anders, and L. Smith-Olinde. 2017. Audiology students’ perception of hybrid simulation experiences: Qualitative evaluation of debriefing sessions. Journal of Early Hearing Detection and Intervention 2, 1: 12–28. [Google Scholar]
- Aldrich, C. 2009. Learning online with games, simulations, and virtual worlds. San Francisco, CA. [Google Scholar]
- American Speech-Language-Hearing Association (ASHA). 2020. Certification standards for speech-language pathology frequently asked questions: Clinical simulation. Available online: https://www.asha.org/Certification/Certification-Standards-for-SLP-Clinical-Simulation/#CS.
- Barabari, P., and K. Moharamzadeh. 2020. Novel Coronavirus (COVID-19) and dentistry: A comprehensive review of the literature. Dentistry Journal 53. [Google Scholar] [CrossRef]
- Benadom, E. M., and N. L. Potter. 2011. The use of simulation in training graduate students to perform transnasal endoscopy. Dysphagia 26: 352–360. [Google Scholar] [CrossRef]
- Boese, T., J. Borum, M. Cato, L. Gonzalez, A. Jones, K. Kennedy, and C. Resse. 2013. Standards of best practice: Simulation. Standard V: Facilitator. Clinical Simulation in Nursing 9, 6: 22–25. [Google Scholar]
- Commission on Dental Accreditation (CODA). 2020. Actions regarding ongoing operations and the impact on educational programs as a result of COVID-19. American Dental Association: Available online: https://www.ada.org/en /coda/accreditation/accreditation-news/covid-19-updates.
- Cook, D. A., R. Hatala, R. Brydges, J. H. Szostek, A. T. Wang, P. J. Erwin, and S. J. Hamstra. 2011. Technology enhanced simulation for health progressions education: A systematic review and meta-analysis. Journal of the American Medical Association 306, 9: 978–988. [Google Scholar] [CrossRef]
- Council for Clinical Certification (CFCC). 2020. 2020 standards and implementation procedures for the certificate of clinical competence in speech-language pathology; American Speech-Language-Hearing Association (ASHA). Available online: https://www.asha.org/certification/2020-slp-certification-standards/.
- Council of Academic Programs in Communication Sciences and Disorders (CAPCSD), and Academic and Clinical Education Task Force. 2019. Best practices in healthcare simulations: Communication sciences and disorders. Available online: https://growthzonesitesprod.azureedge.net/wp-content/uploads/sites/1023/2020/03/Best-Practices-in-CSD.pdf.
- Decker, S., M. Fey, S. Sideras, S. Caballero, L. Rockstraw, T. Boese, and J. Borum. 2013. Standards of best practice: Simulation. Standard VI: The debriefing process. Clinical Simulation in Nursing 9, 6: 26–29. [Google Scholar]
- Ellis, C. M. 2017. Using simulation and critical thinking in speech-language pathology: A university case study. Journal of Human Services: Training, Research, and Practice 2, 2. Available online: https://scholarworks.sfasu.edu/cgi/viewcontent.cgi?article=1044&context=jhstrp.
- Estis, J. M., A. B. Rudd, B. Pruitt, and T. Wright. 2015. Interprofessional simulation-based education enhances student knowledge of health professional roles and care of patients with tracheostomies and Passy-Muir® Valves. Journal of Nursing Education and Practice 5, 6: 123. [Google Scholar] [CrossRef]
- Fanning, R. M., and D. M. Gaba. 2007. The role of debriefing in simulation-based learning. Society for Simulation in Healthcare 2, 4: 115–125. [Google Scholar] [CrossRef]
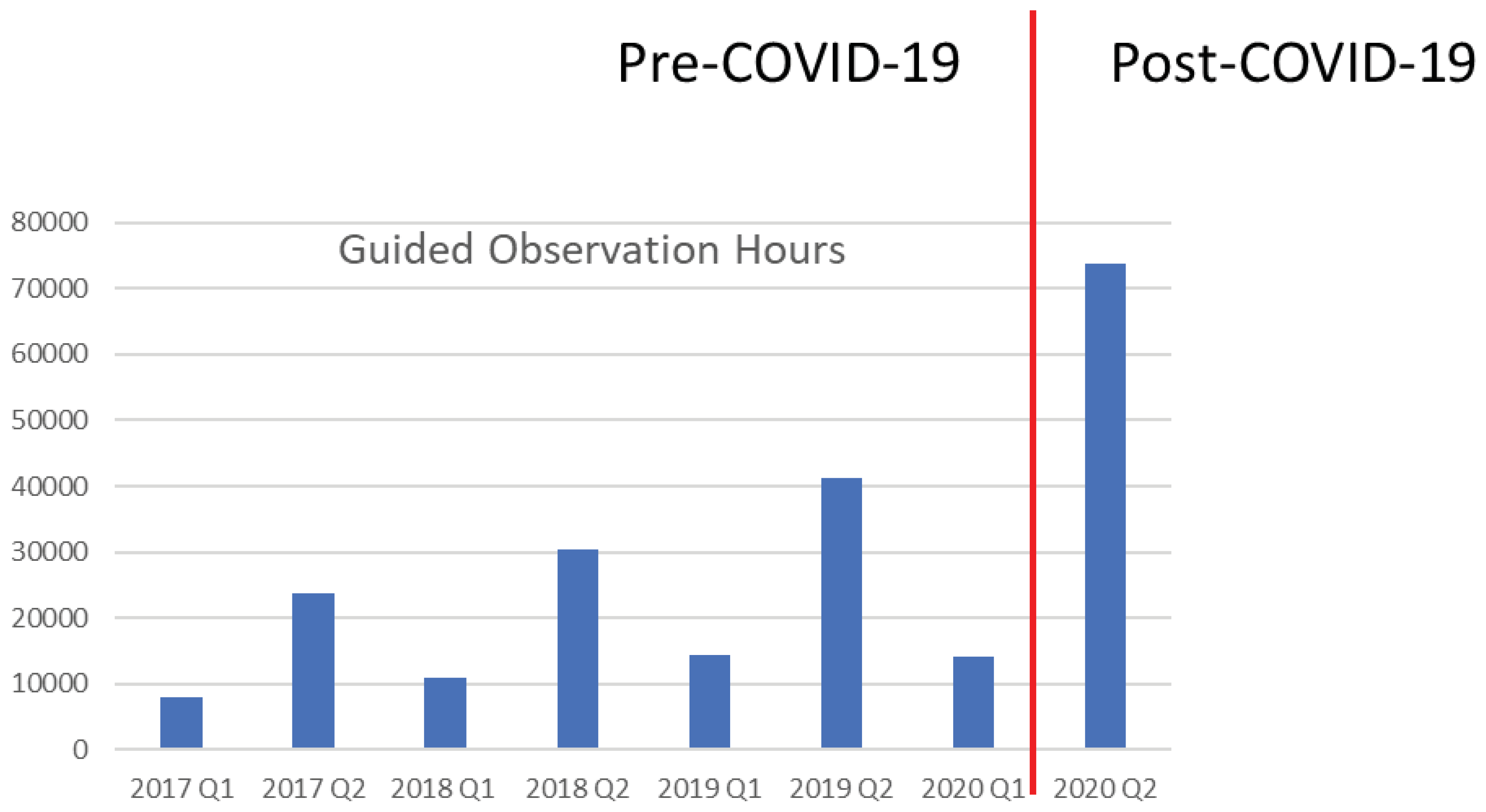
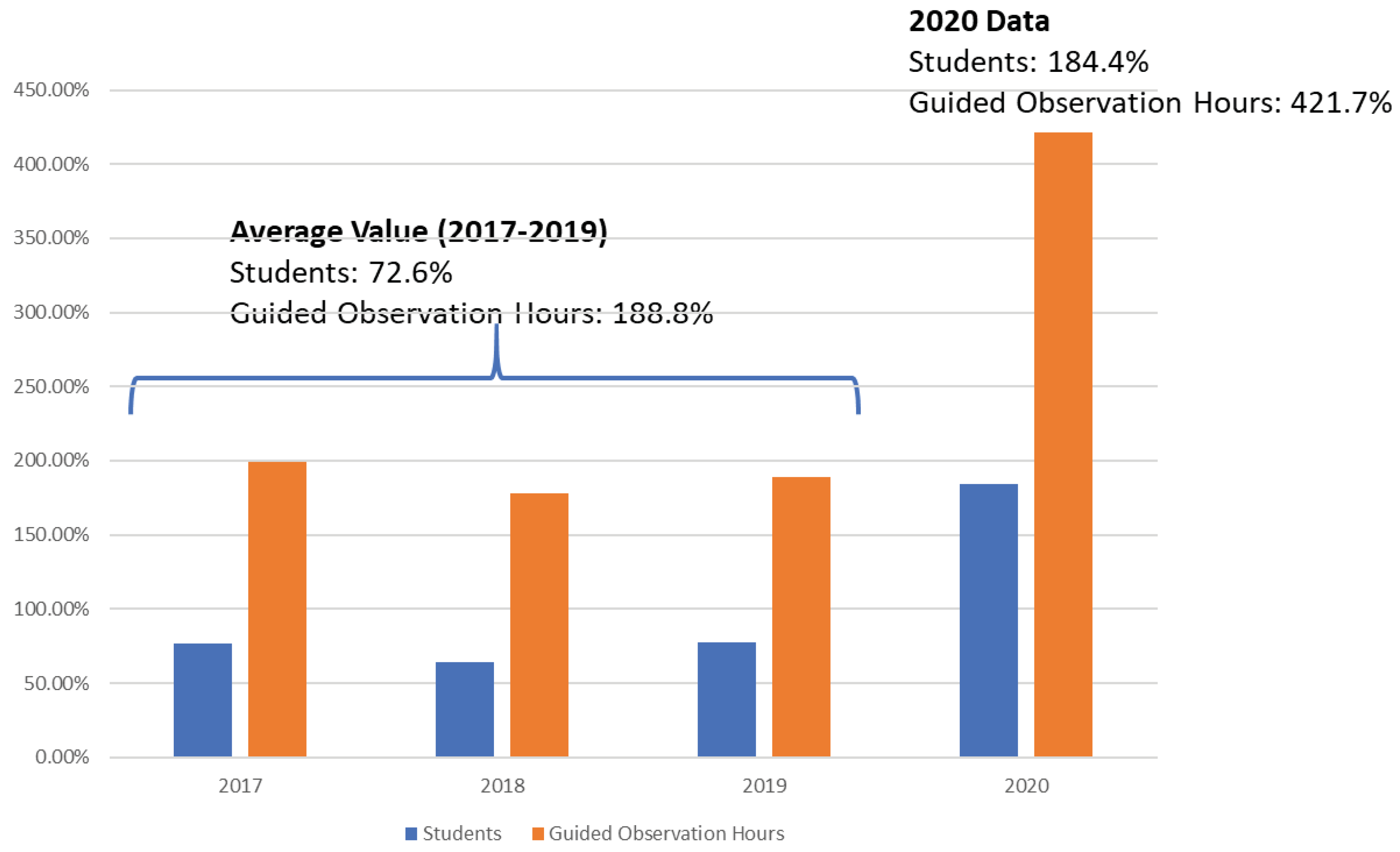
- Fischer, M. A. 2020. [Master Clinician Network pre-COVID-19 and post-COVID-19 website traffic], Unpublished raw data.
- Hayden, J. K., R. A. Smiley, M. Alexander, S. Kardong-Edgren, and P. R. Jeffries. 2014. The NCSBSN national simulation study: A longitudinal, randomized, controlled study replacing clinical hours with simulation in prelicensure nursing education. Journal of Nursing Regulation 5, 2: S4–S41. [Google Scholar] [CrossRef]
- Hill, A. E., B. J. Davidson, S. McAllister, J. Wright, and D. G. Theodoros. 2014. Assessment of student competency in a simulated speech-Language pathology clinical placement. International Journal of Speech-Language Pathology 16, 5: 464–475. [Google Scholar] [CrossRef]
- Hill, A. E., B. J. Davidson, and D. G. Theodoros. 2013. The performance of standardized patients in portraying clinical scenarios in speech-language therapy. International Journal of Language and Communication Disorders 48, 6: 613–624. [Google Scholar] [CrossRef] [PubMed]
- Howells, S., E. A. Cardell, M. C. Waite, A. Bialocerkowski, and N. Tuttle. 2019. A simulation-based learning experience in augmentative and alternative communication using telepractice: Speech pathology students’ confidence and perceptions. Advances in Simulation 4, 23. [Google Scholar] [CrossRef]
- Issenberg, S. B., W. C. McGaghie, E. R. Petrusa, D. L. Gordon, and R. J. Scalese. 2005. Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Medical Teacher 27: 10–28. [Google Scholar] [CrossRef] [PubMed]
- Jansen, L. 2014. The evaluation of computer-based simulated case studies in speech-language pathology education. Doctoral dissertation, Nova Southeastern University, Fort Lauderdale, FL. [Google Scholar]
- Johnson, C. 2020. [Simucase Website Traffic Comparison Spring 2019 and spring 2020]. Unpublished raw data. [Google Scholar]
- Lieberth, A. K., and D. R. Martin. 2005. The instructional effectiveness of a web-based audiometry simulator. Journal of the American Academy of Audiology 16, 2: 79–84. [Google Scholar] [CrossRef]
- LSU Health Shreveport. 2020. Clinical skills center: Task training simulation. Available online: https://www.lsuhs.edu/our-schools/clinical-skills-center/task-trainer-simulation.
- Naeve-Velguth, S., S. A. Christensen, and S. Woods. 2013. Simulated patients in audiology education: Student reports. Journal of the American Academy of Audiology 24, 8: 740–746. [Google Scholar] [CrossRef]
- Potter, N. L., and M. Allen. 2013. Clinical swallow exam for dysphagia: A speech pathology and nursing simulation experience. Clinical Simulation in Nursing 9, 10: e461–e464. [Google Scholar] [CrossRef]
- Rall, M., T. Manser, and S. Howard. 2000. Key elements of debriefing for simulator training. European Journal of Anesthesiology 17: 516–517. [Google Scholar] [CrossRef]
- Salvoldelli, G. L., V. N. Naik, J. Park, H. S. Joo, R. Chow, and S. J. Hamstra. 2006. Value of debriefing during simulated crisis management: Oral versus video-assisted oral feed-back. Anesthesiology 105, 2: 279–285. [Google Scholar] [CrossRef]
- Sheepway, L., M. Lincoln, and L. Togher. 2011. An international study of clinical education practices in speech-language pathology. International Journal of Speech Language Pathology 13, 2: 174–185. [Google Scholar] [CrossRef] [PubMed]
- Singh, H., M. Kalani, S. Acosta-Torres, T. Ahmadieh, J. Loya, and A. Ganju. 2013. History of simulation in medicine: From Resusci Annie to Ann Myers Medical Center. Neurosurgery 73: 9–14. [Google Scholar] [CrossRef] [PubMed]
- Syder, D. 1996. The use of simulated clients to develop the clinical skills of speech and language therapy students. European Journal of Disorders of Communication 31: 181–192. [Google Scholar] [CrossRef] [PubMed]
- Vaughn, M. J. 2001. A pilot study investigating the use of simulation technology to increase clinical knowledge and self confidence levels of graduate students studying speech language pathology. University of Cincinnati (unpublished Master’s thesis). Available online: http://rave.ohiolink.edu/etdc/view?acc_num=ucin992265762.
- Ward, E. C., A. E. Hill, R. L. Nund, A. F. Rumbach, K. Walker-Smith, S. E. Wright, and P. Dodrill. 2015. Developing clinical skills in paediatric dysphagia management using human patient simulation (HPS). International Journal of Speech-Language Pathology 17, 3: 230–240. [Google Scholar] [CrossRef]
- Watson, K., A. Wright, N. Morris, J. McMeeken, D. Rivett, F. Blackstock, and G. Jull. 2012. Can simulation replace part of clinical time? two parallel randomised controlled trials. Medical Education 46, 7: 657–667. [Google Scholar] [CrossRef]
- Williams, S., C. Dudding, and K. Ondo. 2013. Presentation to the American Speech-Language-Hearing Association. Chicago, IL. November. [Google Scholar]
- Zimmerman, E. 2016. Simulation 2: Oral conditions and speech. Boston, MA: Northeastern University. [Google Scholar]
- Zraick, R. 2002. The use of standardized patients in speech-language pathology. Perspectives on Issues in Higher Education 5: 14–16. [Google Scholar] [CrossRef]
- Zraick, R., R. Allen, and S. Johnson. 2003. The use of standardized patients to teach and test interpersonal and communication skills with students in speech-language pathology. Advances in Health Sciences Education 8: 237–248. Available online: http://www.ncbi.nlm.nih.gov/pubmed/14574048. [CrossRef]



© 2020 by the author. 2020 Hope C. Reed
Share and Cite
Reed, H.C. An Introduction to Clinical Simulation (CS) for Orofacial Myologists: COVID-19’s Impact on Clinical Education. Int. J. Orofac. Myol. Myofunct. Ther. 2020, 46, 48-58. https://doi.org/10.52010/ijom.2020.46.1.5
Reed HC. An Introduction to Clinical Simulation (CS) for Orofacial Myologists: COVID-19’s Impact on Clinical Education. International Journal of Orofacial Myology and Myofunctional Therapy. 2020; 46(1):48-58. https://doi.org/10.52010/ijom.2020.46.1.5
Chicago/Turabian StyleReed, Hope C. 2020. "An Introduction to Clinical Simulation (CS) for Orofacial Myologists: COVID-19’s Impact on Clinical Education" International Journal of Orofacial Myology and Myofunctional Therapy 46, no. 1: 48-58. https://doi.org/10.52010/ijom.2020.46.1.5
APA StyleReed, H. C. (2020). An Introduction to Clinical Simulation (CS) for Orofacial Myologists: COVID-19’s Impact on Clinical Education. International Journal of Orofacial Myology and Myofunctional Therapy, 46(1), 48-58. https://doi.org/10.52010/ijom.2020.46.1.5




