Abstract
The purpose of this article is to explain the importance of evaluating and documenting the freeway space (interdental rest position), in initial examinations and at the completion of therapy in patients exhibiting an open mandibular resting position. The freeway space measurements obtained can be shared with parents, patients, and referral sources. To this end, the muscular, neural, and sensory components related to the freeway space are discussed, as well as airway, dental eruption patterns, tactile feedback, and orthodontic relapse considerations. An extraoral method for evaluating the dimensions of the anterior freeway space is proposed.
INTRODUCTION
Orofacial myologists are concerned with teeth-apart postures and behaviors while by contrast, dentists and orthodontists are primarily concerned with teeth-together relationships. This distinguishes the postural and muscle training and retraining work of the orofacial myologist from the dental-occlusal and jaw manipulations of dental/orthodontic providers.
The goals of orofacial myofunctional therapy include the creation, restoration, and stabilization of oral postures and functions that aid in facilitating normal processes of orofacial and dental development (ASHA, 2019; Hanson & Mason, 2003). Orofacial myofunctional therapy typically focuses on the elimination of noxious habit patterns and inappropriate resting postures.
Most orofacial myofunctional disorders are accompanied by the lower jaw being postured in an open position beyond the normal range when a finger, tongue, or other object is positioned between the incisor teeth for extended periods. In the opinion of the authors, there currently is a general lack of recognition of the importance of assessing and correcting an excess dental freeway space, as reflected on websites and in discussion groups of orofacial myologists. Accordingly, in addition to removing noxious habit patterns, it is recommended that an important goal of therapy should be to create or recapture and stabilize a normal resting vertical dimension between the jaws and dental arches.
Although orthodontists and other dental providers often refer patients with tongue thrusting behaviors for orofacial myofunctional therapy, it is the authors’ opinion that many dental specialists lack experience in identifying variations in the vertical rest position of the jaws, or freeway space. Of interest, there is no discussion of the freeway space in two leading orthodontic textbooks (Graber et al., 2016; Proffit et al., 2018). This situation presents an opportunity for orofacial myologists to share information and clinical findings with dental and orthodontic referral sources regarding the freeway dimensions of selected patients.
PURPOSE
The purpose of this article is to explain the importance of evaluating the anterior freeway space in initial examinations and at the completion of orofacial myofunctional therapy in patients exhibiting an open mandibular resting position. To this end, the muscular, neural, and sensory components related to the freeway space will be reviewed. Discussion will include airway considerations, dental eruption scenarios, tactile feedback, and orthodontic relapse evaluation guidelines. An extraoral method will be proposed for evaluating the anterior freeway space.
NORMAL AND ABNORMAL DIMENSIONS OF THE FREEWAY SPACE
The normal rest position of the teeth and jaws is characterized by a small vertical space between the upper and lower teeth (Figure 1). This space is referred to variably in dentistry as the vertical occlusal distance (VOD), occlusal vertical distance (OVD), interocclusal distance, or, most commonly, the freeway space (Aradya & Chowdhary, 2017; Sicher & DuBrul, 1970).
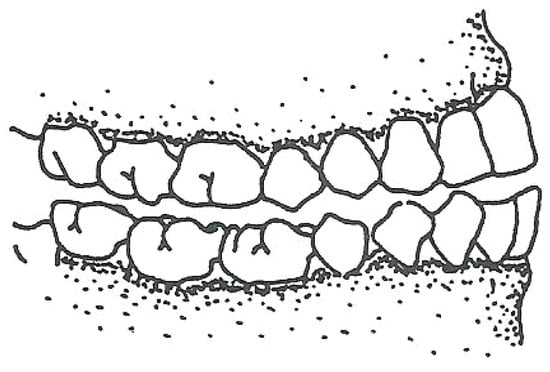
Figure 1.
The resting interocclusal dimension, or freeway space.
In the normal rest position of teeth and jaws, the teeth in opposing dental arches are not in contact but rest slightly apart. A normal resting interocclusal dimension has been determined as 2-3 mm of vertical opening at the first molar teeth, and 2-5 mm at the incisors (Aradya & Chowdhary, 2017; Sicher & DuBrul, 1970). The larger vertical range reported at the incisors is related to the rotation of mandibular condyles within the glenoid fossae that act as a hinge in the opening and closing motions of the mandible, with larger vertical excursions occurring anteriorly than posteriorly.
MUSCLES THAT CONTROL AND MONITOR THE FREEWAY SPACE
Figure 2 illustrates the mandible and its muscular attachments. The two primary muscles that monitor the freeway space by sensory and proprioceptive components are the masseter and temporalis muscles (Weisinger et al., 2019). Ruffini endings and Golgi tendon organs in the temporomandibular joint complex also provide proprioceptive feedback.
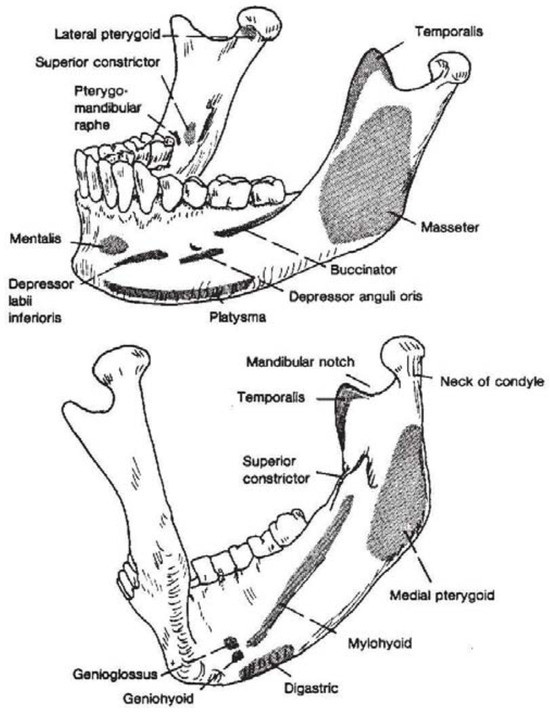
Figure 2.
The mandible, showing its muscular attachments. Note the masseter and medial pterygoid attachments on each side of the mandible at the angle and distal body of the mandible. (From Bateman, H.E., and Mason, R.M.: Applied Anatomy and Physiology of the Speech and Hearing Mechanism, 1984. Courtesy of Charles C. Thomas, Publisher, Springfield, Illinois.).
There has been some speculation that the medial pterygoid (internal pterygoid) muscles may play a small role in monitoring the dimensions of the freeway space. Due to their attachment on the inside of the ramus of the mandible, the medial pterygoids can function as a weak counterpart to the masseter muscles, and are sometimes referred to as internal masseter muscles. All three of these muscles are innervated by the mandibular branch of the trigeminal nerve. The masseter, the strongest of the three, is composed of muscle fibers arranged at an angle to the long axis of the muscle. This arrangement is found to produce shorter muscle fibers, giving great power to the masseter (Widmer et al., 2012; Yabushita et al., 2005).
NEUROMUSCULAR SPINDLES AND THE MASSETER MUSCLES
Muscle spindles are small, spindle-shaped (sensory) stretch receptors located parallel to the main extrafusal muscle fibers in skeletal muscle tissue. Muscle spindles consist of intrafusal muscle fibers that are enclosed in a spindle-shaped connective tissue sac. The spindles are innervated by gamma motor neurons.
Muscle spindles function as stretch receptors within the body of a muscle to primarily detect contains extrafusal, Type I (slow-twitch) fibers. Although muscle spindles and Type I fibers changes in the length of the muscle. They convey length information to the central nervous system via afferent nerve fibers. This information can be processed by the brain as proprioception (Rowland, 2009).
Muscle spindles are sensitive to the rate at which a muscle stretches (phasic stretch) and also to the extent to which the muscle is stretched (tonic stretch). Muscle spindles also participate in regulating muscle tone. The large distribution of neuromuscular spindles in the masseter muscle complex contains extrafusal, Type I (slow-twitch) fibers. Although muscle spindles and Type I fibers appear to be sparse in the superficial part of the masseter, they are abundant in the deep muscle layer (Clark & Solomon, 2012; Rowlerson et al., 1988).
In an often-referenced study by Lennartsson (1980), the distribution of muscle spindles was studied in a rat model. The average number of spindles found was 110 in the masseter, 75 in the temporalis, and 25 in the medial pterygoid muscle. The spindles were predominant in the medial parts of these muscles. No muscle spindles were found in the lateral pterygoid or posterior digastric muscle, and only isolated spindles were found in the anterior digastric muscles. These data provide further confirmation of the important role of the masseter in participating in many tasks such as bite opening and closing, chewing, and in maintaining the normal interocclusal (freeway) dimension (Yin et al., 2007).
Neuromuscular spindles in the masseter serve other functions in addition to maintaining the static posture referred to as the freeway space. The spindles are thought to be important during load compensation tasks such as chewing, and for the development of powerful bite forces in aggressive or defensive situations (Scutter & Kemal, 2001).
MUSCLE TONUS
The rest position of teeth and jaws is independent of the number, shape, and position of teeth, and even the total absence of teeth. Instead, the rest position is determined by the resting tonus of the mandibular musculature and by gravity (Sicher & DuBrul, 1970). Since no muscle is ever totally relaxed, except in deep anesthesia or unconsciousness, the residual tension in a muscle at rest is its resting tonus that is maintained by the intermittent reflex contraction of a certain percentage of fibers in a given muscle (Rowland, 2009).
NEURAL CONNECTIONS
Sensory feedback via cranial nerve V
The trigeminal nerve (CN-V) is a mixed nerve, with both sensory and motor components (Figure 3). The three branches of the nerve (ophthalmic, maxillary, and mandibular) have a remarkable number of different modalities of sensation that are carried over a single nerve to different sites along the brainstem and then relayed to primary sensory and motor cortices within the central nervous system.
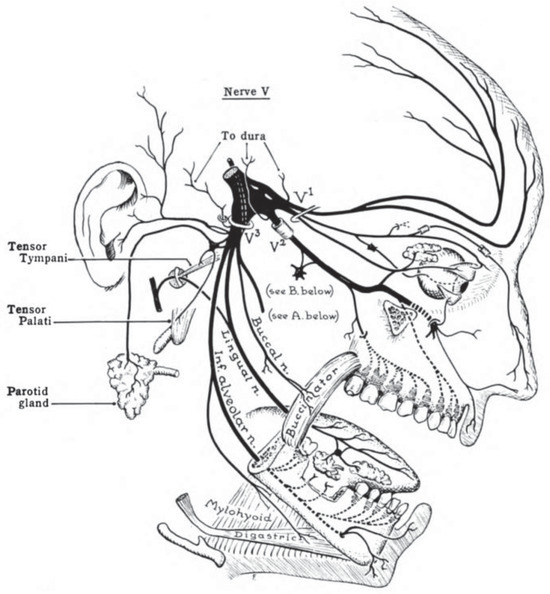
Figure 3.
Cranial nerve V, the trigeminal nerve, showing the trigeminal ganglion. (From: John Charles Boileu Grant, An atlas of anatomy, 1962. Williams and Wilkins, Publisher, Philadelphia, PA).
The uniqueness of the trigeminal ganglion merits discussion. A trigeminal ganglion of about two millimeters in size is located within a space on each side of the skull near the apex of the temporal bone, just anterior to each ear. The space for each ganglion is referred to as the trigeminal cave or Meckel’s cave. Each ganglion is wrapped in dura mater, allowing cerebrospinal fluid to surround and nourish the ganglion.
The three sensory branches of the trigeminal nerve converge at the trigeminal (semilunar or Gasserian) ganglion before the nerve enters the brainstem at the level of the pons where the root and fibers of the nerve then relay messages to the sensory and motor areas of the central nervous system. The three sensory divisions of the trigeminal nerve exit the skull through the superior orbital fissure, foramen rotundum, and foramen ovale (Jones & Vypotil, 2015).
Sensory receptors are generously embedded within the periodontium and in the gingiva, buccal mucosa, posterior hard palate, and also in the masseter and temporalis muscles themselves. The many sensory nerve endings from a variety of locations transmit information via the mandibular and maxillary branches of the trigeminal nerve to the trigeminal ganglion and onward to the brainstem where the need for adjustments in oral postures and functions can be determined and then carried out via motor tracts of the trigeminal nerve (Wiesinger et al., 2019).
Although the mandibular branch of the trigeminal nerve carries sensory information from the lips, anterior tongue, and rugae areas, the sensory receptors in these structures do not participate actively in signaling the brainstem of changes in the freeway space.
Motor division of the trigeminal nerve
Through the mandibular branch of the trigeminal nerve, eight muscles receive innervation. They include the four muscles of mastication (masseter, temporalis, and the two pterygoid muscles), plus the anterior belly of the digastric muscle, the mylohyoid, the tensor tympani, and the tensor veli palatini. All are supplied by axons from the motor nucleus of the trigeminal nerve.
The Trigeminal nerve feedback loop
Feedback from sensory receptors is transmitted along the mandibular branch of the trigeminal nerve to the brainstem and back to the masseter and temporalis muscles via the motor branch of the mandibular nerve. This process constitutes a complex sensory and motor loop that allows the masseter and temporalis muscles to monitor the rest position of the jaws and teeth and to maintain a normal freeway space.
Insights from denture construction regarding stress to the masseter muscles from disruption of the freeway space
Much has been learned about the muscles controlling the freeway space from prosthodontic experience in denture construction (Monteith, 1984; Rosenstiel et al. 2015; Shillingburg et al., 2012). The rest position in edentulous patients becomes very important during denture construction (Rosenstiel et al., 2015). When the denture base has been raised inappropriately to the rest position; that is, with teeth contacting at this position, the result is that the mandibular musculature, especially the masseter, becomes severely stressed. The constant contact of teeth, however light, in such a denture setup causes the neural end organs in the periodontium to relay this situation to the motor nucleus of the trigeminal nerve in the brainstem. This then disrupts the normal, long-established neural firing pattern that results in depriving the masseter and temporalis muscle fibers of their normal resting sequences (Rosenstiel et al., 2015; Sicher & DuBrul, 1970).
The consequences of a denture construction that results in a teeth-together (closed) bite are similar to the problems experienced by individuals with a clenching habit that include muscle spasms, trauma to teeth and supporting structures, and pain in the temporomandibular joint complex.
THE AIRWAY
Orofacial myologists have determined that among the multifactorial causes of orofacial myofunctional disorders, airway incompetencies (e.g., enlarged tonsils, adenoids, hypertrophied nasal turbinates, and/or allergies) are the primary causes of orofacial myofunctional disorders (Abreu et al., 2008; ASHA, 2019; Mason & Franklin, 2014). Clinicians have learned from experience that myofunctional therapy is destined to fail until airway interferences and allergies have been addressed and resolved.
One of the authors’ experience with a large and active private practice in orofacial myology has led to mandatory evaluations by otolaryngology and allergy specialists before beginning therapy. Anecdotal clinical findings have revealed improvements in sleep disordered breathing in children by allergy management alone or in combination with orofacial myofunctional treatment.
The impact of unresolved airway interferences and allergies on maintaining a normal freeway space can be demonstrated by the following example of an 8-year-old male with airway issues and a resting posture in which the tongue rests interdentally. This resting posture serves to open the freeway space beyond the normal range. The open resting position of the mandible is hypothesized to signal the brain to address this situation. The result is the additional, unwanted eruption of posterior teeth, while anterior teeth are prevented from erupting by the interposed tongue.
Proffit et al. (2013) described a similar scenario of a child with a thumb-sucking habit: “When a thumb or finger is placed between the anterior teeth, the mandible must be positioned downward to accommodate it. The interposed thumb directly impedes incisor eruption. At the same time, the separation of the jaws alters the vertical equilibrium on the posterior teeth, and as a result, there is more eruption of posterior teeth than might otherwise have occurred. Because of the geometry of the jaws, 1 mm of elongation posteriorly opens the bite about 2 mm anteriorly, so this can be a powerful contributor to the development of anterior open bite” (Proffit et al., 2013, p. 138).
These examples of increased, unwanted eruption of posterior teeth with no concomitant anterior teeth eruption are referred to in dentistry as differential dental eruption, the eventual result of which is an anterior open bite malocclusion. When teeth continue to erupt in this scenario, the roots of the erupting teeth do not become exposed, or “grow out of their sockets.” This is because the alveolar bone surrounding the teeth “follows along”.
This process is termed vertical drift of alveolar bone (Mason, 2016).
In these examples, the freeway space cannot resume a normal rest position until the forward, interdental rest position of the tongue or interposed thumb have been corrected. If there are airway or allergy conditions that are not resolved, myofunctional therapy to establish and stabilize a normal freeway space cannot be successful (ASHA, 2019; Mason & Franklin, 2014).
DENTAL ERUPTION SCENARIOS AND THE FREEWAY SPACE
As background, maxillary growth reaches a peak around age 8 years of age, with slight increments in growth continuing to around age 12 when maxillary growth has usually been completed. By contrast, the mandible exhibits a prepubertal and pubertal growth spurt that continues through the teen years, with additional mandibular growth occurring in some individuals well into their 20s (Mason & Proffit, 1974; Padmaja et al., 2014).
The normal sequence of eruption of adult teeth usually occurs in the following manner when the freeway space is normal: teeth in the maxillary arch erupt downward and forward, while the mandibular dentition erupts mostly upward (Harvold, 1968). Despite the difference in the eruption pathways of upper and lower teeth, dental occlusion usually remains stable as continued horizontal growth of the mandible keeps pace with the downward and forward eruption of maxillary teeth. However, the mechanisms of tooth eruption remain controversial (Kjaer, 2014).
In a scenario in which the freeway space is habitually open beyond the normal resting dimension, the normal pathways of dental eruption will be disturbed. The brainstem is hypothesized to be signaled about these changes via the trigeminal nerve, and unwanted dental changes will follow.
In another hypothesized dental eruption scenario, if the freeway space is habitually open beyond the normal rest position with the tongue splayed over the biting surfaces of all lower teeth, the maxillary dentition will continue to erupt in a downward and forward direction, while the tongue inhibits the lower dentition from following suit. The result is the eventual development of a Class II malocclusion. In this scenario, the tongue acts much like an orthodontic functional appliance (Mason, 2016).
TONGUE TIP REST POSITION, TACTILE FEEDBACK, AND THE FREEWAY SPACE
Sensory receptors that produce strong tactile feedback are liberally embedded in the tongue tip, lips, rugae area, and the gingiva overlying the lingual surfaces of lower incisors (Dixon, 1962; Grossman & Hattis, 1967). While many orofacial myologists continue to designate the rugae area as the preferred area of contact for the tongue tip at rest, it should be recognized that there are other acceptable contacts for the tongue tip that many individuals use as a rest position. These include: 1) the tongue tip at the lingual (palatal) surface of upper incisor teeth; and 2) the tongue tip at the lingual side of the lower incisors or overlying gingiva.
An individual who has a resting tongue tip at the lower incisors with a normal freeway space can also have a normal dentition that will remain stable over time. In the opinion of the authors, a clinical caveat related to the freeway space is: no matter the tongue tip rest position, except for an interdental rest posture, the dentition is expected to remain in a stable state when the freeway space is within the normal range.
AN ORTHODONTIC RELAPSE SCENARIO
While it is expected that most orthodontists and other dental specialists can easily identify tongue thrust behaviors, few dental specialists are likely to document the vertical interocclusal resting distance. If this is an accurate clinical scenario, it is incumbent upon orofacial myologists to share information with referral sources about the importance of including measurements of the freeway space in evaluations where airway interferences and allergies are suspected.
The following scenario illustrates how knowledge about the freeway space can have clinical value to orofacial myologists: a referral is made by an orthodontist for orofacial myofunctional therapy, based on the observation that relapse into an anterior open bite is occurring during the orthodontic retention period. The orthodontist opines that the tongue is the likely cause of the relapse into the open bite that has been observed.
In responding to this referral, and if examination of this individual reveals: 1) a lips-together rest posture has been established and stabilized; 2) the tongue rest position is either up or down, but not interdental, and 3) the freeway space is within the normal range, then whatever relapse is occurring is not related to a myofunctional disorder. These three caveats are intended to aid clinicians to know when to refer a patient back to a referral source. This discussion acknowledges the difficult challenge in orthodontic treatment to correct anterior open bites and to maintain the stability of the result over time. Myofunctional therapy can be effective in accomplishing the three caveats mentioned.
A METHOD FOR DOCUMENTING THE FREEWAY SPACE
Background
The anatomy of the mandible and the hinge-type rotation of the mandibular condyles in the temporal fossae explain the downward and slightly posteriorward opening path of the mandible. The result of the mandibular opening phase is more anterior than posterior vertical opening; thus, extraoral measurements with the mandible in a position at rest will reveal the anterior freeway space but not the posterior vertical dimension at molar teeth.
Kinematic recordings have been made of freeway space dimensions in several dental patient categories. Martin and colleagues (2000), used a kinesiograph to measure jaw movements without interfering with the motion of the jaw. Their system used a sensor array strapped to the patient’s head that tracks the spatial location of a magnet fixed on the mandibular incisors. The mandibular position was recorded at rest and during jaw movements in maximum excursions, and during swallowing and chewing.
Vinnakota et al. (2016) and Dagdiya et al. (2019) used lateral facial photos to measure various external landmarks on the face and jaws in determining the freeway space. Mishra et al. (2019) compared the freeway space in edentulous and dentulous patients, with and without a head-stabilizing device.
Documenting the freeway space in dentistry has almost exclusively been associated with the process of denture construction in edentulous individuals. Establishing a normal freeway space is critical to the success of patients adapting to dentures (Rosenstiel et al. 2015; Shillingburg et al. 2012).
Of the many methods described by dentists to measure the dimensions of the freeway space, extraoral measurements at the front of the face prevail (Miralles et al. 2001). An extraoral assessment of the anterior freeway space that can be employed by orofacial myologists is proposed.
Method
Two external measurements are made at the median plane using a measurement device of the clinician’s choosing, such as a millimeter ruler, measuring tape, or Boley gauge. The patient’s lips can remain open in both measurement conditions.
The first measurement is made of the distance between the base of the nose and the bottom of the chin with the patient assuming their usual rest position. Many patients will benefit from supportive instructions as to how to relax the mandible to assume its normal rest posture.
A second measurement repeats the measurement from the base of the nose to the bottom of the chin while the patient bites down to maintain bite closure. The millimeter difference between the two measurements will reveal the patient’s anterior freeway space dimension (Mason, 2020).
As with any measurement method proposed, there will be patients who are not easily measured and may not exhibit differences between the two measurement tasks. An example is children with a long-standing thumb-sucking habit whose posterior dentition has over-erupted by the process of differential dental eruption to the extent that measurements are reduced to 1 mm. Such findings can be useful to orthodontists in definitively determining whether or not differential dental eruption has occurred.
Although differences in the resting interocclusal spaces at the molars may exist when there is a unilateral posterior crossbite or lateral open bite, such differences should not impact the anterior measurement of the freeway space. An adult patient group that may exhibit minimal measurement differences between the occlusion and resting conditions are those with a unilateral mandibular asymmetry and posterior crossbite on the affected side whose mandibular asymmetry is related to remodeling of the condylar head and the glenoid fossa (Oh & Cho, 2020; Takada et al., 2015). These conditions will cause the mandible to rotate toward the affected side to assume the rest position.
In such patients, a reduction in the height of the ramus on the affected side and the lateralization of the mandible upon opening may negate the value of measuring the freeway space.
CONCLUSIONS
It is recommended that documenting the anterior resting vertical occlusal distance, or freeway space, should become a part of initial and final evaluations in orofacial myofunctional therapy for selected patients who exhibit signs of airway interferences and allergies, or whose mandibles are in an open resting position beyond the normal freeway dimension. When myofunctional therapy is utilized to establish and stabilize a normal freeway space with appropriate patients, a positive impact is expected in dental stability and in the rest position of the mandible. It is hoped that the results of therapy, including pre- and post-treatment anterior freeway space measurements, will further enhance discussions with patients, parents, and referral sources.
References
- Abreu, R. R., R. L. Rocha, J. A. Lamounier, and Â. F. M. Guerra. 2008. Etiology, clinical manifestations and concurrent findings in mouth-breathing children. Journal de Pediatrica 84, 6: 529–535. [Google Scholar] [CrossRef]
- Aradya, A., and R. Chowdhary. 2017. Re-evaluation of interarch space determination in fully dentate adults with different facial forms: A clinical study. Indian Journal of Dental Research 28, 6: 613–616. [Google Scholar] [CrossRef] [PubMed]
- ASHA. 2019. Orofacial Myofunctional Disorders. American Speech-Language-HearingAssociation Practice Portal. Available online: www.asha.org/Practice-Portal/Clinical-Topics/Orofacial-Myofunctional-Disorders.
- Clark, H. M., and N. P. Solomon. 2012. Muscle tone and the speech-language pathologist: Definitions, neurophysiology, assessment, and interventions. ASHA. Perspectives on Swallowing and Swallowing Disorders (Dysphagia). [Google Scholar] [CrossRef]
- Dagdiya, M., A. Pakhan, S. Dubey, S. Sathe, and M. Dagdiya. 2019. Determination of freeway space in completely edentulous patients using lateral profile photographs—in vivo. International Journal of Recent Surgical and Medical Sciences 5, 1: 6–9. [Google Scholar] [CrossRef]
- Dixon, A. D. 1962. The position, incidence and origin of sensory nerve terminations in oralmucous membrane. Archives of Oral Biology 7, 39–48. [Google Scholar] [CrossRef]
- Graber, L. W., R. L. Vanarsdall, K. W. Vig, and G. J. Huang. 2016. Orthodontics: Current Principles and Techniques, 6th ed. Elsevier: New York City. [Google Scholar]
- Grossman, R. C., and B. Hattis. 1967. Oral mucosal sensory innervation and sensory experience: A review. Edited by J. F. Bosma. In Symposium on Oral Sensation and Perception. Charles C. Thomas Publisher, Springfield, Il. [Google Scholar]
- Hanson, M. L., and R. M. Mason. 2003. Orofacial Myology: International Perspectives, 2nd ed. Charles C. Thomas, Publisher, Springfield, IL. [Google Scholar]
- Harvold, E. 1968. The role of function in the etiology and treatment of malocclusion. Journal of Orthodontics 54: 883–898. [Google Scholar] [CrossRef]
- Jones, H. R., Jr., and M. Vypotil. 2015. Cranial nerve V. iKnowledge. Available online: https://clinicalgate.com/cranial-nerve-v.
- Kjær, I. 2014. Mechanism of human tooth eruption: review article including a new theory for future studies on the eruption process. Scientifica, vol. 2014, Article ID 341905. [Google Scholar] [CrossRef]
- Lennartsson, B. 1980. Number and distribution of muscle spindles in the masticatory muscles of the rat. Journal of Anatomy 130: 279–288. [Google Scholar]
- Martin, C., J. A. Alarcon, and J. C. Palma. 2000. Kinesiographic study of the mandible in young patients with a unilateral posterior crossbite. American Journal of Orthodontics and Dentofacial Orthopedics 118, 5: 541–548. [Google Scholar] [CrossRef]
- Mason, R. M., and W. R. Proffit. 1974. The tongue thrust controversy: background and recommendations. Journal of Speech and Hearing Disorders 39: 115–132. [Google Scholar] [CrossRef]
- Mason, R., and H. Franklin. 2014. Orofacial myofunctional disorders and otolaryngologists. Otolaryngology: Open access 4: e110. [Google Scholar] [CrossRef]
- Mason, R. M. 2016. For Dentists and Physicians. Available online: http://www.orofacialmyology.com/files/ForDentistsandPhysicians.
- Mason, R. M. 2020. The importance of the freeway space in ENT evaluations of airway interferences. Online Journal of Otolaryngology and Rhinology 3: 554–555. [Google Scholar] [CrossRef]
- Miralles, R., C. Dodds, C. Palazzi, C. Jaramillo, A. Quezada, G. Ormeno, and R. Villegas. 2001. Vertical dimension. Part 1: Comparison of clinical freeway space. Journal of Craniomandibular & Sleep Practice 19, 4: 230–236. [Google Scholar] [CrossRef]
- Mishra, K., D. Hegde, S. Shetty, S. Shah, and A. George. 2019. Evaluation and comparison of freeway space in edentulous and dentulous patients with and without head-stabilizing device. International Journal of Oral Care and Research 7, 3: 65–70. [Google Scholar] [CrossRef]
- Monteith, B. 1984. The role of the free-way space in the generation of muscle pain amongdenture-wearers. Journal of Oral Rehabilitation 11, 5: 483–498. [Google Scholar] [CrossRef]
- Oh, M., and J. Cho. 2020. The three-dimensional morphology of mandible and glenoid fossa as contributing factors to menton deviation in facial asymmetry—retrospective study. Progress in Orthodontics 21: 33. [Google Scholar] [CrossRef]
- Padmaja, S., A. Arora, and A. Valiathan. 2014. Age changes of jaws and soft tissue profile. Scientific World Journal. [Google Scholar] [CrossRef]
- Proffit, W. R., H. W. Fields, and D. M. Sarver. 2013. Contemporary Orthodontics, 5th ed. Mosby: St. Louis. [Google Scholar]
- Proffit, W. R., H. W. Fields, B. Larson, and D. M. Sarver. 2018. Contemporary Orthodontics, 6th ed. Mosby: St. Louis. [Google Scholar]
- Rosenstiel, S., M. Land, and J. Fujimoto, eds. 2015. Contemporary Fixed Prosthodontics. Lippincott Williams & Wilkins. Philadelphia. [Google Scholar]
- Rowland, L. P., ed. 2009. Merritt’s Neurology. Lippincott Williams & Wilkins. [Google Scholar]
- Rowlerson, A., F. Mascarello, D. Barker, and H. Saed. 1988. Muscle-spindle distribution in relation to the fiber-type composition of masseter in mammals. Journal of Anatomy 161: 37–60. [Google Scholar] [PubMed]
- Scutter, S. D., and S. T. Kemal. 2001. The role of the muscle spindles in human masseter. Human Movement Science 20: 489–497. [Google Scholar] [CrossRef]
- Shillingburg, H. T., Jr., D. A. Sather, E. L. Wilson, Jr., J. R. Cain, D. L. Mitchell, L. J. Blanco, and J. C. Kessler. 2012. Fundamentals of Fixed Prosthodontics, 4th ed. Quintessence Publishing Company: Chicago. [Google Scholar]
- Sicher, H., and E. L. DuBrul. 1970. Oral Anatomy. Mosby: St. Louis. [Google Scholar]
- Takada, J., J. Miyamoto, T. Yokota, T. Ono, and K. Moriyama. 2015. Comparison of the mandibular hinge axis in adult patients with facial asymmetry with and without posterior unilateral crossbite. European Journal of Orthodontics 37, 1: 22–27. [Google Scholar] [CrossRef]
- Vinnakota, D. N., K. C. Kanneganti, M. Pulagam, and P. K. R. Karnati. 2016. Freeway space determination using lateral profile photographs: A pilot study. Journal of the Indian Prosthodontic Society 16, 3: 242–247. [Google Scholar] [CrossRef]
- Widmer, C., V. D. Nguyen, H. Chiang, and J. Morris-Wiman. 2012. Increased vertical dimension effects on the masseter muscle fiber phenotype during maturation. Angle Orthodontist 83: 57–62. [Google Scholar] [CrossRef] [PubMed]
- Wiesinger, B., B. Häggman-Henrikson, A. Eklund, A. Wänman, and F. Hellström. 2019. Multimodal Sensory Stimulation of the Masseter Reduced Precision but Not Accuracy of Jaw-Opening Movements. Frontiers in Neuroscience. [Google Scholar] [CrossRef] [PubMed]
- Yabushita, T., J. L. Zeredo, K. Toda, and K. Soma. 2005. Role of occlusal vertical dimension in spindle function. Journal of Dental Research 84, 3: 245–249. [Google Scholar] [CrossRef] [PubMed]
- Yin, C. S., Y. J. Lee, and Y. J. Lee. 2007. Neurological influences of the temporomandibular joint. Journal of Body Work and Movement Therapies 11: 285–294. [Google Scholar] [CrossRef]
© 2020 by the authors. 2020 Robert M. Mason, Honor Franklin, Patricia Grant, Ellen B. Role