Abstract
Objective: To evaluate self-care efficacy on reduction of pain and wakefulness bruxism before the treatment with the stabilization splint. Methods: Sixty patients were divided into two groups: 30 belonging to the group that received the self-care guide (G1) and 30 belonging to the control group (G2) who were advised to wait for the beginning of the treatment with the stabilization splint. G1 received a self-care guide for immediate application before any intervention for bruxism treatment. The instructions were given as tips to follow every day for 1 month. Before being given to the patient, the guide was read aloud and clearly by the researcher and clarifying any patients doubts or questions. To evaluate the evolution of each group, the evaluation of physical symptoms occurred at 2 times (M1 and M2). G1 the efficacy of the self-care guide was tested through patient’s report of pain sensation before and after the use of the guide. The control group (G2) was evaluated at M1 and M2, in order to obtain a parameter of pain evaluation in patients not previously subjected to the treatment. Results: The Self-care group presented statistical significance in relation to the group that did not receive self-care. Conclusion: According to the results obtained it can be verified that the patient’s awareness about this problem and the application of a conservative therapy based on self-care was effective reducing the pain level of patients with wakefulness bruxism.
INTRODUCTION
The term temporomandibular disorder (TMD) is used to refer to a group of diseases that affect the masticatory muscles, TMJ and adjacent structures. TMD can be classified into two major subgroups: joint origin, in which the signs and symptoms are related to TMJ; and muscular origin in which the signs and symptoms are related to the stomatognathic musculature (Donnarumma, Muzilli & Ferreira, 2010). TMD are highly prevalent among females aged 25-40, the most active age group in the population. Among the risk factors, there are parafunctional habits, emotional stress, occlusal condition, trauma and deep pain stimuli (Martins, Garcia, Garbin & Sundefeld 2007; Okenson, 2008). Bruxism is a parafunctional habit characterized by the clenching or grinding of teeth in a continuous way (Frugone Zambra & Rodríguez, 2003), which can also occur semiconsciously or unconsciously (Gusson, 1998; Zuanon, 1999; Moysés, 2006). The development of wakefulness bruxism occurs quietly, semi-conscious or unconscious. It is characterized by the teeth tightening and can often be associated with other parafunctional activities such as biting objects, lips and cheeks (Zuanon, 1999). Sleep bruxism is unconscious, resulting in rhythmic contractions and often producing creaking sounds, cracking or light beating of the teeth (Kato, Thie, Huynh, Miyawaki & Lavigne 2003).
The relationship between bruxism and TMD has been studied by several authors due to the damage that this parafunctional habit can cause in the stomatognathic system (Rosa, Oliveira, Faot, Cury & Garcia., 2008). The non-functional mandibular movements as teeth grinding and clenching and also intense muscular contraction, that occur in bruxism results in an abnormal recruitment of the chewing muscles, which in a hyperfunction state can cause painful symptoms and decrease coordination (Zarb, Carlsson, Sessle & Mohl, 2000), which makes this habit an important contributing factor to changes in TMJ (Ciancaglini, Gherlone & Radaelli, 2001; Rosa et al., 2008; Soares, Miranda, Assencio-Ferreira & Di Ninno 2004; Glaros, Williams & Lausten, 2005; Matheus, Ghelardi, Vega Neto, Tanaka, Almeida & Matheus 2005; Koyano, Tsukiyama, Ichiki & Kuwata, 2008). TMJ alterations have multifactorial etiology as macro and micro traumas, occlusal, psychological and genetic factors and are manifested by painful symptomatology caused for example by trigger points in the musculature or atralgias at the TMJ (Bianchini, 2004; Rosa et al., 2008).
The treatment of patients with TMD is based on the following: a correct diagnosis that is formulated/based on information about possible etiological factors and objective and subjective signs and symptoms of each patient. The protocol of care varies according to the level of impairment of muscular and articular structures and the clinical symptomatology. Therefore, treatment should be initiated focusing on relieving symptoms, reducing pain, restoring function and enabling the patient to resume daily activities (Venancio, Camparis & Lizarelli, 2002; Delboni & Abrão, 2005).
Self-care is highly indicated because it is a simple, non-invasive, and is a cost efficient way to control pain and discomfort, reduce muscle tone, and to improve kinetic parameters and TMJ function. A self-care program includes procedures such as counseling, education (habit reversion techniques and correct use of the jaw), thermal therapy, self-massage, stretching, stabilization, coordination and mobilization (Michelotti, de Wijer, Steenks & Farella 2005). Well informed individuals are more likely to actively participate in their care, make more informed decisions and adhere fully to treatment (Epestein, Alper & Quill, 2004). The aim of the present study was to evaluate the efficacy of self-care to reduce the parafunctional habit of wakefulness bruxism and pain, before starting treatment with the stabilization splint.
METHODS
This project was approved by the Ethics Committee on Human Research of Federal University of Juiz de Fora (Minas Gerais, Brazil). Sixty male and female patients, between 18 and 70 years old, previously diagnosed with wakefulness bruxism and myofascial pain were selected by the Clinic of Diagnostic and Guidance Service for Patients with Temporomandibular Disorder (“Serviço ATM”) and the discipline of Temporomandibular Disorder of School of Dentistry - Federal University of Juiz de For a (Minas Gerais, Brazil), according to Research Diagnostic Criteria (RDC/TMD Axis I) (Dworkin and Le Resche, 1992). All patients were asked to sign a free and informed consent form, in duplicate, ensuring their free participation in the study. Patients who were already subjected to any other therapeutic protocol for bruxism treatment, such as stabilization splints, medication, physical therapy, acupuncture and/or those without the diagnosis of myofascial pain, were excluded.
The patients were randomly divided into two groups: 30 patients were placed in the group that received the guidelines for self-care at the initial consultation (G1) and 30 patients were placed in the control group (G2) and were only asked to wait for the start of treatment with the stabilization splint. Prior to the beginning of the evaluations, the pain intensity of every patient was measured using the Visual Analogue Scale (VAS).
Patients in G1 received self-care guidelines, based on the literature and adapted to an easy-to-understand language as tips to follow with the purpose of stimulating self-care, which was organized into the following sections: sleep hygiene; feeding care; self-medication; exercises to obtain myofunctional balance and postural habits; care for immediate application before any therapeutic intervention for wakefulness bruxism. The instructions were followed every day during a period of 1 month. Before being given to the patient, the guide was read aloud and clearly by the researcher and clarifying any patients doubts about the instructions. The change in self-care habits were verified according to the feedback of each patient at the end of 1 month. In order to analyze the symptomatic evolution of individuals from the sample of each group and evaluate the efficacy of therapy, physical symptoms were evaluated twice using the VAS: Moment 1 (M1) - prior to treatment; Moment 2 (M2) - one month after starting treatment with self-care.
The verification of treatment efficacy through the evolution of the physical symptoms was performed through an intra-group evaluation by the Wilcoxon non-parametric test in order to verify whether the values obtained before and after the intervention were statistically different. The non-parametric Mann-Whitney test was used to compare the analog pain scales between both groups. SPSS for Windows 15.0 software was used for statistical analyses and probability values of p<0.05 were considered statistically significant.
RESULTS
In a sample of 60 patients, with age range of 38 to 75 years old, composed of 53 women (88.3%) and 7 men (11.7%), there was no statistically significant difference (p> 0.001) between gender in relation to pain before or after self-care. Regarding the mean age of the G1 sample (40 years), there was a difference between the median pre-self-care pain. The younger group (younger than 40 years) had a median of 8 and an interquartile range of ± 4, and the oldest group (age over 40 years) had a median of 10 and an interquartile range of ± 2, statistically significant (p <0.001). Thus, this data corroborates the self-perception of more intense pain among the older patients prior to the use of the stabilization splint.
The difference between pre and post pain self-care was statistically significant (p <0.001). Table 1 presents data indicating the change in pain levels between the two times of measurement in the G1 group according to VAS. The self-care group was statistically significant in relation to Mann Whitney test (p <0.001), unlike the group that did not receive the self-care guides (p> 0.001). The difference between these medians is shown in Figure 1. Regarding the patients in the control group (G2), because they did not receive the self-care guidelines, their pain sensations remained the same as those measured on the first day through VAS, as shown in Table 2.

Table 1.
Pain levels between the two moments in G1 according to VAS.
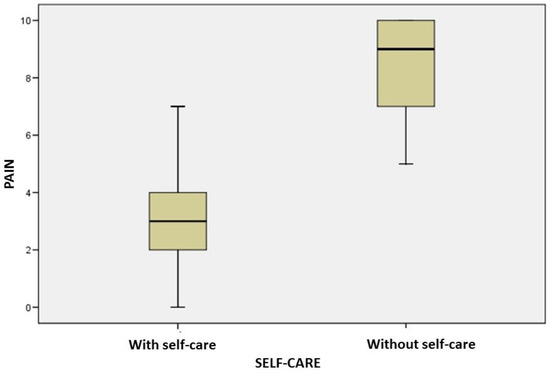
Figure 1.
Difference between pre and post pain self-care.

Table 2.
Difference between initial pain (M1) of the control group that remained the same after a period of one month, at the time of the second evaluation.
DISCUSSION
TMD refers to a group of changes in the masticatory system characterized by the presence of TMJ pain and/or masticatory muscles, joint sound, deviations or restrictions of mandibular movements (Pereira, Andrade, Costa & Portal, 2005; Donnarumma et al., 2010; Versiani, Alves and Silva Junior, 2009; Michelotti, Iodice, Vollaro, Steenks & Farella, 2012; Alfaya, Zukowska, Uemoto, Oliveira, Martinez, Garcia et al., 2013; Campi, Camparis, Jordani & Gonçalves, 2013; Moraes, Sanches, Ribeiro & Guimarães, 2013; Miranda, Maia, Abdon, Torquato & Santos Junior, 2014). Due to the interrelationship between physical and emotional symptoms, there is growing search for the integrative treatment model, which includes psychosocial approaches to the treatment of painful conditions. Scientific literature has shown that behavioral and educational modalities are effective options in the treatment of chronic pain conditions, including TMD. Such educational and behavioral approaches seek to change the perception and evaluation of pain and reduce the suffering and psychosocial changes that accompanies pain (Campi et al., 2013). Education and self-care are approaches based on the pain biopsychosocial model. The existing literature, although not extensive, indicates positive results regarding the application of education and self-care methods in chronic painful TMD, contributing to the improvement of pain symptoms and discomfort (Michelotti et al., 2012; Campi et al., 2013). This was demonstrated in the present study, after the application of the self-care guides.
Okeson, (2008), describes that for a disease to install in the TMJ, it is necessary to have predisposing factors (predisposing the patient to the risk of TMD or orofacial pain: like biomechanical, genetic and psychological factors), triggering factors (things that cause the onset of the disorder: macrotraumas and microtraumas) and perpetuating factors (which interfere with treatment and control: parafunction, hormonal and/or psychosocial factors associated with any predisposing or triggering factor). In order to avoid the last two factors, educational work is always necessary (Michelotti et al., 2012; Miranda et al., 2014). The body is malleable and is in a constant state of adaptation and change, thus requiring constant care. The well-educated and informed patient can become more responsible for their healing process, avoiding adverse factors and being motivated with the treatment (Miranda et al., 2014). In this study, a similar characteristic was observed, since the patients who received the self-care instructions through the guide were able to control their parafunction as per their report and, consequently, their pain sensations were said to be reduced according to the VAS at the time of the second evaluation (M2) when compared to the first one (M1). Although systemic use of medications and the use of interocclusal splints are widely disseminated, patient awareness of their problem seems to be the most relevant therapeutic tool in the clinical approach of bruxism (Pereira, Negreiros, Scarparo, Pigozzo, Consani & Mesquita, 2006). There are suggestive evidences that the degree of success of therapy for this disorder is related to the efficient elucidation of the problem and control of the habit by the patient himself/herself (Pereira et al., 2006; Versiani et al., 2009; Campi et al., 2013; Miranda et al., 2014). In an attempt to obtain a control of parafunction, it is necessary to establish therapy based mainly on two aspects: (1) advise and educate the patient on the possible triggering factors, aiming for self-control when possible; (2) restore normal function of the masticatory apparatus, especially muscles and joints, with protection for the soft and hard structures (Pereira et al., 2006). Some studies indicate that the use of guidelines should be linked to other resources. Truelove, Huggins, Manc & Dworkin (2006) concluded that stabilization splint was less effective than conservative treatment coupled with self-care guidelines. Michelotti et al. (2005) compared treatments based on orientation of self-care and home exercises combined with orientation of self-care and after three months found that the group that received only orientation obtained a 57% improvement and that when the home exercises were combined with the orientation they obtained 77% improvement. Self-care guidelines, clarification of risk factors and training of home exercises provide psychological gains, as they reduce anxiety (Truelove et al., 2006). In the present study, the use of guidelines and counseling was used without the concomitant use of the stabilization splint, in order to stimulate self-care, resulting in a reduction in the patients’ pain level. Cognitive-behavioral therapy, with self-care, is a safe, conservative and easy-to-apply intervention (Versiani et al., 2009; Campi et al., 2013). It is important that this treatment modality becomes part of the therapeutic arsenal provided by service centers that deal with orofacial pain, especially considering that not all patients have access to physiotherapeutic and psychotherapeutic treatment necessary for the desired changes in behaviors and habits (Versiani et al., 2009; Donnarumma et al., 2010).
CONCLUSION
According to the results obtained in the present study, it can be verified that patient’s awareness about their problem and the application of a conservative therapy based on self-care was effective in reducing the wakefulness bruxism and the pain that accompanies it in these patients. Considering the small sample and the importance of self-care in TMD and bruxism treatments, controlled studies on this subject, including larger samples and longer assessment are suggested.
APPENDIX A: SELF-CARE GUIDE
| SLEEP HYGIENE GUIDELINES (ORLANDI et al., 2012) |
| Try to sleep every day at the same time. Thus, your body will always prepare to sleep at the same time. You will fall asleep more quickly in the coming weeks! |
| Do not use the room where you sleep to work, study or eat. It should just be the place to sleep. |
| Avoid watching TV before bed. Watching TV can leave you agitated and can lessen your sleep! |
| Rest your mind and relax your body for at least an hour before bedtime. Do not solve big problems at this time of the day. |
| Do not drink coffee, tea and chocolate after 5 pm. |
| Do not drink alcohol before going to bed. Although they help to relax, they disturb the quality of your sleep; if possible, have a glass of milk. |
| If you are a smoker, do not smoke for two to three hours before bed. |
| Try to make lighter meals over dinner. Good choices are salad and vegetables. Many greasy foods like fried foods, for example, make your stomach heavier and hamper your sleep! |
| Keep your room at a pleasant temperature. Excessive heat and cold change the quality of your sleep. Also, wrap yourself well, to avoid possible muscular “contractures”. |
| Noises and clarity can lead to poor sleep. Therefore, seek to sleep where there is silence and low light. |
| Physical exercises improve the quality of your sleep. But beware: try to work out in the morning or in the afternoon. If done close to bedtime, they will decrease the quality of your sleep. It is also important that you practice exercises that you enjoy, that leave you happy and excited. In addition to improving the quality of your sleep, you stay in shape. |
| Try to elaborate a routine before going to bed. For example: putting the cat out, locking the doors, brushing teeth .... This makes your body used and reminds you that it is time to go to sleep, reducing the time you wait for sleep to arrive. |
| Warm baths before bedtime are recommended to combat your insomnia. They relax your body and your mind. |
| Do not doze more than twice during the same week. This decreases the need for nighttime sleep. |
| Always sleep in a bed where you feel comfortable. This is very important so that you can completely relax to fall asleep. |
| Avoid “fighting” with the bed. Sleep only long enough to feel good. Do not stay in bed longer than the time required. |
| When you feel sleepless, get up and do something tiring or repetitive, such as reading a book from an uninteresting subject. |
| Say no to medicines! You should take sleeping pills only if they are taken with medical advice. |
REFERENCES
- Alencar, F. P. G., Jr. 2005. Oclusão, Dores Orofaciais e Cefaleias, 1st ed. São Paulo: Santos. [Google Scholar]
- Alfaya, T. A., H. R. Zukowska, L. Uemoto, S. S. I. Oliveira, O. E. R. Martinez, M. A. C. Garcia, and et al. 2013. Alterações psicossomáticas e hábitos parafuncionais em indivíduos com disfunção temporomandibular. Saúde e Pesquisa 6, 2: 135–139. [Google Scholar]
- Bianchini, E. M. G. 2004. Articulação temporomandibular e fonoaudiologia. Tratado de fonoaudiologia, São Paulo: Roca. [Google Scholar]
- Campi, L. B., C. M. Camparis, P. C. Jordani, and D. A. G. Gonçalves. 2013. Influência de abordagens biopsicossociais e autocuidados no controle das disfunções temporomandibulares crônicas. Revista Dor 14, 3: 219–222. [Google Scholar] [CrossRef]
- Ciancaglini, R., E. F. Gherlone, and G. Radaelli. 2001. The relationship of bruxism with craniofacial pain and symptoms from the masticatory system in adult population. Journal of Oral Rehabilitation 28, 9: 842–848. [Google Scholar] [CrossRef] [PubMed]
- Delboni, M. E. G., and J. Abrão. 2005. Estudo dos sinais de DTM em pacientes ortodônticos assintomáticos. Dental press Ortodontia e Ortopedia Facial 10, 4: 88–96. [Google Scholar] [CrossRef]
- Donnarumma, M. D. C., C. A. Muzilli, C. Ferreira, and K. Nemr. 2010. Disfunções Temporomandibulares: Sinais, sintomas e abordagem multidisciplinar. CEFAC 5, 2: 788–794. [Google Scholar] [CrossRef]
- Dworkin, S. F., and L. Le Resche. 1992. Research diagnostic criteria for temporomandibular disorders: Review, criteria, examinations and specificarions, critique. Journal Craniomandibular Disorders 6, 4: 301–55. [Google Scholar]
- Epestein, R. M., B. S. Alper, and T. E. Quill. 2004. Communicating evidence for participatory decision making. Journal of the American Medic Association 291, 19: 2359–2366. [Google Scholar] [CrossRef]
- Frugone Zambra, R. E., and C. Rodríguez. 2003. Bruxismo. Avances en Odontoestomatologia 19, 3: 123–130. [Google Scholar] [CrossRef]
- Glaros, A. G., K. Williams, and L. Lausten. 2005. The role of parafunctions, emotions and stress in predicting facial pain. Journal of American Dental Association 136, 4: 451–458. [Google Scholar] [CrossRef]
- Gusson, D. G. D. 1998. Bruxismo em crianças. Jornal Brasileiro de Odontopediatria e Odontologia do Bebê 1, 2: 75–79. [Google Scholar] [CrossRef]
- Jardini, R. S. R., L. S. R. Ruiz, and M. A. A. Moysés. 2006. Electromyographic analysis of masseter buccinators muscles with pro-fono facial exercises use in bruxers. The Journal of Craniomandibular Practice 24: 29–37. [Google Scholar] [CrossRef] [PubMed]
- Kato, T., N. M. Thie, N. Huynh, S. Miyawaki, and G. J. Lavigne. 2003. Topical review: Sleep bruxism and the role of peripheral sensory influences. Journal of Orofacial Pain 17, 3: 191–213. [Google Scholar] [PubMed]
- Koyano, K., Y. Tsukiyama, R. Ichiki, and T. Kuwata. 2008. Assessment of bruxism in the clinic. Journal of Oral Rehabilitation 35, 7: 495–508. [Google Scholar] [CrossRef]
- Martins, R. J., A. R. Garcia, C. A. S. Garbin, and M. L. M. M. Sundefeld. 2007. Associação entre classe econômica e estresse na ocorrência da disfunção temporomandibular. Revista Brasileira de Epidemiolgia 10, 2: 215–222. [Google Scholar] [CrossRef]
- Matheus, R. A., I. R. Ghelardi, D. B. Vega Neto, E. E. Tanaka, S. M. M. Almeida, and A. F. Matheus. 2005. A relação entre os hábitos parafuncionais e a posição do disco articular empacientes sintomáticos para disfunção temporomandibular. Revista Brasileira de Odontologia 62, 1/2: 9–12. [Google Scholar]
- Miranda, M. H., D. A. C. Maia, A. P. V. Abdon, J. A. Torquato, and F. F. U. Santos Junior. 2014. Escola de posturas pode melhorar a qualidade de vida na disfunção temporomandibular? Cadernos ESP 8, 1: 30–40. [Google Scholar]
- Michelotti, A., A. de Wijer, M. Steenks, and M. Farella. 2005. Home-exercises for the management of non-specific temporomandibular disorders. Journal of Oral Rehabilitation 32, 11: 779–785. [Google Scholar] [CrossRef]
- Michelotti, A., G. Iodice, S. Vollaro, M. H. Steenks, and M. Farella. 2012. Evaluation of the short-term effectiveness of education versus a occlusal splint for the treatment of myofascial pain of the jaw muscles. Journal of the American Dental Association 143, 1: 47–53. [Google Scholar] [CrossRef] [PubMed]
- Moraes, A. R., M. L. Sanches, E. C. Ribeiro, and A. S. Guimarães. 2013. Therapeutic exercises for the control of temporomandibular disorders. Dental Press Journal of Orthodontics 18, 5: 134–139. [Google Scholar] [CrossRef]
- Okeson, J. P. 2008. Tratamento das desordens temporomandibulares, 7th ed. Rio de Janeiro. [Google Scholar]
- Pereira, K. N. F., L. L. S. Andrade, M. L. G. Costa, and T. F. Portal. 2005. Sinais e sintomas de pacientes com Disfunção Temporomandibular. CEFAC 7, 2: 221–228. [Google Scholar]
- Pereira, R. P. A., W. A. Negreiros, H. C. Scarparo, M. N. Pigozzo, R. L. X. Consani, and M. F. Mesquita. 2006. Bruxismo e qualidade de vida. Odonto ciência 221, 52: 185–190. [Google Scholar]
- Rosa, R. S., P. A. Oliveira, F. Faot, A. A. B. D. Cury, and R. C. M. R. Garcia. 2008. Prevalência de desordens temporomandibulares e suas associações em jovens universitários. Revista Gaucha de Odontologia 56, 2: 121–126. [Google Scholar]
- Soares, I. S. Q., A. F. V. Miranda, V. J. Assencio-Ferreira, and C. Q. M. S. Di Ninno. 2004. Bruxismo: Desempenho da mastigação em adultos jovens. CEFAC 6, 4: 358–362. [Google Scholar]
- Truelove, E., K. H. Huggins, L. Manc, and S. F. Dworkin. 2006. The efficacy of traditional, low-cost and nonsplint therapies for temporomandibular disorder: A randomized controlled trial. Journal of the American Dental Association 137, 8: 1099–1107. [Google Scholar] [CrossRef] [PubMed]
- Venancio, R. A., C. M. Camparis, and R. F. Z. Lizarelli. 2002. Laser no tratamento de desordens temporomandibulares. Jornal Brasileiro de Oclusão, ATM e dor orofacial 2, 7: 229–234. [Google Scholar]
- Versiani, A. H. V., B. M. F. Alves, and A. A. Silva Junior. 2009. O papel das orientações cognitivo comportamentais aos pacientes com dor orofacial-Uma breve revisão. Migrâneas cefaleias 12, 1: 25–28. [Google Scholar]
- Zarb, G. A., G. E. Carlsson, B. J. Sessle, and N. D. Mohl. 2000. Disfunção na articulação temporomandibular e dos músculos da mastigação. São Paulo: Santos. [Google Scholar]
- Zuanon, A. C. 1999. Bruxismo infantil. Odontologia clínica 9: 41–44. [Google Scholar]
© 2018 by the authors. 2018 Tainara Lopes de Castro Bastos, Rafael de Almeida Spinelli Pinto, Isabela Maddalena Dias, Isabel Cristina Gonçalves Leite, Fabíola Pessôa Pereira Leite