Quantitative Evaluation of the Orofacial Morphology: Anthropometric Measurements in Healthy and Mouth-Breathing Children
Abstract
:INTRODUCTION
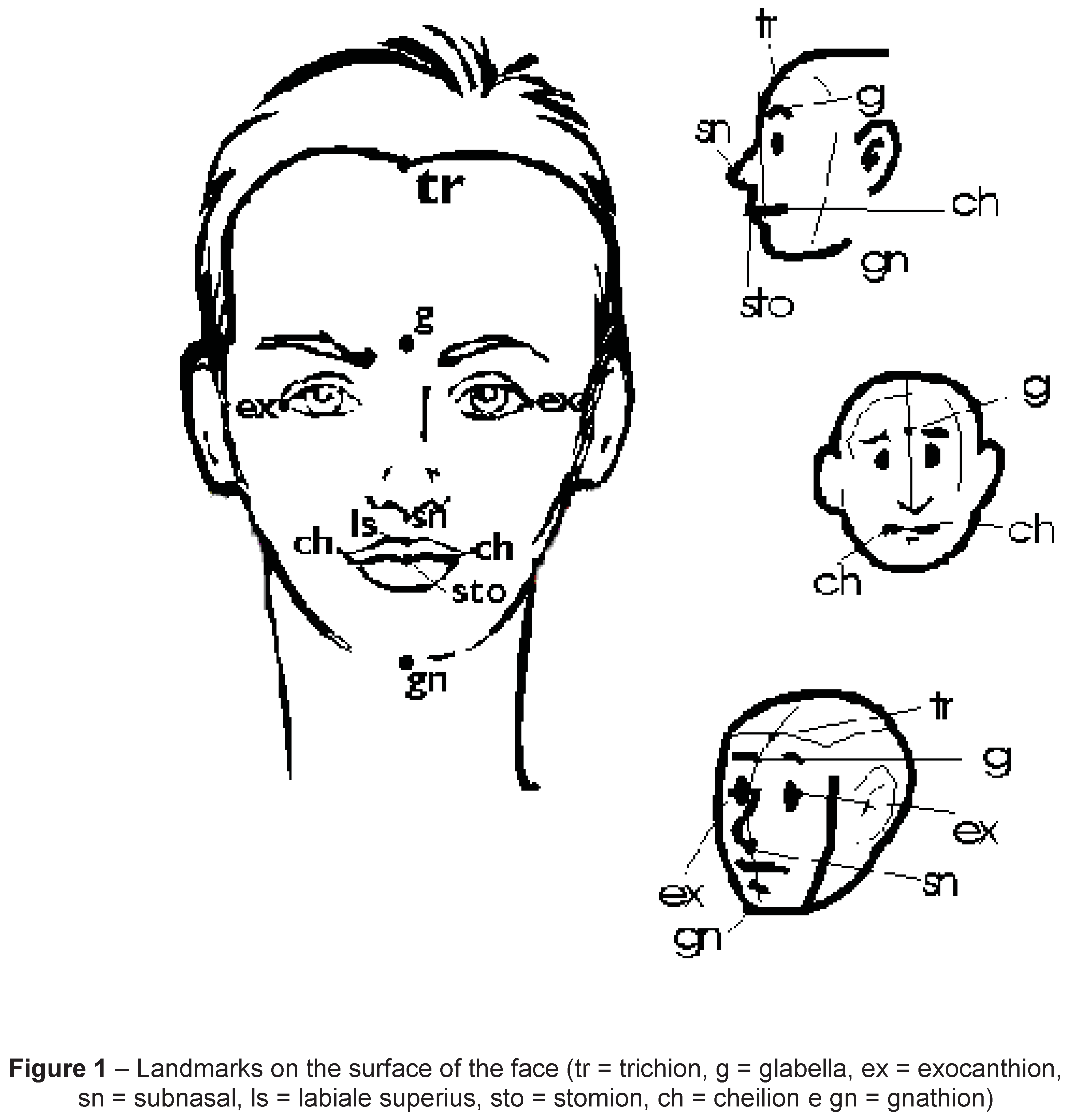
METHODS
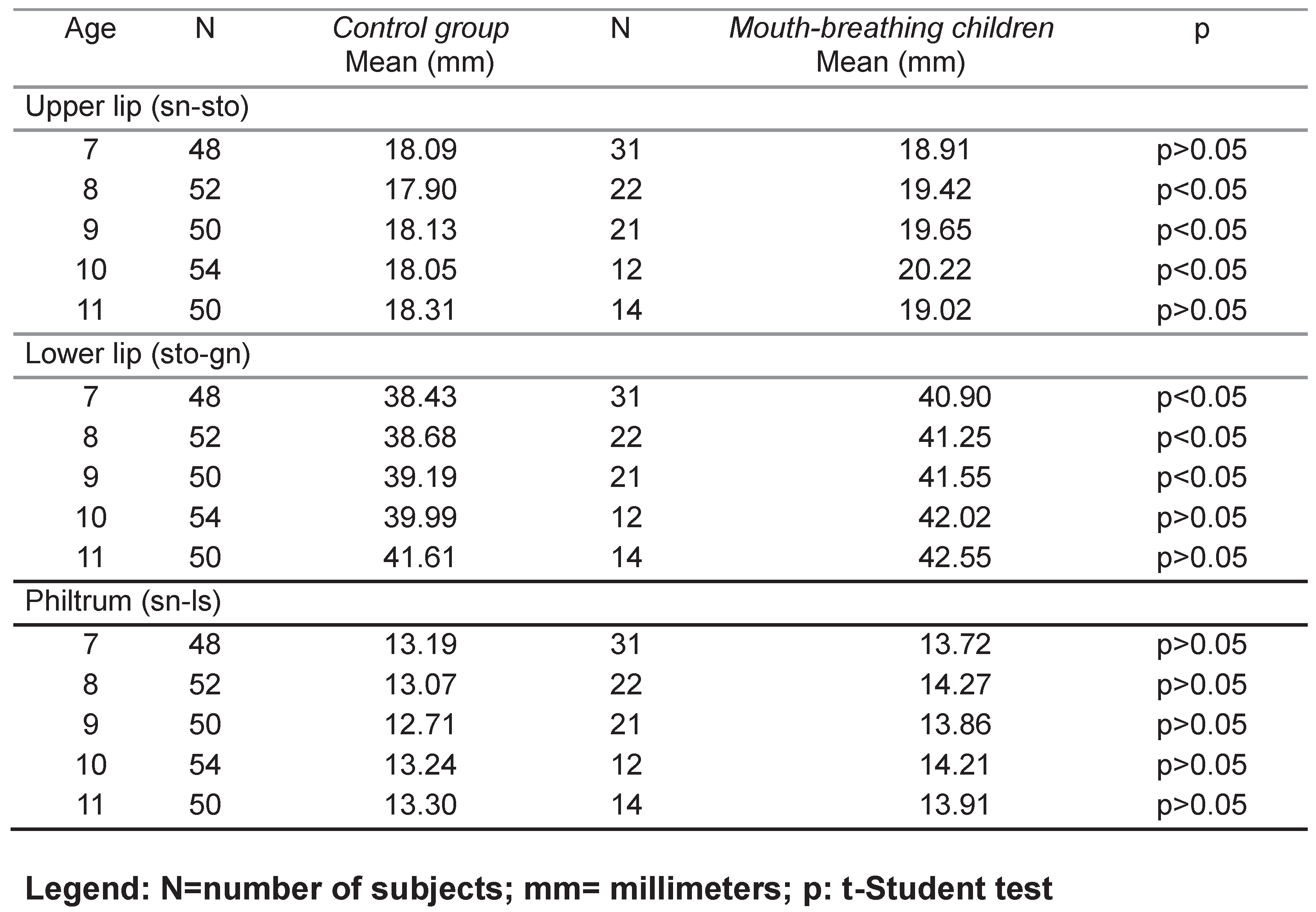
RESULTS
DISCUSSION
CONCLUSIONS
REFERENCES
- Allanson, J.E., and T.R.P. Cole. 1996. Sotos syndrome: evolution of facial phenotype subjective and objective assessment. Am J Med Genet 65: 13–20. [Google Scholar] [CrossRef]
- Andrade, F.V., D.V. Andrade, A.S. Araújo, A.C.C Ribeiro, L.D.G. Deccax, and K. Nemr. 2005. Alterações estruturais de órgãos fonoarticulatórios e más oclusões dentárias em respiradores orais de 6 a 10 anos. Revista Cefac 7, 3: 318–25. [Google Scholar]
- Bianchini, E.M.G. 1998a. Mastigação e ATM: avaliação e terapia. In Fundamentos em fonoaudiologia - aspectos clínicos da motricidade oral. Edited by I.Q. Marchesan. Rio de Janeiro: Guanabara Koogan, pp. 37–49. [Google Scholar]
- Bianchini, E.M.G. 1998b. A cefalometria nas alterações miofuncionais orais – diagnóstico e tratamento fonoaudiológico, 4a Ed. ed. Carapicuíba: Pró-Fono. [Google Scholar]
- Bianchini, E.M.G. 2000. Avaliação fonoaudiológica da motricidade oral: anamnese, exame clínico, o quê e por que avaliar. In Articulação temporomandibular: implicações, limitações e possibilidades fonoaudiológicas. Edited by E.M.G. Bianchini. Carapicuíba: Pró-fono, pp. 191–253. [Google Scholar]
- Borman, H., F. Ozgur, and G. Gursu. 1999. Evaluation of soft-tissue morphology of face in 1,050 young adults. Annals of Plastic Surgery 42, 3: 280–8. [Google Scholar] [CrossRef] [PubMed]
- Budai, M., L.G. Farkas, B. Tompson, M. Katic, and C.R. Forrest. 2003. Relation between anthropometric and cephalometric measurements and proportions of the face of healthy young white adult men and women. Journal of Craniofacial Surgery 14, 2: 154–61. [Google Scholar] [CrossRef]
- Cattoni, D.M. 2003a. Exame fonoaudiológico: medidas faciais em crianças leucodermas sem queixas fonoaudiológicas [dissertação]. São Paulo: Universidade de São Paulo. [Google Scholar]
- Cattoni, D.M. 2003b. Avaliação quantitativa das estruturas orofaciais. In Respiração oral. Edited by L.H. Krakauer and R.C. Marchesan Di Francesco I.Q. São José dos Campos: Pulso, pp. 81–8. [Google Scholar]
- Cattoni, D.M. 2004. Alterações da mastigação e deglutição. In Tratado de fonoaudiologia. Edited by L.P. Ferreira, D.M. Befi-Lopes and S.C.O. Limongi. São Paulo: Roca, pp. 277–91. [Google Scholar]
- Cattoni, D.M. 2006a. O uso do paquímetro na avaliação da morfologia orofacial. Revista da Sociedade Brasileira de Fonoaudiologia 11, 1: 52–8. [Google Scholar]
- Cattoni, D.M. 2006b. O uso do paquímetro na motricidade orofacial: procedimentos de avaliação. Barueri: Pró-fono. [Google Scholar]
- Cattoni, D.M., and F.D.M. Fernandes. 2004. Medidas e proporções faciais em crianças: contribuições para a avaliação miofuncional orofacial. Pró-fono 16, 1: 7–18. [Google Scholar]
- Cattoni, D.M., and F.D.M. Fernandes. 2005. Comparação das medidas antropométricas faciais entre crianças brasileiras e norte-americanas. XIII Congresso Brasileiro de Fonoaudiologia, 2005, Santos, Revista da Sociedade Brasileira de Fonoaudiologia [CD-ROM]. (Supl especial). [Google Scholar]
- Cattoni, D.M., F.D.M. Fernandes, I.Q. Marchesan, and M.R.D.O. Latorre. 2003. Medidas antropométricas faciais em crianças segundo períodos da dentição mista. Revista Cefac 5, 1: 21–29. [Google Scholar]
- Cattoni, D.M., F.D.M. Fernandes, C.R.F. Andrade, and M.R.D.O. Latorre. 2005. Estudo sobre as medidas faciais em crianças: correlações com alteração de mordida e uso de aparelho ortodôntico. Revista da Sociedade Brasileira de Fonoaudiologia 10, 1: 1–6. [Google Scholar]
- Choe, K.S., A.P. Sclafani, J.A. Litner, G.P. Yu, and T. Romo. 2001. The Korean American woman’s face: anthropometric measurements and quantitative analysis of facial aesthetics. Archives of Facial Plastic Surgery 6: 244–52. [Google Scholar] [CrossRef] [PubMed]
- Di Francesco, R.C. 2003a. Conseqüências da respiração oral. In Respiração oral. Edited by L.H. Krakauer, R.C. Di Francesco and I.Q. Marchesan. São José dos Campos: Pulso, pp. 19–25. [Google Scholar]
- Di Francesco, R.C. 2003b. Crescimento craniofacial e distúrbios da respiração oral do ponto de vista otorrinolaringológico. In Respiração oral. Edited by L.H. Krakauer, R.C. Di Francesco and I.Q. Marchesan. São José dos Campos: Pulso, pp. 27–35. [Google Scholar]
- Farkas, L.G. 1994a. Examination. In Anthropometry of the head and face, Edited by L.G. Farkas. , 2nd ed. New York: Raven Press, pp. 3–56. [Google Scholar]
- Farkas, L.G. 1994b. Sources of error in anthropometry and anthroposcopy. In Anthropometry of the head and face, 2nd ed. Edited by L.G. Farkas. New York: Raven Press, pp. 57–70. [Google Scholar]
- Farkas, L.G., and C.K. Deutsch. 1996. Anthropometric determination of craniofacial morphology [editorial]. American Journal of Medical Genetics (1): 1–4. [Google Scholar] [CrossRef] [PubMed]
- Farkas, L.G., and J.C. Posnick. 1992. Growth and development of regions units in the head and face based on anthropometric measurements. Cleft Palate-Craniofacial Journal 29, 4: 301–2. [Google Scholar] [CrossRef] [PubMed]
- Farkas, L.G., J.C. Posnick, Hreczko, and M. T. 1992a. Growth patterns of the face: a morphometric study. Cleft Palate-Craniofacial Journal 29, 4: 308–15. [Google Scholar] [CrossRef]
- Farkas, L.G., J.C. Posnick, T.M. Hreczko, and G.E. Pron. 1992b. Growth patterns of the nasolabial region: a morphometric study. Cleft Palate-Craniofacial Journal 29, 4: 318–24. [Google Scholar] [CrossRef]
- Farkas, L.G., T.M. Hreczko, and M.J. Katic. 1994a. Craniofacial norms in North American Caucasians from birth (one year) to young adulthood. In Anthropometry of the head and face, 2nd ed. Edited by L.G. Farkas. New York: Raven Press, pp. 241–312. [Google Scholar]
- Farkas, L.G., and R.C.K Ngim Venkatadri. 1994b. Racial and ethnic morphometry differences in the craniofacial complex. In Anthropometry of the head and face, 2nd ed. Edited by L.G. Farkas. New York: Raven Press, pp. 201–18. [Google Scholar]
- Farkas, L.G., T.M. Hreczko, M.J. Katic, and C.R. Forrest. 2003. Proportion indices in craniofacial regions of 284 healthy North American white children between 1 and 5 years of age. Journal of Craniofacial Surgery 14, 1: 13–28. [Google Scholar] [CrossRef]
- Fonseca, R.A., T.A. Tucci, R.C.L. Rodrigues, I.C.D. Gomes, and E.M.G. Bianchini. 2005. A correlação entre o ceceio frontal e o crescimento infantil. Revista da Sociedade Brasileira de Fonoaudiologia 10, 4: 211–7. [Google Scholar]
- Hunter, A.G.W. 1996. Craniofacial anthropometric analysis in several types of chondrodysplasia. American Journal of Medical Genetics 65: 5–12. [Google Scholar] [CrossRef]
- Jardini, R.S.R. 1999. Uso do exercitador labial: estudo preliminar para alongar e tonificar os músculos orbiculares orais. Pró-fono 11, 1: 8–12. [Google Scholar]
- Jardini, R.S.R. 2005. Avaliação facial a partir da relação eletromiográfica e antropométrica do músculo bucinador. Revista da Sociedade Brasileira de Fonoaudiologia 10, 3: 161–7. [Google Scholar]
- Junqueira, P. 2004. Avaliação e diagnóstico fonoaudiológico em motricidade oral. In Tratado de fonoaudiologia. Edited by L.P. Ferreira, D.M. Befi-Lopes and S.C.O. Limongi. São Paulo: Roca, pp. 230–6. [Google Scholar]
- Junqueira, P.A.S., R.C. Di Francesco, P. Trezza, F.E. Zeratti, R. Frizzarini, and M.E.J. Faria. 2002. Alterações funcionais do sistema estomatognático pré e pós-adenoamigdalectomia. Pró-fono 14, 1: 17–22. [Google Scholar]
- Le, T.T., L.G. Farkas, R.C.K. Ngim, S. Levin, and C.R. Forrest. 2002. Proportionality in Asian and North American Caucasian faces using neoclassical facial canons as criteria. Aesthetic Plastic Surgery 26, 1: 64–9. [Google Scholar] [CrossRef]
- Lessa, F.C.R, C. Enoki, M.F.N. Feres, F.C.P. Valera, W.T.A. Lima, and M.A.N. Matsumoto. 2005. Influência do padrão respiratório na morfologia craniofacial. Revista Brasileira de Otorrinolaringologia 71, 2: 156–60. [Google Scholar] [CrossRef] [PubMed]
- Marchesan, I.Q. 1998. Avaliação e terapia dos problemas da respiração. In Fundamentos em fonoaudiologia - aspectos clínicos da motricidade oral. Edited by I.Q. Marchesan. Rio de Janeiro: Guanabara Koogan, pp. 23–36. [Google Scholar]
- Marchesan, I.Q. 2000. The speech pathology treatment with alterations of the stomatognathic system. International Journal of Orofacial Myology 26: 5–12. [Google Scholar] [CrossRef]
- Marchesan, I.Q. 2004. Frênulo lingual: proposta de avaliação quantitativa. Revista Cefac 6, 3: 288–93. [Google Scholar]
- Miyajima, K., J.A. McNamara, T. Kimura, S. Murata, and T. Iizuka. 1996. Craniofacial structure of Japanese and European-American adults with normal occlusions and well-balanced faces. American Journal of Orthodontics and Dentofacial Orthopedics 110: 431–8. [Google Scholar] [CrossRef]
- Moore, E.S, R.E Ward, P.L. Jamison, C.A. Morris, P.I. Bader, Hall, and D. B. 2001. The subtle facial signs of prenatal exposure to alcohol: an anthropometric approach. Journal of Pediatrics 139, 2: 215–9. [Google Scholar] [CrossRef]
- Pierotti, S. 2004. Atuação fonoaudiológica na estética facial. In Comitê de Motricidade Orofacial – SBFa. Motricidade orofacial: como atuam os especialistas. Pulso: São José dos Campos, pp. 281–7. [Google Scholar]
- Porter, J.P. 2004. The average African American male face: an anthropometric analysis. Archives of Facial Plastic Surgery 6: 78–81. [Google Scholar] [CrossRef] [PubMed]
- Quintal, M., A. Tessitore, J.R. Paschoal, and L.N. Pfeilsticker. 2004. Quantificação da paralisia facial com paquímetro digital. Revista Cefac 6, 2: 170–6. [Google Scholar]
- Rodrigues, K.A., A.P. Lefèvre, L.B. Mott, D. Tugumia, and P.L. Pena. 2003. Análise comparativa entre o lado de predominância mastigatória e medidas da mandíbula por meio do paquímetro. Revista Cefac 5: 347–51. [Google Scholar]
- Rodrigues, H.O.S.N., S.R. Faria, F.S.G. Paula, and A.R. Motta. 2005. Ocorrência de respiração oral e alterações miofuncionais orofaciais em sujeitos em tratamento ortodôntico. Revista Cefac 7, 3: 356–62. [Google Scholar]
- Seikel, J.A., D.W. King, and D.G. Drumright. 2005. Physiology of mastication and deglutition. In Anatomy & physiology for speech, language, and hearing, 3rd ed. Edited by J.A. Seikel, D.W. King and D.G. Drumright. New York: Thomson: pp. 391–405. [Google Scholar]
- Shaner, D.J., S. Bamforth, A.E. Peterson, and O.B. Beattie. 1998. Technical note: different techniques, different results - comparison of photogrammetric and caliper-derived measurements. American Journal of Physical Anthropology 106, 4: 547–52. [Google Scholar] [CrossRef]
- Silva, H.J., and D.A. Cunha. 2003. Considerações sobre o uso do paquímetro em motricidade oral. Fonoaudiologia Brasil, 59–64. [Google Scholar]
- Suguino, R., A.L. Ramos, H.H. Terada, L.Z. Furquim, L. Maeda, and O.G. Silva Filho. 1996. Análise facial. Revista Dental Press Ortodontia e Ortopedia Maxilar 1, 1: 86–107. [Google Scholar]
- Tessitore, A. 2004. Alterações oromiofuncionais em respiradores orais. In Tratado de fonoaudiologia. Edited by L.P. Ferreira, D.M. Befi-Lopes and S.C.O. Limongi. São Paulo: Roca, pp. 261–76. [Google Scholar]
- Tsuji, D.H., and D. Chung. 2003. Causas da obstrução nasal. In Respiração oral. Edited by L.H. Krakauer, R.C. Di Francesco and I.Q. Marchesan. São José dos Campos: Pulso, pp. 91–100. [Google Scholar]
- Ward, R.E. 1989. Facial morphology as determined by anthropometry: keeping it simple. Journal of Craniofacial Genetics and Developmental Biology 9: 45–60. [Google Scholar]
- Ward, R.E., and P.L. Jamison. 1991. Measurement precision and reliability in craniofacial anthropometry: implications and suggestions for clinical application. Journal of Craniofacial Genetics and Developmental Biology 11: 156–64. [Google Scholar]
- Ward, R.E., P.L. Jamison, and L.G. Farkas. 1998. Craniofacial variability index: a simple measure of normal and abnormal variation in the head and face. American Journal of Medical Genetics 80, 3: 232–40. [Google Scholar] [CrossRef]
- Ward, R.E., P.L. Jamison, and J.E. Allanson. 2000. Quantitative approach to identifying abnormal variation in human face exemplified by a study of 278 individuals with five craniofacial syndromes. American Journal of Medical Genetics 91, 1: 8–17. [Google Scholar] [CrossRef]
- Yokota, M. 2005. Head and facial anthropometry of mixed-race US Army male soldiers for military design and sizing: a pilot study. Applied Ergonomics 36, 3: 379–83. [Google Scholar] [CrossRef] [PubMed]
 |
 |
 |
© 2009 by the author. 2009 Débora Martins Cattoni, Fernanda Dreux Miranda Fernandes, Renata Cantisani Di Francesco, Maria Do Rosário Dias De Oliveira Latorre
Share and Cite
Cattoni, D.M.; Fernandes, F.D.M.; Di Francesco, R.C.; Latorre, M.D.R.D.D.O. Quantitative Evaluation of the Orofacial Morphology: Anthropometric Measurements in Healthy and Mouth-Breathing Children. Int. J. Orofac. Myol. Myofunct. Ther. 2009, 35, 44-54. https://doi.org/10.52010/ijom.2009.35.1.4
Cattoni DM, Fernandes FDM, Di Francesco RC, Latorre MDRDDO. Quantitative Evaluation of the Orofacial Morphology: Anthropometric Measurements in Healthy and Mouth-Breathing Children. International Journal of Orofacial Myology and Myofunctional Therapy. 2009; 35(1):44-54. https://doi.org/10.52010/ijom.2009.35.1.4
Chicago/Turabian StyleCattoni, Débora Martins, Fernanda Dreux Miranda Fernandes, Renata Cantisani Di Francesco, and Maria Do Rosário Dias De Oliveira Latorre. 2009. "Quantitative Evaluation of the Orofacial Morphology: Anthropometric Measurements in Healthy and Mouth-Breathing Children" International Journal of Orofacial Myology and Myofunctional Therapy 35, no. 1: 44-54. https://doi.org/10.52010/ijom.2009.35.1.4
APA StyleCattoni, D. M., Fernandes, F. D. M., Di Francesco, R. C., & Latorre, M. D. R. D. D. O. (2009). Quantitative Evaluation of the Orofacial Morphology: Anthropometric Measurements in Healthy and Mouth-Breathing Children. International Journal of Orofacial Myology and Myofunctional Therapy, 35(1), 44-54. https://doi.org/10.52010/ijom.2009.35.1.4




