INTRODUCTION
In bilateral mastication the masticatory effort is usually distributed evenly on the teeth stabilizing the periodontal tissues and synchronizing the activity of masticatory muscles innervated by the fifth cranial nerve. Any disorder affecting the complex interaction between the masticatory muscles, the teeth, and the temporomandibular joints required to grind or pulverize food may seriously compromise mastication (
Pereira et al, 2006).
Peripheral facial paralysis (PFP) usually affects facial nerve function in part or in whole on one side of the face (
Alonso-Navarro et al, 2005). Two stages may be recognized: one flaccid, marked by the absence of nerve impulses; the other with incomplete recovery and anomalous reinnervation that characterizes its sequelae.
In the flaccid stage, due to muscle incompetence on the paralyzed side of the face, patients display sagging facial muscles and loss of facial expression, while wrinkles tend to smoothen out (
Bento et al, 1996). Once movement on the paralyzed side has been compromised, the patient cannot protrude, retract or close the lips properly, nor fully inflate the cheeks (
Goffi-Gomez, 1999).
Clinically during orofacial evaluation, few patients with PFP can chew on the paralyzed side because the affected buccinator muscle no longer guides and retains the food between the teeth. In addition, the sagging of the ipsilateral lip commissure tends to compromise oral competence. In spite of these associations, literature on mastication difficulties in PFP patients is scarce, perhaps because the facial nerve has been considered to be responsible primarily for facial expression.
When the flaccid stage of PFP exceeds six months, patients are at risk for chronic muscle and facial asymmetry (
Sinsel et al, 2003). Subjective orofacial evaluation may not reveal real cause and can lead to misdiagnosis. However, technological advances(such as surface electromyography) have provided objective methods for both diagnostic purposes and to evaluate myofunctional therapy (
Hanawa et al, 2008).
The objective of the present study was to evaluate the impact of long-term flaccid peripheral facial nerve paralysis on mastication, especially with regard to:
clinical mastication preference
clinical masseter activity during food bolus formation
electromyographic activity of the masseters.
METHODS
Participants Subjects were recruited among patients referred for myofunctional treatment by the Facial Nerve Paralysis Team at the Division of Clinical Otorhinolaryngology, Hospital of the University of São Paulo Medical School(HCFM/USP).
Inclusion criteria:
Age ≥ 16 years
Flaccid unilateral peripheral facial nerve
paralysis for ≥ 6 months
Permanent natural dentition, whether complete or not
Presence of premolars and/or molars in all half-arches
PFP of idiopathic, iatrogenic or traumatic origin (e.g. from gunshot or cranial fracture)
Exclusion criteria:
Previous PFP
Congenital PFP
Congenital facial asymmetry
Fewer than 8 teeth in each arch
History of speech therapy associated with orofacial motricity/neuromotor disorder
Changes/complaints involving the temporomandibular joints
Visible skin disorders, or beard interfering with electrodes contact
Twenty-seven patients were selected during a period from July 2006 and December 2007. This group included 16 female with ages ranging from 16 to 61 and 11 male with ages ranging from 19 to 69
Procedure
The evaluation was carried out in two steps: 1) anamnesis and clinical evaluation of mastication, and 2) electromyographic testing. The anamnesis included open questions about the time of onset and cause of PFP, mastication preference prior to PFP, pain during mastication, retention of food residues in the oral cavity and mastication difficulties associated with PFP. Subsequently, patients were examined clinically for bite marks during the clench movement, dental condition, and orofacial muscle function according to a standard protocol in orofacial myology. This included:
Orbicularis oris: lip protrusion and closure
Buccinators: alternated cheek inflation
Masseters: clenching during maximum intercuspidation
Disposable silicone gloves, wooden spatulas, and split loaves of French bread were used in the clinical habitual mastication study, when checking for (
Marchesan, 2005):
Lateral preference in mastication
Pain
Presence of food residues after swallowing
Use of hand to support cheek during mastication
The electromyographic evaluation of the surface bundles of the right and left masseter was performed with disposable bipolar surface electrodes(Ag-AgCI double Hal) leading to a Miotec® device with Miograph 400 software. The right sternocleidomastoid muscle was used as a reference recording site by placement of a disposable unipolar surface electrode (200 Medi Trace Foam°). After the skin had been prepared by rubbing with 70° alcohol to improve action potential conduction and control system impedance, electrodes filled with conductive gel were attached longitudinally along the muscle bundles to avoid interference from adjacent muscles on the anterior right side of the neck and on the thickest part of the masseters near the gonial angle of the jaw (
Rahal and Pierotti, 2004).
The electromyographic tests consisted of 1) clenching during maximum intercuspidation, and 2) habitual mastication (movements repeated during 15 seconds). In the former test, patients were asked to clench their teeth with maximum effort for three seconds and then release and relax. Three repetitions were performed within 15 seconds. In the habitual mastication test, patients were asked to chew comfortably on three seedless raisins.
The following evaluation criteria were used:
Clinical observation:
Angle’s bite classification system. Class I = normal; Class II and III = abnormal.
Dental condition: absence of caries at visual inspection = good dental condition; presence of caries at visual inspection = poor dental condition.
Evaluation of orofacial muscle function:
Orbicularis oris
Protrusion was considered symmetrical when centralized; and asymmetrical when diverted. Diversion towards the healthy side (H) occurred due to increased activity on that side.
Lip closure with inflated cheeks was considered symmetrical when maintained for 10 seconds with no air escape, and asymmetrical when air was observed to escape. The side of reduced strength and air escape was recorded.
Buccinators
Masseters
Evaluation of mastication:
Lateral preference: “yes” was checked if the patient chewed on only one side during habitual mastication. The preferred side was registered (H for “healthy”; P for “paralyzed”). “No” was checked if mastication was bilateral or alternated.
Pain: the presence (“yes”) or absence (“no”) of pain and the side of occurrence (H or P) were registered as reported by the patient.
Residues: “Yes” was checked if residues were present in the oral cavity after swallowing. “No” was checked if not. The side (H or P) on which food residue was observed was also registered.
Use of hand to support cheek during mastication: “Yes” was checked if the patient used the hand to support the cheek during mastication. “No” was checked if not. The supported side (H or P) was also registered.
Electromyographic tests:
The electromyographic evaluation of the surface bundles of the right and left masseter was performed with disposable bipolar surface electrodes(Ag-AgCI double Hal) leading to a Miotec® device with Miograph 400 software. The right sternocleidomastoid muscle was used as a reference recording site by placement of a disposable unipolar surface electrode (200 Medi Trace Foam°). After the skin had been prepared by rubbing with 70° alcohol to improve action potential conduction and control system male and thirty female, with ages ranging from 25 to 45. Control data consisted of retrospective EMG masticatory assessment that was obtained from another study (
Rodrigues and Ferreira, 2004).
The EMG procedure was the same for both groups. EMG equipment used in the control group was K6 I, Myotronics with disposable bipolar electrodes (Ag-AgCI double Hal) over the right and left masseter and a disposable unipolar reference electrode (200 Medi Trace Foam°) over the right sternocleidomastoid muscle.
Statistical analysis
The masseter activity index (MAI) between the two sides was calculated from the electromyographic data. In PFP patients and controls with confirmed lateral preference in mastication, MAI was obtained by dividing the electromyographic activity on the non-preferred side by the electromyographic activity on the preferred side. In patients with no lateral preference, MAI was calculated by dividing the electromyographic activity on the paralyzed side by the electromyographic activity on the unaffected side (PFP patients) or by dividing activity on the right side by activity on the left side (controls). The MAI values were then compared for PFP patients and controls according to the presence of lateral preference in mastication.
The comparison between the experimental group and the control group data was possible, despite the use of different equipment because we considered the MAI (masseter activity index) rather than the absolute RMS values.
Normal distribution was determined with the Kolmogorov-Smirnov test. Categorical variables were described in terms of frequency while qualitative variables were expressed in mean values and standard deviation. Odds ratios were calculated for associations between categorical variables. When applicable, mean values were analyzed by Student’s t test and paired t test. All statistical tests were two-tailed, and the level of significance was set at p<0.05.
RESULTS
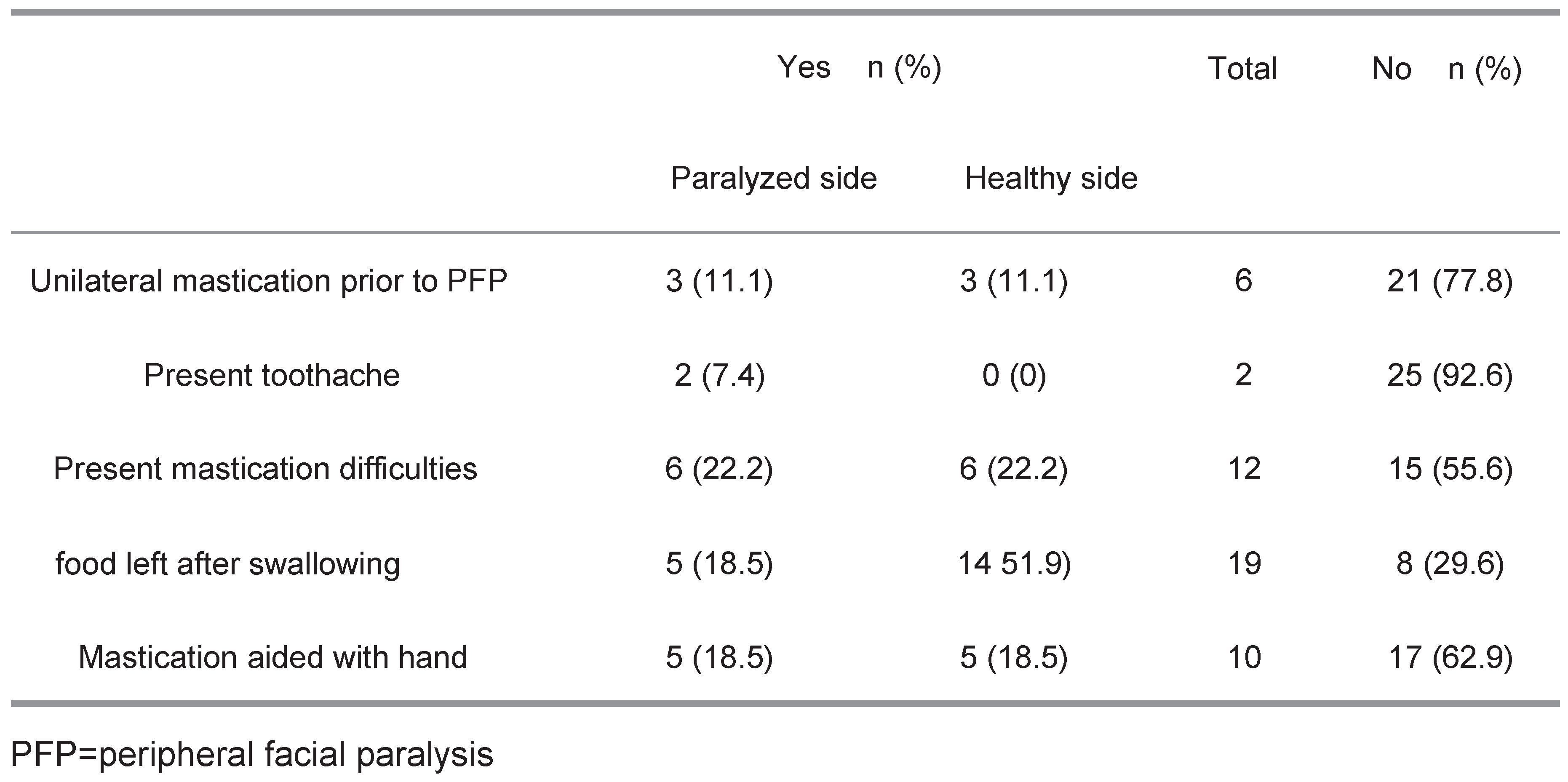
According to the anamnesis (
Table 1), most patients (77.8%) reported chewing on both sides before onset of PFP. More than half the subjects denied having mastication difficulties or aiding mastication with the hand (55.6% and 62.9%, respectively), at least 6 months after the onset of the PFP.
Table 2 shows that of 19 (70%) patients with Class I bite, only 12 (44%) reported preferring to chew on the healthy side. All patients with Class II bite preferred the healthy side. Although all patients (100%) had asymmetrical lips upon protrusion (
Table 3), as many as 40.7% presented with adequate lip closure.
As shown in
Table 4, 100% of the patients had asymmetrical buccinators with greater activity on the healthy (H) side, whereas 25.9% presented asymmetrical masseters (22.2% with greater activity on the healthy side).
The clinical study revealed that 85.2% of the subjects had a lateral preference in mastication (H = 77.8%). Pain and hand-aided mastication were infrequently observed (7.7% and 14.8%, respectively). Residues were seen in 63% of cases (P = 100%) (
Table 5).
Table 6 shows the distribution of patients according to clinically evaluated lip condition and lateral preference in mastication during the habitual mastication test.
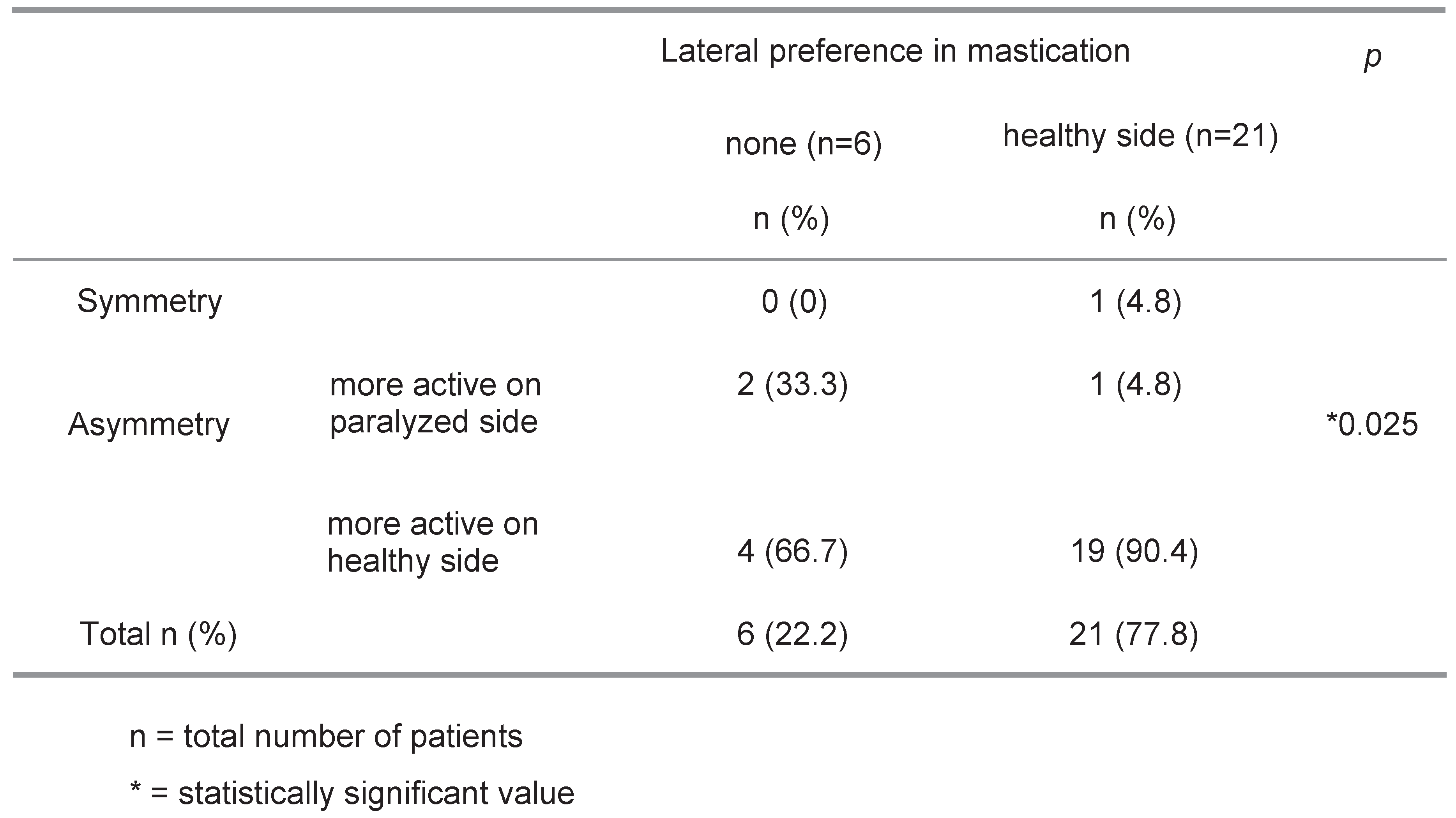
Patients with and without clinically evaluated lateral preference in mastication differed significantly during habitual mastication with regard to the clinical condition of the buccinators (
p=0.025) (
Table 7)
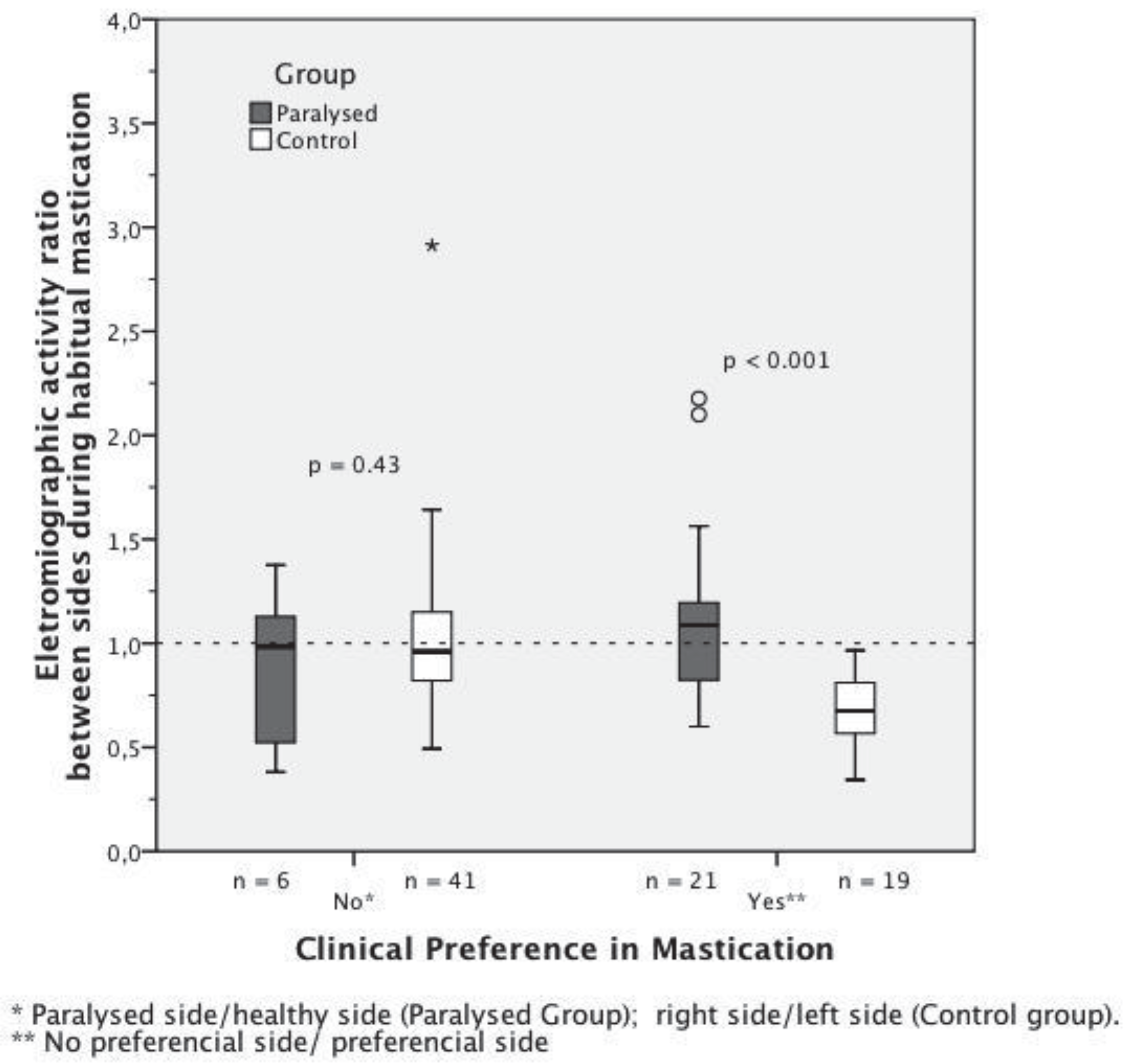
Lateral preference in mastication occurred more frequently among PFP patients than among controls (
p<0.001), as shown in
Figure 1. The odds ratio of a subject with lateral preference in mastication belonging to the group of PFP patients was 7.6 times greater than that of belonging to the group of controls (CI: 95%; range: 2.6–21.6).
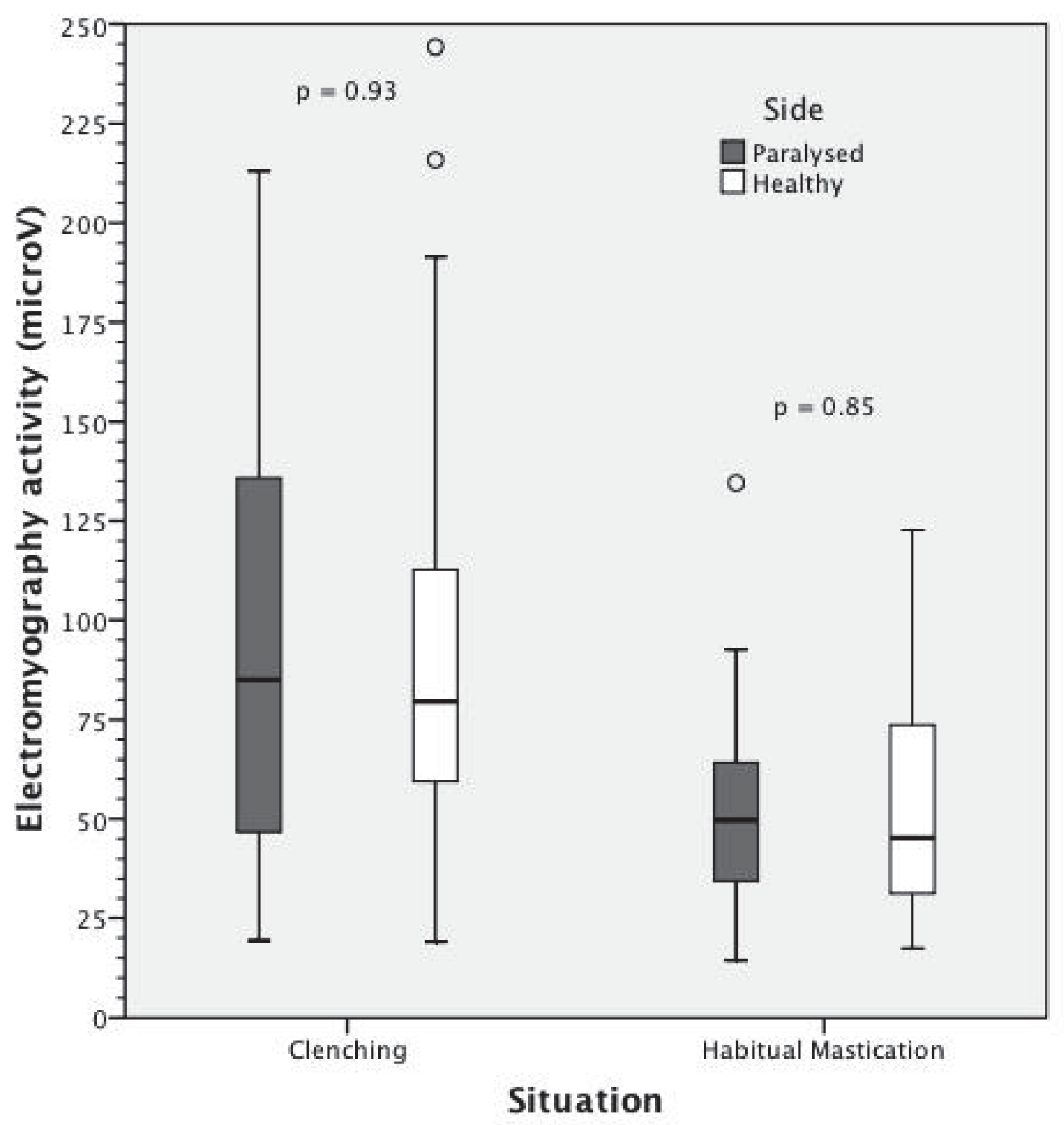
Comparison between facial paralysis group (PFP) and control group regarding the MAI (masseter activity index) during clenching and habitual mastication, are shown in
Figure 2 and
Figure 3 for those patients who did not show any preference and in those who showed lateral preference during mastication.
Table 1.
Distribution of 27 patients with PFP exceeding 6 months according to time of onset.
Table 1.
Distribution of 27 patients with PFP exceeding 6 months according to time of onset.
Table 2.
Distribution of 27 patients with PFP for 6 months or longer according to type of occlusion and lateral mastication preference.
Table 2.
Distribution of 27 patients with PFP for 6 months or longer according to type of occlusion and lateral mastication preference.
Table 3.
Distribution of 27 patients with PFP for 6 months or longer according to myofunctional condition of the orbicularis oris.
Table 3.
Distribution of 27 patients with PFP for 6 months or longer according to myofunctional condition of the orbicularis oris.
Table 4.
Distribution of 27 patients with PFP for 6 months or longer according to clinical condition of buccinator and masseter bulk.
Table 4.
Distribution of 27 patients with PFP for 6 months or longer according to clinical condition of buccinator and masseter bulk.
Table 5.
Distribution of 27 patients with PFP for 6 months or longer according mastication evaluation.
Table 5.
Distribution of 27 patients with PFP for 6 months or longer according mastication evaluation.
Table 6.
Distribution of 27 patients with PFP for 6 months or longer according to clinically evaluated lip condition and lateral preference in mastication during the habitual mastication test.
Table 6.
Distribution of 27 patients with PFP for 6 months or longer according to clinically evaluated lip condition and lateral preference in mastication during the habitual mastication test.
Table 7.
Distribution of 27 patients with PFP for 6 months or longer according to the clinical condition of the buccinators and clinically evaluated lateral preference in mastication during habitual mastication.
Table 7.
Distribution of 27 patients with PFP for 6 months or longer according to the clinical condition of the buccinators and clinically evaluated lateral preference in mastication during habitual mastication.
Figure 1.
Lateral preference in mastication occurred more frequently among PFP patients than among controls (p<0.001). The odds ratio of a subject with lateral preference in mastication belonging to the group of PFP patients was 7.6 times greater than that of belonging to the group of controls (CI: 95%; range: 2.6–21.6).
Figure 1.
Lateral preference in mastication occurred more frequently among PFP patients than among controls (p<0.001). The odds ratio of a subject with lateral preference in mastication belonging to the group of PFP patients was 7.6 times greater than that of belonging to the group of controls (CI: 95%; range: 2.6–21.6).
Figure 2.
Comparison between facial paralysis group (PFP) and control group regarding the MAI (masseter activity index) during clenching in those patients who did not show any preference and in those who showed lateral preference during mastication.
Figure 2.
Comparison between facial paralysis group (PFP) and control group regarding the MAI (masseter activity index) during clenching in those patients who did not show any preference and in those who showed lateral preference during mastication.
Figure 3.
Comparison between facial paralysis group (PFP) and control group regarding the MAI (masseter activity index) during habitual mastication in those patients who did not show any preference and in those who showed lateral preference during mastication.
Figure 3.
Comparison between facial paralysis group (PFP) and control group regarding the MAI (masseter activity index) during habitual mastication in those patients who did not show any preference and in those who showed lateral preference during mastication.
DISCUSSION
Patients with flaccid PFP are often referred to a speech, physical, or orofacial myofunctional therapist in order to stimulate orofacial muscle function. In fact, studies on treatment of PFP have described the difficulties of PFP patients in performing daily actions such as eating, chewing, speaking, and socializing, along with some of the emotional problems that may ensue from this condition (
Novak, 2004).
In the clinical orofacial myology practice, we have found that most PFP patients have mastication difficulties on the affected side due to buccinator dysfunction compromising the maintenance of the food between the teeth and causing residues to remain after swallowing. Likewise, patients commonly present lip incompetence caused the flaccidity of the lip commissure on the affected side (Goffi-Gomez et al., 2004). In spite of the medical and social implications of these difficulties, studies on mastication in PFP patients are scarce, perhaps because the facial nerve has conventionally been considered to be responsible primarily for facial expression, while the masticatory muscles are innervated by the fifth cranial nerve.
Masseter function was evaluated electromyographically by
Rahal and Goffi-Gomez (2007) during mastication in six subjects with flaccid unilateral PFP during a period of six months. They found no significant difference in electromyographic activity between the masseters on the two sides of the face. Due to the small sample size, the study did not compare electromyographic findings with clinical mastication outcomes.
The present study included only patients with flaccid PFP for 6 months or longer. This criterion was adopted because the orofacial muscles are known to require 6 or more months to adjust to anatomical and functional changes (Marchesan & Sanseverino, 2004).
The findings here show that 100% of the subjects (27/27) presented asymmetrical buccinator function with greater muscle action on the unaffected side. Likewise, in all patients (27/27) the orbicularis oris was more competent on the healthy side upon lip protrusion while 60% (16/27) displayed insufficient lip closure on the paralyzed side. Tomiyama et al. (2003) found that the duration and amplitude of the facial muscle movements depend on mastication cycles and on the contact between the upper and lower lip. This would explain why PFP patients are unable to chew consistently when the orbicularis oris is compromised.
On the other hand, 74% (20/27) of subjects in this study presented symmetrical masseters. Only one patient (3%) displayed larger muscle bulk on the affected side. Differences between buccinator and masseter function were statistically significant. The current findings suggest that in flaccid PFP patients lateral preference in mastication may be directly associated with loss of buccinator function, rather than masseter thickness. Not even was related to its increase in thickness. This appears to contradict the electromyographic and ultrasonographic findings published by
Georgiaki et al. (
2007) on lateral preference in mastication in women showing a direct relationship between masseter thickness and myoelectrical activity during clenching. In addition, according to those authors, lateral preference in mastication was directly associated with masseter bulk.
Moreover, even though the dental condition and changes in occlusion are known to be important factors directly related to adequate mastication and lateral preference (
Bianchini, 2005), only 22% (6/27) of this study’s patients presented with a poor dental condition (observed on both sides), and none of these manifested any lateral preference.
In this study, 70% (19/27) of the subjects presented normal Class I occlusion while 30% (8/27) were rated as Class II. None were assigned to Class III. It should be remembered that dental occlusion influences masseter strength.
Of 19 patients (70%) rated as Class I, 12 (44%) preferred to chew on the healthy side, 1 (4%) preferred the paralyzed side and 6 (22%) presented no lateral preference. All Class II patients in this study (n=8; 30%) preferred to masticate on the unaffected side. Nevertheless, considering that Class II dentitions represent antero-posterior deviations, there should be no influence in the masticatory preference.
Prior to onset of PFP and regardless of dental abnormalities, 22% (6/27) reported chewing on one side only (3 on the healthy side and; 3 on the paralyzed side). Results here lend support to the findings of
Nissan et al. (
2004) who demonstrated a relation between lateral preference and brain hemisphere dominance. Likewise, these authors found lateral preference to be unrelated to tooth loss, implants, or full dentition.
The anamnesis and the clinical evaluation revealed that subjects with PFP tend to masticate on the unaffected side, especially due to the inability of the buccinator to eliminate food residue (70.4%). Twelve subjects (44%) reported having chewing difficulties on the paralyzed side, and upon clinical evaluation 77.8% (21/27) were observed to prefer masticating on the healthy side. Food residue was found after swallowing in 63% (17/27), invariably on the affected side. Being previously warned to the use of the hands as a helpful tool during mastication, 37% (10/27) claimed mastication improved when the hand was pressed against the cheek. We, however, observed this practice in only 14.8% (4/27) of the subjects. Even fewer (7.4%; n=2) reported pain in the masseter on the affected side during the clinical evaluation.
When submitting 30 healthy subjects with clinically normal occlusion and temporomandibular joints to electro-myographical testing of the masseters during clenching and habitual mastication,
Rahal and Goffi-Gomez (
2009) observed significant average differences between the right and left side (clenching: 24%; habitual mastication: 27%). In the present study, the corresponding figures were much lower (2% and 3%, respectively).
EMG activity during clenching and habitual mastication in patients with PFP and in the control group of both sexes was compared. We divided them into two subgroups according to their masticatory lateral preference. Among those subjects who did not show any masticatory preference there was no statistical difference of the masseter activity index (MAI) between the control and the PFP group in both tests. Among those subjects who showed lateral masticatory preference there was a statistical significant difference between the two groups in both tests. This finding shows that masticatory preference is accompanied by higher masseter activity. However, in the PFP group, this was not observed. This may be due to a stronger action of the buccinator muscle. Oncins et al (2006) performed electromyographic and electrognathographic tests of the temporal muscles and masseters of 26 healthy volunteers during mandibular rest and habitual mastication of raisins. The study revealed that 65.4% preferred masticating on one side, even in the absence of anatomical changes. On the other hand, in a study involving 30 healthy subjects with full dentition and clinically normal occlusion and temporomandibular joints, similar electromyographic patterns for the masseters on both sides of the face were found (
Bérzin, 2004). Interestingly, this is in agreement with the findings in this current study, even though subjects were affected with PFP.
Patients with and without lateral preference in mastication did not differ significantly with regard to lip condition. It may thus be concluded that the orbicularis oris was not a major determinant in lateral preference. However, the same two groups of patients differed significantly with regard to buccinator activity, which was invariably greater on the unaffected side in patients preferring to masticate on this side.
Pignataro, et.al. (2004) compared the clinical findings of mastication with carrots and parafilm to electromyographic findings of the masseters in 29 healthy subjects with full dentition and clinically normal temporomandibular joints. Mastication preference was assumed to differ between the left and right masseter by 20%. With an 88.8% agreement between clinical and electromyographic findings, the authors concluded that 72.4% of the subjects had a lateral preference in mastication. The current study indicates that even though unaffected and affected masseter thickness and electromyographic activity were similar, patients still preferred to masticate on the unaffected side. Thus, neither dental condition, nor occlusion, pain in the temporomandibular joints or lip incompetence could explain the mastication preference of patients with PFP. It follows that buccinator dysfunction, compromising the maintenance of the food between the teeth and causing residues to remain after swallowing, is the major factor determining lateral preference in mastication in patients with PFP.