Orofacial Myofunctional Deficits in Elderly Individuals
Abstract
:NTRODUCTION
REVIEW
OMD in the elderly
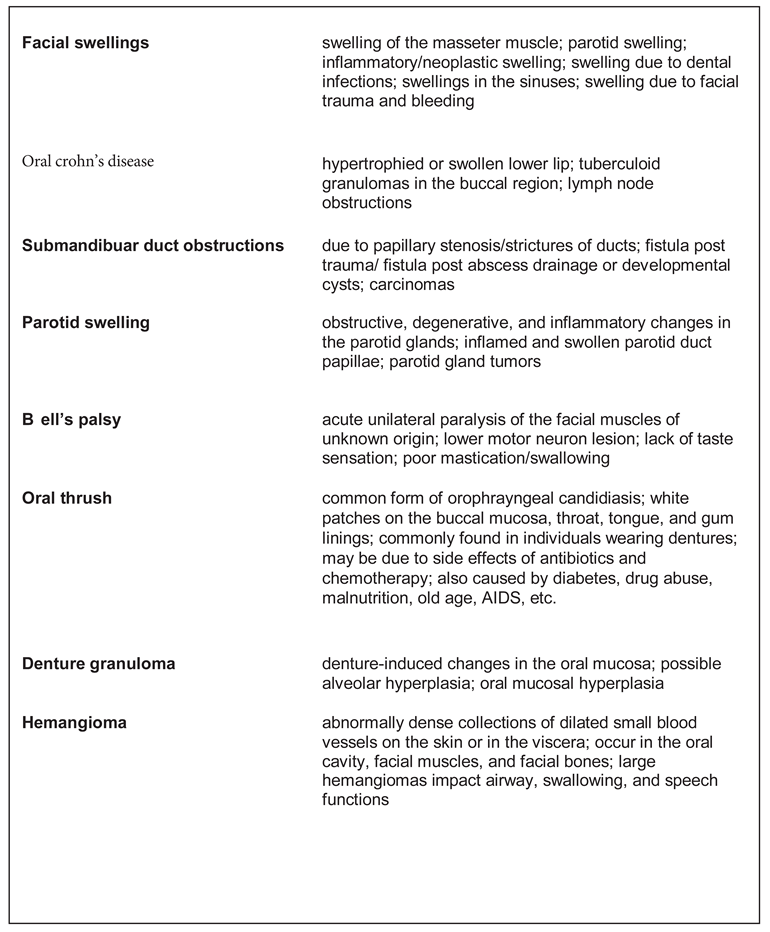
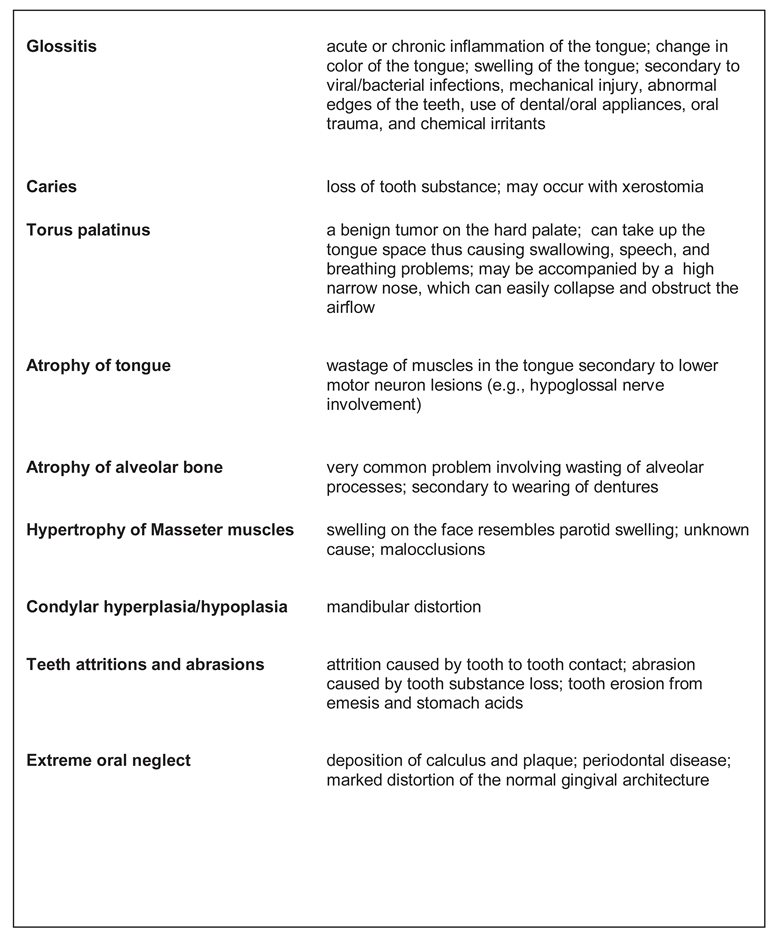
Orofacial Myofunctional Dysfunctions
Tongue Thrusting and OMD
Myofascial Pain and OMD
Speech Problems and OMD
Down Syndrome in Adults and OMD
Bruxism and OMD
Sleep apnea and OMD
Aging of the face
Psychiatric Disorders and OMD
Craniomandibular disorders
- crowding of upper incisors
- labial/lingual position of one canine
- labial/lingual position of two canines
- labial/lingual position of three canines
- labial/lingual position of all canines
- posterior crowding
- spacing
- overjet
- retroclined maxillary incisors
- edge-to-edge bite
- anterior crossbite
- negative overjet
- distocclusion
- mesiocclusion
- mixed occlusion
Drugs and OMD
CONCLUSIONS
References
- Adams, S. G. 1997. Edited by R. McNeil M. Hypokinetic dysarthria in Parkinson’s disease. In Clinical management of sensory motor speech disorders. Thematic Medical Publishers: pp. 261–285. [Google Scholar]
- Akeel, R., M. Nilner, and K. Nilner. 1992. Masticatory efficiency in individuals with natural dentition. Swedish Dental Journal 16, 5: 191–198. [Google Scholar] [PubMed]
- Allison, P. J., M. A. Peyron, M. Faye, and M. Hennequin. 2004. Video evaluation for mastication validation in persons with Down’s Syndrome. Dysphagia 19: 95–99. [Google Scholar] [CrossRef]
- American Speech and Hearing Association. 1989. Report: Ad Hoc Committee on labial-lingual posturing function. Asha 31, 11: 92–94. [Google Scholar]
- American Speech and Hearing Association. 1993. Orofacial myofunctional disorders: Knowledge and skills. Asha 35, 21–23. [Google Scholar]
- American Speech-Language-Hearing Association. 1991. The role of the speech-language pathologist in the management of oral myofunctional disorders. Asha 33 Suppl. 5, 7. [Google Scholar]
- Baum, B. J., J. A. Ship, and A. Wu. 1992. Salivary gland function and aging: A model for studying the interaction of aging and systemic disease. Critical Review of Oral Biological Medicine 4: 53–64. [Google Scholar] [CrossRef] [PubMed]
- Bergdahl, M. 2000. Salivary flow and oral complaints in adult dental patients. Community Dental Oral Epidemiology 28: 59–66. [Google Scholar] [CrossRef]
- Bigenzahn, W., L. Fischman, and U. Mayrhofer-Krammel. 1992. Myofunctional Therapy in Patients with Orofacial Dysfunctions Affecting Speech. Folia Phoniatrica 44, 5: 238–244. [Google Scholar] [CrossRef]
- Bodin, I., E. L. Jaghagen, and A. Isberg. 2004. Intraoral Sensation Before and After Radiotherapy and Surgery for Oral and Pharyngeal Cancer. Head & Neck, 923–929. [Google Scholar]
- Borea, G., M. Magi, R. Mingarelli, and C. Zamboni. 1990. The Oral Cavity in Down Syndrome. Journal of Pedodontics 14: 139–140. [Google Scholar]
- Catovic, A., V. Jerolimov, and A. Catic. 2000. Tooth Loss and the Condition of the Prosthodontic Appliances in a Group of Elderly Home Residents. Journal of Oral Rehabilitation 27, 3: 199–204. [Google Scholar] [CrossRef] [PubMed]
- Chambers, M. S., A. S. Garden, M. S. Kies, and J.W. Martin. 2004. Radiation Induced Xerostomia in Patients with Head and Neck Cancer: Pathogenesis, impact on quality of life, and management. Head & Neck, 796–806. [Google Scholar]
- Council on Clinical Affairs. 2004. Policy on Oral habits. Reference Manual 2003–2004.
- deSwart, B. J. M., J. G. Verheij, and C. H. Beurskens. 2003. Problems with eating and drinking in patients with unilateral peripheral facial paralysis. Dysphagia 18: 267–273. [Google Scholar] [CrossRef]
- Duffy, J. R. 1995. Motor speech disorders: Substrates, differential diagnosis, and management. Mosby Year Book. [Google Scholar]
- Freed, D. B. 2000. Motor speech disorders. Singular Thompson Learning. [Google Scholar]
- Gesch, D., O. Bernhardt, D. Alte, T. Kocher, U. John, and E. Hensel. 2004. Malocclusions and clinical signs or subjective symptoms of temporomandibular Disorders (TMD) in Adults. Journal of Orofacial Orthopedics 65: 88–103. [Google Scholar] [CrossRef] [PubMed]
- Hanson, M. L. 1988. Orofacial myofunctional disorder. Guidelines for assessment and treatment. International Journal of Orofacial Myology 14: 27–32. [Google Scholar] [CrossRef]
- Hennequin, M., D. Faulks, J. L. Veyrune, and P. Bourdiol. 1999. Significance of oral health in persons with Down Syndrome. A literature review. Developmental Medicine and Child Neurology 41: 275–283. [Google Scholar] [CrossRef]
- Horowitz, M., M. Horowitz, M. Ochs, R. Carrau, and A. Kassam. 2004. Trigeminal neuralgia and glossopharyngeal neuralgia: Two Orofacial pain syndromes encountered by dentists. Journal of American Dental Association 135: 1427–1433. [Google Scholar] [CrossRef]
- Korbmacher, H., and Kahl-Neike. 2001. Optimizing interdisciplinary cooperation for patients with orofacial dysfunctions. Journal of Orofacial Orthopedics 62: 246–250. [Google Scholar] [CrossRef]
- Kuna, S. T., and J. S. Smickley. 1997. Superior pharyngeal constrictor activation in obstructive sleep apnea. American Journal of Respiratory Critic Care and Medicine 156: 874–880. [Google Scholar] [CrossRef]
- Kuten, A., H. Ben-Aryeh, and I. Berdicevsky. 1986. Oral side effects of head and neck irradiation: Correlation between clinical manifestations and laboratory data. International Journal of Radiation, Oncology, Biology and Physics 12: 401–405. [Google Scholar] [CrossRef]
- Langmore, S. E., and M. E. Lehman. 1994. Physiologic deficits in orofacial system underlying dysarthria in amyotrophic lateral sclerosis. Journal of Speech and Hearing Research 37, 1: 28–37. [Google Scholar] [CrossRef] [PubMed]
- Limeback, H. 1998. Implications of oral infections on systematic diseases in the institutionalized elderly with a special focus on pneumonia. Annals of Periodontology 3: 262–275. [Google Scholar] [CrossRef] [PubMed]
- McComas, A. J. 1998. Orofacial muscles: Internal structure, function, and ageing. The Gerontology Association 15, 1: 3–14. [Google Scholar]
- Millwood, J., and J. Fiske. 2001. Lip biting in patients with profound neurodisability. Dental Update 28: 105–108. [Google Scholar] [CrossRef]
- Narhi, T. O. 1994. Prevalence of subjective feelings of dry mouth in the elderly. Journal Dental Research 73: 20–25. [Google Scholar] [CrossRef]
- Narhi, T. O., J. H. Meurman, A. Ainamo, J. M. Nevalainen, K. G. Schmidt-Kaunisaho, P. Siukosaari, J. Valvanne, T. Erkinjuntti, R. Tilvis, and E. Makila. 1992. Association between salivary flow rate and the use of systemic medication among 76-, 81-, and 86–year-old inhabitants in Helsinki, Finland. Journal of Dental Research 71, 12: 1875–1880. [Google Scholar] [CrossRef]
- Newton, J. P., R. Yemm, R. W. Abel, and S. Menhinick. 1993. Changes in human jaw muscles with age and dental state. Gerodontology 10, 1: 16–22. [Google Scholar] [CrossRef]
- Riley, J. L., G. H. Gilbert, and M. W. Heft. 1999. Health care utilization by older adults in response to painful orofacial symptoms. Pain 81: 67–75. [Google Scholar] [CrossRef]
- Smith, R. G., and A. P. Burtner. 1994. Oral side-effects of the most frequently prescribed drugs. Special Care Dentistry 14: 96–102. [Google Scholar] [CrossRef]
- Sreebny, L. M., and S. S. Swartz. 1997. A reference guide to drugs and dry mouth. Gerodontology 14, 1: 33–48. [Google Scholar] [CrossRef]
- Tyldesley, W. R. 1991. Orofacial diseases, 2nd ed. Wolfe Publishing Ltd. [Google Scholar]
- Walls, A. W. G., and J. G. Steele. 2004. The relationship between oral health and nutrition in older people. Mechanisms of Aging and Development 125: 853–857. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. 2001. International classification of functioning, disability, and health. World Health Organization. [Google Scholar]
 |
 |
 |
 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2008 by the authors. 2008 Jayanti Ray
Share and Cite
Ray, J. Orofacial Myofunctional Deficits in Elderly Individuals. Int. J. Orofac. Myol. Myofunct. Ther. 2006, 32, 22-31. https://doi.org/10.52010/ijom.2006.32.1.2
Ray J. Orofacial Myofunctional Deficits in Elderly Individuals. International Journal of Orofacial Myology and Myofunctional Therapy. 2006; 32(1):22-31. https://doi.org/10.52010/ijom.2006.32.1.2
Chicago/Turabian StyleRay, Jayanti. 2006. "Orofacial Myofunctional Deficits in Elderly Individuals" International Journal of Orofacial Myology and Myofunctional Therapy 32, no. 1: 22-31. https://doi.org/10.52010/ijom.2006.32.1.2
APA StyleRay, J. (2006). Orofacial Myofunctional Deficits in Elderly Individuals. International Journal of Orofacial Myology and Myofunctional Therapy, 32(1), 22-31. https://doi.org/10.52010/ijom.2006.32.1.2




