Abstract
A number of developmental changes occur in eating patterns from infancy through childhood. Initially a primitive reflexive process, deglutition develops into a complex, integrated voluntary/reflexive process. The movements of the tongue, lips and mandible are easily observed to undergo a transformation from synergistic, undifferentiated movements in the infant, to differentiated and refined movements required for biting, chewing, bolus formation and propulsion in the toddler and young child. This transformation is also crucial for the development of higher levels of articulatory precision and coordination required for verbal communication. This developmental process does not always occur in individuals exhibiting orofacial myofunctional disorders. This article will review current research in this area as well as describe how to evaluate for normal tongue, lip and jaw differentiation, and present exercises to develop these skills, which are necessary for successful outcomes in orofacial myofunctional treatment.
INTRODUCTION
It is generally accepted in the motor development literature, that movement patterns develop from gross, generalized reflexive patterns towards movements requiring finer, isolated motor control (Marshalla, 1992; Ayres, 1979). For example, the young infant first uses the whole hand to grasp objects and then eventually learns isolated finger control and a refined pincer grasp. In addition, the establishment of a stable base from which to move is a critical element of refined motor skill and movement, such as when an infant can weight-bear and stabilize the shoulder girdle in a prone position, he then can use one arm to reach for distant objects. These very same principles of differentiation and stability underlie the development of the orofacial mechanism for swallowing and deglutition as well as for verbal speech skills.
The orofacial complex first functions as a unit within the whole body. Jaw and lip movements occur simultaneously with head bobbing to produce bilabial sequences in babbling. The rooting reflex involves mouth opening combined with head movement toward the stimulus. Differentiation occurs developmentally: the head from the body; the jaw from the head; the lips from the jaw; the tongue from the jaw; the tongue tip from the tongue body; the tongue back from the tongue body; and the tongue’s lateral margins from the tongue body. Independent use of each part is necessary for higher level, refined movements required for mature speech and mature patterns of deglutition. Correct positioning and movement of the tongue and lips are based upon stability of the jaw (referred to as external stability) and the tongue’s ability to remain in a neutral position in relation to the jaw (referred to as internal stability) (Marshalla, 1992; Ayres, 1979).
There has been much investigation of these principles in relation to the development of normal speech development and normal feeding and orofacial functions, but relatively little in relation to orofacial myofunctional disorders. This article will explore the concepts of differentiation and stability in relation to normal swallowing development and their influence in the treatment of orofacial myofunctional disorders.
LITERATURE REVIEW: NORMAL SWALLOWING DEVELOPMENT
Suckling
Nutritive sucking is well established in the infant at birth. It is generally accepted that nutritive sucking is primarily a reflex stimulated automatically through the tactile receptors in the face and mouth (Oetter, 1988). Fletcher (1970) describes the sucking pattern of the newborn as involving a complete peripheral seal around the nipple with the tongue and lower lip forming the anterior seal, the fat pads in the cheeks supporting the lateral seal, and the tensor veli palatini muscle in the soft palate and tongue root forming the posterior seal. The tongue, lip, and mandible then are raised together as one unit and the tongue tip simultaneously thrusts forward against the base of the nipple. This is followed by a rippling/or stripping action along the dorsum of the tongue, which expresses the milk from the nipple. Two biomechanical models of nutritive sucking have been described by Oetter, Richter, and Frick (1988), occupational therapists, in their text, MORE: Integrating the Mouth with Sensory and Postural Functions. The first model follows the compression description of Fletcher’s where fluid is squeezed from the bottle or breast (See Figure 1). The second model describes how negative pressure creates a vacuum in the oral cavity. This requires a seal created around the nipple by the lips, jaw, and tongue and an increase in the space in the oral cavity by dropping the posterior portion of the tongue and jaw (See Figure 2).
Dr. Rika Ayano, and colleagues described this suckling pattern in detail with the help of ultrasound imaging at the IAOM Convention in San Diego in 1998. They concluded that in the “motions of suckling feeding, the tongue and jaw move together rather than independently.” In their ultrasound observations, they found that the tongue tip was almost fixed with the tongue and jaw squeezing the nipple against the alveolar ridge.
In 1996, Tamura and associates examined the coordination of tongue movements and perioral muscle activity during nutritive sucking in infants. They found significant correlations between jaw motion, tongue movement and suckling pressure. They described the tongue and jaw elevating together in the process. Their findings suggested that the opening and closing of the jaw assisted dynamic tongue movements involved in sucking.
Suck-Swallow: Liquids and Solids
Initially, stability in the oral region is achieved via the jaw and cheeks, which form boundaries for the tongue and help stabilize the nipple. Mandibular movements are rudimentary – primarily anterior/posterior, and inferior/superior. As early as four months, however, the infant gains more stability in the jaw, neck and shoulders and the primitive suckling pattern begins to modify. This allows the infant more voluntary control of oral motor, and head and neck action. With the introduction of solid foods, differentiation of postural and transport motions begins. The changes involved include the development of a more distal or forward locus of control involving the lips and cheeks, and anterior 1/3 of the tongue. The tongue tip begins to elevate, the sides of the tongue curl up for better bolus control, and the lips can form a pucker. The lips assist in bringing food into the mouth, the lateral portions of the tongue begin to elevate to form a central groove. Ayano (1998) and colleagues found these distinct movements developing as early as 8-10 months of age. Initial attempts by the infant at handling non-liquid foods are similar in form to the suckle pattern: The mandible elevates and the tongue thrusts forward in contact with the lower lip and the ability to swallow with the lips closed begins to develop. Bosma (1963) called attention to the importance of labial closure as a developmental landmark in mature swallowing development. Ayano (1998) and colleagues studied labial closing pressures and found that they increased steadily from 5 months until 5 years of age.
Fletcher (1970) hypothesizes that non-liquid foods bring a new set of sensory inputs to the mouth, which trigger motor reorganization and new motor skills. According to Oetter (1988) and colleagues, the tongue achieves strength and gradation of movement from the back 1/3 progressively toward the front. As the tongue tip achieves more mobility, interest in exploring new sensory experiences, such as taste and texture emerges.
Ayano (1998) and colleagues describe the beginning of differentiated tongue tip movement at this early stage, where the tip of the tongue elevates to the alveolar ridge and begins to make peristaltic waves to transport the food into the pharynx. Differentiated tongue, lip and jaw movements are well established during semi-solid food feeding as early by 10 months as described by Suzanne Evans-Morris (1987) in the Developmental Pre Feeding Checklist. The jaw remains in a stable position at 6-7 months with the lips assisting in food intake at 10 months and the tongue tip elevating intermittently at 12 months and consistently at 18 months with no extension/retraction or protrusion of the tongue occurring.
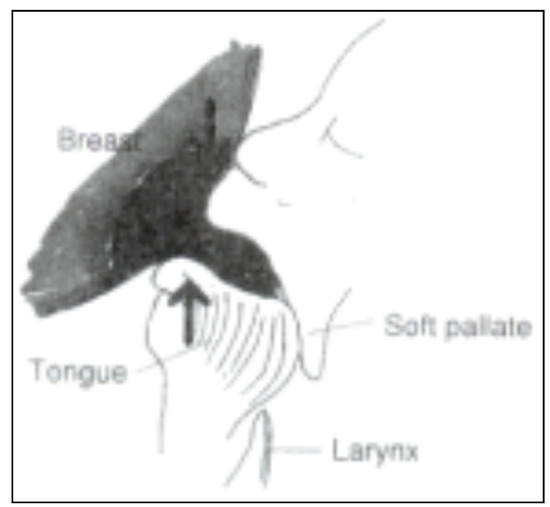
Figure 1.
Compression of the lips, tongue and gums forces the flow from the nipple.
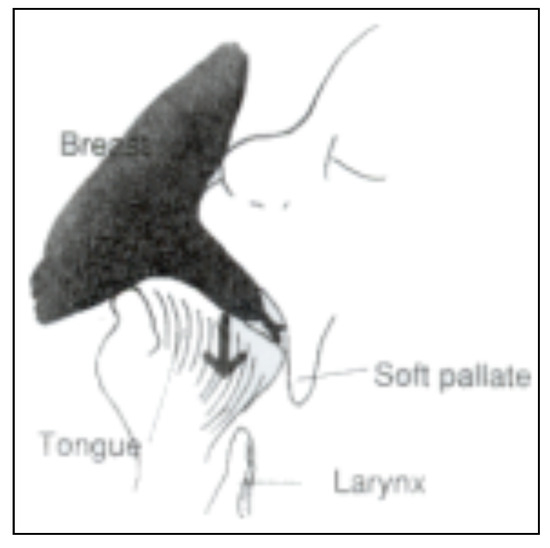
Figure 2.
The downward action of the jaw creates vacuum pressure space in the oral cavity drawing the flow from the nipple.
Mastication
Fletcher (1970) describes the addition of the dental occlusion as being an important source of stabilization for a mature swallow, which allows the tongue to develop more precise control of the bolus during deglutition. Initially, lip closure and perioral contractions provide stability in the anterior oral region. As the teeth erupt, stability is achieved through sensory feedback in the periodontal structures of the teeth and gums, which allows the tongue the freedom necessary to sort food, and form a bolus. Ayano (1998) and colleagues described these movements in a 10-month old eating a cookie. Lateral movements of the tongue were observed as the food was brought to the chewing or “mashing” surfaces, and the formation of a central groove in the tongue was observed to assist in forming and transporting the bolus. The ability to form a central groove was thought to be essential to the ability to form a bolus. In studying the development of tongue motion using ultrasound, Ayano and colleagues were unable to detect central grooves in the tongue of a normal 5 month old infant but were able to detect central grooves at 8 months of age. They noted that the depth of the central grooves on the tongue surface increased with age. In 1886, Wassilief observed this phenomena and reported that touching the surface of the infant tongue elicited suckling movements whereas similar stimulation of an adult tongue caused it to curve into the shape of a spoon.
Imai (1995) and associates found similar movements of the tongue during mastication by adults. The tongue turned the food, mixed it with saliva, sorted out unsuitable particles and aided in bolus formation. Evans-Morris (1987) describes these same skills in a 24 month-old. At this early age, the child is able to swallow solid foods including those with mixed textures with easy lip closure and consistent tongue tip elevation for swallowing, and is able to use a controlled sustained bite with graded jaw movements, and a stable midline head position. By 24 months, the child is able to transfer food side to side and from side to center of the mouth, again with precise tongue tip elevation and no extension/retraction movements of the tongue.
Mature Speech Patterns
While the feeding literature clearly indicates that the refined movements necessary for a mature swallow are developed by the age of 24 months, and are often observed even earlier, as in Ayano’s (1998) work, investigations into the areas of motor skills necessary for mature speech patterns indicate that motor skill refinement continues up until the age of 6-7 years. Green et al. (2000) studied lip and jaw coordination in the development of speech motor control and found that, “the coordinative organization of these gestures was shown to change dramatically during the first several years of life and to continue to undergo refinement past age 6.” They found that the involvement of upper lip, lower lip, and jaw for oral closure was similar between 6 year old and adult subjects. Their one-year-old subjects assimilated lower lip movements into established jaw movement patterns. They went on to hypothesize that the following coordinative features observed in their study may limit sound producing capabilities during the first few years of life: a) the prevalence of jaw movement; b) poor lip and jaw coupling; c). poor lip control; and d) poor upper and lower lip movement independence.
Gibbon (1999) reviewed the literature on electropalatography (EPG) and studies of undifferentiated lingual gestures in children with articulation/phonological disorders. In studies using EPG in normal children, Fletcher (1970) found that for all lingual consonants the number of sensors contacted decreased with the age of the subjects, indicating an increased ability to move the tongue tip/blade independently of tongue body movement. In her literature review, Gibbon (1999) found that 71% of children with articulation/phonological disorders show evidence of undifferentiated lingual gestures. One characteristic of mature lingual control is that the tongue tip/blade and tongue body do not always move together, but demonstrate the ability to move relatively independently of each other and to coarticulate, which is the modification of movement according to the preceding or following sound. Children with undifferentiated EPG patterns have additional difficulties in the control of the lateral and medial regions of the tongue. Control of the lateral margins of the tongue is thought to be essential to normal speech production because lateral anchoring gives stability to the whole tongue. Gibbon concludes that undifferentiated lingual gestures reflect a speech motor constraint involving regions of the tongue that in normal speakers function relatively independently.
Therefore, it may be stated that lack of independent, differentiated movement of the oral structures not only limits the development of mature swallowing and deglutition but also has an equally detrimental effect on the development of mature speech patterns. If our goal in orofacial myofunctional therapy is, as our colleague, Galen Peachey (2000) states, “to establish NOMF: normal oral muscle function”, then we clearly have to evaluate for the presence of undifferentiated lip, tongue and jaw movements and facilitate the development of the more refined, independent movements required for mature patterns of swallowing and deglutition.
In my practice, I evaluate and document each patient’s ability to differentiate lip, tongue and jaw movements. In 1999, I collected data on tongue and jaw differentiation. Of the 40 patients discharged from oral myofunctional therapy in 1999, 95% were unable to differentiate tongue and jaw movements prior to therapy. For patients discharged from articulation therapy, 90 % were unable to differentiate tongue and jaw movements, prior to therapy.
Other areas worth investigating are speed and pattern of diadochokinesis. I have not systematically kept data on all patients, but on many oral myofunctional patients and articulation patients, diadochokinesis for tongue and lip repetitions are below average in speed at the time of the evaluation and increase in speed and accuracy after completion of therapy.
Undifferentiated Movements In Orofacial Myofunctional Disorders
These are some of the manifestations seen in patients experiencing Orofacial Myofunctional Disorders.
Drinking:
- Tongue comes forward to meet the cup.
- Lips and jaw open simultaneously. Lack of lip seal around edge of cup may be observed.
- Circumoral contraction for stability may be present.
- Jaw movement during consecutive swallows demonstrates an infantile pattern.
- Head, upper body comes forward to take sip with lack of head, mouth, and hand differentiation.
Eating:
- Tongue comes forward to meet the food.
- Food is crammed in the mouth vs. taking bites.
- Tongue is positioned forward during bite with the tongue and jaw biting together.
- Tongue smacking, protrusion during chewing - tongue moving in same pattern as jaw may be observed.
- Circumoral contraction for stability may be present.
Other Observations:
- Inability to open the mouth without tongue movement forward or down.
- Inability to elevate tongue to the spot with jaw open.
- Inability to protrude tongue without associated lip and jaw movement.
- Tendency to protrude tongue when lips close. (Tip moves forward to lingual or cutting
- Tendency to protrude tongue when lips purse.
- Tendency to protrude tongue when an object or finger approach the mouth.
- Inability to maintain tip on the spot when opening or closing jaw, or opening or closing ips.
- Inability to maintain tongue tip up, back tongue down rest posture: always have a linguapalatal seal at rest.
Assessment
Some ways of evaluating for the presence of tongue, lip, jaw differentiation include:
- Lip pucker and smile: Have the patient close his/her mouth and then alternately smile and pucker. Make sure the patient smiles to show the teeth and then puckers. Is there associated jaw movement or tongue movement during this task? Do you see the jaw and/or tongue moving during either phase of the activity? If so, there is poor lip/jaw differentiation.
- Open mouth, stick out tongue: Instruct the patient to “Open your mouth and stick out your tongue as far as you can.” Does this happen sequentially or simultaneously? Does the jaw open as the tongue is protruded or does the tongue remain in contact with the lips as it is protruded - if so, there is poor tongue/jaw differentiation.
- Elevate the tongue to touch the nose : While the patient has his/her tongue protruded, instruct to “Slowly lift your tongue up to touch your nose.” Is there accessory jaw elevation? Is the tongue in contact with teeth? If so, there is poor differentiation of tongue/jaw.
- Depress tongue to touch chin: With the patient’s tongue protruded, instruct “ Now slowly try and touch your chin with your tongue.” Is there jaw movement (elevation, lateral sliding), does the tongue remain in contact with teeth?
- Lateralize tongue side to side:: With the tongue protruded, instruct the patient to “Wiggle your tongue from side to side.” Is there jaw movement? Is the tongue in contact with mandibular teeth? If so, tongue/jaw differentiation is poor.
- Diadochokinesis: When evaluating bilabial consonant repetitions (puh), watch for mandibular movement. With alveolar consonant repetitions, (tuh), watch for mandibular movement, place of articulation (linguadental, interdental, alveolar) as well as what part of the tongue is being used - tip, blade, dorsum. With velar consonant repetitions, (kuh), watch for mandibular movement and degree of lingual movement.
- Speech articulation: Have patient repeat words and phrases containing tongue tip sounds, and sibilants such as “It’s hot. Not now. Too late. I like licorice.”Watch for associated jaw movements in speech and place of articulation and what part of tongue is making contact. Patients with poor differentiation tend to make minimal tongue tip movements and use the blade of the tongue to articulate alveolar consonants and often have associated jaw elevation or lateral shifting during speech.
Treatment Techniques
These are some of the exercises I have developed to facilitate improved tongue, lip, and jaw differentiation in patients with oral myofunctional disorders and articulation disorders.
- Oral Tactile Stimulation: “Brush and Hold”: Have patient open mouth widely and protrude tongue. Use Toothette to brush the sides of tongue (stimulates lateral stability), tip of tongue, and the “SPOT”. This stimulation will frequently stimulate the lateral borders of the tongue to contract and stabilize for better tongue point. The patient then elevates the tongue tip to the spot, closes the back teeth and lips and holds this position for ten seconds. This is repeated ten times. Each subsequent day of practice the patient holds this position ten seconds longer, (20 seconds, 30 seconds, and so on).
- Spot Tapping: This teaches tongue tip elevation without associated jaw movement. Instruct the patient to open widely, and elevate the tip of the tongue to the SPOT and back down behind the lower incisors ten times without moving the jaw or touching the teeth with the tongue. Helps develop elevation/depression movements of tongue versus extension/retraction pattern of tongue thrust. Many patients may need to stabilize their chin with their hand or use a bite block to stabilize jaw.
- Skinny-Fat: Develops ability to protrude the tongue without associated jaw, or lip movement as well as train lateral tongue stability and awareness of and strength in the lateral borders of the tongue. The patient is instructed to open wide, and stick out the tongue without letting the tongue touch the lips or teeth and point the tongue and then relax. This is repeated ten times. “Wagging” the tongue side to side will also help pull in the lateral tongue muscles. Following a moving target (e.g., tongue depressor or toothette) with the tongue protruded will also help develop a point as will licking without touching the lips or moving the chin.
- Clicking: This encourages tongue tip stability while differentiating posterior and lateral tongue movement. Develops the slurping/gathering muscles and an awareness of the lateral tongue muscles. This is often called the “Giddy-up” exercise as it is the sound made while riding a horse. The patient is instructed to suck the tongue up softly to the roof of the mouth behind the teeth and let go of the suction in the back and sides only without letting go of the tip. Having the patient open the mouth slightly will aid in seeing the movement. This is repeated ten times.
- Frog: This develops independent posterior tongue movement and posterior tongue awareness. The patient is instructed to open wide and while keeping the tongue on the floor of the mouth, pull the tongue back in the mouth and say “Guh” without letting the jaw/chin move. This is repeated ten times.
- Tongue pop-open/close: This develops the ability to maintain a linguapalatal seal with the necessary jaw movement required for mature liquid, soft food, and solid food swallows. The patient is instructed to suck the tongue up to the roof of the mouth and holding the suction, slowly close and open the jaw/teeth. This is repeated ten times. The patient is instructed to keep the lingual frenum stretched during the opening phase.
- Lip pucker/smile: This encourages maintenance of a stable tongue tip while creating an appropriate lip seal for cup drinking without associated jawmovement or tongue movement. The patient is instructed to place elastic on the tip of the tongue and elevate it to the spot and then close the back teeth. Holding this position, the patient retracts (smile) and puckers the lips without letting the jaw or tongue move. This is repeated 10 times.
- Tongue tapping: This develops medial tongue awareness and facilitates the development of the midline groove necessary for bolus control with liquids/solids. The patient is instructed to open wide and keep the tongue flat and relaxed on the floor of the mouth. With a tongue depressor, he/she then taps the middle section of the tongue, just anterior to the first molars and presses this t down to form a “bowl” shape. This is repeated ten times.
- Lip Stick: This develops tongue tip stability and jaw stability. The patient places an elastic on the tip of the tongue and lifts to the spot then closes the back teeth and lips. The patient then is instructed to say “oo” to get the lips sufficiently in front of the teeth, and a flavored tongue depressor is placed in between the lips and the patient is instructed to say “mm” to close the lips around the depressor and hold. Frequently, patients will move their jaw, disocclude their back teeth to protrude the lips. The elastic serves to help stabilize the tongue tip as well as a conscious reminder of tongue resting posture.
- Squeaky Sips and Hold: When introducing cup drinking, this facilitates independent yet coordinated movements of lips for lip seal, tongue suction and linguapalatal seal for control of bolus prior to swallow. The patient is instructed to pucker the lips, bring the cup to the lips, (this is important, often the patient will bring his/her head forward toward the cup), and “kiss the cup”, suck in a small amount of liquid on top of the tongue and then suck and trap the liquid with the tongue on the roof of the mouth like a tongue pop and hold with teeth apart, for 3 seconds. This is repeated ten times.
Encouraging Development of Differentiated Movement Patterns
These are just a few of the possibilities for developing better orofacial function. I am sure many members of the International Association of Orofacial Myology have more suggestions.
- Begin cup drinking at 12 months and start limiting the bottle/breast.
- Introduce chewable foods at 8-12 months.
- Encourage mouthing of objects/foods at 4 months which helps develop sensory skills.
- Encourage chewing using crunchy foods and chewing activities, and other oral tactile activities.
- Avoid pacifiers, and “sippy” cups past 12 months. Start cup drinking at 8-12 months.
- Use “to go cup” design vs. sippy cup for spill control.
- Keep nasal airway clear/monitored.
- Develop other self-calming skills at 2-3 years to avoid prolonged sucking habits.
CONCLUSION AND RECOMMENDATIONS
It is critical for orofacial myologists to understand the normal developmental progression of differentiation and stability of the orofacial complex. Treatment programs for swallowing, deglutition, and for verbal speech skills will offer greater success for the patient if the orofacial myologist applies the principles of differentiation and stability to their therapeutic activities. with a thorough understanding of normal developmental processes underlying deglutition, swallowing and speech skills, the therapist will be more able to customize his or her therapy program to meet the individual needs of the patient as well as provide an adequate explanation of the rationale for each exercise to the patient or parent.
Utilizing the growing body of knowledge of normal developmental processes involved in swallowing development, there is a need to identify the presence or absence of differentiation in patients exhibiting orofacial myofunctional disorders. Another area of investigation would be documentation of improvement in tongue, lip, and jaw differentiation following myofunctional therapy. Documentation of improvement in speed and accuracy of speech movements following myofunctional therapy that involves specific attention to tongue, lip, and jaw differentiation would also be an area worth investigating.
References
- Ayano, R., F. Tamura, Y. Ohtsuka, and Y. Mukai. 1998. Development of normal feeding and swallowing. In Presentation given at International Association of Orofacial Myology Convention. San Diego CA. [Google Scholar]
- Ayres, A.J. 1979. Sensory integration and the child. Los Angeles CA: Western Psychological Services.
- Bosma, J. F. 1963. Maturation of function of the oral and pharyngeal region. American Journal of Orthodontics 49: 94–104. [Google Scholar] [CrossRef]
- Evans Morris, S. 1987. Developmental pre-feeding checklist. Therapy Skill Builders: Tuscon, AZ. [Google Scholar]
- Fletcher, S. 1970. Processes and maturation of mastication and deglutition in speech and the dentofacial complex: The state of the art, proceedings of the workshop. ASHA Reports, vol. 5. [Google Scholar]
- Gibbon, F. 1999. Undifferentiated lingual gestures in children with articulation/phonological disorders. Journal of Speech, Language, and Hearing Research 42: 382–397. [Google Scholar] [CrossRef] [PubMed]
- Green, J., C. Moore, M. Higashikawa, and R. Steeve. 2000. The physiologic development of speech motor control: lip and jaw coordination. Journal of Speech Language and Hearing Research 43: 239256. [Google Scholar] [CrossRef] [PubMed]
- Imai, A., M. Tanaka, M. Tatsuta, and T. Kawazoe. 1995. Ultrasonic images of tongue movement during mastication. Journal of Osaka Dental University 29, 2: 61–69. [Google Scholar] [PubMed]
- Marshalla, P. 1992. Oral motor techniques in articulation therapy. Workshop Handbook.
- Oetter, P., E. Richter, and S. Frick. 1988. M.O.R.E.: Integrating the mouth with sensory and postural functions. Hugo MN: PDP Press. [Google Scholar]
- Peachey, G. 2000. Personal Communication.
- Tamura, Y., Y. Horikawa, and S. Yoshida. 1996. Co-ordination of tongue movements and peri-oral muscle activities during nutritive suckling. Developmental Medicine and Child Neurology 38: 503–510. [Google Scholar] [CrossRef] [PubMed]
- Wassilieff, N. W. 1886. Uber eine localisirte reflectorisshce. Bewegungder Zunge. Zbl. Med. WISs 24: 209–210. [Google Scholar]
© 2000 by the author. 2000 Patricia G. Meyer.