Advancing Syphilis Research: Exploring New Frontiers in Immunology and Pharmacological Interventions
Abstract
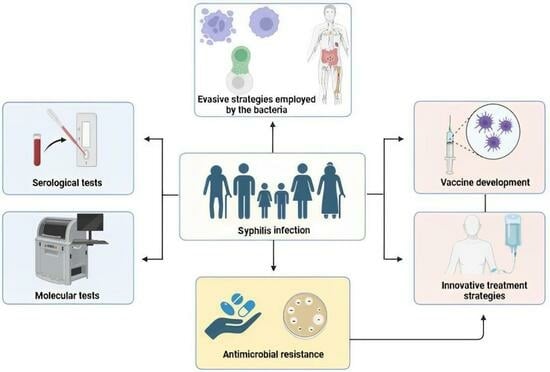
1. Introduction
2. Epidemiology of Syphilis: Current Trends and Future Challenges
2.1. Immunology and Pathogenesis of Syphilis
2.2. Risk Factors
3. Diagnosis of Syphilis: Advances and Challenges
3.1. Direct Tests for T. pallidum Detection
3.2. Serological Tests for Detection of Antibodies against T. pallidum
3.2.1. Non-Treponemal Tests (NTT) Limitations, including Special Populations
3.2.2. Authorized Tests: aRPR and RPR-S
3.3. Treponemal Tests for Detection of Antibodies
3.4. Molecular Techniques and Mass Spectrometry
4. Pharmacological Interventions
4.1. Penicillin: The Cornerstone of Syphilis Treatment
4.2. Alternative Antibiotics and DoxyPrEP
4.3. Azithromycin Resistance in Syphilis
4.4. Challenges and Future Directions in Syphilis Treatment
5. Future Approaches in Syphilis Prevention and Control
5.1. Development of Effective Vaccines
5.2. Innovative Point-of-Care Diagnostics
5.3. Targeted Prevention Strategies
5.4. Integration of Syphilis Services into Primary Healthcare
6. Future Directions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Marks, M.; Solomon, A.W.; Mabey, D.C. Endemic Treponemal Diseases. Trans. R. Soc. Trop. Med. Hyg. 2014, 108, 601–607. [Google Scholar] [CrossRef]
- Kojima, N.; Klausner, J.D. An Update on the Global Epidemiology of Syphilis. Curr. Epidemiol. Rep. 2018, 5, 24–38. [Google Scholar] [CrossRef]
- Tiecco, G.; Degli Antoni, M.; Storti, S.; Marchese, V.; Focà, E.; Torti, C.; Castelli, F.; Quiros-Roldan, E. A 2021 Update on Syphilis: Taking Stock from Pathogenesis to Vaccines. Pathogens 2021, 10, 1364. [Google Scholar] [CrossRef]
- Li, S.; Li, W.; Jin, Y.; Wu, B.; Wu, Y. Advancements in the Development of Nucleic Acid Vaccines for Syphilis Prevention and Control. Hum. Vaccin. Immunother. 2023, 19, 2234790. [Google Scholar] [CrossRef]
- Peeling, R.W.; Mabey, D.; Chen, X.-S.; Garcia, P.J. Syphilis. Lancet 2023, 402, 336–346. [Google Scholar] [CrossRef]
- Osias, E.; Hung, P.; Giacani, L.; Stafylis, C.; Konda, K.A.; Vargas, S.K.; Reyes-Díaz, E.M.; Comulada, W.S.; Haake, D.A.; Haynes, A.M.; et al. Investigation of Syphilis Immunology and Treponema Pallidum Subsp. Pallidum Biology to Improve Clinical Management and Design a Broadly Protective Vaccine: Study Protocol. BMC Infect. Dis. 2020, 20, 444. [Google Scholar] [CrossRef]
- Mues, N.; Chu, H.W. Out-Smarting the Host: Bacteria Maneuvering the Immune Response to Favor Their Survival. Front. Immunol. 2020, 11, 819. [Google Scholar] [CrossRef]
- Scott, B.N.V.; Sarkar, T.; Kratofil, R.M.; Kubes, P.; Thanabalasuriar, A. Unraveling the Host’s Immune Response to Infection: Seeing Is Believing. J. Leukoc. Biol. 2019, 106, 323–335. [Google Scholar] [CrossRef]
- Huemer, M.; Mairpady Shambat, S.; Brugger, S.D.; Zinkernagel, A.S. Antibiotic Resistance and Persistence—Implications for Human Health and Treatment Perspectives. EMBO Rep. 2020, 21, e51034. [Google Scholar] [CrossRef]
- Murugaiyan, J.; Kumar, P.A.; Rao, G.S.; Iskandar, K.; Hawser, S.; Hays, J.P.; Mohsen, Y.; Adukkadukkam, S.; Awuah, W.A.; Jose, R.A.M.; et al. Progress in Alternative Strategies to Combat Antimicrobial Resistance: Focus on Antibiotics. Antibiotics 2022, 11, 200. [Google Scholar] [CrossRef]
- Miethke, M.; Pieroni, M.; Weber, T.; Brönstrup, M.; Hammann, P.; Halby, L.; Arimondo, P.B.; Glaser, P.; Aigle, B.; Bode, H.B.; et al. Towards the Sustainable Discovery and Development of New Antibiotics. Nat. Rev. Chem. 2021, 5, 726–749. [Google Scholar] [CrossRef]
- Cohen, S.E.; Klausner, J.D.; Engelman, J.; Philip, S. Syphilis in the Modern Era. Infect. Dis. Clin. N. Am. 2013, 27, 705–722. [Google Scholar] [CrossRef]
- Peeling, R.W.; Mabey, D.; Kamb, M.L.; Chen, X.-S.; Radolf, J.D.; Benzaken, A.S. Syphilis. Nat. Rev. Dis. Primers 2017, 3, 17073. [Google Scholar] [CrossRef]
- Avelleira, J.C.R.; Bottino, G. Sífilis: Diagnóstico, Tratamento e Controle. An. Bras. Dermatol. 2006, 81, 111–126. [Google Scholar] [CrossRef]
- Singh, A.E.; Romanowski, B. Syphilis: Review with Emphasis on Clinical, Epidemiologic, and Some Biologic Features. Clin. Microbiol. Rev. 1999, 12, 187–209. [Google Scholar] [CrossRef]
- Tsimis, M.E.; Sheffield, J.S. Update on Syphilis and Pregnancy. Birth Defects Res. 2017, 109, 347–352. [Google Scholar] [CrossRef]
- Stoltey, J.E.; Cohen, S.E. Syphilis Transmission: A Review of the Current Evidence. Sex. Health 2015, 12, 103. [Google Scholar] [CrossRef]
- Bilman, V.; Bertoglio, L.; Melissano, G.; Chiesa, R. Contained Rupture of an Aortic Arch Aneurysm in a Patient with Syphilitic Aortitis. A Case Report. J. Vasc. Bras. 2021, 20, e20210160. [Google Scholar] [CrossRef]
- Cocora, M.; Nechifor, D.; Lazar, M.-A.; Mornos, A. Impending Aortic Rupture in a Patient with Syphilitic Aortitis. Vasc. Health Risk Manag. 2021, 17, 255–258. [Google Scholar] [CrossRef]
- Stamm, L.V. Syphilis: Re-Emergence of an Old Foe. Microb. Cell 2016, 3, 363–370. [Google Scholar] [CrossRef]
- Tang, Y.; Zhou, Y.; He, B.; Cao, T.; Zhou, X.; Ning, L.; Chen, E.; Li, Y.; Xie, X.; Peng, B.; et al. Investigation of the Immune Escape Mechanism of Treponema Pallidum. Infection 2023, 51, 305–321. [Google Scholar] [CrossRef] [PubMed]
- Carlson, J.A.; Dabiri, G.; Cribier, B.; Sell, S. The Immunopathobiology of Syphilis: The Manifestations and Course of Syphilis Are Determined by the Level of Delayed-Type Hypersensitivity. Am. J. Dermatopathol. 2011, 33, 433–460. [Google Scholar] [CrossRef] [PubMed]
- Cruz, A.R.; Ramirez, L.G.; Zuluaga, A.V.; Pillay, A.; Abreu, C.; Valencia, C.A.; La Vake, C.; Cervantes, J.L.; Dunham-Ems, S.; Cartun, R.; et al. Immune Evasion and Recognition of the Syphilis Spirochete in Blood and Skin of Secondary Syphilis Patients: Two Immunologically Distinct Compartments. PLoS Negl. Trop. Dis. 2012, 6, e1717. [Google Scholar] [CrossRef] [PubMed]
- Giacani, L.; Molini, B.J.; Kim, E.Y.; Godornes, B.C.; Leader, B.T.; Tantalo, L.C.; Centurion-Lara, A.; Lukehart, S.A. Antigenic Variation in Treponema Pallidum: TprK Sequence Diversity Accumulates in Response to Immune Pressure during Experimental Syphilis. J. Immunol. 2010, 184, 3822–3829. [Google Scholar] [CrossRef]
- Liu, D.; Tong, M.-L.; Lin, Y.; Liu, L.-L.; Lin, L.-R.; Yang, T.-C. Insights into the Genetic Variation Profile of TprK in Treponema Pallidum during the Development of Natural Human Syphilis Infection. PLoS Negl. Trop. Dis. 2019, 13, e0007621. [Google Scholar] [CrossRef]
- Zhou, J.; Zhang, H.; Tang, K.; Liu, R.; Li, J. An Updated Review of Recent Advances in Neurosyphilis. Front. Med. 2022, 9, 800383. [Google Scholar] [CrossRef] [PubMed]
- Clement, M.E.; Okeke, N.L.; Hicks, C.B. Treatment of Syphilis A Systematic Review. JAMA 2014, 312, 1905. [Google Scholar] [CrossRef]
- Liu, H.; Han, Y.; Chen, X.; Bai, L.; Guo, S.; Li, L.; Wu, P.; Yin, Y. Comparison of Efficacy of Treatments for Early Syphilis: A Systematic Review and Network Meta-Analysis of Randomized Controlled Trials and Observational Studies. PLoS ONE 2017, 12, e0180001. [Google Scholar] [CrossRef]
- LaFond, R.E.; Lukehart, S.A. Biological Basis for Syphilis. Clin. Microbiol. Rev. 2006, 19, 29–49. [Google Scholar] [CrossRef]
- Radolf, J.D.; Deka, R.K.; Anand, A.; Šmajs, D.; Norgard, M.V.; Yang, X.F. Treponema Pallidum, the Syphilis Spirochete: Making a Living as a Stealth Pathogen. Nat. Rev. Microbiol. 2016, 14, 744–759. [Google Scholar] [CrossRef]
- Morshed, M.G.; Singh, A.E. Recent Trends in the Serologic Diagnosis of Syphilis. Clin. Vaccine Immunol. 2015, 22, 137–147. [Google Scholar] [CrossRef]
- Church, B.; Wall, E.; Webb, J.R.; Cameron, C.E. Interaction of Treponema Pallidum, the Syphilis Spirochete, with Human Platelets. PLoS ONE 2019, 14, e0210902. [Google Scholar] [CrossRef]
- Pereira Nogueira, W.; Figueiredo Nogueira, M.; de Almeida Nogueira, J.; Freire, M.E.M.; Gir, E.; de Oliveira e Silva, A.C. Syphilis in Riverine Communities: Prevalence and Associated Factors. Rev. Esc. Enferm. USP 2022, 56, e20210258. [Google Scholar] [CrossRef]
- Schmidt, R.; Carson, P.J.; Jansen, R.J. Resurgence of Syphilis in the United States: An Assessment of Contributing Factors. Infect. Dis. Res. Treat. 2019, 12, 117863371988328. [Google Scholar] [CrossRef]
- Workowski, K.A.; Bachmann, L.H.; Chan, P.A.; Johnston, C.M.; Muzny, C.A.; Park, I.; Reno, H.; Zenilman, J.M.; Bolan, G.A. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recomm. Rep. 2021, 70, 187. [Google Scholar] [CrossRef] [PubMed]
- Copen, C.E.; Brookmeyer, K.A.; Haderxhanaj, L.T.; Hogben, M.; Torrone, E.A. Sexual Risk Behaviors Among Persons Diagnosed With Primary and Secondary Syphilis Who Reported High-Risk Substance Use: Data from the National Notifiable Diseases Surveillance System, 2018. Sex. Transm. Dis. 2022, 49, 99–104. [Google Scholar] [CrossRef]
- Ye, X.; Li, F.-R.; Pan, Q.; Li, Z.; Yu, G.-Q.; Liu, H.; Liu, J.; Huai, P.-C.; Zhang, F.-R. Prevalence and Associated Factors of Sexually Transmitted Infections among Methamphetamine Users in Eastern China: A Cross-Sectional Study. BMC Infect. Dis. 2022, 22, 7. [Google Scholar] [CrossRef]
- Jennings, J.M.; Wagner, J.; Tilchin, C.; Schumacher, C.M.; Thornton, N.; Hamill, M.M.; Rompalo, A.; Ruhs, S.; Rives, S.; Ghanem, K.G.; et al. Methamphetamine Use, Syphilis, and Specific Online Sex Partner Meeting Venues Are Associated with HIV Status among Urban Black Gay and Bisexual Men Who Have Sex Men. Sex. Transm. Dis. 2021, 48, S32–S39. [Google Scholar] [CrossRef] [PubMed]
- da Costa Dantas, J.; Marinho, C.D.S.R.; Pinheiro, Y.T.; Fernandes Ferreira, M.Â.; Rosendo da Silva, R.A. Spatial Distribution of Gestational Syphilis in Brazil: Socioeconomic and Health Services Inequalities. Am. J. Trop. Med. Hyg. 2023, 109, 42–49. [Google Scholar] [CrossRef]
- Ramos, R.D.S.P.D.S.; Carneiro, G.R.; Oliveira, A.L.S.D.; Cunha, T.N.D.; Ramos, V.P. Incidence of Congenital Syphilis According to Inequalities and Living Conditions in the City of Recife, Pernambuco, Brazil. Rev. Bras. Saúde Matern. Infant. 2021, 21, 785–794. [Google Scholar] [CrossRef]
- Smock, L.; Caten, E.; Hsu, K.; DeMaria, A. Economic Disparities and Syphilis Incidence in Massachusetts, 2001–2013. Public Health Rep. 2017, 132, 309–315. [Google Scholar] [CrossRef]
- Marques dos Santos, M.; Lopes, A.K.B.; Roncalli, A.G.; Lima, K.C.D. Trends of Syphilis in Brazil: A Growth Portrait of the Treponemic Epidemic. PLoS ONE 2020, 15, e0231029. [Google Scholar] [CrossRef] [PubMed]
- Ren, M.; Dashwood, T.; Walmsley, S. The Intersection of HIV and Syphilis: Update on the Key Considerations in Testing and Management. Curr. HIV/AIDS Rep. 2021, 18, 280–288. [Google Scholar] [CrossRef]
- Ribeiro, A.; Trevizol, A.; Oluwoye, O.; McPherson, S.; McDonell, M.G.; Briese, V.; Miguel, A.C.; Fratzinger, R.C.; Laranjeira, R.R.; Alonso, A.L.; et al. HIV and Syphilis Infections and Associated Factors among Patients in Treatment at a Specialist Alcohol, Tobacco, and Drugs Center in São Paulo’s “Cracolândia”. Trends Psychiatry Psychother. 2020, 42, 1–6. [Google Scholar] [CrossRef]
- Simões, L.A.; Mendes, J.C.; Silveira, M.R.; Costa, A.M.G.D.; Lula, M.D.; Ceccato, M.D.G.B. Fatores Associados à Coinfecção HIV/Sífilis No Início Da Terapia Antirretroviral. Rev. Saude Publica 2022, 56, 59. [Google Scholar] [CrossRef]
- Quiros-Roldan, E.; Izzo, I.; Carriero, C.; Antoni, M.D.; Storti, S.; Tiecco, G.; Gardini, G.; Focà, E.; Castelli, F. Decrease in New Diagnosis of HIV/AIDS in the Two Years Period 2019-2020: Impact of COVID-19 Pandemic. J. Public health Res. 2022, 11, jphr.2021.2256. [Google Scholar] [CrossRef]
- Kalichman, S.C.; Pellowski, J.; Turner, C. Prevalence of Sexually Transmitted Co-Infections in People Living with HIV/AIDS: Systematic Review with Implications for Using HIV Treatments for Prevention. Sex. Transm. Infect. 2011, 87, 183–190. [Google Scholar] [CrossRef]
- Schillinger, D. Social Determinants, Health Literacy, and Disparities: Intersections and Controversies. HLRP Health Lit. Res. Pract. 2021, 5, e234–e243. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Granger, J.; Espadafor López, B.; Cobo, F.; Blasco Morente, G.; Sampedro Martinez, A.; Tercedor Sánchez, J.; Aliaga-Martinez, L.; Padilla-Malo de Molina, A.; Navarro-Marí, J.M. Update on the Diagnosis of Sexually Transmitted Infections. Actas Dermo-Sifiliográficas (Engl. Ed.) 2020, 111, 711–724. [Google Scholar] [CrossRef]
- Caitano, A.R.; Gusmão, C.M.G.; Dias-Trindade, S.; Barbalho, I.M.P.; Morais, P.S.G.; Caldeira-Silva, G.J.P.; Romão, M.H.; Valentim, J.L.R.S.; Dias, A.P.; Alcoforado, J.L.M.; et al. Massive Health Education through Technological Mediation: Analyses and Impacts on the Syphilis Epidemic in Brazil. Front. Public Health 2022, 10, 944213. [Google Scholar] [CrossRef] [PubMed]
- Macêdo, V.C.D.; Lira, P.I.C.D.; Frias, P.G.D.; Romaguera, L.M.D.; Caires, S.D.F.F.; Ximenes, R.A.D.A. Risk Factors for Syphilis in Women: Case-Control Study. Rev. Saude Publica 2017, 51, 78. [Google Scholar] [CrossRef]
- Solaimalai, D.; Gupta, A.; George, L.; Manesh, A.; Karthik, R.; Sathishkumar, D.; Peter, C.V.D.; Varghese, G.M.; Pulimood, S.A.; Kannangai, R.; et al. Upward Trends of Syphilis in the Non-Pregnant Adults: A Six-Year Report on Clinical and Epidemiological Profile of Syphilis from a Tertiary Care Center, India. Front. Public Health 2022, 10, 908591. [Google Scholar] [CrossRef]
- Varshney, K.; Ikanovic, A.; Ghosh, P.; Shet, P.; Di Sipio, M.; Khatri, C.; Mahmood, M.Q. A Global Scoping Review of the Factors Associated with HIV and Syphilis Co-Infection: Findings from 40 Countries. Venereology 2022, 1, 98–113. [Google Scholar] [CrossRef]
- Peterman, T.A.; Furness, B.W. Public Health Interventions to Control Syphilis. Sex. Health 2015, 12, 126. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Xie, Y.; Xiao, Y. Laboratory Diagnostic Tools for Syphilis: Current Status and Future Prospects. Front. Cell. Infect. Microbiol. 2021, 10, 574806. [Google Scholar] [CrossRef] [PubMed]
- Wolgemuth, C.W. Flagellar Motility of the Pathogenic Spirochetes. Semin. Cell Dev. Biol. 2015, 46, 104–112. [Google Scholar] [CrossRef]
- Forrestel, A.K.; Kovarik, C.L.; Katz, K.A. Sexually Acquired Syphilis. J. Am. Acad. Dermatol. 2020, 82, 17–28. [Google Scholar] [CrossRef]
- Hook, E.W.; Roddy, R.E.; Lukehart, S.A.; Hom, J.; Holmes, K.K.; Tam, M.R. Detection of Treponema Pallidum in Lesion Exudate with a Pathogen-Specific Monoclonal Antibody. J. Clin. Microbiol. 1985, 22, 241–244. [Google Scholar] [CrossRef]
- Ito, F.; Hunter, E.F.; George, R.W.; Pope, V.; Larsen, S.A. Specific Immunofluorescent Staining of Pathogenic Treponemes with a Monoclonal Antibody. J. Clin. Microbiol. 1992, 30, 831–838. [Google Scholar] [CrossRef]
- Morshed, M.G. Current Trend on Syphilis Diagnosis: Issues and Challenges. In Infectious Diseases and Nanomedicine II; Advances in Experimental Medicine and Biology; Springer: New Delhi, India, 2014; pp. 51–64. [Google Scholar]
- Mallma, P.; Garcia, P.; Carcamo, C.; Torres-Rueda, S.; Peeling, R.; Mabey, D.; Terris-Prestholt, F. Rapid Syphilis Testing Is Cost-Effective Even in Low-Prevalence Settings: The CISNE-PERU Experience. PLoS ONE 2016, 11, e0149568. [Google Scholar] [CrossRef]
- García Luna, J.A.; Romero-Rosas, N.; Silva Pena, S.A.; Oviedo Sarmiento, O.J.; Galindo Orrego, X.; Lenis Quintero, W.; Perea, L.C.; Buitrago, E.M.; Osorio, L.; Salazar, J.C.; et al. Smith Diagnostic performance of two rapid tests for syphilis screening in people living with HIV in Cali, Colombia. PLoS ONE 2023, 18, e0282492. [Google Scholar] [CrossRef]
- Gao, K.; Shen, X.; Lin, Y.; Zhu, X.-Z.; Lin, L.-R.; Tong, M.-L.; Xiao, Y.; Zhang, H.-L.; Liang, X.-M.; Niu, J.-J.; et al. Origin of Nontreponemal Antibodies During Treponema Pallidum Infection: Evidence From a Rabbit Model. J. Infect. Dis. 2018, 218, 835–843. [Google Scholar] [CrossRef]
- Leroy, A.-G.; Robert, M.; Carpentier, M.; Bastidon, C.; Gautreau, B.; Lefebvre, M.; Bonnet, B.; Bernier, C.; Corvec, S.; Guillouzouic, A. Assessment of a Fully Automated RPR Assay (Mediace RPR) for Serological Diagnosis and Follow-up of Syphilis: A Retrospective Study. Diagn. Microbiol. Infect. Dis. 2022, 104, 115767. [Google Scholar] [CrossRef]
- Osbak, K.; Abdellati, S.; Tsoumanis, A.; Van Esbroeck, M.; Kestens, L.; Crucitti, T.; Kenyon, C. Evaluation of an Automated Quantitative Latex Immunoturbidimetric Non-Treponemal Assay for Diagnosis and Follow-up of Syphilis: A Prospective Cohort Study. J. Med. Microbiol. 2017, 66, 1130–1139. [Google Scholar] [CrossRef]
- Wu, Y.; Zhu, W.; Sun, C.; Yue, X.; Zheng, M.; Fu, G.; Gong, X. Prevalence of Syphilis among People Living with HIV and Its Implication for Enhanced Coinfection Monitoring and Management in China: A Meta-Analysis. Front. Public Health 2022, 10, 1002342. [Google Scholar] [CrossRef]
- Marchese, V.; Tiecco, G.; Storti, S.; Degli Antoni, M.; Calza, S.; Gulletta, M.; Viola, F.; Focà, E.; Matteelli, A.; Castelli, F.; et al. Syphilis Infections, Reinfections and Serological Response in a Large Italian Sexually Transmitted Disease Centre: A Monocentric Retrospective Study. J. Clin. Med. 2022, 11, 7499. [Google Scholar] [CrossRef]
- Sena, A.C.; Wolff, M.; Martin, D.H.; Behets, F.; Van Damme, K.; Leone, P.; Langley, C.; McNeil, L.; Hook, E.W. Predictors of Serological Cure and Serofast State After Treatment in HIV-Negative Persons With Early Syphilis. Clin. Infect. Dis. 2011, 53, 1092–1099. [Google Scholar] [CrossRef]
- Ramos, A.N., Jr. Persistence of Syphilis as a Challenge for the Brazilian Public Health: The Solution Is to Strengthen SUS in Defense of Democracy and Life. Cad. Saúde Pública 2022, 38, PT069022. [Google Scholar] [CrossRef]
- Shukla, M.R.; Pereira, L.; Gaynor, A.M.; Sun, Y.; Edwards, D.; Simmons, T.; Andrews, C.W.; Park, I.U.; Hong, J.; Cao, W.; et al. Evaluation of Three Automated Nontreponemal Rapid Plasma Reagin (RPR) Tests for the Laboratory Diagnosis of Syphilis. J. Clin. Microbiol. 2023, 61, e00168-23. [Google Scholar] [CrossRef]
- Singhal, N.; Kumar, M.; Kanaujia, P.K.; Virdi, J.S. MALDI-TOF Mass Spectrometry: An Emerging Technology for Microbial Identification and Diagnosis. Front. Microbiol. 2015, 6, 791. [Google Scholar] [CrossRef]
- Douglas, J.M. Penicillin Treatment of Syphilis. JAMA 2009, 301, 769. [Google Scholar] [CrossRef] [PubMed]
- Janier, M.; Unemo, M.; Dupin, N.; Tiplica, G.S.; Potočnik, M.; Patel, R. 2020 European Guideline on the Management of Syphilis. J. Eur. Acad. Dermatol. Venereol. 2021, 35, 574–588. [Google Scholar] [CrossRef] [PubMed]
- Silverberg, B.; Moyers, A.; Hinkle, T.; Kessler, R.; Russell, N.G. 2021 CDC Update: Treatment and Complications of Sexually Transmitted Infections (STIs). Venereology 2022, 1, 23–46. [Google Scholar] [CrossRef]
- Katanami, Y.; Hashimoto, T.; Takaya, S.; Yamamoto, K.; Kutsuna, S.; Takeshita, N.; Hayakawa, K.; Kanagawa, S.; Ohmagari, N. Amoxicillin and Ceftriaxone as Treatment Alternatives to Penicillin for Maternal Syphilis. Emerg. Infect. Dis. 2017, 23, 827–829. [Google Scholar] [CrossRef]
- Bolan, R.K.; Beymer, M.R.; Weiss, R.E.; Flynn, R.P.; Leibowitz, A.A.; Klausner, J.D. Doxycycline Prophylaxis to Reduce Incident Syphilis among HIV-Infected Men Who Have Sex With Men Who Continue to Engage in High-Risk Sex. Sex. Transm. Dis. 2015, 42, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Fan, Y.; Chen, J.; Yang, J.; Gao, L.; Wu, X.; Xu, X.; Zhang, Y.; Yue, P.; Cao, W.; et al. Efficacy and Safety of Treatments for Different Stages of Syphilis: A Systematic Review and Network Meta-Analysis of Randomized Controlled Trials and Observational Studies. Microbiol. Spectr. 2022, 10, e02977-22. [Google Scholar] [CrossRef]
- Hamill, M.M.; Onzia, A.; Wang, T.-H.; Kiragga, A.N.; Hsieh, Y.-H.; Parkes-Ratanshi, R.; Gough, E.; Kyambadde, P.; Melendez, J.H.; Manabe, Y.C. High Burden of Untreated Syphilis, Drug Resistant Neisseria Gonorrhoeae, and Other Sexually Transmitted Infections in Men with Urethral Discharge Syndrome in Kampala, Uganda. BMC Infect. Dis. 2022, 22, 440. [Google Scholar] [CrossRef]
- Grant, J.S.; Stafylis, C.; Celum, C.; Grennan, T.; Haire, B.; Kaldor, J.; Luetkemeyer, A.F.; Saunders, J.M.; Molina, J.-M.; Klausner, J.D. Doxycycline Prophylaxis for Bacterial Sexually Transmitted Infections. Clin. Infect. Dis. 2020, 70, 1247–1253. [Google Scholar] [CrossRef]
- Stamm, L.V. Hope for New Antibiotics for Syphilis Treatment. EBioMedicine 2021, 66, 103320. [Google Scholar] [CrossRef]
- Haynes, A.M.; Giacani, L.; Mayans, M.V.; Ubals, M.; Nieto, C.; Pérez-Mañá, C.; Quintó, L.; Romeis, E.; Mitjà, O. Efficacy of Linezolid on Treponema Pallidum, the Syphilis Agent: A Preclinical Study. EBioMedicine 2021, 65, 103281. [Google Scholar] [CrossRef]
- Katz, K.A.; Klausner, J.D. Azithromycin Resistance in Treponema Pallidum. Curr. Opin. Infect. Dis. 2008, 21, 83–91. [Google Scholar] [CrossRef]
- Chen, X.-S.; Yin, Y.-P.; Wei, W.-H.; Wang, H.-C.; Peng, R.-R.; Zheng, H.-P.; Zhang, J.-P.; Zhu, B.-Y.; Liu, Q.-Z.; Huang, S.-J. High Prevalence of Azithromycin Resistance to Treponema Pallidum in Geographically Different Areas in China. Clin. Microbiol. Infect. 2013, 19, 975–979. [Google Scholar] [CrossRef]
- Orbe-Orihuela, Y.C.; Sánchez-Alemán, M.Á.; Hernández-Pliego, A.; Medina-García, C.V.; Vergara-Ortega, D.N. Syphilis as Re-Emerging Disease, Antibiotic Resistance, and Vulnerable Population: Global Systematic Review and Meta-Analysis. Pathogens 2022, 11, 1546. [Google Scholar] [CrossRef]
- Cameron, C.E.; Lukehart, S.A. Current Status of Syphilis Vaccine Development: Need, Challenges, Prospects. Vaccine 2014, 32, 1602–1609. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.N. Immunity in Experimental Syphilis. J. Immunol. 1973, 110, 1206–1215. [Google Scholar] [CrossRef] [PubMed]
- Vickram, A.S.; Dhama, K.; Thanigaivel, S.; Chakraborty, S.; Anbarasu, K.; Dey, N.; Karunakaran, R. Strategies for Successful Designing of Immunocontraceptive Vaccines and Recent Updates in Vaccine Development against Sexually Transmitted Infections—A Review. Saudi J. Biol. Sci. 2022, 29, 2033–2046. [Google Scholar] [CrossRef]
- Ávila-Nieto, C.; Pedreño-López, N.; Mitjà, O.; Clotet, B.; Blanco, J.; Carrillo, J. Syphilis Vaccine: Challenges, Controversies and Opportunities. Front. Immunol. 2023, 14, 1126170. [Google Scholar] [CrossRef]
- Xu, M.; Xie, Y.; Zheng, K.; Luo, H.; Tan, M.; Zhao, F.; Zeng, T.; Wu, Y. Two Potential Syphilis Vaccine Candidates Inhibit Dissemination of Treponema Pallidum. Front. Immunol. 2021, 12, 759474. [Google Scholar] [CrossRef]
- Cameron, C.E. Syphilis Vaccine Development: Requirements, Challenges, and Opportunities. Sex. Transm. Dis. 2018, 45, S17–S19. [Google Scholar] [CrossRef] [PubMed]
- Kojima, N.; Konda, K.A.; Klausner, J.D. Notes on Syphilis Vaccine Development. Front. Immunol. 2022, 13, 952284. [Google Scholar] [CrossRef]
- Cullen, P.A.; Cameron, C.E. Progress towards an Effective Syphilis Vaccine: The Past, Present and Future. Expert Rev. Vaccines 2006, 5, 67–80. [Google Scholar] [CrossRef]
- Ambrose, C.T. Vaccines and the Looming Threat of Syphilis. Glob. Vaccines Immunol. 2015, 1, 8–13. [Google Scholar] [CrossRef][Green Version]
- Giacani, L. Strategies for Syphilis Vaccine Development. J. Bras. Doenças Sex. Transm. 2022, 34, e22341249. [Google Scholar] [CrossRef]
- Pham, M.D.; Ong, J.J.; Anderson, D.A.; Drummer, H.E.; Stoové, M. Point-of-Care Diagnostics for Diagnosis of Active Syphilis Infection: Needs, Challenges and the Way Forward. Int. J. Environ. Res. Public Health 2022, 19, 8172. [Google Scholar] [CrossRef] [PubMed]
- Mabey, D.C.; Sollis, K.A.; Kelly, H.A.; Benzaken, A.S.; Bitarakwate, E.; Changalucha, J.; Chen, X.-S.; Yin, Y.-P.; Garcia, P.J.; Strasser, S.; et al. Point-of-Care Tests to Strengthen Health Systems and Save Newborn Lives: The Case of Syphilis. PLoS Med. 2012, 9, e1001233. [Google Scholar] [CrossRef]
- Causer, L.M.; Kaldor, J.M.; Conway, D.P.; Leslie, D.E.; Denham, I.; Karapanagiotidis, T.; Ryan, C.; Wand, H.; Anderson, D.A.; Robertson, P.W.; et al. An Evaluation of a Novel Dual Treponemal/Nontreponemal Point-of-Care Test for Syphilis as a Tool to Distinguish Active From Past Treated Infection. Clin. Infect. Dis. 2015, 61, 184–191. [Google Scholar] [CrossRef]
- Caya, C.; Maheu-Giroux, M.; Xia, Y.; Serhir, B.; Morin, V.; Libman, M.; Corsini, R.; Goldfarb, D.M.; Wong, T.; Singh, A.E.; et al. Stopping Syphilis Transmission in Arctic Communities through Rapid Diagnostic Testing: The STAR Study Protocol. PLoS ONE 2022, 17, e0273713. [Google Scholar] [CrossRef]
- Toskin, I.; Blondeel, K.; Peeling, R.W.; Deal, C.; Kiarie, J. Advancing Point of Care Diagnostics for the Control and Prevention of STIs: The Way Forward. Sex. Transm. Infect. 2017, 93, S81–S88. [Google Scholar] [CrossRef]
- Basing, L.A.W.; Simpson, S.V.; Adu-Sarkodie, Y.; Linnes, J.C. A Loop-Mediated Isothermal Amplification Assay for the Detection of Treponema Pallidum Subsp. Pertenue. Am. J. Trop. Med. Hyg. 2020, 103, 253–259. [Google Scholar] [CrossRef]
- Tharakan, S.; Faqah, O.; Asghar, W.; Ilyas, A. Microfluidic Devices for HIV Diagnosis and Monitoring at Point-of-Care (POC) Settings. Biosensors 2022, 12, 949. [Google Scholar] [CrossRef]
- Christodouleas, D.C.; Kaur, B.; Chorti, P. From Point-of-Care Testing to EHealth Diagnostic Devices (EDiagnostics). ACS Cent. Sci. 2018, 4, 1600–1616. [Google Scholar] [CrossRef]
- Naeem, F.; Karellis, A.; Nair, S.; Routy, J.-P.; Yansouni, C.P.; Kim, J.; Pai, N. Multiplexed Technologies for Sexually Transmitted Infections: Global Evidence on Patient-Centered and Clinical Health Outcomes. BMJ Glob. Health 2021, 6, e005670. [Google Scholar] [CrossRef]
- Karellis, A.; Naeem, F.; Nair, S.; Mallya, S.D.; Routy, J.-P.; Gahagan, J.; Yansouni, C.P.; Kim, J.; Pai, N.P. Multiplexed Rapid Technologies for Sexually Transmitted Infections: A Systematic Review. Lancet Microbe 2022, 3, e303–e315. [Google Scholar] [CrossRef]
- Osbak, K.K.; Van Raemdonck, G.A.; Dom, M.; Cameron, C.E.; Meehan, C.J.; Deforce, D.; Ostade, X.V.; Kenyon, C.R.; Dhaenens, M. Candidate Treponema Pallidum Biomarkers Uncovered in Urine from Individuals with Syphilis Using Mass Spectrometry. Future Microbiol. 2018, 13, 1497–1510. [Google Scholar] [CrossRef]
- Wang, C.; Liu, M.; Wang, Z.; Li, S.; Deng, Y.; He, N. Point-of-Care Diagnostics for Infectious Diseases: From Methods to Devices. Nano Today 2021, 37, 101092. [Google Scholar] [CrossRef] [PubMed]
- Valentine, J.A.; Bolan, G.A. Syphilis Elimination: Lessons Learned Again. Sex. Transm. Dis. 2018, 45, S80–S85. [Google Scholar] [CrossRef] [PubMed]
- Peterman, T.A.; Cha, S. Context-Appropriate Interventions to Prevent Syphilis: A Narrative Review. Sex. Transm. Dis. 2018, 45, S65–S71. [Google Scholar] [CrossRef] [PubMed]
- Copen, C.E.; Rushmore, J.; De Voux, A.; Kirkcaldy, R.D.; Fakile, Y.F.; Tilchin, C.; Duchen, J.; Jennings, J.M.; Spahnie, M.; Norris Turner, A.; et al. Factors Associated With Syphilis Transmission and Acquisition Among Men Who Have Sex With Men: Protocol for a Multisite Egocentric Network Study. JMIR Res. Protoc. 2022, 11, e40095. [Google Scholar] [CrossRef] [PubMed]
- Welch, J. Antenatal Screening for Syphilis. BMJ 1998, 317, 1605–1606. [Google Scholar] [CrossRef][Green Version]
- Paiva, J.C.D.L.; Dias-Trindade, S.; Gonzalez, M.O.A.; Barros, D.M.D.S.; Cardoso, P.H.; Bezerra, P.H.C.; Lima, T.G.F.D.M.S.; Lacerda, J.D.S.; Muneiro, L.C.; Cunha-Oliveira, A.; et al. Analysis of the Impact of Communication Campaigns under the Project “Syphilis No”: A National Tool for Inducing and Promoting Health. Int. J. Environ. Res. Public Health 2022, 19, 15884. [Google Scholar] [CrossRef]
- Nguyen, S.H.; Dang, A.K.; Vu, G.T.; Nguyen, C.T.; Le, T.H.T.; Truong, N.T.; Hoang, C.L.; Tran, T.T.; Tran, T.H.; Pham, H.Q.; et al. Lack of Knowledge about Sexually Transmitted Diseases (STDs): Implications for STDs Prevention and Care among Dermatology Patients in an Urban City in Vietnam. Int. J. Environ. Res. Public Health 2019, 16, 1080. [Google Scholar] [CrossRef] [PubMed]
- Valentine, J.A.; Delgado, L.F.; Haderxhanaj, L.T.; Hogben, M. Improving Sexual Health in U.S. Rural Communities: Reducing the Impact of Stigma. AIDS Behav. 2022, 26, 90–99. [Google Scholar] [CrossRef]
- Grieb, S.M.; Jackman, K.-M.; Jennings, J.M. Recommendations From Black Sexual Minority Men: Building Trust to Improve Engagement and Impact of HIV/STI Research. Health Promot. Pract. 2021, 22, 395–403. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira Saes, M.; Duro, S.M.S.; de Souza Gonçalves, C.; Tomasi, E.; Facchini, L.A. Assessment of the Appropriate Management of Syphilis Patients in Primary Health Care in Different Regions of Brazil from 2012 to 2018. Cad. Saúde Pública 2022, 38, EN231921. [Google Scholar] [CrossRef]
- Santos, M.M.D.; Rosendo, T.M.S.D.S.; Lopes, A.K.B.; Roncalli, A.G.; Lima, K.C.D. Weaknesses in Primary Health Care Favor the Growth of Acquired Syphilis. PLoS Negl. Trop. Dis. 2021, 15, e0009085. [Google Scholar] [CrossRef]
- van Weel, C.; Kidd, M.R. Why Strengthening Primary Health Care Is Essential to Achieving Universal Health Coverage. Can. Med. Assoc. J. 2018, 190, E463–E466. [Google Scholar] [CrossRef]
- McCormack, H.; Guy, R.; Bourne, C.; Newman, C.E. Integrating Testing for Sexually Transmissible Infections into Routine Primary Care for Aboriginal Young People: A Strengths-based Qualitative Analysis. Aust. N. Z. J. Public Health 2022, 46, 370–376. [Google Scholar] [CrossRef] [PubMed]
- Guedes, A.L.d.L.; Guimarães, D.C.d.S.; Sarkis, D.J.; Gabriel, T.T.; Delgado, C.S.; Campos, A.A.L.; Nogueira, M.C.; Ribeiro, L.C. Factors Associated with Women Diagnosed with Syphilis Who Received Prenatal Care in a Primary Healthcare Unit. Einstein (São Paulo) 2023, 31, eAO0046. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fajemiroye, J.O.; Moreira, A.L.E.; Ito, C.R.M.; Costa, E.A.; Queiroz, R.M.; Ihayi, O.J.; Moreira, C.V.; Costa, R.F.; Teixeira, C.C.; Bortolini, M.J.S.; et al. Advancing Syphilis Research: Exploring New Frontiers in Immunology and Pharmacological Interventions. Venereology 2023, 2, 147-163. https://doi.org/10.3390/venereology2040013
Fajemiroye JO, Moreira ALE, Ito CRM, Costa EA, Queiroz RM, Ihayi OJ, Moreira CV, Costa RF, Teixeira CC, Bortolini MJS, et al. Advancing Syphilis Research: Exploring New Frontiers in Immunology and Pharmacological Interventions. Venereology. 2023; 2(4):147-163. https://doi.org/10.3390/venereology2040013
Chicago/Turabian StyleFajemiroye, James Oluwagbamigbe, Andre Luis Elias Moreira, Célia Regina Malveste Ito, Elson Alves Costa, Rafaella Misael Queiroz, Ogbu John Ihayi, Caroline Vitória Moreira, Rafael Fernandes Costa, Claudia Carneiro Teixeira, Miguel Júnior Sordi Bortolini, and et al. 2023. "Advancing Syphilis Research: Exploring New Frontiers in Immunology and Pharmacological Interventions" Venereology 2, no. 4: 147-163. https://doi.org/10.3390/venereology2040013
APA StyleFajemiroye, J. O., Moreira, A. L. E., Ito, C. R. M., Costa, E. A., Queiroz, R. M., Ihayi, O. J., Moreira, C. V., Costa, R. F., Teixeira, C. C., Bortolini, M. J. S., & Silva, O. N. (2023). Advancing Syphilis Research: Exploring New Frontiers in Immunology and Pharmacological Interventions. Venereology, 2(4), 147-163. https://doi.org/10.3390/venereology2040013