Abstract
Background: Efforts to increase acceptance and reduce avoidance behaviors in patients who suffer from chronic pain are likely to have additional beneficial effects on pain management. The primary aim of the current study was to evaluate whether a sequential approach to treatment, where acceptance-based coping strategies are taught prior to problem-focused coping strategies using manualized group therapies, improves pain-related outcomes. Methods: The current investigation is a single-group, longitudinal ex post facto study. A sample of 168 Veterans participated in the current study at a midwestern VA medical center. All participants were administered a standard pre- and post-intervention assessment battery. The primary outcome analysis was a 4 × 2 repeated-measures multivariate analysis of variance. Results: The current study did not find a significant interaction effect for intervention x time but did find a significant main effect for time. All treatment conditions were associated with decreases in pain severity, pain interference, illness-focused coping strategies, catastrophizing behaviors, and global distress. Participation in both of the combined groups did not produce significantly different pain-related outcomes compared to participation in one group. Conclusion: These findings reinforce common factors theory in psychotherapy and provide insight into treatment dosage for patients who suffer from chronic pain. The current findings underline the importance of researching pain management, as it is a fundamental aspect of clinical practice, training, and research in rheumatology.
1. Introduction
The previous literature has established the effectiveness of Acceptance and Commitment Therapy (ACT) and Cognitive-Behavioral Therapy (CBT) in the treatment of chronic pain among different populations, including Veterans [1]. As part of their efforts toward the dissemination of empirically-based practices, the Department of Veterans Affairs (VA) is committed to making treatments such as ACT and CBT widely available to Veterans with mental and behavioral health conditions [2]. Prior studies comparing ACT [3,4,5,6,7,8] and CBT [9,10,11,12,13,14] for chronic pain have found both treatments to be effective in decreasing pain intensity, disability, distress, pain interference, and catastrophizing, with little to no significant differences in improvements noted between treatments [1,15,16].
The results of these past studies affirm aspects of the foundational knowledge of psychological intervention. Originally proposed by Saul Rosenzweig [17], common factors theory of psychotherapy suggests that psychotherapy outcomes depend on a set of factors that are common to all treatment modalities, as opposed to those that are specific to a particular treatment. Based on studies across a variety of contexts, Wampold [18] presented an update summarizing the evidence supporting both common and specific factors in psychotherapy and concluded, again, that common factors, such as therapist–patient alliance (including goal consensus/collaboration) and patient expectations of treatment, are essential to psychotherapy outcome. However, there remains a need to understand how to optimally implement these treatments to improve patient outcomes related to pain management and whether an adaptive or sequential treatment strategy may be effective toward this goal.
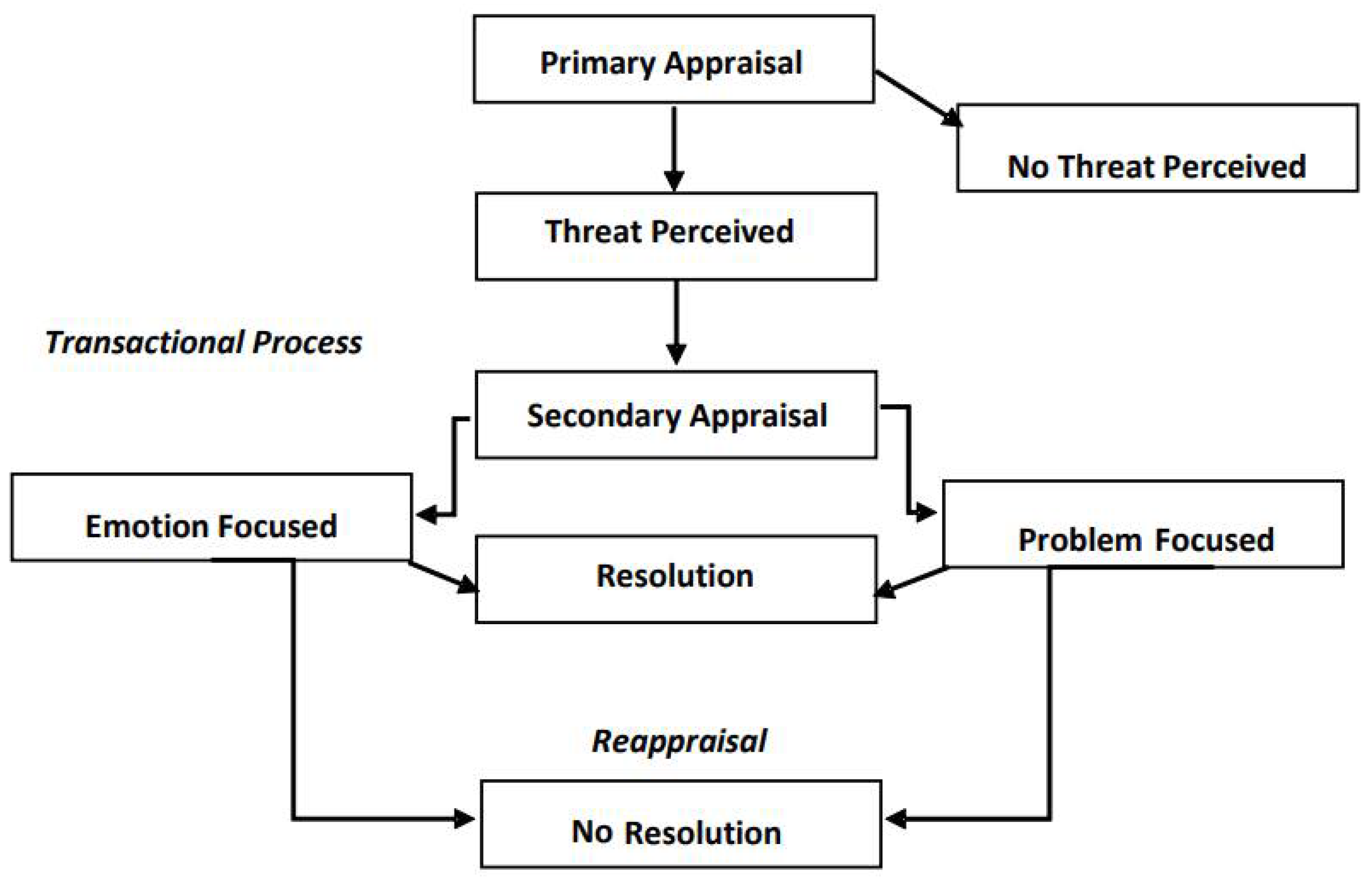
Transactional Model of Stress and Coping. With the transactional theory of stress and coping, Lazarus [19] proposed that a person’s appraisal of a stressor and their ability to cope with the stressor lie at the center of the stress experience. Once a stressor has been evaluated to be threatening, individuals undergo a specific process of cognitive appraisal to evaluate whether they have the resources to effectively manage the stressor, which will then determine what coping strategies are employed. Folkman and Lazarus [20] differentiated emotion-focused and problem-focused coping strategies, proposing that individuals will rely on emotion-focused coping responses if they feel a lack of control over the situation but will turn to problem-focused coping responses if they believe they have the resources to manage the challenge (see Figure 1). Walinga [21] expanded on the application of this theory and described how changes in an individual’s primary appraisal of a stressor (through reappraisal) may impact the individual’s response. Individuals were more likely to generate creative solutions to a change or stressor and, thus, cope more effectively, when it was perceived as non-threatening, compared to when it was perceived as threatening [21].
Figure 1.
Transactional Model of Stress and Coping.
This has important implications for a patient who suffers from chronic pain. In this context, “pain” is the stressor, which may be perceived either as threatening or non-threatening. For many patients with chronic pain, pain is perceived as a threatening stressor, for which individuals must determine whether they have the resources to cope or manage. If individuals perceive that their pain is out of their control, according to Folkman and Lazarus [20], they will engage in emotion-focused coping strategies such as distancing, wishful thinking, or emphasizing the positive. ACT may be used to impart emotion-focused skills that can ultimately lead to reappraisal. If, on the other hand, individuals perceive that they do have the resources to manage their pain effectively, they are likely to employ a problem-focused approach to coping, such as analyzing the problem and finding a solution. CBT may be used to impart problem-focused coping skills that can ultimately lead to reappraisal. However, based on Walinga’s [21] findings, if a patient who suffers from chronic pain can develop an alternative primary appraisal of the pain, such that it is viewed as non-threatening, they are more likely to find creative solutions to managing their pain. Taken together, these two theories provide support for an approach to chronic pain treatment that first facilitates the development of acceptance-based coping strategies and supplements them with problem-focused approaches for managing chronic pain.
Building Acceptance. There is some evidence to suggest that emotion-focused coping strategies, such as acceptance, may be most effective when applied as a complement to problem-focused coping skills. For instance, although individuals are more likely to apply problem-focused coping strategies when they perceive a higher level of control over a particular situation, an increase in acceptance-based coping strategies, regardless of the controllability of the situation, has been associated with decreases in negative affect [22]. In the context of chronic pain, negative affect has been associated with increases in pain severity, pain interference, neuroinflammation, and opioid misuse, suggesting that negative affect remains an important target for chronic pain management [23,24,25]. However, negative life events have also been shown to have a graded association with psychosocial distress, pain severity, suicidal ideation, and the use of maladaptive pain-coping strategies, including rumination, helplessness, and decreased acceptance [26,27]. For individuals with higher numbers of self-reported negative life events, acceptance-based interventions aimed at improving strategies for coping with pain are, thus, likely to be beneficial toward reducing distress. This is particularly relevant among Veteran populations, who may experience high levels of negative life events prior, during, and after their time in the military.
In a study on the effects of CBT for chronic pain, participants who reported higher degrees of pre-treatment acceptance of their condition were shown to experience larger pain reductions than those who were less accepting of their condition [28]. This finding is consistent with the previous literature, which found that acceptance accounted for more variance in functional disability and pain in patients who suffer from chronic pain than other cognitive-behavioral factors [29]. Moreover, avoidance behaviors have been associated with increases in depression, helplessness, and increased medication consumption [28]. Therefore, efforts to increase acceptance and reduce avoidance behaviors in patients who suffer from chronic pain are likely to have beneficial effects on pain management, regardless of the modality of the treatment being administered.
The purpose of this study is to examine the implications of sequencing order of two evidence-based group psychotherapies, ACT and CBT, on chronic pain in Veterans. The primary aim of this study is to assess whether the primary and secondary outcomes related to chronic pain differ as a product of the sequencing order of group psychotherapy treatment. Based on the focus of ACT treatment on emotion-focused coping and radical acceptance, we hypothesize that participants receiving ACT prior to CBT for chronic pain will report greater improvements on outcome measures related to pain interference and pain severity than those receiving CBT before ACT. As a basis for evaluating the effects of sequencing order, we will also be testing the hypothesis that Veterans receiving both treatments will show a significantly greater improvement in pain-outcome measures than those receiving just one of the treatments.
2. Materials and Methods
2.1. Participants
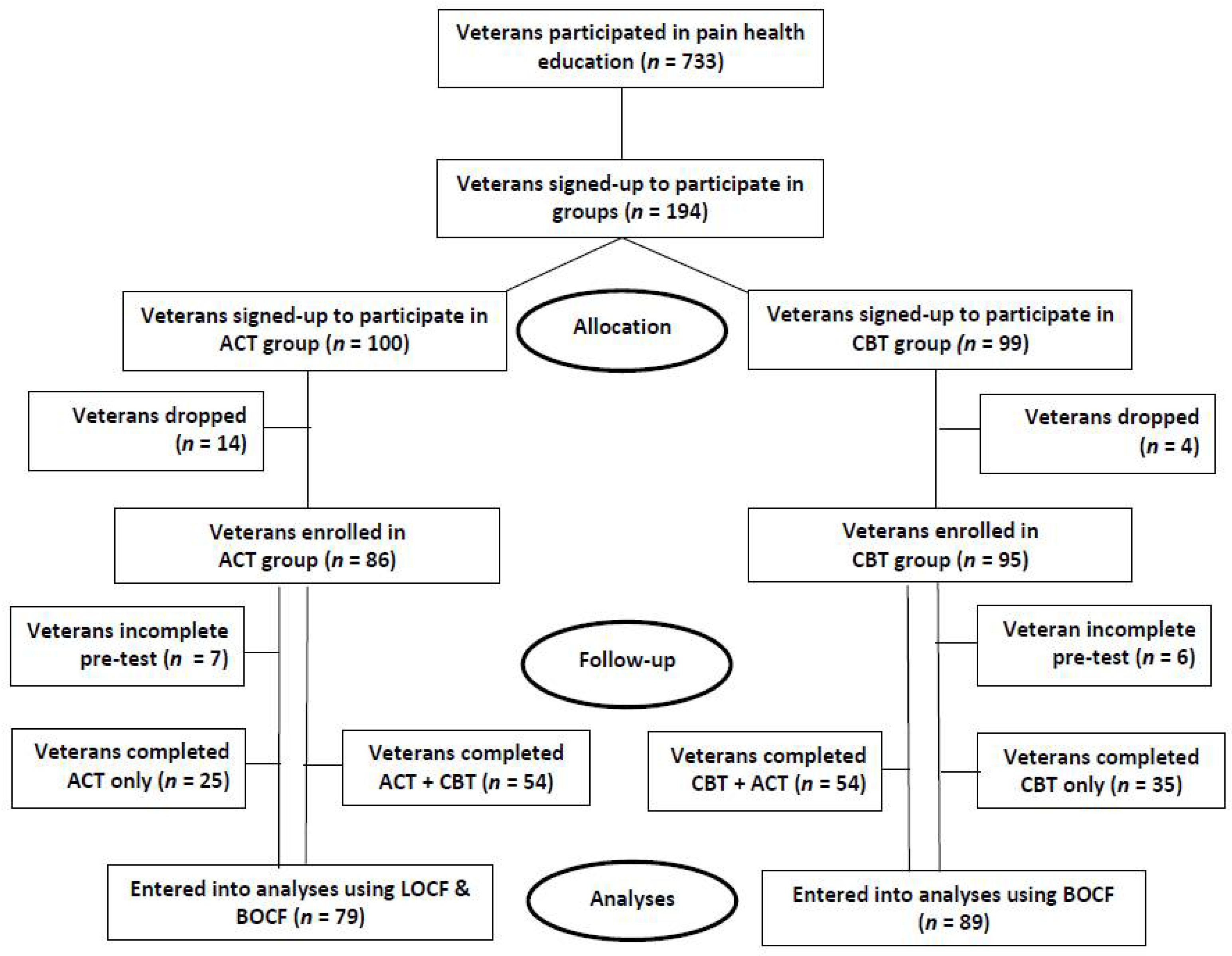
One hundred ninety-four Veterans self-selected to participate in pain groups at a midwestern VA medical center between 1 November 2009 and 30 November 2012. Those who dropped out of treatment or whose pre-test measures were not completed were excluded from the study, leaving 168 valid cases for analysis (see Figure 2). Four conditions were evaluated in this study: 15% of participants completed ACT only (n = 25), 21% completed CBT only (n = 35), 32% completed ACT prior to CBT (n = 54), and 32% completed CBT prior to ACT (n = 54). The participants were predominately African American (80%); of the remainder, 16% identified as Caucasian, and 4% identified as Hispanic/Latino. Most of the participants were male (83%), with a small sample of females (17%). The largest proportion of participants was between the ages of 45–64 (73%), and Veterans above age 75 were the least represented (4%). There were no exclusion criteria used for the study; Veterans diagnosed with psychosis, mania, and substance abuse were included in the real-world interventions.
Figure 2.
Flowchart of study participants.
2.2. Procedure
Veterans enrolled in a pre-treatment process, a health education program at a midwestern VA medical center, were then given the opportunity to elect to participate in ACT and CBT group interventions for chronic pain. During the health education program, Veterans learned about the 23 different modalities of chronic pain management offered by the hospital, including ACT and CBT treatments. Veterans were specifically informed about key points related to both treatments, including that ACT is (1) highly experiential and patients’ success depends on how much they put into it; (2) an opportunity for patients to learn and practice new and more flexible ways of responding when they experience pain; (3) for patients to learn ways of no longer letting pain be in the way of doing what they want to do; and (4) about changing how patients relate with themselves about living better. They also learned that CBT is (1) based on the notion that pain is a complex physical experience that is influenced by an individual’s cognitions, affect, and behavior [30,31]; and (2) about providing an opportunity for Veterans to learn, apply, and maintain new coping skills [32].
Upon learning about the ACT and CBT interventions, Veterans were free to choose which treatment to pursue. Each Veteran was subsequently scheduled for 10 weeks of one-hour ACT or 12 weeks of one-hour CBT group treatment. After completing the first intervention (ACT or CBT), the Veterans could then elect to be scheduled for the alternative group or to discontinue treatment (see Figure 2). Groups were held weekly, with the exception of holidays. Veterans voluntarily participated in the pain-management groups and were free to withdraw at any time. Participants were given free parking validation or transportation reimbursement, if they were in attendance and qualified for such programs. The current study included 14 cohorts of the ACT group and 12 cohorts of the CBT group. Groups were co-led by three different licensed clinical psychologists, with training in the respective treatment modality (ACT or CBT), and one of eight different psychology trainees. The current study protocol was reviewed and approved by the affiliated university’s Institutional Review Board (IRB) and the VA’s Research & Development office. A waiver of informed consent was granted due to the retrospective nature of the study and the minimal risk to subjects who participated.
2.3. Interventions
Acceptance and Commitment Therapy (ACT). ACT group treatment for chronic pain utilizes acceptance, mindfulness, commitment, and behavior-change strategies to increase psychological flexibility related to chronic pain. Broadly, ACT treatment involves experiential exercises related to six core processes to effect change: willingness to accept a range of experiences, engagement with the present moment, observing of the self, defusion from thoughts, identifying values, and committing to values-aligned action. The ACT for chronic pain group protocol in the current study was based upon an amalgamation of existing ACT treatment manuals [33,34,35] and has been shared in the literature [36].
Cognitive-Behavioral Therapy (CBT). CBT group treatment for chronic pain is a structured, present-focused therapy that helps patients modify dysfunctional thinking patterns and maladaptive behaviors to resolve pain-related problems. CBT for chronic pain includes psychoeducation about pain, thinking skills (e.g., cognitive restructuring), behavioral skills (e.g., relaxation strategies), time-based-activity pacing, and pleasant-activities scheduling. The CBT for chronic pain group protocol in the current study was based upon an existing CBT treatment manual [37].
2.4. Outcome Measures
As part of the introduction and conclusion of each intervention, all participants completed a set of pre- and post-intervention standard assessments. The battery of measures in the current study included the Readiness Questionnaire (M. Jensen, personal communication, August 23, 2004), the Brief Pain Inventory-Short Form (BPI) [38], the Oswestry Disability Index (ODI) [39], the Coping Strategies Questionnaire–Catastrophizing Scale (CSQ) [40], the Chronic Pain Coping Inventory–Short Form (CPCI) [41], and the Brief Symptom Inventory 18 (BSI-18) [42]. These measures were chosen based on their brevity and ease of administration as well as their reliability and validity in prior research.
Readiness Questionnaire. Participants were asked to select one out of five statements that best described their stage of readiness to adopt a self-management approach to their pain. Scores ranged from “1” to “5”, with larger numbers indicating a more advanced stage of readiness to adopt a self-management approach to their pain. Test–retest reliability for this item in previous research was 0.63 [43]. The test–retest reliability of this item for the current study was 0.479, which is considered unacceptable. Thus, the instrument was eliminated from the outcome analysis due to poor temporal stability.
Brief Pain Inventory–Short Form (BPI). The BPI asks participants to rate their pain at the time of responding to the questionnaire (pain severity right now) and at its worst, least, and average over the previous 24 h. The BPI also asks for ratings of the degree to which pain interferes with mood, walking and other physical activity, work, social activity, relations with others, and sleep. The internal consistency of the BPI, in past research, ranged from α = 0.80 to 0.87 for pain severity and from α = 0.89 to 0.92 for pain interference. Cronbach’s alpha for the current study was α = 0.851 for pain severity and α = 0.891 for pain interference. Permission has been obtained to use the BPI in a publication and research trial.
BPI–Numeric Rating Scale. In previous studies, one item from the BPI has been used to measure a respondent’s pain in the moment by asking participants to: “Please rate your pain by circling the one number that tells how much pain you have RIGHT NOW” on an 11-point scale from 0–10. The test–retest reliability of this item for the current study was 0.635, which is considered questionable. Therefore, for this study, pain severity is measured using a composite score comprised of pain right now, worst pain, least pain, and average pain over the last 24 h. Cronbach’s alpha for the pain-severity composite score in the current study was α = 0.851.
Oswestry Disability Index (ODI). The ODI is used to measure a participant’s permanent functional disability. The ODI consists of 10 questions for which the participant selects the best answer that describes their typical pain and/or limitations within the last two weeks. The test has been around for 25 years and is considered the gold standard of functional outcome tools. The internal consistency of the ODI in past research was α = 0.85. Cronbach’s alpha for the current study was α = 0.852. Permission has been obtained to use the ODI in a publication and research trial from MAPI Research Trust.
Coping Strategies Questionnaire–Catastrophizing Scale (CSQ). The CSQ uses a “0–5” Likert scale to rate five statements that measure negative self-statements, catastrophizing thoughts, and ideations about their pain. Data analysis has revealed that the Catastrophizing Scale was internally reliable (α = 0.82) and had high test–retest reliability over 6 months. Cronbach’s alpha for the current study was α = 0.867.
Chronic Pain Coping Inventory–Short Form (CPCI). Eight strategies for coping with chronic pain were assessed using the 16-item short form of the CPCI, which were illness-focused (such as guarding, resting, and asking for assistance) and wellness-focused (such as exercise/stretching, relaxation, task persistence, seeking social support, and coping self-statements). The instructions to participants specifically state, “During the past week (past 7 days) how many days did you use each of the following at least once in the day to cope with your pain? Please include days when you used the coping strategy to prevent or minimize pain, even if you did not have pain at that time.” The validity of the short form of the CPCI has previously been established by correlations with the subscales of the 65-item version and measures of pain and pain-related function. The median internal consistency for the CPCI ranges from α = 0.70 to 0.94. Cronbach’s alpha for the current study was α = 0.861.
Brief Symptom Inventory 18 (BSI-18). The BSI-18 requires participants to rate their level of distress over the past 7 days using a 5-point Likert scale. The BSI-18 provides subscale scores, including a score on global distress (calculated based on all 18 items). The internal consistency of the BSI was reported to be α = 0.89. Cronbach’s alpha for the current study was α = 0.941. Permission to use the BSI-18 is inherent for the qualified purchase of the test materials.
2.5. Analytic Methods
The current investigation is a single-group, longitudinal ex post facto study. A one-way analysis of variance (ANOVA) identified differences on demographic and outcome variables at baseline. The primary outcome analysis was a 4 × 2 repeated measures (RM) multivariate analysis of variance (MANOVA), with “Intervention Condition” as the between-subjects factor and “Time” as the within-subjects factor. The dependent variables were the primary outcome variables of pain severity and interference, and the secondary variables of disability, catastrophizing, illness- and wellness-focused coping strategies, and global distress. Outcome studies used an efficacy subset analysis strategy, which selects the subset of the patients who received the intended programming and who did not drop out for any reason. A power analysis was calculated with a 4 × 2 design, an anticipated effect size of Cohen’s d = 0.20 (n2 = 0.01), and p ≤ 0.05, at both 70% and 80% power. For 70% power, the minimum total sample size was n = 173, and the sample size per treatment cell was n = 43; for 80% power, the minimum total sample size was n = 201, and the sample size per treatment cell was n = 50. The effect size used was low because past meta-analyses suggest that the difference between a psychological treatment and a treatment-as-usual control group is relatively small [44]. A last-observation-carried-backward approach was used for missing pre-intervention assessment data, and a baseline-observation-carried-forward approach was used for missing post-intervention assessment data [45,46]. These conservative methods allow for the analysis of the data, by treating missing data as if the past had continued unchanged. SPSS version 25 was used for all outcome analyses. The results are presented using Transparent Reporting of Evaluations with Non-Randomized Designs guidelines [47].
3. Results
3.1. Baseline Characteristics
Veterans had mixed idiopathic chronic pain conditions, with 62% reporting “trunk/abdomen/back/buttock” pain and 61% reporting “legs/thighs/feet” pain, according to the diagrams on the BPI. At baseline, the reported pain score now for all participants was “5.94” (moderate pain), with the average pain score being “6.18”, the worst score being “7.31”, and the least score being “4.92”. On average, participants reported being in the preparation stage (M = 3.2, SD = 1.23) of readiness to adopt a self-management approach, before beginning the intervention. Participants engaged in a moderate level of catastrophizing (M = 13.3, SD = 7.3) and moderate levels of illness-focused (~3.95 days/week) and wellness-focused (~3.6 days/week) coping strategies. At baseline, participants reported poor overall emotional health (M = 25.56, SD = 15.68) at clinical levels, when compared to community norms.
3.2. Differences at Pre-Intervention
In the current study, there were pre-intervention differences between groups based on gender and age cohort which may be associated with initial treatment choice. Consistent with the previous literature, females were found to be less ready to adopt a self-management approach (M = 2.73, SD = 1.28; contemplation stage) at pre-intervention compared to their male counterparts (M = 3.28, SD = 1.22, preparation stage) (see Table 1) [1,48]. There were significant differences at baseline based on age cohort, where younger Veterans were found to report higher levels of catastrophizing, global distress, and pain interference than older Veterans. Although this is consistent with the results of another study involving Veterans [1], an earlier study within the general population found that pain tends to interfere with everyday life increasingly with age [49].

Table 1.
Baseline outcome measure scores by patient characteristics (n = 168).
3.3. Hypothesis 1: ACT vs. CBT
Prior to running the main analysis, a 2 × 2 RM MANOVA was conducted to compare the outcomes between the ACT and CBT interventions. There was no significant interaction effect of “Intervention × Time” (Wilks’ λ = 0.714, F(7, 45) = 0.648), and no significant main effect for “Intervention” (Wilks’ λ = 0.569, F(7, 45) = 0.829). However, there was a significant main effect for “Time” (Wilks’ λ = 0.031, F(7, 45) = 2.46). These results are consistent with a previous study, which showed no difference between ACT and CBT interventions in primary pain outcomes [1].
A significant univariate main effect was obtained for the primary measure of pain interference (F(1, 51) = 8.69, p = 0.005, n2 = 0.15), though not for pain severity (composite) (F(1, 51) = 2.12, p = 0.152). Moreover, significant main effects were obtained for secondary measures of illness-focused coping (F(1, 51) = 6.16, p = 0.016, n2 = 0.11), global distress (F(1, 51) = 9.78, p = 0.003, n2 = 0.16), and catastrophizing (F(1, 51) = 6.97, p = 0.011, n2 = 0.12).
3.4. Hypothesis 2: Sequential Order
The outcome analysis was a 4 × 2 RM MANOVA. There was no significant interaction effect for “Intervention × Time” (Wilks’ λ = 0.969, F(21,419) = 0.504), and no significant main effect for “Intervention” (Wilks’ λ = 0.143, F(21,419) = 1.342). These results indicate that the type of treatment did not produce significantly different outcomes on the dependent variables studied. However, as with the initial analysis comparing ACT vs. CBT, there was a significant main effect for “Time” (Wilks’ λ < 0.001, F(7146) = 4.66), indicating that participants exhibited improvement in at least one of the primary or secondary outcomes studied, as a result of engaging in treatment.
Similar univariate results were obtained for the four-condition analysis, as described above. Significant univariate main effects were obtained for both primary measures of pain severity (F(1152) = 5.02, p = 0.03, n2 = 0.03), and pain interference (F(1152) = 7.75, p = 0.01, n2 = 0.05). In addition, significant main effects were noted for secondary outcome measures of illness-focused coping (F(1152) = 4.58, p = 0.03, n2 = 0.03), global distress (F(1152) = 16.57, p < 0.001, n2 = 0.10), and catastrophizing (F(1152) = 18.98, p < 0.001, n2 = 0.11). There was no significant main effect found for wellness-focused coping (F(1152) = 104.19, p = 0.27), or disability (F(1152) = 1.01, p = 0.32) (see Table 2). These findings largely replicate those from a previous study [1], though the significant effects in pain severity are unique to this study.

Table 2.
Changes in outcome measures by intervention.
4. Discussion
ACT is a third-wave psychotherapy that may compliment traditional CBT therapy by adding other skills, such as mindfulness techniques, acceptance strategies, and value-based work. ACT and CBT also differ in the way they handle maladaptive thinking. CBT works by helping patients identify and change negative or destructive thoughts, while ACT encourages patients to accept all thoughts, good and bad, rather than trying to change them. ACT and CBT are both behavior-based therapies that have been shown to be effective in the treatment of chronic pain in past research. However, practitioners may benefit from understanding how to optimally implement these treatments, whether alone or sequentially, to improve patient outcomes related to pain management.
The results of the current study indicate that patients experienced reductions in primary and secondary pain outcomes as a result of engaging in psychological treatment for pain. However, we found that treatment outcomes did not differ, whether the patient received ACT, CBT, or both for chronic pain; across all conditions, the interventions had a small effect on pain severity, pain interference, and illness-focused coping, and a moderate-to-large effect on global distress and catastrophizing. Past research has suggested little difference between ACT and CBT [1], which may explain why the current study showed null results. One suggestion has been that the data on ACT and related approaches have influenced traditional CBT, toward a new model that emphasizes being open, centered, and mindful and actively pursuing values. That may be why ACT and CBT have become more difficult to distinguish. More recently, Cosio and Ariel-Donges [50] also found that CBT’s focus on modifying maladaptive behaviors may inadvertently increase acceptance of chronic pain via decreased behavioral avoidance.
Not only does this suggest that treatment-specific differences may not account for psychotherapy outcomes for chronic pain as proposed by the common factors theory, but it also refutes the hypothesis that sequencing the order of group intervention has a significant impact on outcomes. We did not find a significant difference in outcomes, regardless of whether participants completed one or both groups. Previous research has studied the dose–response relationship in psychotherapy with mixed results. One of the initial studies on patient outcomes related to treatment duration suggested that optimal therapeutic gain was achieved when patients remained in therapy for at least 20 sessions [51]. However, in a general mental health setting, studies have suggested that clinically significant change can occur in between 11–18 sessions of psychotherapy, which is more in line with the time-limited nature of psychological treatment offered in a VA setting [52]. In line with this data, our study suggests that more sessions (i.e., >20) do not necessarily produce better outcomes for Veterans experiencing chronic pain; instead, statistically significant change can occur when the patient participates in time-limited evidence-based psychotherapies for chronic pain. From a resource-optimization standpoint—those of the provider in administering the intervention and those of the patient in attending scheduled appointments—these findings support that it may not be necessary for patients to receive both interventions to receive maximum benefit, as may be implied by the Transactional Model of Stress and Coping. Past research has also indicated that treatment effects on chronic pain can be witnessed in as few as six group sessions of CBT [11]. It would be valuable to conduct additional research on dose response to group intervention for chronic pain to further inform this conclusion, such as an investigation of briefer models of these interventions (focused ACT and brief CBT), alone and in combination. It may also be valuable to assess whether the observed changes in mean scores are associated with clinically significant change in pain-related outcomes in daily life.
In a previous study, group intervention for chronic pain was associated with improvements in factors related to functional status, such as pain interference, illness-focused coping behaviors, catastrophization, and overall distress, rather than pain severity [1]. These changes are consistent with the general theory behind psychological intervention for chronic pain, where greater emphasis is placed on improving patient function and quality of life than on reducing pain-severity scores [53]. The current study replicated the previous findings but also found significant improvements in pain severity from pre- to post-treatment. This raises an important question about patient expectations for treatment: Does it benefit patients to anticipate a reduction in perceived pain as a result of participating in group intervention for chronic pain? Or, is it possible that this expectation may detract from a patient’s ability to make improvements in functional status during treatment? Although patients may be more likely to engage in a treatment that is perceived to contribute to reductions in pain scores, providers must consider the implications of a focus on pain reduction vs. functional improvement. Future studies may evaluate the impact of patient expectations (i.e., reduction in pain severity vs. improvement in functionality/quality of life) on pain-treatment outcomes. Taken together, these findings support that it may be the “sales pitch” given to patients at the outset of treatment that is most important in determining response to group intervention for chronic pain.
Limitations in this study include its quasi-experimental design, use of self-report data, and sample characteristics. Unlike a randomized control trial, the current study used a pre/post-test design without a control group. Although this design afforded the ability to offer an intervention to all study participants from a vulnerable population who could potentially benefit, it is not sufficient for system-wide dissemination. Future studies could overcome this limitation by including a wait-list control group or “usual care” intervention. Self-report measures were used in the current study, which may constitute another intervention, as they cause participants to reflect on their own experience. Since the current study proposed that common factors may be at play with the current findings, future studies may want to consider using treatment expectancy and/or therapeutic alliance measures. This study also did not take into account participant engagement in other modalities of pain rehabilitation, as a possible explanation for change in pain-related outcomes. As all Veterans participated in a preliminary health education program prior to the start of the intervention and were aware of the treatments for chronic pain offered within the facility, it is plausible that participants were also engaging in other forms of treatment simultaneously and, thus, treatment effects cannot solely be attributed to the group interventions delineated here. Finally, the current sample was not necessarily representative of the typical Veteran profile; instead, it was predominately African American and had a large sample of females [54]. This limits the ability to generalize the results outside of the current Veteran sample.
5. Conclusions
Considering that outcomes are similar regardless of which modality of treatment is received, whether singularly or in sequence, providers can encourage patient collaboration in establishing a treatment plan and help them select an intervention plan that is most in line with their goals and values. At sites where both treatments are available, though patients may elect to receive both treatments based on personal preference, this approach may only benefit them in the sense of increasing patient–provider alliance. As treatment for chronic pain emphasizes the importance of patients to assume an active self-management approach to their healthcare, providers should be judicious when helping patients select interventions that will be most likely to facilitate this goal, as opposed to encouraging dependence on treatment. Furthermore, the current findings underline the importance of pain management, as it is a fundamental aspect of clinical practice, training, and research in rheumatology, as delineated in the Pain Management Task Force of the American College of Rheumatology report, published in 2010 [55].
Author Contributions
Conceptualization, D.C.; methodology, D.C.; software, M.S.; validation, D.C.; formal analysis, D.C. and M.S.; investigation, D.C.; resources, D.C.; data curation, D.C.; writing—original draft preparation, M.S.; writing—review and editing, D.C. and M.S.; visualization, D.C.; supervision, D.C.; project administration, D.C.; funding acquisition, none. All authors have read and agreed to the published version of the manuscript.
Funding
This study was part of a government employment. There was no additional funding.
Institutional Review Board Statement
IRB approval # 1479524: An Exploration of the Implications of Sequencing Order on Group Pain Interventions from the JBVAMC IRB.
Informed Consent Statement
Informed consent was exempt due to the investigation being a retrospective study.
Data Availability Statement
Data is available upon request from the principle investigator.
Acknowledgments
The authors would like to thank all the Veterans, therapists, and supervisors who made this research possible, especially Nasya Breach, Josh Greco, Jessica Pieczynski, Genna Popovich-Hymowitz, Scott Sperling, Sujata Swaroop, Erin Watson, Bonnie Yap, Tracy Bisterfelt, and Susan Payvar. The authors would also like to thank the staff members at the Jesse Brown VA Medical Center’s Psychology and Pain Management departments, for their vision and ongoing support of the pain psychology program.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Cosio, D. Practice-based evidence for outpatient, acceptance & commitment therapy for veterans with chronic, non-cancer pain. J. Context. Behav. Sci. 2015, 5, 23–32. [Google Scholar] [CrossRef]
- Veterans’ Health Administration Issues Notice Regarding Rescission of BHA Program Guide 1103.3. Mental Health Guidelines for the New Veterans Health Administration. In VHA Handbook 1160.01; Health Reference Center Academic; U.S. Department of Veterans Affairs: Washington, DC, USA, 2013.
- Cosio, D.; Schafer, T. Implementing an acceptance and commitment therapy group protocol with veterans using VA’s stepped care model of pain management. J. Behav. Med. 2015, 38, 984–997. [Google Scholar] [CrossRef] [PubMed]
- De Boer, M.J.; Steinhagen, H.E.; Versteegen, G.J.; Struys, M.M.R.F.; Sanderman, R. Mindfulness, Acceptance and Catastrophizing in Chronic Pain. PLoS ONE 2014, 9, e87445. [Google Scholar] [CrossRef]
- Johnston, M.; Foster, M.; Shennan, J.; Starkey, N.; Johnson, A. The Effectiveness of an Acceptance and Commitment Therapy Self-help Intervention for Chronic Pain. Clin. J. Pain 2010, 26, 393–402. [Google Scholar] [CrossRef] [PubMed]
- McCracken, L.M.; Vowles, K.E.; Eccleston, C. Acceptance-based treatment for persons with complex, long standing chronic pain: A preliminary analysis of treatment outcome in comparison to a waiting phase. Behav. Res. Ther. 2005, 43, 1335–1346. [Google Scholar] [CrossRef] [PubMed]
- Vowles, K.E.; McCracken, L.M.; McLeod, C.; Eccleston, C. The Chronic Pain Acceptance Questionnaire: Confirmatory factor analysis and identification of patient subgroups. Pain 2008, 140, 284–291. [Google Scholar] [CrossRef]
- Wicksell, R.; Melin, L.; Lekander, M.; Olsson, G. Evaluating the effectiveness of exposure and acceptance strategies to improve functioning and quality of life in longstanding pediatric pain: A randomized controlled trial. Pain 2009, 141, 248–257. [Google Scholar] [CrossRef] [PubMed]
- Cosio, D. Replication of a cognitive behavioral therapy for chronic pain group protocol by therapists in training. Postgrad. Med. 2014, 127, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, D.L.; Kaplan, K.H.; Nadeau, M.G.; Brodeur, C.; Smith, S.; Schmid, C.H. A Controlled Study of a Stress-Reduction, Cognitive-Behavioral Treatment Program in Fibromyalgia. J. Musculoskelet. Pain 1994, 2, 53–66. [Google Scholar] [CrossRef]
- Lamb, S.; Hansen, Z.; Lall, R.; Castelnuovo, E.; Withers, E.J.; Nichols, V.; Potter, R.; Underwood, M.R. Group cognitive behavioural treatment for low-back pain in primary care: A randomised controlled trial and cost-effectiveness analysis. Lancet 2010, 375, 916–923. [Google Scholar] [CrossRef]
- McCracken, L.M.; Turk, D.C. Behavioral and Cognitive–Behavioral Treatment for Chronic Pain: Outcome, predictors of outcome, and treatment process. Spine 2002, 27, 2564–2573. [Google Scholar] [CrossRef]
- Reid, M.C.; Otis, J.; Barry, L.; Kerns, R.D. Cognitive-behavioral therapy for chronic low back pain in older persons: A preliminary study. Pain Med. 2003, 4, 223–230. [Google Scholar] [CrossRef]
- Smeets, R.J.; Vlaeyen, J.W.; Kester, A.D.; Knottnerus, J.A. Reduction of Pain Catastrophizing Mediates the Outcome of Both Physical and Cognitive-Behavioral Treatment in Chronic Low Back Pain. J. Pain 2006, 7, 261–271. [Google Scholar] [CrossRef] [PubMed]
- Vowles, K.; Wetherell, J.L.; Sorrell, J.T. Targeting Acceptance, Mindfulness, and Values-Based Action in Chronic Pain: Findings of Two Preliminary Trials of an Outpatient Group-Based Intervention. Cogn. Behav. Pract. 2009, 16, 49–58. [Google Scholar] [CrossRef]
- Wetherell, J.L.; Afari, N.; Rutledge, T.; Sorrell, J.T.; Stoddard, J.A.; Petkus, A.J.; Solomon, B.C.; Lehman, D.H.; Liu, L.; Lang, A.J.; et al. A randomized, controlled trial of acceptance and commitment therapy and cognitive-behavioral therapy for chronic pain. Pain 2011, 152, 2098–2107. [Google Scholar] [CrossRef] [PubMed]
- Rosenzweig, S. Some implicit common factors in diverse methods of psychotherapy: At last the Dodo said, Everybody has won and all must have prizes. Am. J. Orthopsychiatry 1936, 6, 412–415. [Google Scholar] [CrossRef]
- Wampold, B.E. How important are the common factors in psychotherapy? An update. World Psychiatry 2015, 14, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, R.S. Psychological Stress and the Coping Process; McGraw-Hill: New York, NY, USA, 1966. [Google Scholar]
- Folkman, S.; Lazarus, R.S. Coping as a mediator of emotion. J. Pers. Soc. Psychol. 1988, 54, 466–475. [Google Scholar] [CrossRef] [PubMed]
- Walinga, J. Toward a Theory of Change Readiness: The roles of appraisal, focus, and perceived control. J. Appl. Behav. Sci. 2008, 44, 315–347. [Google Scholar] [CrossRef]
- Finkelstein-Fox, L.; Park, C.L.; Riley, K.E. Mindfulness’ effects on stress, coping, and mood: A daily diary goodness-of-fit study. Emotion 2019, 19, 1002–1013. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, D.S.; Kim, M.; Akeju, O.; Torrado-Carvajal, A.; Edwards, R.R.; Zhang, Y.; Bergan, C.; Protsenko, E.; Kucyi, A.; Wasan, A.D.; et al. The neuroinflammatory component of negative affect in patients with chronic pain. Mol. Psychiatry 2019, 26, 864–874. [Google Scholar] [CrossRef]
- Carpenter, R.W.; Lane, S.P.; Bruehl, S.; Trull, T.J. Concurrent and lagged associations of prescription opioid use with pain and negative affect in the daily lives of chronic pain patients. J. Consult. Clin. Psychol. 2019, 87, 872–886. [Google Scholar] [CrossRef] [PubMed]
- Ravyts, S.G.; Dzierzewski, J.M.; Raldiris, T.; Perez, E. Sleep and pain interference in individuals with chronic pain in mid- to late-life: The influence of negative and positive affect. J. Sleep Res. 2019, 28, e12807. [Google Scholar] [CrossRef] [PubMed]
- Moreno, J.L.; Nabity, P.S.; Kanzler, K.; Bryan, C.J.; McGeary, C.A.; McGeary, D.D. Negative Life Events (NLEs) Contributing to Psychological Distress, Pain, and Disability in a U.S. Military Sample. Mil. Med. 2019, 184, e148–e155. [Google Scholar] [CrossRef]
- Thoresen, S.; Mehlum, L. Traumatic Stress and Suicidal Ideation in Norwegian Male Peacekeepers. J. Nerv. Ment. Dis. 2008, 196, 814–821. [Google Scholar] [CrossRef]
- Samwel, H.J.A.; Kraaimaat, F.W.; Crul, B.J.P.; Dongen, R.D.; Evers, A.W.M. Multidisciplinary allocation of chronic pain treatment: Effects and cognitive-behavioural predictors of outcome. Br. J. Health Psychol. 2009, 14, 405–421. [Google Scholar] [CrossRef]
- McCracken, L.; Eccleston, C. The relative utility of copingbased versus acceptance-based approaches to chronic pain. Eur. J. Pain 2006, 10, 23–29. [Google Scholar] [CrossRef]
- Keefe, F.J.; Gil, K.M. Behavioral concepts in the analysis of chronic pain syndromes. J. Consult. Clin. Psychol. 1986, 54, 776–783. [Google Scholar] [CrossRef]
- Turk, D.; Meichenbaum, D.; Genest, M. Pain and Behavioral Medicine: A Cognitive-Behavioral Perspective; Guilford Press: New York, NY, USA, 1983. [Google Scholar]
- Keefe, F. Cognitive behavioral therapy for managing pain. Clin. Psychol. 1996, 49, 4–5. [Google Scholar] [CrossRef][Green Version]
- Dahl, J.; Lundgren, T. Living Beyond Your Pain: Using Acceptance and Commitment Therapy to Ease Chronic Pain; Newly Harbinger Publications: Oakland, CA, USA, 2006. [Google Scholar]
- Dahl, J.; Wilson, K.; Luciano, C.; Hayes, S. Acceptance and Commitment Therapy for Chronic Pain; Context Press: Reno, NV, USA, 2005. [Google Scholar]
- Vowles, K.; Sorrell, J. Life with Chronic Pain: An Acceptance-Based Approach (Therapist Guide and Patient Workbook). 2007. Available online: http://contextualscience.org/files/CP_Acceptance_Manual_09.2008.pdf (accessed on 1 July 2022).
- Cosio, D. A group-based, acceptance & commitment therapy intervention for chronic pain. Soc. Work Groups 2019, 43, 334–346. [Google Scholar] [CrossRef]
- Otis, J. Managing Chronic Pain: A Cognitive-Behavioral Therapy Approach Therapist Guide (Treatments that Work); Oxford University Press: New York, NY, USA, 2007. [Google Scholar]
- Cleeland, C.S.; Ryan, K.M. Pain assessment: Global use of the Brief Pain Inventory. Ann. Acad. Med. Singap. 1994, 23, 129–138. [Google Scholar] [PubMed]
- Fairbank, J.C.T.; Couper, J.; Davies, J.B.; O’Brien, J.P. Oswestry Low Back Pain Disability Questionnaire. Physiotherapy 1980, 66, 271–273. [Google Scholar] [CrossRef] [PubMed]
- Rosenstiel, A.K.; Keefe, F.J. The use of coping strategies in chronic low back pain patients: Relationship to patient characteristics and current adjustment. Pain 1983, 17, 33–44. [Google Scholar] [CrossRef]
- Jensen, M.P.; Turner, J.A.; Romano, J.M.; Strom, S.E. The chronic pain coping inventory: Development and preliminary validation. Pain 1995, 60, 203–216. [Google Scholar] [CrossRef]
- Derogatis, L. Brief Symptom Inventory; Clinical Psychometric Research: Baltimore, MD, USA, 1975. [Google Scholar]
- Cosio, D.; Lin, E.H. Effects of a pain education program for Veterans with chronic, non-cancer pain: A pilot study. J. Pain Palliat. Care Pharmacother. 2013, 27, 340–349. [Google Scholar] [CrossRef]
- Williams, A.; Eccleston, C.; Morley, S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst. Rev. 2012, 11, CD007407. [Google Scholar] [CrossRef]
- Blankers, M.; Koeter, M.W.J.; Schippers, G.M. Missing Data Approaches in eHealth Research: Simulation Study and a Tutorial for Nonmathematically Inclined Researchers. J. Med. Internet. Res. 2010, 12, e54. [Google Scholar] [CrossRef]
- D’Souza, D.D.; Liu-Seifert, H.; Zhang, S.; Skljarevski, V. A closer look at the baseline-observation-carried-forward (BOCF). Patient Prefer. Adherence 2010, 4, 11–16. [Google Scholar] [CrossRef]
- Des Jarlais, D.C.; Lyles, C.; Crepaz, N.; the TREND Group. Improving the Reporting Quality of Nonrandomized Evaluations of Behavioral and Public Health Interventions: The TREND Statement. Am. J. Public Health 2004, 94, 361–366. [Google Scholar] [CrossRef]
- Kerns, R.D.; Rosenberg, R.; Jamison, R.; Caudill, M.A.; Haythornthwaite, J. Readiness to adopt a self-management approach to chronic pain: The Pain Stages of Change Questionnaire (PSOCQ). Pain 1997, 72, 227–234. [Google Scholar] [CrossRef]
- Thomas, E.; Peat, G.; Harris, L.; Wilkie, R.; Croft, P.R. The prevalence of pain and pain interference in a general population of older adults: Cross-sectional findings from the North Staffordshire Osteoarthritis Project (NorStOP). Pain 2004, 110, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Cosio, D.; Ariel-Donges, A. Does Cognitive Behavioral Therapy increase acceptance of chronic pain amongst veterans? J. Behav. Cogn. Ther. 2020, 30, 283–290. [Google Scholar] [CrossRef]
- Seeman, J. Counselor judgments of therapeutic process and outcome. In Psychotherapy and Personality Change; Rogers, C.R., Dymond, R.F., Eds.; University of Chicago Press: Chicago, IL, USA, 1954; pp. 99–108. [Google Scholar]
- Anderson, E.M.; Lambert, M.J. A survival analysis of clinically significant change in outpatient psychotherapy. J. Clin. Psychol. 2001, 57, 875–888. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.L.; McKellar, J.D.; Raffa, S.D.; Clark, M.E.; Kerns, R.D.; Karlin, B.E. Cognitive Behavioral Therapy for Chronic Pain among Veterans: Therapist Manual; U.S. Department of Veterans Affairs: Washington, DC, USA.
- American Community Survey: Profile of Veterans. Data from the American Community Survey. National Center for Veterans Analysis and Statistics. 2009. Available online: https://www.va.gov/vetdata/docs/SpecialReports/Profile_of_Veterans_2009_FINAL.pdf (accessed on 3 September 2020).
- Borenstein, D.G.; Hassett, A.L.; Pisetsky, D. Pain management in rheumatology research, training, and practice. Clin. Exp. Rheumatol. 2017, 35 (Suppl. 107), 2–7. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).