HEARTS Study Protocol: Helping Enable Access and Remove Barriers To Support for Young Adults with Mental Health-Related Disabilities
Abstract
1. Introduction
1.1. Aim
1.2. Mixed-Methods Research Question
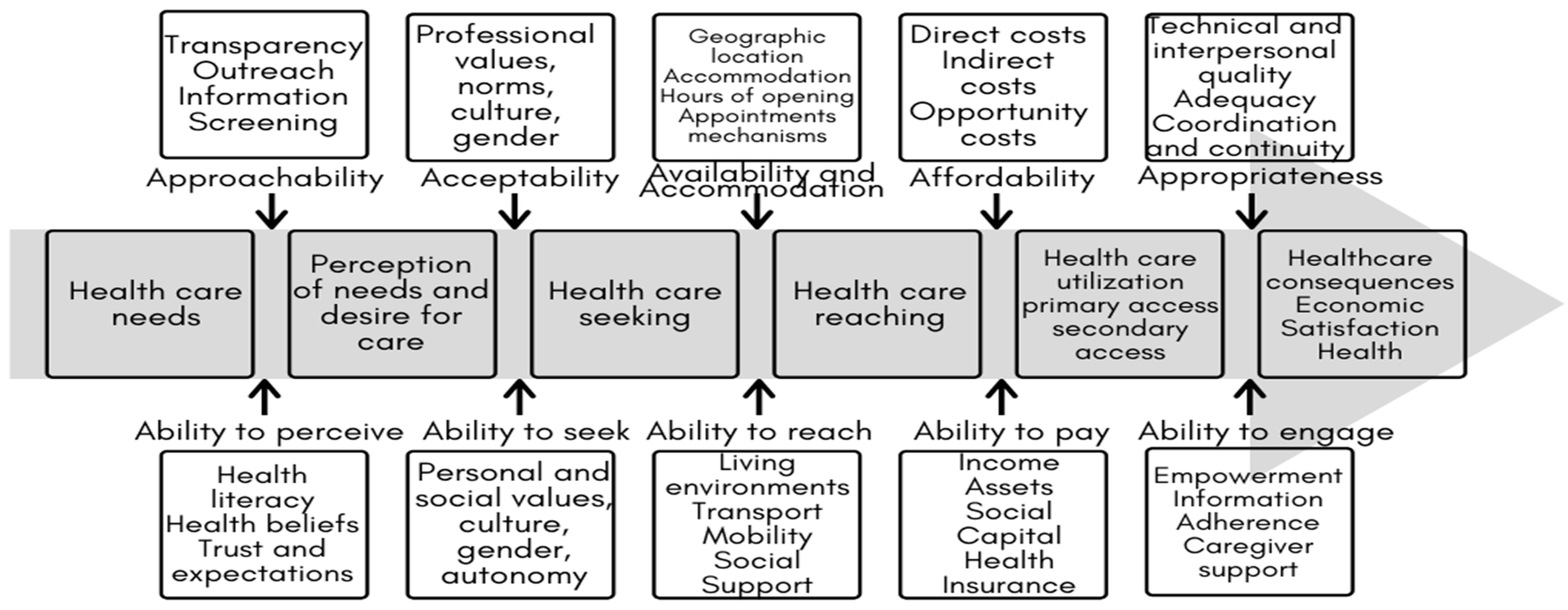
1.3. Integrated Analysis Framework
2. Materials and Methods
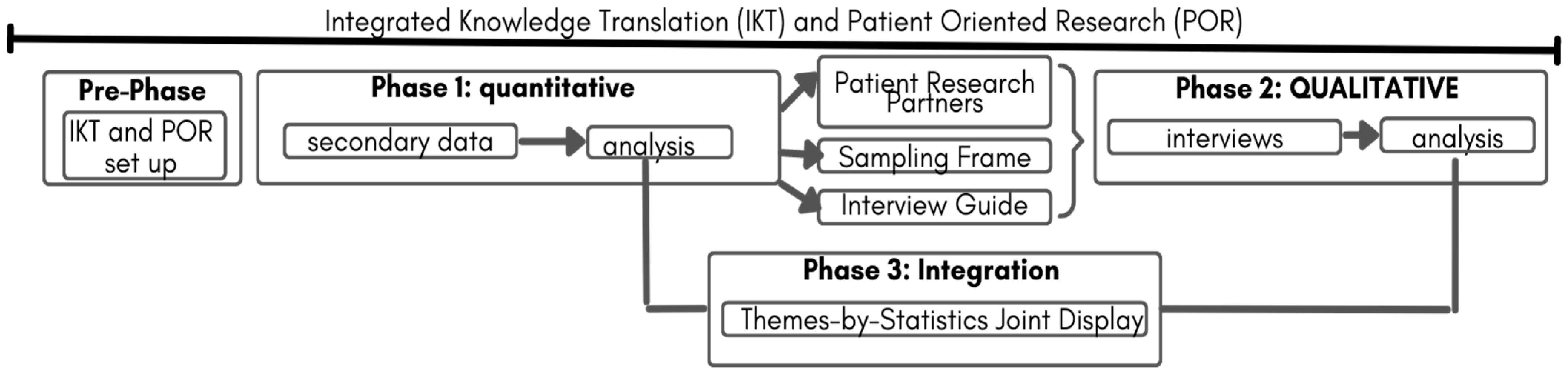
2.1. Study Design
2.2. Pre-Phase: POR and Integrated Knowledge Translation
2.3. Phase 1: Quantitative Extensive Data
2.3.1. Research Question
2.3.2. Sample and Measures
2.3.3. Data Analysis Procedures
2.4. Phase 2: Qualitative Intensive Study
2.4.1. Research Questions:
- What are the experiences and perceptions of YMHDs regarding access to mental healthcare?
- How do YMHDs perceive the impact of functional impairments on their access to mental healthcare?
- How do demographic factors and determinants of health shape the experiences and perceptions of YMHDs regarding access to mental healthcare?
- What do young adults perceive as barriers and facilitators to accessing mental healthcare for YMHDs?
2.4.2. Sample
Recruitment
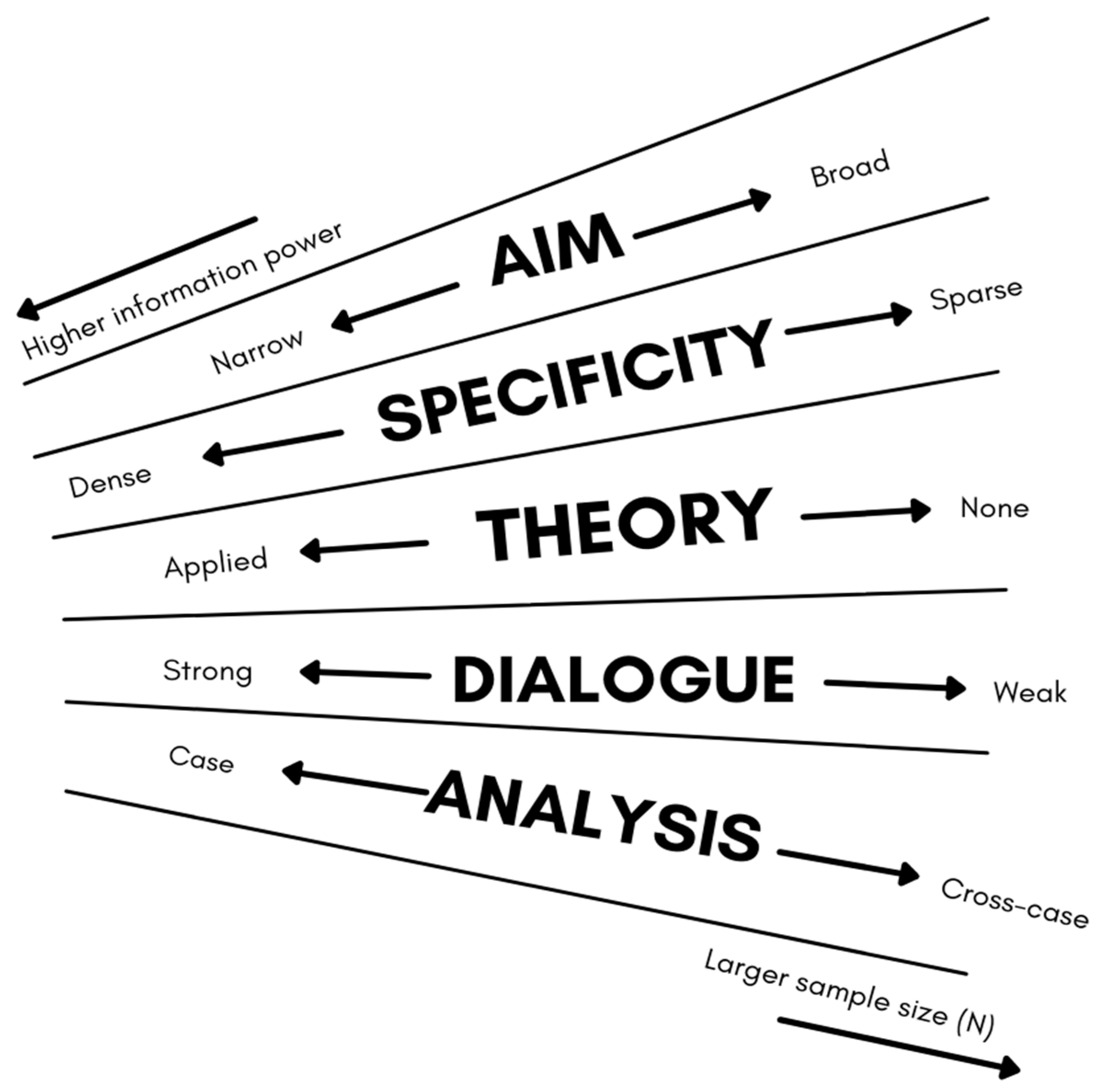
2.4.3. Sample Size
2.4.4. Data Collection
- “Can you think back to the times when you didn’t get the healthcare you needed? Why do you think that happened?”
- “What troubles do you run into when trying to look after your health because you have trouble remembering things or staying focused?”
- “Have there been times when you think your trouble with memory or focusing, and feeling anxious, stopped you from getting healthcare? Tell me about that.”
2.4.5. Data Analysis
2.5. Phase 3: Integration of Data Themes by Joint Display
2.5.1. Data Management and Storage
2.5.2. Ethical Considerations
2.5.3. Informed Consent
2.5.4. Risk–Benefit Analysis
3. Anticipated Results
4. Strengths and Limitations
5. Timeline
6. Budget
7. Conclusions and Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chaudhury, P.K.; Deka, K.; Chetia, D. Disability associated with mental disorders. Indian J. Psychiatry 2006, 48, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Statistics Canada. Canadian Survey on Disability. 2017. Available online: https://www150.statcan.gc.ca/n1/pub/11-627-m/11-627-m2019005-eng.htm (accessed on 6 May 2022).
- Wiens, K.; Bhattarai, A.; Pedram, P.; Dores, A.; Williams, J.; Bulloch, A.; Patten, S. A growing need for youth mental health services in Canada: Examining trends in youth mental health from 2011 to 2018. Epidemiol. Psychiatr. Sci. 2020, 29, e115. [Google Scholar] [CrossRef] [PubMed]
- Society for Adolescent Health and Medicine. Young Adult Health and Well-Being: A Position Statement of the Society for Adolescent Health and Medicine. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med. 2017, 60, 758–759. [Google Scholar] [CrossRef] [PubMed]
- Arnett, J.J. Emerging adulthood: A theory of development from the late teens through the twenties. Am. Psychol. 2000, 55, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Gilmore, K.J.; Meersand, P. The Little Book of Child and Adolescent Development; Oxford University Press: New York, NY, USA, 2015; ISBN 978-0-19-989922-7. [Google Scholar]
- Valeras, A. “We don’t have a box”: Understanding Hidden Disability Identity Utilizing Narrative Research Methodology. Disabil. Stud. Q. 2010, 30. [Google Scholar] [CrossRef]
- Dunn, D.S.; Burcaw, S. Disability identity: Exploring narrative accounts of disability. Rehabil. Psychol. 2013, 58, 148–157. [Google Scholar] [CrossRef]
- Evans, M.; Baillie, L. Usher Syndrome, an Unseen/Hidden Disability: A Phenomenological Study of Adults across the Lifespan Living in England. Disabil. Soc. 2022, 37, 1636–1658. [Google Scholar] [CrossRef]
- Bengtsson, S. Out of the frame: Disability and the body in the writings of Karl Marx. Scand. J. Disabil. Res. 2017, 19, 151–160. [Google Scholar] [CrossRef]
- Goodley, D. Dis/entangling critical disability studies. Disabil. Soc. 2013, 28, 631–644. [Google Scholar] [CrossRef]
- Hanebutt, R.; Mueller, C. Disability Studies, Crip Theory, and Education. Oxford Research Encyclopedia of Education. Available online: https://oxfordre.com/education/view/10.1093/acrefore/9780190264093.001.0001/acrefore-9780190264093-e-1392 (accessed on 13 May 2022).
- Malla, A.; Shah, J.; Iyer, S.; Boksa, P.; Joober, R.; Andersson, N.; Lal, S.; Fuhrer, R. Youth Mental Health Should Be a Top Priority for Health Care in Canada. Can. J. Psychiatry 2018, 63, 216–222. [Google Scholar] [CrossRef]
- Bhaskar, R. Explaining Society: An Introduction to Critical Realism in the Social Sciences, 1st ed.; Routledge: London, UK, 2005. [Google Scholar] [CrossRef]
- Bhaskar, R. A Realist Theory of Science; Routledge: London, UK, 2008. [Google Scholar] [CrossRef]
- Levesque, J.-F.; Harris, M.F.; Russell, G. Patient-centred access to health care: Conceptualising access at the interface of health systems and populations. Int. J. Equity Health 2013, 12, 18. [Google Scholar] [CrossRef]
- World Health Organization. Towards a Common Language for Functioning, Disability and Health; The international Classification of Functioning, Disability and Health; World Health Organizatioin: Geneva, Switzerland, 2002; pp. 1–23. [Google Scholar]
- Bhaskar, R.; Danermark, B. Metatheory, Interdisciplinarity and Disability Research: A Critical Realist Perspective. Scand. J. Disabil. Res. 2006, 8, 278–297. [Google Scholar] [CrossRef]
- Fletcher, A.J. Applying Critical Realism in Qualitative Research: Methodology Meets Method. Int. J. Soc. Res. Methodol. 2017, 20, 181–194. [Google Scholar] [CrossRef]
- Porpora, D.V. Reconstructing Sociology: The Critical Realist Approach; Cambridge University Press: Cambridge, 2015. [Google Scholar] [CrossRef]
- Vincent, S.; O’Mahoney, J. Critical Realism and Qualitative Research: An Introductory Overview. In The SAGE Handbook of Qualitative Business and Management Research Methods: History and Traditions; SAGE Publications Ltd: London, UK, 2018; pp. 201–216. [Google Scholar] [CrossRef]
- Ustün, T.B.; Chatterji, S.; Bickenbach, J.; Kostanjsek, N.; Schneider, M. The International Classification of Functioning, Disability and Health: A new tool for understanding disability and health. Disabil. Rehabil. 2003, 25, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Canadian Institutes of Health Research Strategy for Patient-Oriented Research—Patient Engagement Framework—CIHR. Available online: https://cihr-irsc.gc.ca/e/48413.html (accessed on 31 October 2020).
- Gagliardi, A.R.; Berta, W.; Kothari, A.; Boyko, J.; Urquhart, R. Integrated knowledge translation (IKT) in health care: A scoping review. Implement. Sci. 2016, 11, 38. [Google Scholar] [CrossRef] [PubMed]
- Statistics Canada Canadian Community Health Survey—Annual Component (CCHS). Available online: https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&Id=795204 (accessed on 17 April 2021).
- Long, S. Regression Models for Categorical and Limited Dependent Variables; Advanced Quantitative Techniques in the Social Sciences; Sage Publications: Thousand Oaks, CA, USA, 1997. [Google Scholar]
- Bujang, M.A.; Sa’at, N.; Sidik, T.M.I.T.A.B.; Joo, L.C. Sample Size Guidelines for Logistic Regression from Observational Studies with Large Population: Emphasis on the Accuracy Between Statistics and Parameters Based on Real Life Clinical Data. Malays. J. Med. Sci. MJMS 2018, 25, 122–130. [Google Scholar] [CrossRef] [PubMed]
- van Smeden, M.; Moons, K.G.; de Groot, J.A.; Collins, G.S.; Altman, D.G.; Eijkemans, M.J.; Reitsma, J.B. Sample size for binary logistic prediction models: Beyond events per variable criteria. Stat. Methods Med. Res. 2019, 28, 2455–2474. [Google Scholar] [CrossRef]
- Malterud, K.; Siersma, V.D.; Guassora, A.D. Sample Size in Qualitative Interview Studies: Guided by Information Power. Qual. Health Res. 2016, 26, 1753–1760. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Thematic Analysis: A Practical Guide; Sage Publications Ltd: Thousand Oaks, CA, USA, 2021. [Google Scholar]
- Edwards, P.K.; O’Mahoney, J.; Vincent, S. Critical Realism and Mixed Methods Research. In Studying Organizations Using Critical Realism; Edwards, P.K., O’Mahoney, J., Vincent, S., Eds.; Oxford University Press: Oxford, UK, 2014; pp. 241–263. [Google Scholar] [CrossRef]
- Zachariadis, M.; Scott, S.; Barrett, M. Methodological Implications of Critical Realism for Mixed-Methods Research. MIS Q. 2013, 37, 855–879. Available online: https://www.jstor.org/stable/43826004 (accessed on 17 March 2022). [CrossRef]
- Mukumbang, F.C. Retroductive Theorizing: A Contribution of Critical Realism to Mixed Methods Research. J. Mix. Methods Res. 2021, 17, 93–114. [Google Scholar] [CrossRef]
- Pilgrim, D. Some implications of critical realism for mental health research. Soc. Theory Health 2014, 12, 1–21. [Google Scholar] [CrossRef]
- Pilgrim, D. Critical realism and mental health research. In Routledge International Handbook of Critical Mental Health; Routledge: London, UK, 2017. [Google Scholar]
- Braun, V.; Clarke, V. One Size Fits All? What Counts as Quality Practice in (Reflexive) Thematic Analysis? Qual. Res. Psychol. 2021, 18, 328–352. [Google Scholar] [CrossRef]
- Guetterman, T.C. Descriptions of Sampling Practices within Five Approaches to Qualitative Research in Education and the Health Sciences. Forum Qual. Sozialforschung Forum Qual. Soc. Res. 2015, 16, 1–23. [Google Scholar] [CrossRef]
- Johnson, R.E.; Grove, A.L.; Clarke, A. Pillar Integration Process: A Joint Display Technique to Integrate Data in Mixed Methods Research. J. Mix. Methods Res. 2019, 13, 301–320. [Google Scholar] [CrossRef]
- Government of Canada, I. Tri-Agency Research Data Management Policy. Available online: https://science.gc.ca/site/science/en/interagency-research-funding/policies-and-guidelines/research-data-management/tri-agency-research-data-management-policy (accessed on 5 April 2023).
- Guillemin, M.; Gillam, L. Ethics, Reflexivity, and “Ethically Important Moments” in Research. Qual. Inq. 2004, 10, 261–280. [Google Scholar] [CrossRef]
- Kipnis, K. Seven Vulnerabilities in the Pediatric Research Subject. Theor. Med. Bioeth. 2003, 24, 107–120. [Google Scholar] [CrossRef]
- Kipnis, K. Vulnerability in Research Subjects: A Bioethical Taxonomy; Commissioned Papers: Rockville, MD, USA, 2001. [Google Scholar]
- Sieber, J. Planning Ethically Responsible Research; SAGE Publications, Inc.: Newbury Park, CA, USA, 1992. [Google Scholar] [CrossRef]
- Rid, A.; Emanuel, E.J.; Wendler, D. Evaluating the risks of clinical research. JAMA 2010, 304, 1472–1479. [Google Scholar] [CrossRef]
- McCambridge, J.; Witton, J.; Elbourne, D.R. Systematic review of the Hawthorne effect: New concepts are needed to study research participation effects. J. Clin. Epidemiol. 2014, 67, 267–277. [Google Scholar] [CrossRef]



| Canadian Community Health Survey | |
|---|---|
| Variable Name | Concept |
| Age of respondent (ANC1) | actual age of the respondent |
| Relationship without confirmation (RNC) | the relationship of an individual to someone else in the household when any previously collected relationship is not to be confirmed |
| Main activity (MAC) | main activity in the last week |
| General health (GEN) | data on self-perceived health, satisfaction with life, self-perceived mental health, self-perceived stress at work and with life in general, and sense of belonging to local community |
| Washington Group—disability measure (WDM) | describes and monitors persons with limitations in basic activity functioning |
| Activities of daily living (ADL) | the impact of a physical, mental or health problem on common activities of daily living |
| Changes made to improve health (CIH) | questions related to changes in behaviour that they have made in the past year (and intentions for the future) to improve their health |
| Sleep (SLP) | questions related to sleep |
| Alcohol use (ALC) | questions about how often and how much alcohol the respondent has drunk in the past 12 months, and if they have ever had a drink in their life. |
| Alcohol use during the past week (ALW) | had a drink in the past 12 months about their drinking consumption on each day of the past week. |
| Medication use (MED) | use of prescription and non-prescription medications in the past 12 months, including different pain relievers, stimulants and sedatives |
| Physical activities—adults 18 years and older (PAA) | how active respondents, 18 years of age and older, have been in the last seven days. |
| Consultations about mental health (CMH) | number of times in the past 12 months that the respondents have consulted with mental health professionals to discuss their emotional or mental health, and which professionals they saw or talked to. |
| Satisfaction with life (SWL) | level of satisfaction with various aspects of their life |
| Distress (DIS) | Level of distress |
| Depression (DEP) | Likelihood of depression |
| Sources of stress (STS) | identify the most common sources of stress |
| Social provisions (SPS) | respondent’s level of attachment, social integration, reassurance of worth, reliable alliance, and guidance |
| Stress and relationships (STR) | self-rate their ability to handle day-to-day demands and the level to which they can rely on others. |
| Primary healthcare (PHC) | topics related to the use of primary health care |
| Medical doctor attachment (MDA) | the level of attachment of Canadians to their doctor |
| Contacts with health professionals—extended block (CP2) | frequency of contact with various health professionals during the past 12 months for physical, emotional or mental health |
| Perceived need for care (PNC) | different kinds of help respondents received or thought they needed for problems with their emotions, mental health or use of alcohol or drugs in the past 12 months. |
| Patient satisfaction—community-based care (PSC) | whether respondents received any community-based health care services in the past 12 months (outside of a hospital or doctor’s office), and includes their rating of the quality and satisfaction with the care received. |
| Access to healthcare services (ACC) | experiences and perceptions regarding access to various types of health care services |
| Unmet healthcare needs (UCN) | identify respondents who needed health care (other than home care services) in the last 12 months but did not receive it |
| Labor force (LBF) | questions about the respondent’s current labour force activities during the past week |
| Socio-demographic characteristics (SDC) | important social and demographic information is collected, including immigrant status, country/province of birth, ethnic origin, aboriginal status, racial/cultural group, language, dwelling type and sexual orientation |
| Health insurance coverage (INS) | whether they have insurance to cover all or part of the cost of prescription medications, home care or long-term care |
| Prescriptions—cost-related non-adherence (PCN2) | non-adherence to prescription medication due to cost |
| Food security (FSC) | issues associated with food security |
| Income (INC) | the amount of their household income and other income sources, including supplement for disability |
| Quantitative Results (e.g., Organized by Major Results or Levels of Categorical Variables, “None, Mild, Moderate, Severe, Extreme”) | ||||
|---|---|---|---|---|
| Characteristics | Key Result 1 | Key Result 2 | Key Result 3 | Key Result 4 |
| Characteristic 1 | Describe sample | |||
| Characteristic 2 | ||||
| Characteristic 3 | ||||
| Quantitative Results (Organized by Key Results and Constructs) | Qualitative Interview Questions |
|---|---|
| Result 1 | Related Question |
| Result 2 | Related Question |
| Result 3 | Related Question |
| Result 4 | Related Question |
| Steps to Identify Magnitude | Factors That Influence Magnitude |
|---|---|
| (1) Identify the potential harms posed by the proposed research activity; | (1) The experience, such as pain or embarrassment, associated with the harm; (2) The burden of efforts to mitigate the harm (e.g., distress protocols); (3) The effects of the harm on the person’s ability to perform daily life activities; (4) Effects on the person’s ability to pursue life goals; (5) Duration of the harm; (6) Extent to which the person can adapt to the new circumstances if they cannot be mitigated; (7) Burden imposed by the adaptation. |
| (2) Categorize the magnitude of the potential harm into one of seven harm levels on a scale; | |
| (3) Estimate the likelihood of each potential harm; | |
| (4) Compare the likelihood of each potential harm with the likelihood of harms of the same magnitude and probability of occurrence. |
| Benefit Type | Description |
|---|---|
| Scientific Knowledge | Partners and participants will be provided with infographics and handouts that are short, balanced, and interesting summaries of relevant knowledge at the time of their participation. The material will be carefully edited, clear, simple, and devoid of professional jargon. It will utilize visual images where possible to be culturally sensitive as well as attempt to have a linguistic translation or cultural brokers to decolonize the information. Researchers will also be available to discuss any of the material with participants if they so desire. All persons involved in this study will be made aware of the timelines of the study and expectations around publications, presentations, and study outcomes. |
| Personally Relevant | Personally relevant benefits are limited. However, PRPs, and to a lesser extent participants, may gain insight, training, empowerment, and future opportunities as natural outcomes. |
| Psychosocial Benefits | Psychosocial benefits include the benefits of altruism, participation in an experiment that makes one feel worthwhile, and receiving favorable attention and esteem from a skilled investigator. These are the typical outcomes of receiving professional and respectful treatment. |
| Kinship Benefits | None identified. |
| Benefits to the Community or Organization | None identified; however, some may result from a Hawthorne effect [45], in which respect and attention paid to members of the mood and anxiety disorder community improve their outlook and performance. |
| Table | Phase | Procedure | Product | |
|---|---|---|---|---|
| Year 1 (May 2022–May 2023) | May 2022 | Research Ethics | Submission of REB | Approval of REB |
| August 2022 | Pre-Phase | Submit proposal to access data to the Prairie Regional Data Centre for access to the 2017–2018 Canadian Community Health Survey microdata Recruitment for YYMHD PRP for Phase 1 (N = 2–3) | Proposal for RDC Recruitment of YYMHD PRP | |
| September 2022 | 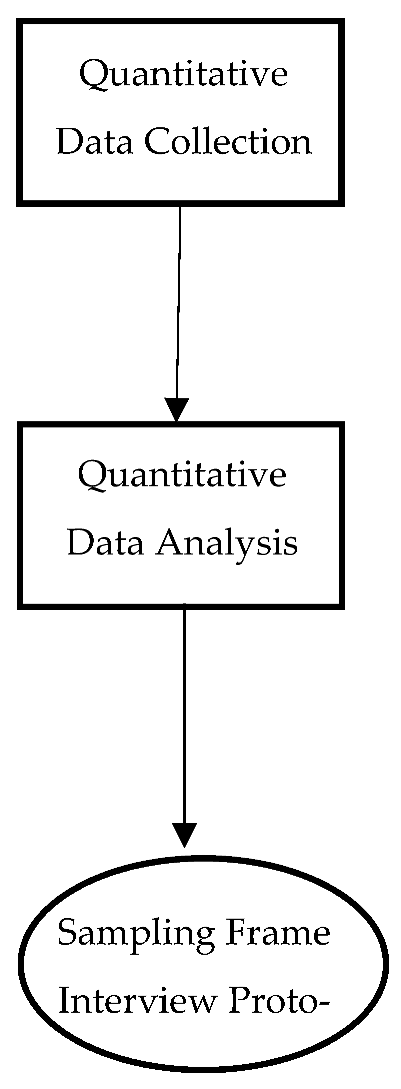 | Data Plan reviewed and updated Cross-sectional secondary data from CCHS. Import into STATA v 17 Sending working files to RDC DV = unmet health needs IV = organized by Integrated Analysis Framework (N = 1636) | Data Plan reviewed and approved by PRP Numeric Data | |
| October 2022 | Data cleaning/Data screening Recoding categorical variables Select cases: Age (20–29), diagnosis if N > 500 for explanatory power Univariate and Bivariate Analysis Assumption of Multicollinearity | Descriptive Statistics Missing Data Inferential Statistics Regression Analysis | ||
| Nov 2022 | Data visualization (infographics) and presentation for PRP Feedback and updating from engagement with PRP | Participant Joint Display Interview Question Joint Display | ||
| Dec 2022–Jan 2023 | Purposefully selecting, additional PRP (N = 5) and study participants based on sampling frame (N = 6–10) based on maximal variation sampling, extreme case sampling Developing interview questions for semi-structured interview with PRP | Sample N = 6–10 Semi-structured interview protocol | ||
| January 2023–April 2023 | 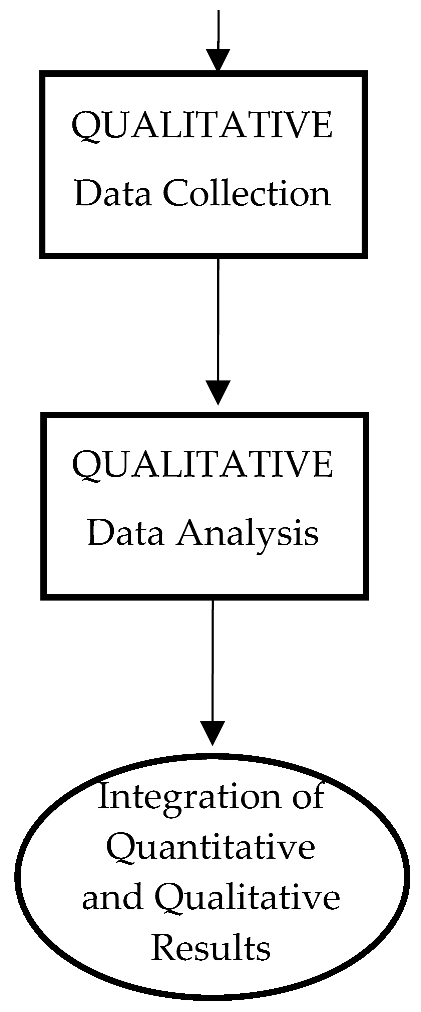 | Recruitment YYMHD study participants Continuous refinement of interview questions Individual in-depth interviews with 6–10 participants (information power) Rolling orthographic transcription Review with YYMHD PRP | Text data (interview transcriptions) Reflexive journals | |
| Year 2 (May 2023–May 2024) | May 2023–March 2024 | Braun & Clarke’s Reflexive Thematic Analysis Reflexive Journal Visual Mapping Retrodiction and Retroduction CAQDAS NVivo 11 for codes and themes Review codes and themes with YYMHD PRP | Reflexive journals Memos Annotations Codes and Themes—rich descriptions Visual mapping of codes and themes | |
| April 2024–May 2024 | Integration of quantitative and qualitative results Interpretation an explanation of factors that influence unmet healthcare needs Review with PRP | Themes by statistics joint display Discussion Implications for system/policy/practice change Future research | ||
| Year 3 | June 2024–Dec 2025 | Study close Research Outputs | Development with PRP academic and non-academic research outputs | Publications Conference Presentations Community and Stakeholder Resources |
| Category | Item | Quantity | Unit Cost | Total Cost |
|---|---|---|---|---|
| Research Team | Principal Investigator | 1 | Covered within Institution | |
| Co-Investigators | 2–7 | Covered within Appreciation Costs | ||
| Advisory Committee | 2 | Covered within Institution | ||
| Equipment | Computer | 1 | Covered within Institution | |
| Printer Services | 1 | Covered within Institution | ||
| Software Licenses: STATA | 1 | Covered within Institution | ||
| Software Licenses: Nvivo | 1 | Covered within Institution | ||
| Travel/Accommodations | Conferences | 3 | CAD 1000 | CAD 3000 |
| Supplies | Office Supplies | CAD 250 | CAD 250 | |
| YMHD Partners (5) | Appreciation Costs | 7 | CAD 125 | CAD 875 |
| Training Costs | 5 | CAD 40 | CAD 200 | |
| Travel Costs | 3–5 | CAD 20 | CAD 60–100 | |
| Virtual Equipment Costs | 3–5 | CAD 25 | CAD 75–125 | |
| Study Participants | Appreciation Costs | 6–10 | CAD 25 | CAD 150–250 |
| Knowledge Translation | Publication Fees | 2 | Covered within Institution | |
| Website Hosting | 1 | CAD 100 | CAD 100 | |
| Print Materials | 100 | CAD 1 | CAD 100 | |
| Conference Registration | 3 | CAD 200 | CAD 600 | |
| Miscellaneous | Indirect Costs | CAD 500 | CAD 500 | |
| Total Budget | CAD 5910–6100 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rao, S.; Dimitropoulos, G.; Milaney, K.; Eurich, D.T.; Patten, S.B. HEARTS Study Protocol: Helping Enable Access and Remove Barriers To Support for Young Adults with Mental Health-Related Disabilities. Youth 2024, 4, 107-123. https://doi.org/10.3390/youth4010008
Rao S, Dimitropoulos G, Milaney K, Eurich DT, Patten SB. HEARTS Study Protocol: Helping Enable Access and Remove Barriers To Support for Young Adults with Mental Health-Related Disabilities. Youth. 2024; 4(1):107-123. https://doi.org/10.3390/youth4010008
Chicago/Turabian StyleRao, Sandy, Gina Dimitropoulos, Katrina Milaney, Dean T. Eurich, and Scott B. Patten. 2024. "HEARTS Study Protocol: Helping Enable Access and Remove Barriers To Support for Young Adults with Mental Health-Related Disabilities" Youth 4, no. 1: 107-123. https://doi.org/10.3390/youth4010008
APA StyleRao, S., Dimitropoulos, G., Milaney, K., Eurich, D. T., & Patten, S. B. (2024). HEARTS Study Protocol: Helping Enable Access and Remove Barriers To Support for Young Adults with Mental Health-Related Disabilities. Youth, 4(1), 107-123. https://doi.org/10.3390/youth4010008







