Spatial Analysis of Vulnerability and Social Capital in Relation to COVID-19 Mortality in the 50 States of the U.S. in the First Year of the Pandemic
Abstract
1. Introduction
2. Materials and Methods
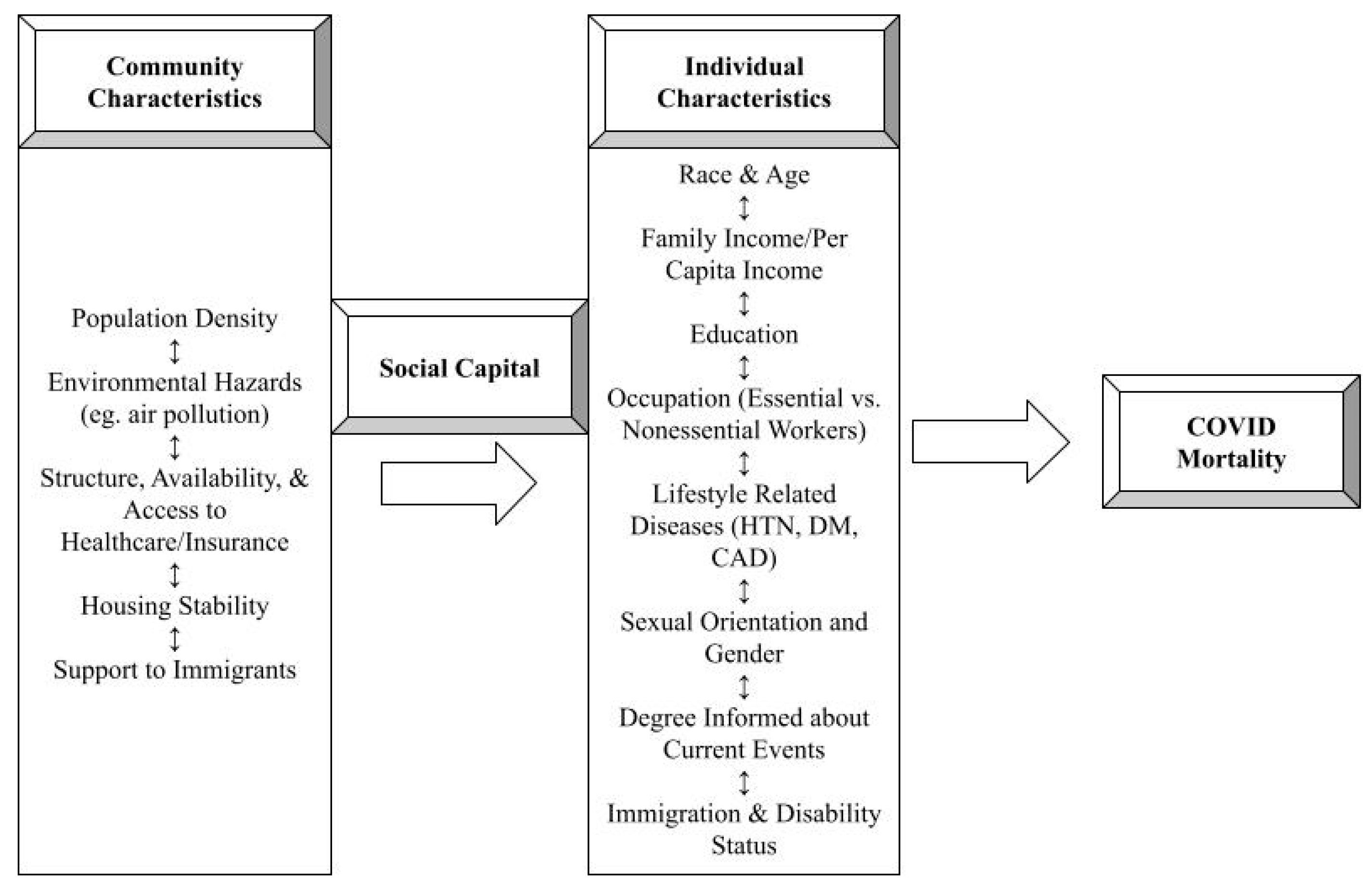
2.1. Study Design and Variables Investigated
2.2. Outcome Measure
2.3. Main Exposures
2.4. Covariates
2.5. Statistical Analysis
3. Results
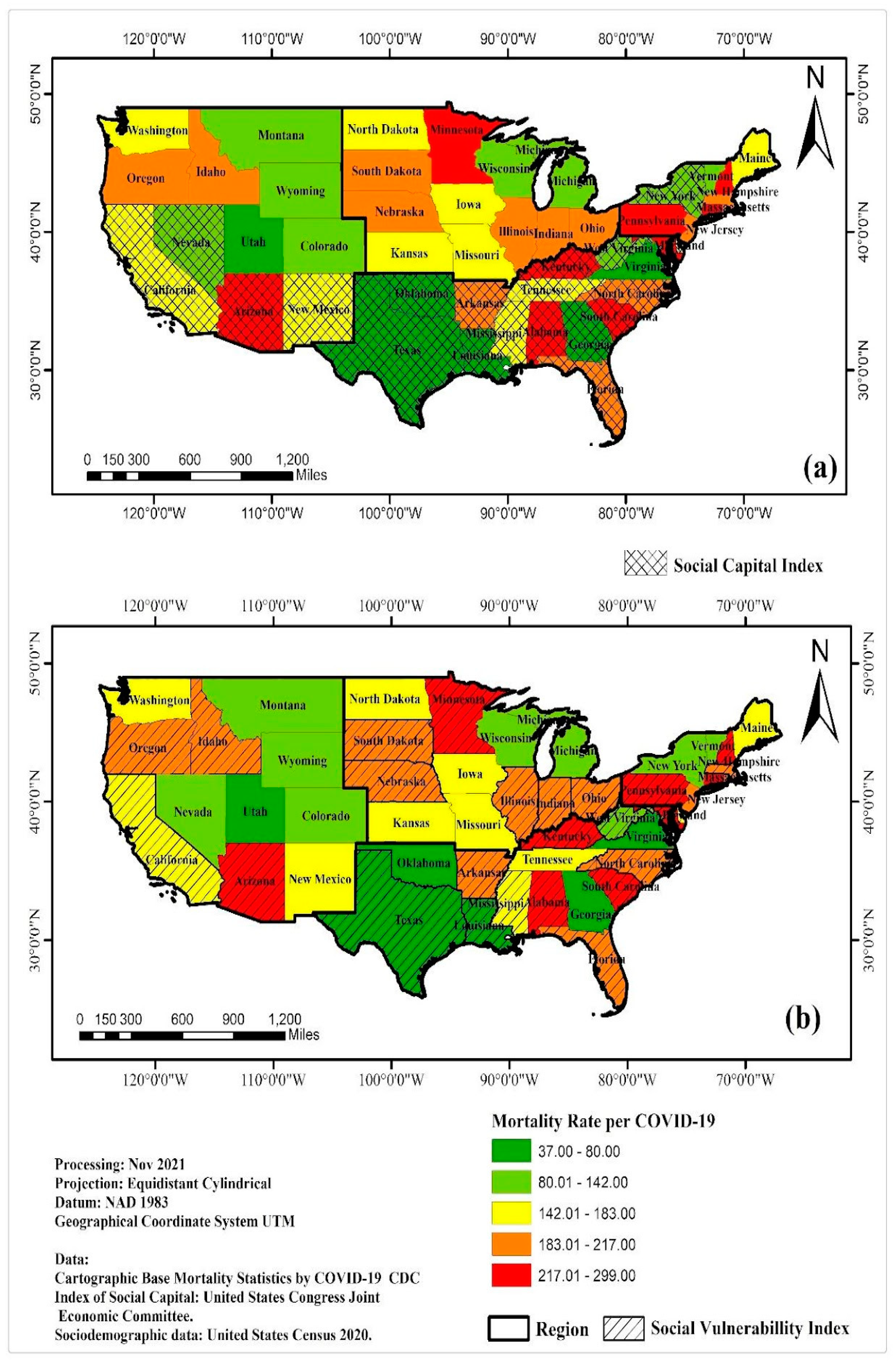
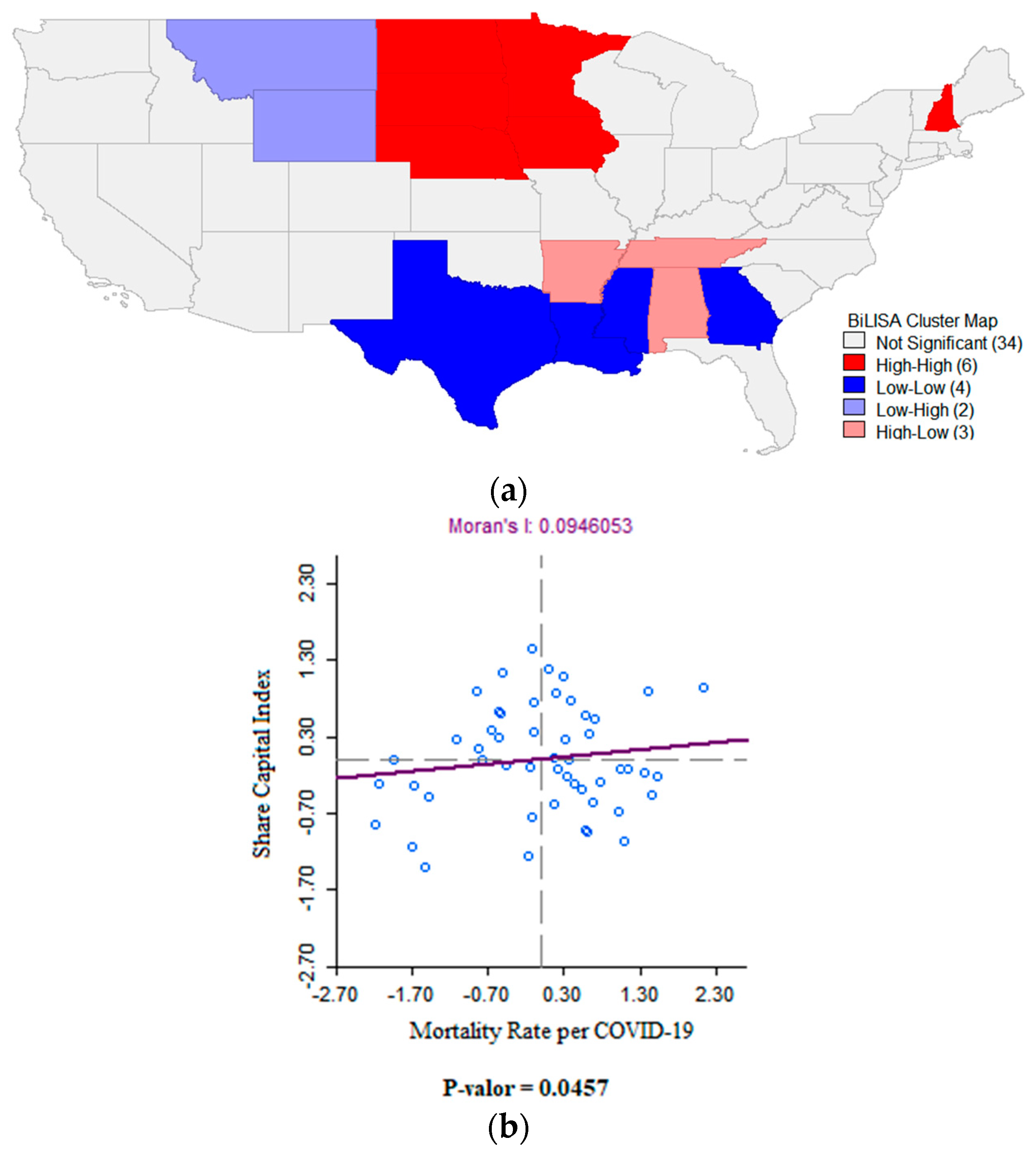
3.1. Spatial Analysis
3.2. Spatial Regression Analysis
4. Discussion
Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Martines, R.B.; Ritter, J.M.; Matkovic, E.; Gary, J.; Bollweg, B.C.; Bullock, H.; Goldsmith, C.S.; Silva-Flannery, L.; Seixas, J.N.; Reagan-Steiner, S.; et al. Pathology and Pathogenesis of SARS-CoV-2 Associated with Fatal Coronavirus Disease, United States. Emerg. Infect. Dis. 2020, 26, 2005–2015. [Google Scholar] [CrossRef]
- World Health Organization. Archived: WHO Timeline—COVID-19. 28 April 2020. Available online: https://www.who.int/news/item/27-04-2020-who-timeline---covid-19 (accessed on 5 February 2021).
- AJMC Staff. A Timeline of COVID-19 Developments in 2020. AJMC. 2021. Available online: https://www.ajmc.com/view/a-timeline-of-covid19-developments-in-2020 (accessed on 5 February 2021).
- CDC. COVID Data Tracker. Centers for Disease Control and Prevention. 2021. Available online: https://covid.cdc.gov/covid-data-tracker/#cases_totaldeaths (accessed on 5 February 2021).
- Barranco, R.; Caristo, I.; Spigno, F.; Ponzano, M.; Trevisan, A.; Signori, A.; Di Biagio, A.; Ventura, F. Management of the Medico-Legal Dispute of Healthcare-Related SARS-CoV-2 Infections: Evaluation Criteria and Case Study in a Large University Hospital in Northwest Italy from 2020 to 2021. Int. J. Environ. Res. Public Health 2022, 19, 16764. [Google Scholar] [CrossRef]
- Kelly, A. COVID-19 and medical litigation: More than just the obvious. Emerg. Med. Australas. 2020, 32, 703–705. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sepandi, M.; Taghdir, M.; Alimohamadi, Y.; Afrashteh, S.; Hosamirudsari, H. Factors Associated with Mortality in COVID-19 Patients: A Systematic Review and Meta-Analysis. Iran. J. Public Health 2020, 49, 1211–1221. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Brown, J.C.; Gerhardt, T.E.; Kwon, E. Risk Factors For Coronary Artery Disease. StatPearls Publishing. January 2021. Available online: https://www.ncbi.nlm.nih.gov/books/NBK554410/ (accessed on 11 February 2021).
- Centers for Disease Control and Prevention. Heart Disease Facts. Available online: https://www.cdc.gov/heart-disease/about/index.html (accessed on 11 February 2021).
- Centers for Disease Control and Prevention. Know Your Risk for Heart Disease. 9 December 2019. Available online: https://www.cdc.gov/heart-disease/risk-factors/index.html (accessed on 11 February 2021).
- Kreatsoulas, C.; Anand, S.S. The impact of social determinants on cardiovascular disease. Can. J. Cardiol. 2010, 26, 8C–13C. [Google Scholar] [CrossRef]
- Hendren, N.S.; de Lemos, J.A.; Ayers, C.; Das, S.R.; Rao, A.; Carter, S.; Rosenblatt, A.; Walchok, J.G.; Omar, W.; Khera, R.; et al. Association of Body Mass Index and Age With Morbidity and Mortality in Patients Hospitalized With COVID-19. Circulation 2021, 143, 135–144. [Google Scholar] [CrossRef]
- Tartof, S.Y.; Qian, L.; Hong, V.; Wei, R.; Nadjafi, R.F.; Fischer, H.; Li, Z.; Shaw, S.F.; Caparosa, S.L.; Nau, C.L.; et al. Obesity and Mortality Among Patients Diagnosed With COVID-19: Results From an Integrated Health Care Organization. Ann. Intern. Med. 2020, 173, 773–781. [Google Scholar] [CrossRef]
- Zaki, N.; Alashwal, H.; Ibrahim, S. Association of hypertension, diabetes, stroke, cancer, kidney disease, and high-cholesterol with COVID-19 disease severity and fatality: A systematic review. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1133–1142. [Google Scholar] [CrossRef]
- Jin, J.; Agarwala, N.; Kundu, P.; Harvey, B.; Zhang, Y.; Wallace, E.; Chatterjee, N. Individual and community-level risk for COVID-19 mortality in the United States. Nat. Med. 2021, 27, 264–269. [Google Scholar] [CrossRef]
- Statista. U.S.—Seniors as a Percentage of the Population 1950–2050. 20 January 2021. Available online: https://www.statista.com/statistics/457822/share-of-old-age-population-in-the-total-us-population/ (accessed on 16 February 2021).
- Mikami, T.; Miyashita, H.; Yamada, T.; Harrington, M.; Steinberg, D.; Dunn, A.; Siau, E. Risk Factors for Mortality in Patients with COVID-19 in New York City. J. Gen. Intern. Med. 2020, 36, 17–26. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tian, T.; Zhang, J.; Hu, L.; Jiang, Y.; Duan, C.; Li, Z.; Wang, X.; Zhang, H. Risk factors associated with mortality of COVID-19 in 3125 counties of the United States. Infect. Dis. Poverty 2021, 10, 3. [Google Scholar] [CrossRef]
- CDC. Cases, Data, and Surveillance. Centers for Disease Control and Prevention. 2020. Available online: https://data.cdc.gov/Case-Surveillance/COVID-19-Case-Surveillance-Public-Use-Data/vbim-akqf/about_data (accessed on 16 February 2021).
- Kawachi, I.; Kennedy, B.P.; Lochner, K.; Prothrow-Stith, D. Social capital, income inequality, and mortality. Am. J. Public Health 1997, 87, 1491–1498. [Google Scholar] [CrossRef]
- World Health Organization. Q&A Detail. 7 May 2013. Available online: https://www.who.int/news-room/q-a-detail/social-determinants-of-health-key-concepts (accessed on 16 February 2021).
- Joshi, R.; Jan, S.; Wu, Y.; MacMahon, S. Global inequalities in access to cardiovascular health care. J. Am. Coll. Cardiol. 2008, 52, 1817–1825. [Google Scholar] [CrossRef]
- Levenson, J.W.; Skerrett, P.J.; Gaziano, J.M. Reducing the global burden of cardiovascular disease: The role of risk factors. Prev. Cardiol. 2002, 5, 188–199. [Google Scholar] [CrossRef] [PubMed]
- Fielding-Miller, R.K.; Sundaram, M.E.; Brouwer, K. Social determinants of COVID-19 mortality at the county level. PLoS ONE 2020, 15, e0240151. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Office of the Assistant Secretary For Planning and Evaluation. 2020 Poverty Guidelines. ASPE. 2 January 2020. Available online: https://aspe.hhs.gov/2020-poverty-guidelines (accessed on 18 February 2021).
- Seligman, B.; Ferranna, M.; Bloom, D.E. Social determinants of mortality from COVID-19: A simulation study using NHANES. PLoS Med. 2021, 18, e1003490. [Google Scholar] [CrossRef]
- United States Census Bureau. U.S. Census Bureau QuickFacts: United States. Census Bureau QuickFacts. 2019. Available online: https://www.census.gov/quickfacts/ (accessed on 23 February 2021).
- Centers for Disease Control and Prevention. Cases, Data, and Surveillance. 2020. Available online: https://www.cdc.gov/covid/php/surveillance/index.html (accessed on 2 December 2021).
- Andrasfay, T.; Goldman, N. Association of the COVID-19 Pandemic With Estimated Life Expectancy by Race/Ethnicity in the United States, 2020. JAMA Netw. Open 2021, 4, e2114520. [Google Scholar] [CrossRef]
- Hayes-Bautista, D.E.; Hsu, P.; Hernández, G.D.; UCLA Health. The Surge of Summer Through Winter, 2020–2021: COVID-19 Burned Through California’s Latino Population. 2021. Available online: https://www.uclahealth.org/sites/default/files/documents/Report-13_The-Surge-of-Summer-through-Winter-2020-2021-COVID-19-Burned-Through-Californias-Latino-Population_March-2021.pdf?f=e1e5ce6c (accessed on 23 February 2021).
- Laurencin, C.T.; McClinton, A. The COVID-19 Pandemic: A Call to Action to Identify and Address Racial and Ethnic Disparities. J. Racial Ethn. Health Disparities 2020, 7, 398–402. [Google Scholar] [CrossRef]
- Vallejos, N.B. El capital social como determinante de salud pública [Social capital as a determinant of public health]. Rev. de Calid. Asist. 2017, 32, 342–346. [Google Scholar] [CrossRef] [PubMed]
- Office of Disease Prevention and Health Promotion. Social Determinants of Health. Healthy People 2020. 2014. Available online: https://www.cdc.gov/nchs/healthy_people/hp2020.htm (accessed on 5 April 2020).
- Kawachi, I.; Kennedy, B.P.; Glass, R. Social capital and self-rated health: A contextual analysis. Am. J. Public Health 1999, 89, 1187–1193. [Google Scholar] [CrossRef]
- Bourdieu, P. The forms of capital. In Handbook of Theory and Research for the Sociology of Education; Richardson, J.G., Ed.; Greenwood Press: New York, NY, USA, 1986; pp. 241–258. [Google Scholar]
- Coleman, J.S. Social capital in the creation of human capital. Am. J. Sociol. 1988, 94, S95–S120. [Google Scholar] [CrossRef]
- Putnam. Social Capital. Stanford. Available online: https://cs.stanford.edu/people/eroberts/cs181/projects/effect-on-interpersonal-skills/Rec4.htm#:%7E:text=Putnam%20describes%20social%20capital%20as,in%20community%20activities%20and%20associations (accessed on 5 March 2021).
- Grootaert, C.; Narayan, D.; Jones, V.N.; Woolcock, M. Measuring Social Capital: An Integrated Questionnaire; World Bank: Washington, DC, USA, 2004. [Google Scholar]
- Campos, A.C.V.; Borges, C.M.; Vargas, A.M.D.; Gomes, V.E.; Lucas, S.D.; e Ferreira, E.F. Measuring social capital through multivariate analyses for the IQ-SC. BMC Res. Notes 2015, 8, 11. [Google Scholar] [CrossRef]
- United States Joint Congress Economic Committee. The Geography of Social Capital in America. 11 April 2018. Available online: https://www.jec.senate.gov/public/index.cfm/republicans/2018/4/the-geography-of-social-capital-in-america (accessed on 11 February 2021).
- Kouvonen, A.; Kivimäki, M.; Vahtera, J.; Oksanen, T.; Elovainio, M.; Cox, T.; Virtanen, M.; Pentti, J.; Cox, S.J.; Wilkinson, R.G. Psychometric evaluation of a short measure of social capital at work. BMC Public Health 2006, 6, 251. [Google Scholar] [CrossRef]
- Paiva, P.C.P.; De Paiva, H.N.; de Oliveira Filho, P.M.; Lamounier, J.A.; e Ferreira, E.F.; Ferreira, R.C.; Kawachi, I.; Zarzar, P.M. Development and Validation of a Social Capital Questionnaire for Adolescent Students (SCQ-AS). PLoS ONE 2014, 9, e103785. [Google Scholar] [CrossRef]
- Rostila, M. The Facets of Social Capital. J. Theory Soc. Behav. 2011, 41, 308–326. [Google Scholar] [CrossRef]
- Arachchi, J.I.; Managi, S. The role of social capital in COVID-19 deaths. BMC Public Health 2021, 21, 434. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Elgar, F.J.; Stefaniak, A.; Wohl, M.J. The trouble with trust: Time-series analysis of social capital, income inequality, and COVID-19 deaths in 84 countries. Soc. Sci. Med. 2020, 263, 113365. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Makridis, C.A.; Wu, C. Correction: How social capital helps communities weather the COVID-19 pandemic. PLoS ONE 2021, 16, e0258021. [Google Scholar] [CrossRef]
- Bargain, O.; Aminjonov, U. Trust and compliance to public health policies in times of COVID-19. J. Public Econ. 2020, 192, 104316. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Murayama, H.; Nakamoto, I.; Tabuchi, T. Social Capital and COVID-19 Deaths: An Ecological Analysis in Japan. Int. J. Environ. Res. Public Health 2021, 18, 10982. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Borgonovi, F.; Andrieu, E.; Subramanian, S. The evolution of the association between community level social capital and COVID-19 deaths and hospitalizations in the United States. Soc. Sci. Med. 2021, 278, 113948. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yanagisawa, M.; Kawachi, I.; Scannell, C.A.; Oronce, C.I.A.; Tsugawa, Y. Association between county-level social capital and the burden of COVID-19 cases and deaths in the United States. Ann. Epidemiol. 2021, 59, 21–23. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Matrajt, L.; Leung, T. Evaluating the Effectiveness of Social Distancing Interventions to Delay or Flatten the Epidemic Curve of Coronavirus Disease. Emerg. Infect. Dis. 2020, 26, 1740–1748. [Google Scholar] [CrossRef]
- Ebell, M.H.; Bagwell-Adams, G. Mandatory Social Distancing Associated With Increased Doubling Time: An Example Using Hyperlocal Data. Am. J. Prev. Med. 2020, 59, 140–142. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. COVID Data Tracker 2020. 28 March. Available online: https://covid.cdc.gov/covid-data-tracker/#cases_deathsper100k (accessed on 2 April 2022).
- State Fact Sheets. USDA ERS—State Fact Sheets. 1 November 2021. Available online: https://www.ers.usda.gov/data-products/state-fact-sheets/. (accessed on 14 November 2021).
- Population Distribution by Sex. KFF. 23 October 2020. Available online: https://www.kff.org/other/state-indicator/distribution-by-sex/?currentTimeframe=0&sortModel=%7B%22colId%22%3A%22Location%22%2C%22sort%22%3A%22asc%22%7D (accessed on 14 November 2021).
- Federal Reserve Bank of St. Louis. Federal Reserve Economic Data: Fred: St. Louis Fed. FRED. Available online: https://fred.stlouisfed.org/?gclid=Cj0KCQiAhMOMBhDhARIsAPVml-Fk0_6rmz9IlDHT95yTWvXe4SBVD8gce30_3JkfSh1zeXMRtu1bR88aAgWlEALw_wcB. (accessed on 14 November 2021).
- U.S. Immigrant Population by State and County. Migrationpolicy.Org. 26 March 2021. Available online: https://www.migrationpolicy.org/programs/data-hub/charts/us-immigrant-population-state-and-county (accessed on 14 November 2021).
- United States Census Bureau. Small Area Health Insurance Estimates. Available online: https://www.census.gov/programs-surveys/sahie.html (accessed on 14 November 2021).
- Moran, P.A.P. The interpretation of statistical maps. J. R. Stat. Soc. B 1948, 10, 243–251. [Google Scholar] [CrossRef]
- Borges, C.M.; Pollock, J.C.; Crowley, M.; Purandare, R.; Sparano, J.; Spike, K. Social capital or vulnerability: Which has the stronger connection with selected U.S. health outcomes? SSM-Popul. Health 2021, 15, 100812. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hawkins, R.; Charles, E.; Mehaffey, J. Socio-economic status and COVID-19–related cases and fatalities. Public Health 2020, 189, 129–134. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Núñez-Cortés, R.; Ortega-Palavecinos, M.; Soto-Carmona, C.; Torres-Gangas, P.; Concha-Rivero, M.P.; Torres-Castro, R. Social determinants of health associated with severity and mortality in patients with COVID-19. Gac. Medica Mex. 2023, 157, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Vásquez, A.; Gamboa-Unsihuay, J.E.; Vargas-Fernández, R.; Azañedo, D. Exceso de mortalidad en Lima Metropolitana durante la pandemia de COVID-19: Comparación a nivel distrital [Excess mortality in Metropolitan Lima during the COVID-19 pandemic: A district level comparison]. Medwave 2020, 20, e8032. [Google Scholar] [CrossRef]
- Baggio, J.A.O.; Machado, M.F.; Carmo, R.F.D.; Armstrong, A.d.C.; dos Santos, A.D.; de Souza, C.D.F. COVID-19 in Brazil: Spatial risk, social vulnerability, human development, clinical manifestations and predictors of mortality—A retrospective study with data from 59 695 individuals. Epidemiol. Infect. 2021, 149, e100. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, M.L.; Behrman, P.; Dulin, A.; Baskin, M.L.; Buscemi, J.; I Alcaraz, K.; Goldstein, C.M.; Carson, T.L.; Shen, M.; Fitzgibbon, M. Addressing inequities in COVID-19 morbidity and mortality: Research and policy recommendations COMMENT. Transl. Behav. Med. 2020, 10, 516–519. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Islam, N.; Lacey, B.; Shabnam, S.; Erzurumluoglu, A.M.; Dambha-Miller, H.; Chowell, G.; Kawachi, I.; Marmot, M. Social inequality and the syndemic of chronic disease and COVID-19: County-level analysis in the USA. J. Epidemiol. Community Health 2021, 75, 496–500. [Google Scholar] [CrossRef] [PubMed]
- Fraser, T.; Aldrich, D.P.; Page-Tan, C. Bowling Alone or Masking Together? The Role of Social Capital in Excess Death Rates from COVID-19. Soc. Sci. Med. 2020, 284, 114241. [Google Scholar] [CrossRef] [PubMed]
- Varshney, L.R.; Socher, R. COVID-19 growth rate decreases with social capital. medRxiv 2020. [Google Scholar] [CrossRef]
- Bartscher, A.K.; Seitz, S.; Siegloch, S.; Slotwinski, M.; Wehrhöfer, N. Social capital and the spread of COVID-19: Insights from European countries. J. Health Econ. 2021, 80, 102531. [Google Scholar] [CrossRef]
- Fraser, T.; Aldrich, D.P. The dual effect of social ties on COVID-19 spread in Japan. Sci. Rep. 2021, 11, 1596. [Google Scholar] [CrossRef]
- Rodgers, J.; Valuev, A.V.; Hswen, Y.; Subramanian, S. Social capital and physical health: An updated review of the literature for 2007–2018. Soc. Sci. Med. 2019, 236, 112360. [Google Scholar] [CrossRef] [PubMed]
- Duh-Leong, C.; Dreyer, B.P.; Huang, T.T.-K.; Katzow, M.; Gross, R.S.; Fierman, A.H.; Tomopoulos, S.; Di Caprio, C.; Yin, H.S. Social Capital as a Positive Social Determinant of Health: A Narrative Review. Acad. Pediatr. 2021, 21, 594–599. [Google Scholar] [CrossRef]
- Morelli, V. Social Determinants of Health: An Overview for the Primary Care Provider. Prim. Care Clin. Off. Pract. 2023, 50, 507–525. [Google Scholar] [CrossRef]
- Buehler, J.W.; Castro, J.C.; Cohen, S.; Zhao, Y.; Melly, S.; Moore, K. Personal and Neighborhood Attributes Associated with Cervical and Colorectal Cancer Screening in an Urban African American Population. Prev. Chronic Dis. 2019, 16, E118. [Google Scholar] [CrossRef]
- Thiam, Y.; Allaire, J.-F.; Morin, P.; Hyppolite, S.-R.; Doré, C.; Zomahoun, H.T.V.; Garon, S. A Conceptual Framework for Integrated Community Care. Int. J. Integr. Care 2021, 21, 5. [Google Scholar] [CrossRef] [PubMed]
- Tian, C.Y.; Xu, R.H.; Mo, P.K.-H.; Dong, D.; Wong, E.L.-Y. Generic Health Literacy Measurements for Adults: A Scoping Review. Int. J. Environ. Res. Public Health 2020, 17, 7768. [Google Scholar] [CrossRef] [PubMed]
- Wu, C. Social capital and COVID-19: A multidimensional and multilevel approach. Chin. Sociol. Rev. 2021, 53, 27–54. [Google Scholar] [CrossRef]
- Borgonovi, F.; Andrieu, E. Bowling together by bowling alone: Social capital and COVID-19. Soc. Sci. Med. 2020, 265, 113501. [Google Scholar] [CrossRef] [PubMed]
- Hao, F.; Shao, W.; Huang, W. Understanding the influence of contextual factors and individual social capital on American public mask wearing in response to COVID–19. Health Place 2021, 68, 102537. [Google Scholar] [CrossRef]
- Palanisamy, B.; Gopichandran, V.; Kosalram, K. Social capital, trust in health information, and acceptance of Measles–Rubella vaccination campaign in Tamil Nadu: A case-control study. J. Postgrad. Med. 2018, 64, 212–219. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Andrade-Molina, D.M.; Fernández-Cadena, J.C.; Fernandez, M.A.; Rhodes, L.A.; Sánchez, G.E. I’ll be good for grandma: Institutional and relational trust and COVID-19 restriction compliance. Econ. Pap. A J. Appl. Econ. Policy 2023, 42, 172–182. [Google Scholar] [CrossRef]
| Dimension Name | Dimension Description |
|---|---|
| Family Unity | Family Unity was measured by the following statistics:
|
| Family Interaction | Family Interaction was measured by the following statistics:
|
| Social Support | Social Support was measured by the following statistics:
|
| Community Health | Community Health was measured by the following statistics:
|
| Institutional Health | Institutional health was measured by the following statistics:
|
| Collective Efficacy | Collective efficacy was measured by violent crimes per 100,000 inhabitants. |
| Philanthropic Health | Philanthropic Health was measured by those who report having made a donation of >USD 25 to a charitable group in the past year. |
| Variables | Description | Year |
|---|---|---|
| % female | Percentage of the state population that is female. | 2019 |
| Population per square mile | Number of people per square mile. | 2010 |
| % of population born in a foreign country | Numerator: number of foreign born persons. Denominator: total population. Multiplier: 100. | 2015–2019 |
| Unemployment rate | Numerator: number of unemployed people. Denominator: total population. Multiplier: 100. | 2019 |
| % of children in families that receive public assistance | Numerator: number of children that receive public assistance. Denominator: total number of children in that same state. Multiplier: 100. | 2019 |
| % of persons aged 25+ years that are high school graduates or higher | Numerator: number of people aged 25+ that graduated from high school. Denominator: total number of adults aged 25+ in the state. Multiplier: 100. | 2015–2019 |
| % of persons aged 25 years+ with a bachelor’s degree or higher | Numerator: number of people aged 25+ that graduated from a 4-year higher education program. Denominator: total number of adults aged 25+ in the state. Multiplier: 100. | 2015–2020 |
| % of residents reporting fair or poor health | Numerator: number of Behavioral Risk Factor Surveillance System (BRFSS) survey respondents in the state reporting fair or poor health. Denominator: total number of BRFSS respondents in the state. Multiplier: 100. | 2019 |
| % of population with a disability under age 65 years | Numerator: number of people under the age of 65 that have a disability. Denominator: total population under the age of 65. Multiplier: 100. | 2015–2019 |
| Prevalence of diabetes among U.S. adults ≥ 18 years | Numerator: number of cases of diabetes (type 1 or 2) among people aged ≥ 18 years. Denominator: total population ≥ 18 years. Multiplier: 100,000 | 2017 |
| Current smoking among adults aged ≥ 18 years | Numerator: number of current smokers aged ≥ 18. Denominator: total population aged ≥ 18 years. Multiplier: 100,000 | 2018 |
| Deaths per 100,000 due to influenza/pneumonia | Numerator: number of deaths due to influenza. Denominator: total population. Multiplier: 100,000 | 2019 |
| Binge drinking among adults ≥ 18 years | Numerator: number of men ≥18 who consume 5 or more drinks in about 2 h or women ≥18 who consume 4 or more drinks in about 2 h. Denominator: Total population aged ≥18. | 2018 |
| Coronary heart disease deaths per 100,000 U.S. adults ≥ 18 years | Numerator: number of people diagnosed with CHD aged ≥ 18. Denominator: total population aged ≥ 18 years. Multiplier: 100,000. | 2017 |
| CVA deaths per 100,000 U.S. adults (18+) | Numerator: number of people who died of CVA aged ≥18. Denominator: total population aged ≥ 18 years. Multiplier: 100,000. | 2017 |
| Prevalence of two or more chronic conditions among Medicare-enrolled persons aged ≥ 65 | Numerator: number of people diagnosed with ≥ 2 chronic conditions among Medicare-enrolled persons aged ≥ 65. Denominator: total Medicare-enrolled persons aged ≥ 65. | 2015 |
| Median household income | Defined as the median income of a householder plus the income of all individuals 15 years or older. | 2019 |
| % adult obesity | Numerator: number of adults with BMI ≥ 30. Denominator: total adult population. Multiplier: 100. | 2019 |
| % obesity Asian alone | Numerator: number of Asian adults with BMI ≥ 30. Denominator: total adult population. Multiplier: 100. | 2019 |
| % obesity Black/African American alone | Numerator: number of Black/African American adults with BMI ≥ 30. Denominator: total adult population. Multiplier: 100. | 2019 |
| % obesity non-Hispanic white alone | Numerator: number of non-Hispanic white American adults with BMI ≥ 30. Denominator: total adult population. Multiplier: 100. | 2019 |
| % obesity Hispanic or Latino | Numerator: number of Hispanic or Latino adults with BMI ≥ 30. Denominator: total adult population. Multiplier: 100. | 2019 |
| % population in poverty | The Census Bureau uses a set of income thresholds that vary by family size and composition to determine who is in poverty. If a family’s total income is less than the threshold, then that family and every individual in it is considered in poverty. | 2019 |
| % persons without health insurance under 65 years | Numerator: number of persons without health insurance under 65 years. Denominator: total population under 65 years. Multiplier: 100. | 2018 |
| % rural inhabitants | Numerator: number of people living in rural areas in the state. Denominator: total population in the state. Multiplier: 100. | 2010 |
| % internet subscription | Numerator: number of households with broadband internet subscription. Denominator: total number of households. Multiplier: 100. | 2015–2019 |
| % birth to unmarried women | Numerator: number of births to unmarried women. Denominator: number of total births. Multiplier: 100. | 2019 |
| Average county % of population with ≥3 risk factors for COVID-19 mortality | The Community Resilience Estimates (CRE) groups the population estimates into 3 categories: 0 risk factors, 1–2 risk factors, and 3 plus risk factors. The data file includes the population estimate, estimate margin of error, rate, and rate margin of error for each of the 3 categories. | 2014 |
| Region | Population 1 | Mortality Rate COVID-19 | Number of States 1 | ||
|---|---|---|---|---|---|
| Low (%) | Medium (%) | High (%) | |||
| Midwest | 68,329,004 | 3 (23.08) | 2 (13.33) | 7 (30.43) | 12 |
| Northeast | 56,688,552 | 5 (38.46) | 3 (20.00) | 2 (8.70) | 10 |
| South | 124,874,699 | 3 (23.08) | 2 (13.33) | 11 (47.83) | 16 |
| West | 78,347,268 | 2 (15.38) | 8 (53.33) | 3 (13.04) | 13 |
| Total | 328,239,523 | 13 (25.49) | 15(29.41) | 23(45.10) | 51 |
| Source: DCEU/CDC. | |||||
| Coefficients | Standard Deviation | t | p-Value | |
|---|---|---|---|---|
| (Constant) | 77.037 | 23.036 | 3.344 | 0.002 |
| Social Capital Index | 23.256 | 8.780 | 2.649 | 0.011 |
| Social Vulnerability Index | 150.316 | 35.492 | 4.235 | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borges, C.M.; Conlan, M.; Khateeb, A.; Tomczynski, E. Spatial Analysis of Vulnerability and Social Capital in Relation to COVID-19 Mortality in the 50 States of the U.S. in the First Year of the Pandemic. Hygiene 2025, 5, 1. https://doi.org/10.3390/hygiene5010001
Borges CM, Conlan M, Khateeb A, Tomczynski E. Spatial Analysis of Vulnerability and Social Capital in Relation to COVID-19 Mortality in the 50 States of the U.S. in the First Year of the Pandemic. Hygiene. 2025; 5(1):1. https://doi.org/10.3390/hygiene5010001
Chicago/Turabian StyleBorges, Carolina Marques, Matthew Conlan, Areeb Khateeb, and Emma Tomczynski. 2025. "Spatial Analysis of Vulnerability and Social Capital in Relation to COVID-19 Mortality in the 50 States of the U.S. in the First Year of the Pandemic" Hygiene 5, no. 1: 1. https://doi.org/10.3390/hygiene5010001
APA StyleBorges, C. M., Conlan, M., Khateeb, A., & Tomczynski, E. (2025). Spatial Analysis of Vulnerability and Social Capital in Relation to COVID-19 Mortality in the 50 States of the U.S. in the First Year of the Pandemic. Hygiene, 5(1), 1. https://doi.org/10.3390/hygiene5010001






