Abstract
This study assessed knowledge, attitudes, and practices related to food hygiene among mothers from Malawi’s rural communities against the WHO Five Keys to Safer Food (WHO-FKSF) and good pre-and post-harvest practices (GPPHPs) as reference points. Five hundred twenty-two mothers from six rural communities across two districts were selected for the survey. The results indicated limited knowledge among participating mothers regarding managing food hazards, including mycotoxins, bacteria, viruses, and parasites (BVPs). A significant proportion (89.5%) of women reported inconsistent or no handwashing with soap after using the toilet. In addition, 48.7% failed to plant with the first good rains, 38.7% neglected to check for moldy cobs during harvesting, 57.4% dried maize on bare soil, and 99.2% bought maize with noticeable mold. Higher education, knowledge, and positive attitudes were associated with enhanced BVP control practices, while larger households and positive attitudes were linked to improved mold/mycotoxin management (p < 0.05). Mothers showed lower (p < 0.05) knowledge and attitude levels regarding molds than BVPs but demonstrated relatively better practices for mold control. A comprehensive education program based on the WHO Five Keys to Safer Foods, tailored to local socio-cultural norms and incorporating mold and mycotoxin management guidelines, is recommended.
1. Introduction
Food contamination remains a significant and recurring challenge to global public health, leading to morbidity and mortality. The 2010 estimates from the Foodborne Epidemiology Reference Group (FERG) of the World Health Organization (WHO) on the global impact of foodborne diseases (FBDs) highlight millions of deaths and disability-adjusted life years (DALYs) linked to these conditions [1]. FERG suggests that the global burden of illnesses due to food safety issues is comparable to that of malaria and tuberculosis. However, it is argued that the true impact of foodborne diseases may be even more significant than FERG estimates suggest [2]. To address this concern, a process to update these estimates was announced in 2021, with an expected completion date in 2025 [3].
The burden of foodborne diseases (FBDs) is particularly severe in regions such as Asia and Africa and among vulnerable demographics, especially children [1]. In these areas, the tropical and subtropical climates create favorable conditions for the proliferation of pathogenic microorganisms, including bacteria, viruses, and parasites (BVPs) [4,5]. Additionally, mycotoxins—harmful compounds produced by certain fungi that thrive particularly well in these climates—can contaminate food and pose serious health risks, such as poisoning, immune suppression, and cancer [6]. Implementing comprehensive Good Pre- and Post-Harvest Practices (GPPHPs) is crucial to mitigate these risks. Pre-harvest strategies, such as selecting resistant crop varieties and effective pest management, along with post-harvest practices, such as proper drying and storage, can significantly reduce mycotoxin contamination to safe levels, thereby protecting consumer health [7]. However, food safety often takes a backseat to food and nutrition security concerns, primarily because of persistent food shortages in these regions [8].
FBDs primarily result from deficiencies in food safety practices within households, and they are preventable when food safety guidelines are diligently adhered to throughout the entire production-to-consumption continuum [9,10]. The domestic kitchen has been characterized as the ‘front line’ in the ongoing effort to combat foodborne diseases (FBDs), highlighting its critical role in this battle [9]. The actions of a household food handler are also pivotal, as they can either exacerbate or mitigate the risk of FBDs within the household, particularly when preparing food for vulnerable populations such as infants and young children.
In 2001, the WHO launched the “Five Keys to Safer Food” (FKSF) manual, aimed at reducing the burden of foodborne diseases (FBDs) [11]. This manual offers straightforward recommendations to enhance food safety. These recommendations are accompanied by actionable (practical) steps detailing how to effectively implement each of the five key principles supported with specific evidence. The core messages of the Five Keys to Safer Food are: (1) Keep clean; (2) Separate raw and cooked; (3) Cook thoroughly; (4) Keep food at safe temperatures; (5) Use safe water and raw materials. Since then, the Five Keys to Safer Food manual has been translated into different languages to facilitate the spread of this message.
In Sub-Saharan Africa (SSA), the central role of female household members in reducing the burden of FBDs cannot be overstated. They serve as principal food handlers, assuming responsibilities spanning food cultivation, procurement, storage, and preparation. More research must address the knowledge, attitudes, and practices related to food safety among women and girls residing in rural subsistence settings of SSA households. Hence, this study aimed to examine the prevailing knowledge, attitudes, and practices associated with food safety, specifically focusing on BVP, molds, and mycotoxins. This study focused on mothers and pregnant women in rural Malawi, with Central Malawi (Salima and Dedza districts) as case study locations. This study also investigated the relationship between socioeconomic factors and food hygiene practices. The insights gleaned from this study will establish a foundational dataset crucial for designing a comprehensive food safety education program tailored to rural subsistence settings characterized by similar socio-economic structures.
2. Materials and Methods
2.1. Study Design and Setting
A community-based cross-sectional survey was conducted from November to December 2019. This survey was conducted in three traditional authorities (TAs), sub-divisions of a district consisting of villages in the Salima and Dedza districts (Figure 1). All six TAs are situated in rural areas and fall within the purview of the Deutsche Gesellschaft fuer Internationale Zusammenarbeit (GIZ)-Food and Nutrition Security Programme (FNSP). The FNSP is integral to the global GIZ initiative ‘One World–No Hunger’ and aligns with Malawi’s national ‘Scaling up Nutrition’ initiative. The primary objective of these initiatives is to combat malnutrition in Malawi with a specific focus on pregnant and lactating women (PLW), infants, and young children. Implementation is carried out through collaborative efforts involving CARE International, United Purpose, Village Reach, and Welthungerhilfe. The program employs a care group approach, which involves empowering identified lead mothers (cluster leaders) to disseminate information and support to 12–16 women within their proximity [12]. These cluster leaders undergo training facilitated by a promoter overseeing up to nine Care Groups.
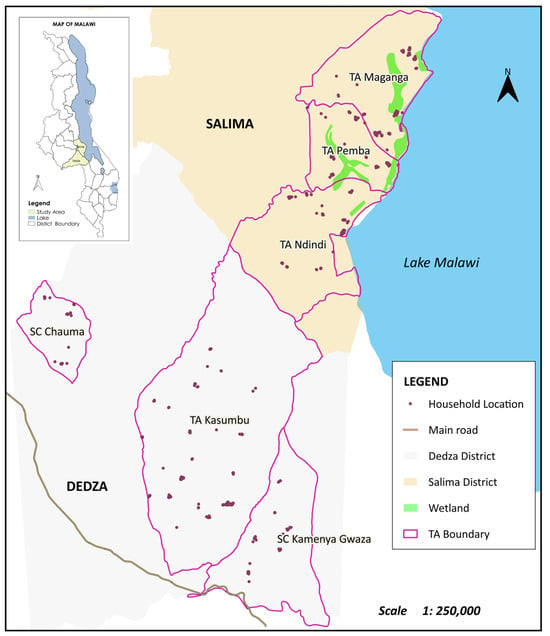
Figure 1.
Map showing study areas in Dedza and Salima.
2.2. Study Population
This study included all mothers residing in the selected TAs during the data collection period, except for critically ill mothers. A list of eligible households was compiled using information from the community health workers’ register, locally known as Disease Control and Surveillance Assistants (DCSAs). This list included households with children aged between 6 and 24 months who had access to a pit latrine and safe water within 500 m.
2.3. Sample Size Determination and Sampling Procedure
The sample size for this study was determined by using a single population proportion formula (Equation (1)) while considering specific assumptions. These assumptions included a prevalence of 85% for women’s attitude towards observing personal cleanliness while cooking food in Dedza district, Malawi, after an intervention [13], a 95% level of confidence, and a 5% margin of error.
The formula used for sample size calculation is as follows:
where N represents the required sample size, α is the level of significance, z is the standard normal distribution curve value for a 95% confidence level (1.96), p represents the women’s attitude towards observing personal cleanliness during cooking food, and d stands for the margin of error. Considering a design effect of 2 (multistage sampling), a 10% non-response rate, and missing data, the minimum adequate sample size was 522.
N = ((z(α⁄2))2 p(1 − p))/d2 = ((1.96)2 (0.85)(0.15))/[(0.05)]2 = 196
To select study participants, a multistage sampling technique was employed to ensure a more representative sample. In the first stage, villages were randomly selected in proportion to their population from the six TAs. In the second stage, households within each sampled village were chosen through a systematic sampling approach, specifically selecting every 5th household. Additionally, to reach a minimum sample size of 30, at least five care group promoters were conveniently sampled from each of the six TAs. This multistage approach allowed the capture of a diverse and representative population cross-section, enhancing the findings’ reliability and generalizability.
2.4. Data Collection Instrument and Method
Upon introducing themselves and explaining the purpose of their visit to each selected household, investigators sought consent to conduct interviews with mothers or pregnant women, hereafter referred to as “mothers”. Data collection was performed using a closed-ended structured questionnaire. Initially, the questionnaire was developed in the vernacular language, Chichewa, and then translated into English by a public health professional. Subsequently, another public health professional translated it back into Chichewa to ensure translation accuracy. Any discrepancies in translation were minimal and resolved by the investigators and translators. Trained enumerators conducted the survey using the validated structured questionnaire.
The questionnaire encompassed four sections, which inquired about (1) socio-demographic data, including education, household water accessibility, (2) household food insecurity access score, constructed by authors with guidance from Coates et al. [14], sanitation facilities, and conditions, (3) household assets, and (4) knowledge, attitudes, and practice regarding the WHO Five Keys to Safer Foods [11]. Questions about the respondent’s practice (behavior) were asked before those concerning knowledge and attitude to avoid providing the participants with hints of ideal hygienic behaviors.
2.5. Determination of Knowledge, Attitude, and Practice Regarding Food Safety and FBDs
Participants’ knowledge was assessed using a 3-level scale, with positively worded questions scored as follows: True (2 points), Don’t know (1 point), and False (0 points). Similarly, attitudes were evaluated on a 3-level scale, with positively worded questions scored as follows: Agree (2), Not sure (1), and Disagree (0). In contrast, hygienic practices were evaluated on a 5-level scale as follows: Always (4), Often (3), Sometimes (2), Occasionally (1), and Never (0). Scoring was reversed for negatively worded questions or unhygienic behaviors and practices. Non-applicable scenarios were treated as missing. Aggregated knowledge, attitudes, and practice test scores were individually expressed as percentages.
2.6. Statistical Analysis
Data were analyzed using the IBM Statistical Package for the Social Sciences (IBM SPSS) for Windows version 23 (IBM Corp, Armonk, NY, USA). Frequencies and percentages for categorical variables were used to describe the socio-demographic characteristics of the participants. In addition, Pearson correlation coefficients were employed to assess correlations between continuous variables. Comparisons of mean scores of knowledge, attitudes, and practice among different groups were performed using one-way analysis of variance (ANOVA). Post-hoc mean separations were conducted through Tukey’s honestly significant difference test. To test for differences in mothers’ KAP scores between BVP and molds/mycotoxins, paired sample t-tests were employed. Ordered logistic regression was used on the mothers’ practice scores to determine the independent effects of explanatory variables. The level of significance was set at p < 0.05.
3. Results
3.1. Socio-Demographic Characteristics of the Mothers
About 90% of the surveyed mothers were aged 45 or younger. Among these, 66% were married, and only 10% had education levels higher than primary school (Table 1; Supplementary Table S1). Over 80% of the participants did not hold leadership roles in the village or were affiliated with agricultural or health/nutritional groups. In addition, a significant portion of households had basic, unimproved simple pit latrines (80%) that lacked drop hole covers (41%). Semi-structured observations in this study revealed that only 10.5% of the households had functioning handwashing facilities at the toilet, and none of the surveyed households had a hand-washing facility at food preparation points. Mothers spent significant time fetching water from distant sources, with 10% reporting a minimum of 30 min for a round trip. Additionally, about 60% of the households were classified as experiencing moderate or severe food insecurity.

Table 1.
Socio-demographic characteristics of the mothers in this study’s sample (n = 522).
3.2. Knowledge Regarding BVP and Molds/Mycotoxins
Mothers exhibited knowledge gaps in critical aspects of food safety. These included misconceptions about handwashing, with 33% unaware of the insufficiency of soapless handwashing for BVP elimination (Table 2; Supplementary Table S1). The mothers exhibited a deficiency in understanding the health risks associated with consuming raw animal milk, as well as the hazards linked to exposure to infant feces. Knowledge gaps extended to factors promoting mold issues, including misunderstandings about the impact of drought. Additionally, mothers needed to be made aware of practices promoting mold growth, such as late planting and leaving crops in the field. They also needed to be made aware of the persistence of mycotoxins after standard heating and soaking of moldy grains.

Table 2.
Level of knowledge of the mothers regarding bacteria, viruses, pathogens, and molds/mycotoxins (n = 522).
3.3. Attitude of the Mothers Regarding BVPs and Moulds/Mycotoxins
The mothers highlighted several challenges of maintaining good hygiene practices, particularly in resource-limited households (Table 3; Supplementary Table S1). The findings reveal a complex interplay of attitudes shaped by cultural, ethical, and practical considerations.

Table 3.
Attitudes of the mothers regarding bacteria, viruses, and pathogens (BVPs) and molds/mycotoxins (n = 522).
3.4. Practices Regarding BVPs and Molds/Mycotoxins
Despite a significant proportion of mothers claiming consistent handwashing, soap use was infrequent, with only a tiny fraction reporting consistent soap usage (Table 4). Poor hygienic practices were also evident in various aspects, including water usage, utensil cleaning, food handling during illness, and infant feeding. Moreover, many mothers exhibited deficiencies in adhering to critical pre- and post-harvest mold prevention and management practices.

Table 4.
Practices of mothers regarding bacteria, viruses, pathogens (BVPs), and molds/mycotoxins (n = 522).
3.5. Overall Assessment of KAP of Mothers Regarding BVPs and Molds/Mycotoxins
According to the paired t-test, the mothers’ knowledge and attitude scores related to BVPs were significantly (p < 0.05) higher compared with those of molds/mycotoxins (Figure 2). However, the difference reversed for mothers’ practice levels, i.e., mothers’ practice scores related to BVPs were significantly (p < 0.05) lower than those of molds/mycotoxins.
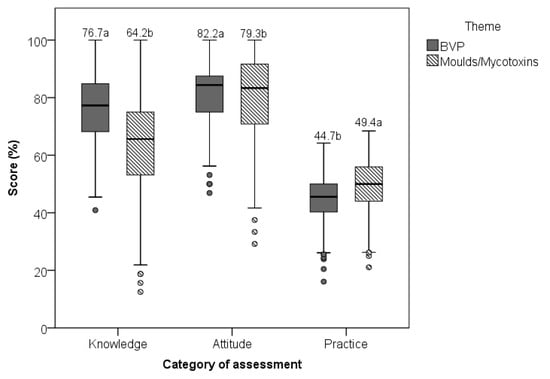
Figure 2.
The distribution and paired differences in mothers’ KAP scores between BVPs and molds/mycotoxins are being examined. The values displayed above each box represent the mean, and different letters (a and b) within each category of assessment (Knowledge, Attitude, and Practice) indicate statistically significant differences (p < 0.05) according to paired t-tests.
3.6. Determinants for Mothers’ Practices Related to BVPs and Molds/Mycotoxins
The level of education, knowledge, and attitude (related to BVPs) positively influenced practice level regarding BVP control, whereas household size and attitude levels (related to molds/mycotoxins) had a positive effect on practice level regarding molds/mycotoxin control (Table 5).

Table 5.
Factors Associated with Mother’s Practices regarding control of bacteria, viruses, and pathogens (BVPs) and control of molds/toxins.
4. Discussion
This study reveals two noteworthy findings. First, despite displaying a positive attitude towards controlling and managing BVPs and molds in food, the mothers demonstrated limited knowledge of the subject. Consequently, they engaged in various unhygienic practices. Second, the mothers exhibited lower levels of knowledge and attitudes regarding molds than BVPs. Surprisingly, they implemented more effective practices for controlling molds than BVPs.
The significantly higher proportion of the mothers in the study area who reported regular handwashing after using a toilet or changing diapers/nappies compared with those documented in other regions of the continent [15] could be attributed to the influence of the GIZ FNSP program, which is currently active in the study area. Regrettably, the hand-washing practices of these mothers may have had limited impact on disease prevention since soap was mostly not used [16,17,18,19].
The absence of functional tip-taps around toilets implies that mothers used buckets despite claiming to wash their hands regularly after using a toilet. This practice is unhygienic as individuals dip their hands in the bucket, potentially contaminating the water and increasing the risk of disease transmission.
The mothers’ reported perception that they considered it uncultured to demand soap or water for handwashing in someone’s home or public settings or to demand pouring water when everyone else is directly dipping their hands in a shared washing basin/bucket demonstrates that actual practice is influenced not only by knowledge but also by cultural taboos and social customs [20,21]. Therefore, there is a need to develop culturally acceptable behavioral interventions if the desired hygienic behaviors are to be effectively promoted and adopted.
The lower knowledge level regarding molds compared with that of BVPs among the mothers was not surprising. In Malawi, educational materials, information, and communication related to food safety predominantly focus on BVPs. This bias is likely prevalent in many parts of the world, as evidenced by the WHO Five Keys to Safer Foods [11]. While the WHO manual remains a comprehensive guide for ensuring food safety, it primarily emphasizes BVPs and offers limited actionable recommendations for addressing molds. Consequently, it might have been partly responsible for the care group promoters having lower knowledge and exhibiting less favorable behaviors concerning molds than BVPs. It is worth noting that, in recent times, there have been some initiatives in Malawi, primarily led by private sector companies, aimed at combating molds and mycotoxins, particularly in groundnuts. Unfortunately, these efforts have mainly focused on products intended for export rather than those for domestic consumption [22].
Adequate and correct information is critical for successfully implementing preventive behaviors [23,24,25]. Interestingly, in the current study, there was a discordance between mothers’ knowledge regarding molds and the mother’s practices regarding the same. Ideally, the mothers’ practice scores were expected to be equal to or lower than their knowledge levels. However, in this study, despite the mothers’ lack of knowledge about the dangers and control of molds, they performed the most critical preventive steps. This suggests that their actions were motivated by maximizing yields rather than specifically mitigating mold-related issues.
This is because the same practices that optimize productivity, such as early planting and effective pest disease control, inadvertently reduce mold proliferation and mycotoxin contamination [7]. Similarly, an earlier study reported that some farmers sorted and discarded moldy fractions of their produce to improve taste and not necessarily facilitate food safety [26].
The finding that household size positively influenced practice score on control of mycotoxins is attributable to the availability of manual labor. Farming relies almost entirely on family-derived manual labor in the study area and most parts of SSA. In a short rainfall season, this often leads to labor bottlenecks at critical points in the cropping cycle. Families with large memberships will likely accomplish most of the tasks, e.g., land preparation, planting, weeding, etc., on time [27], thus minimizing the risk of mycotoxin contamination [7].
The lack of statistical difference in KAP scores between those who belonged to care groups (promoters, cluster leaders, and members) and those who did not is attributable to the aggregated nature of the comprehensive KAP test. This study evaluated respondents using a comprehensive test based on the WHO Five Keys to Safer Foods and general good pre-and post-harvest practices. Most of these elements are not featured in the intervention or need to be better elaborated in training modules used by the care groups in Malawi. Therefore, these KAP test results may not provide insights into the program delivery or performance. However, a focus on an inventory of some key sanitary facilities such as a toilet, a hand washing facility, a drop hole cover for a toilet, and a refuse pit, which are central to the training program, show higher prevalence (p < 0.05) among the care group members (Supplementary Table S2). Therefore, these findings highlight the need for a holistic integration of food safety aspects in food security and nutrition programs. Workers’ labor is in vain unless food safety is central to a nutrition program. This is because most highly nutritious foods are also prone to BVPs and mold contamination. Therefore, efforts to increase their consumption without accompanying action to improve safety may also increase FBDs, thus resulting in net adverse health effects [28].
A clear roadmap can be developed to remediate the issues identified in this study. Firstly, it is necessary to adapt the WHO’s five keys to include specific guidelines for addressing mold contamination in addition to bacterial and viral pathogens (BVPs) [6,28]. Developing a tailored manual that considers a country’s socioeconomic status and cultural norms is essential. For instance, alternative preservation methods such as drying can be recommended for food storage without adequate refrigeration facilities. Moreover, promoting tip taps in toilets and kitchen areas for handwashing can improve hygiene practices among mothers. Emphasizing personal hygiene and maternal care actions tailored to cultural norms and taboos can further enhance the adoption of hygienic behaviors.
This study demonstrates strengths in its focused exploration of mothers, a pivotal group responsible for household food preparation. This targeted approach enriches the relevance of findings for family-level food hygiene practices. Incorporating both quantitative and qualitative data provides a nuanced understanding of the behaviors of the mothers, offering valuable context to complement the quantitative results. However, it is essential to acknowledge that this study did not assess risk perception and health literacy, which could significantly contribute to understanding knowledge, attitudes, and practices related to food hygiene among rural Malawian mothers. Additionally, the sample size of 522 participants is limited and only represents individuals from two specific districts. While this highlights the need for further research with a more diverse sample, it also presents an opportunity to gather more comprehensive insights for a broader understanding, such as cultural settings.
5. Conclusions
The findings have demonstrated that the mothers generally held positive attitudes but had limited knowledge and inconsistent hygienic practices, rendering the entire population vulnerable. Socio-cultural norms influenced attitudes, particularly around the use of soap and water. Behaviorally, handwashing practices were common but lacked the use of soap, and a lack of functional handwashing facilities contributed to unhygienic practices.
Therefore, a comprehensive education program should be developed based on the WHO Five Keys to Safer Foods and general good pre- and post-harvest practices. The program designers should pay particular attention to knowledge aspects that received low correct responses in this study. These programs should address socio-cultural barriers, particularly soap use and the importance of sanitary facilities. Communication messages should emphasize that hand washing without soap is inadequate to remove BVPs and fails to reduce FBD risk. Further research is also recommended to understand factors such as risk perception and health literacy that may influence knowledge, attitude, and practices related to food safety.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/hygiene4030028/s1, Table S1: Distribution of responses to each knowledge, altitude and practice item from the questionnaire; Table S2: Comparison of sanitary facilities and conditions among various social groups.
Author Contributions
Conceptualization, V.B., M.K. (Martina Kress), E.L., M.M., A.S., B.D., I.J. and L.M.; methodology V.B., M.K. (Martina Kress), E.L., M.M., D.P., H.P., A.P.G., K.C., A.S., B.D., I.J. and L.M.; formal analysis, V.B., M.K. (Martina Kress), E.L., M.M., D.P., H.P., A.P.G., K.C., A.S., B.D., I.J., A.T.M., K.M., G.C.-P., P.L.C., S.K., C.K., S.S., M.K. (Mphatso Kamndaya) and L.M.; investigation, V.B., M.K. (Martina Kress), E.L., K.C., A.S., B.D., I.J. and L.M.; data curation, V.B., E.L., M.M., D.P., H.P., A.P.G., M.K. (Mphatso Kamndaya) and L.M.; writing—original draft preparation, V.B., M.K. (Martina Kress), E.L., M.M., D.P., H.P., A.P.G., K.C., A.S., B.D., I.J., A.T.M., K.M., G.C.-P., P.L.C., S.K., C.K., S.S., M.K. (Mphatso Kamndaya) and L.M.; writing—review and editing, V.B., M.K. (Martina Kress), E.L., M.M., D.P., H.P., A.P.G., K.C., A.S., B.D., I.J., A.T.M., K.M., G.C.-P., P.L.C., S.K., C.K., S.S., M.K. (Mphatso Kamndaya) and L.M.; visualization, V.B and L.M.; supervision, M.K. (Martina Kress) and L.M.; project administration, M.K. (Martina Kress); funding acquisition, M.K. (Martina Kress). All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Malawi Food and Nutrition Security Programme (FNSP) under the “ONE WORLD-No Hunger” Global Initiative, which is funded by the German Ministry for Economic Cooperation and Development and implemented by the Deutsche Gesellschaft für Internationale Zusammenarbeit (GIZ) GmbH between February 2015 and March 2025.
Institutional Review Board Statement
The Provisional LUANAR Institutional Review Board waived ethical review and approval for this study due to its nature.
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
Data can be accessed from the authors on request.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of this study, in the collection, analyses, or interpretation of data, in the writing of the manuscript, or in the decision to publish the results.
References
- Havelaar, A.H.; Kirk, M.D.; Torgerson, P.R.; Gibb, H.J.; Hald, T.; Lake, R.J.; World Health Organization Foodborne Disease Burden Epidemiology Reference Group. World Health Organization Global Estimates and Regional Comparisons of the Burden of Foodborne Disease in 2010. PLoS Med. 2015, 12, e1001923. [Google Scholar] [CrossRef] [PubMed]
- Pires, S.M.; Devleesschauwer, B. Estimates of global disease burden associated with foodborne pathogens. In Foodborne Infections and Intoxications; Academic Press: Cambridge, MA, USA, 2021; pp. 3–17. [Google Scholar]
- WHO. WHO Steps up Action to Improve Food Safety and Protect People from Disease. 7 June 2021. Available online: https://www.who.int/news/item/07-06-2021-who-steps-up-action-to-improve-food-safety-and-protect-people-from-disease (accessed on 22 January 2024).
- Oduoye, M.O.; Akilimali, A.; Karim, K.A.; Moradeyo, A.A.; Abdullahi, Z.Z.; Muzata, D.; Christopher, G.U.; Chipinga, J.; Simiyu, B.W.; Isiko, I. Diseases Transmitted to Humans through Foodborne Microbes in the Global South. In Food Safety and Quality in the Global South; Springer Nature: Singapore, 2024; pp. 561–597. [Google Scholar]
- Kirk, M.D.; Pires, S.M.; Black, R.E.; Caipo, M.; Crump, J.A.; Devleesschauwer, B.; Döpfer, D.; Fazil, A.; Fischer-Walker, C.L.; Angulo, F.J. World Health Organization estimates of the global and regional disease burden of 22 foodborne bacterial, protozoal, and viral diseases, 2010: A data synthesis. PLoS Med. 2015, 12, e1001921. [Google Scholar]
- Gruber-Dorninger, C.; Jenkins, T.; Schatzmayr, G. Global mycotoxin occurrence in feed: A ten-year survey. Toxins 2019, 11, 375. [Google Scholar] [CrossRef] [PubMed]
- Matumba, L.; Namaumbo, S.; Ngoma, T.; Meleke, N.; De Boevre, M.; Logrieco, A.F.; De Saeger, S. Five keys to prevention and control of mycotoxins in grains: A proposal. Glob. Food Secur. 2001, 30, 100562. [Google Scholar] [CrossRef]
- Matumba, L.; Van Poucke, C.; Njumbe Ediage, E.; De Saeger, S. Keeping mycotoxins away from the food: Does the existence of regulations have any impact in Africa? Crit. Rev. Food Sci. Nutr. 2017, 57, 1584–1592. [Google Scholar] [CrossRef]
- Redmond, E.C.; Griffith, C.J. The importance of hygiene in the domestic kitchen: Implications for preparation and storage of food and infant formula. Perspect. Public Health 2009, 129, 69–76. [Google Scholar] [CrossRef]
- Byrd-Bredbenner, C.; Berning, J.; Martin-Biggers, J.; Quick, V. Food safety in home kitchens: A synthesis of the literature. Int. J. Environ. Res. Public Health 2013, 10, 4060–4085. [Google Scholar] [CrossRef]
- World Health Organization. Five Keys to Safer Food Manual; WHO: Geneve, Switzerland, 2012. Available online: https://www.who.int/publications/i/item/five-keys-to-safer-food-manual (accessed on 8 November 2023).
- Davis, T.P.; Wetzel, C.; Avilan, E.H.; de Mendoza Lopes, C.; Chase, R.P.; Winch, P.J.; Perry, H.B. Reducing child global undernutrition at scale in Sofala Province, Mozambique, using Care Group Volunteers to communicate health messages to mothers. Glob. Health Sci. Pract. 2013, 1, 35–51. [Google Scholar] [CrossRef]
- Geresomo, N.C.; Mbuthia, E.K.; Matofari, J.W.; Mwangwela, A.M. Targeting caregivers with context specific behavior change training increased uptake of recommended hygiene practices during food preparation and complementary feeding in Dedza district of Central Malawi. Ecol. Food Nutr. 2018, 57, 301–313. [Google Scholar] [CrossRef]
- Coates, J.; Swindale, A.; Bilinsky, P. Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access: Indicator Guide, 3rd ed.; Academy for Educational Development: Washington, DC, USA, 2007. [Google Scholar]
- Demberere, T.; Chidziya, T.; Ncozana, T.; Manyeruke, N. Knowledge and practices regarding water, sanitation and hygiene (WASH) among mothers of under-fives in Mawabeni, Umzingwane District of Zimbabwe. Phys. Chem. Earth Part A/B/C 2016, 92, 119–124. [Google Scholar] [CrossRef]
- Todd, E.C.; Michaels, B.S.; Holah, J.; Smith, D.; Greig, J.D.; Bartleson, C.A. Outbreaks where food workers have been implicated in the spread of foodborne disease. Part 10. Alcohol-based antiseptics for hand disinfection and a comparison of their effectiveness with soaps. J. Food Prot. 2010, 73, 2128–2140. [Google Scholar] [CrossRef] [PubMed]
- Burton, M.; Cobb, E.; Donachie, P.; Judah, G.; Curtis, V.; Schmidt, W.P. The effect of handwashing with water or soap on bacterial contamination of hands. Int. J. Environ. Res. Public Health 2011, 8, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Luby, S.P.; Agboatwalla, M.; Feikin, D.R.; Painter, J.; Billhimer, W.; Altaf, A.; Hoekstra, R.M. Effect of handwashing on child health: A randomised controlled trial. Lancet 2005, 366, 225–233. [Google Scholar] [CrossRef] [PubMed]
- Luby, S.P.; Halder, A.K.; Huda, T.; Unicomb, L.; Johnston, R.B. The effect of handwashing at recommended times with water alone and with soap on child diarrhea in rural Bangladesh: An observational study. PLoS Med. 2011, 8, e1001052. [Google Scholar] [CrossRef]
- Lokossou, Y.U.A.; Tambe, A.B.; Azandjèmè, C.; Mbhenyane, X. Socio-cultural beliefs influence feeding practices of mothers and their children in Grand Popo, Benin. J. Health Popul. Nutr. 2021, 40, 33. [Google Scholar] [CrossRef]
- Napier, A.D.; Ancarno, C.; Butler, B.; Calabrese, J.; Chater, A.; Chatterjee, H.; Guesnet, F.; Horne, R.; Jacyna, S.; Jadhav, S.; et al. Culture and health. Lancet 2014, 384, 1607–1639. [Google Scholar] [CrossRef]
- Magamba, K.; Matumba, L.; Matita, G.; Gama, A.P.; Singano, L.; Monjerezi, M.; Njoroge, S.M. Aflatoxin risk management in commercial groundnut products in Malawi (Sub-Saharan Africa): A call for a more socially responsible industry. J. Consum. Prot. Food Saf. 2017, 12, 309–316. [Google Scholar] [CrossRef]
- Liao, Q.; Cowling, B.J.; Lam, W.W.T.; Fielding, R. The influence of social-cognitive factors on personal hygiene practices to protect against influenzas: Using modelling to compare avian A/H5N1 and 2009 pandemic A/H1N1 influenzas in Hong Kong. Int. J. Behav. Med. 2011, 18, 93–104. [Google Scholar] [CrossRef]
- Pereboom, M.T.; Manniën, J.; Spelten, E.R.; Schellevis, F.G.; Hutton, E.K. Observational study to assess pregnant women’s knowledge and behaviour to prevent toxoplasmosis, listeriosis and cytomegalovirus. BMC Pregnancy Childbirth 2013, 13, 98. [Google Scholar] [CrossRef]
- Bloomfield, S.; Ackerley, L. Developing better understanding of hygiene is key to developing hygiene behaviour change in home and everyday life settings. Perspect. Public Health 2023, 22, 17579139231163734. [Google Scholar] [CrossRef]
- Matumba, L.; Monjerezi, M.; Kankwamba, H.; Njoroge, S.M.C.; Ndilowe, P.; Kabuli, H.; Kambewa, D.; Njapau, H. Knowledge, attitude, and practices concerning presence of molds in foods among members of the general public in Malawi. Mycotoxin Res. 2016, 32, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Martey, E.; Al-Hassan, R.M.; Kuwornu, J.K. Commercialization of smallholder agriculture in Ghana: A Tobit regression analysis. Afr. J. Agric. Res. 2012, 7, 2131–2141. [Google Scholar]
- Grace, D. Food safety in low- and middle-income countries. Int. J. Environ. Res. Public Health 2015, 12, 10490–10507. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).