Anatomical Distribution of Ultraviolet Radiation Depends on Phototherapy Unit Design and on Personal Height and Body Mass
Abstract
1. Introduction
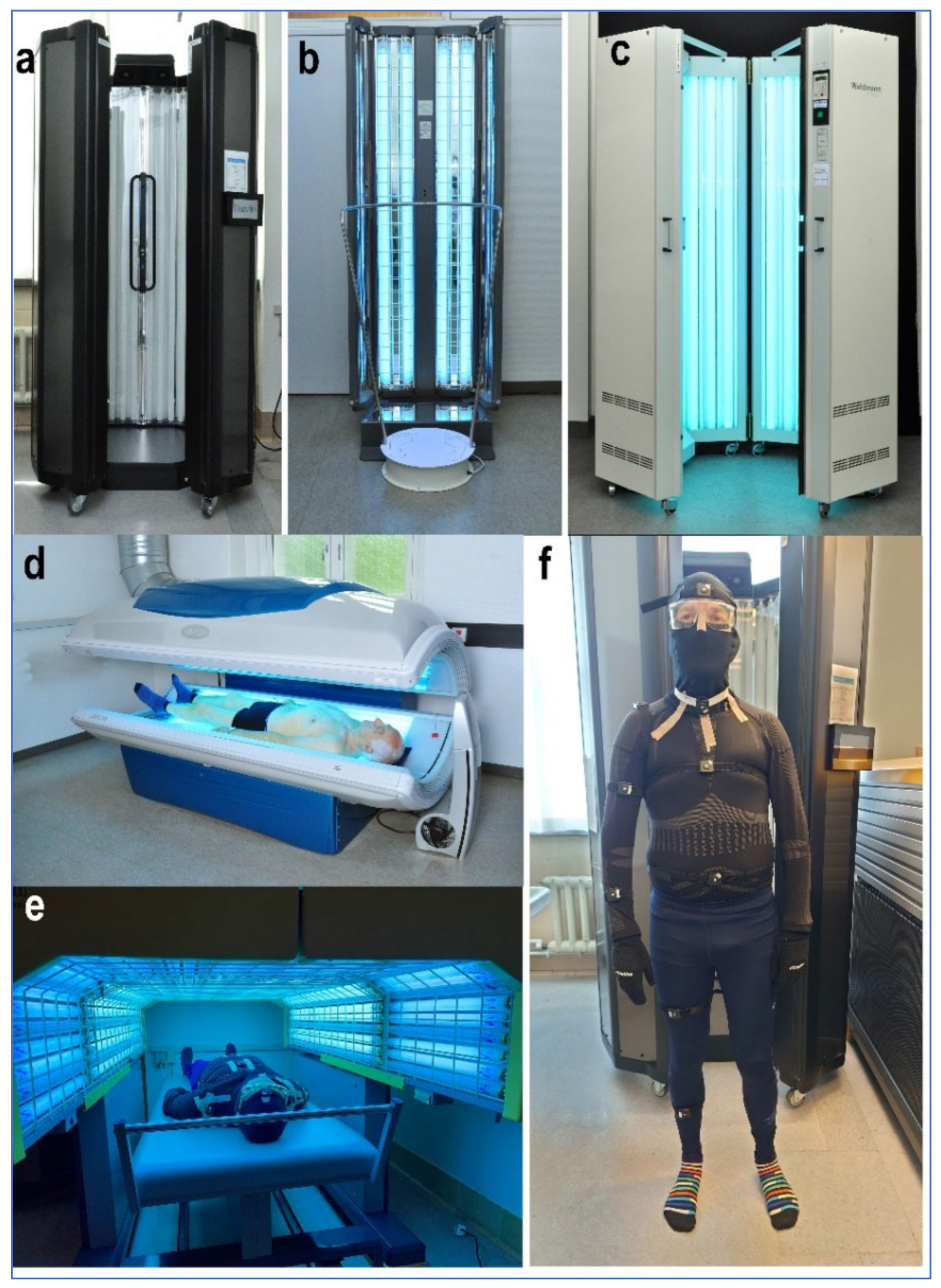
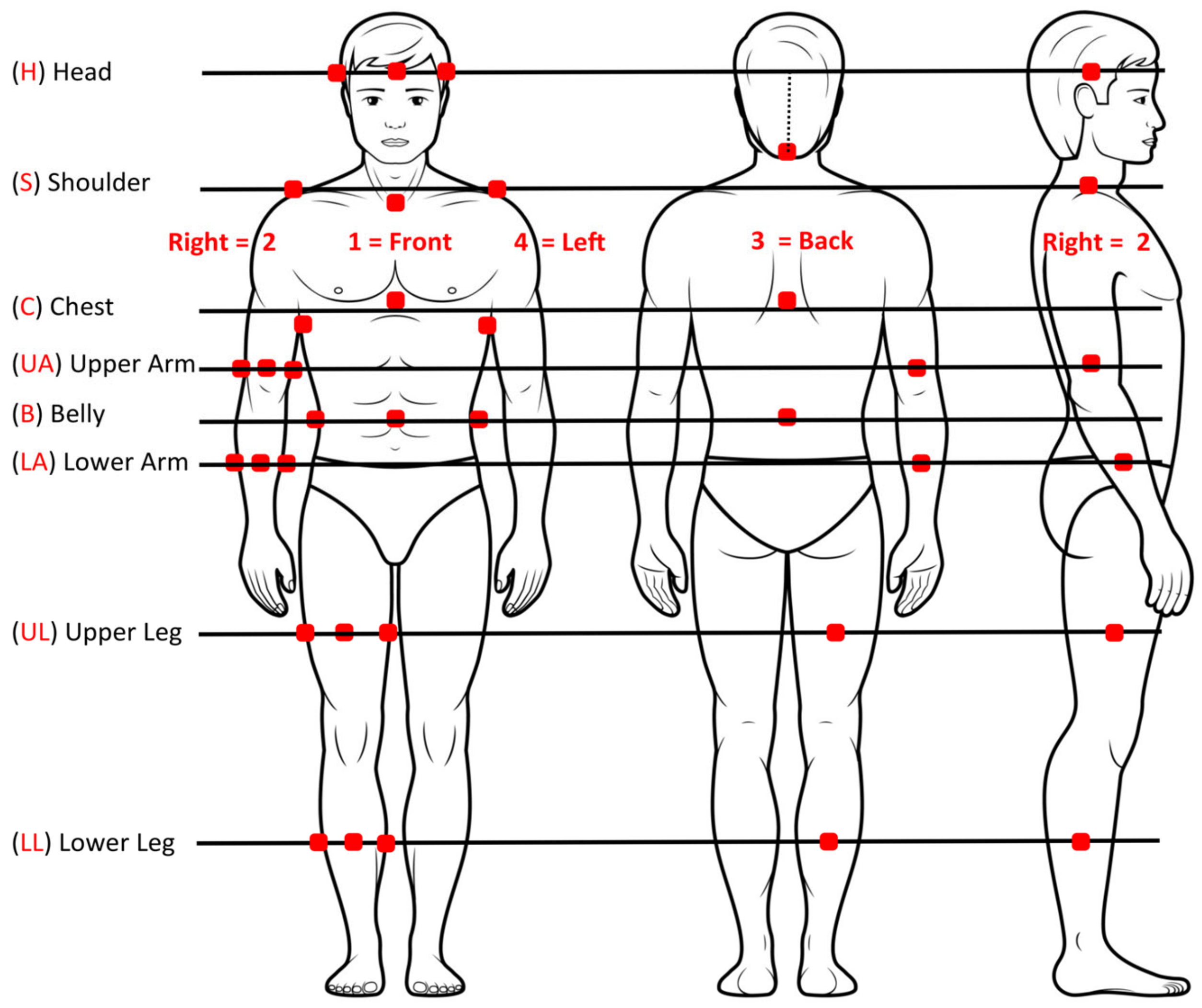
2. Materials and Methods
2.1. Unit A
2.2. Unit B
2.3. Unit C
2.4. Unit D
2.5. Unit E
2.6. Statistics
3. Results
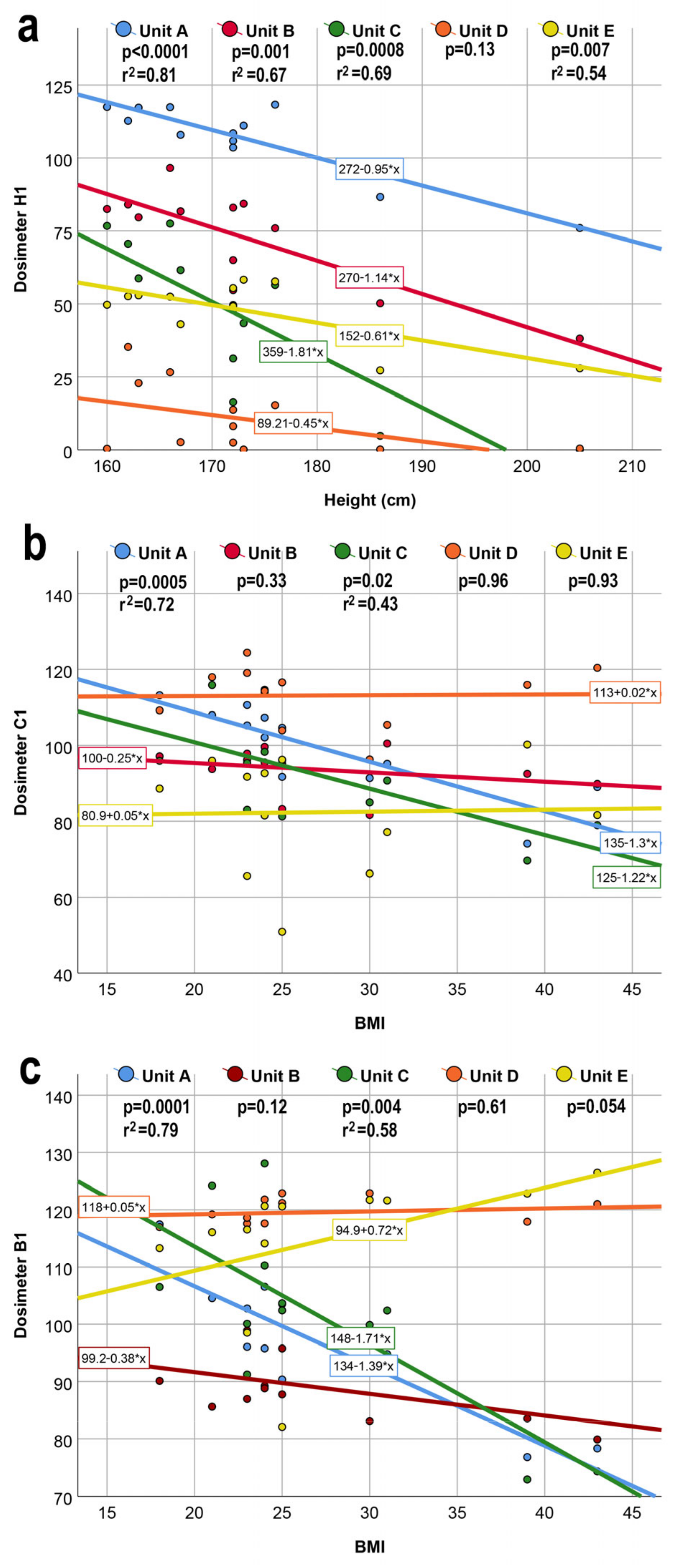
3.1. Importance of Body Shape
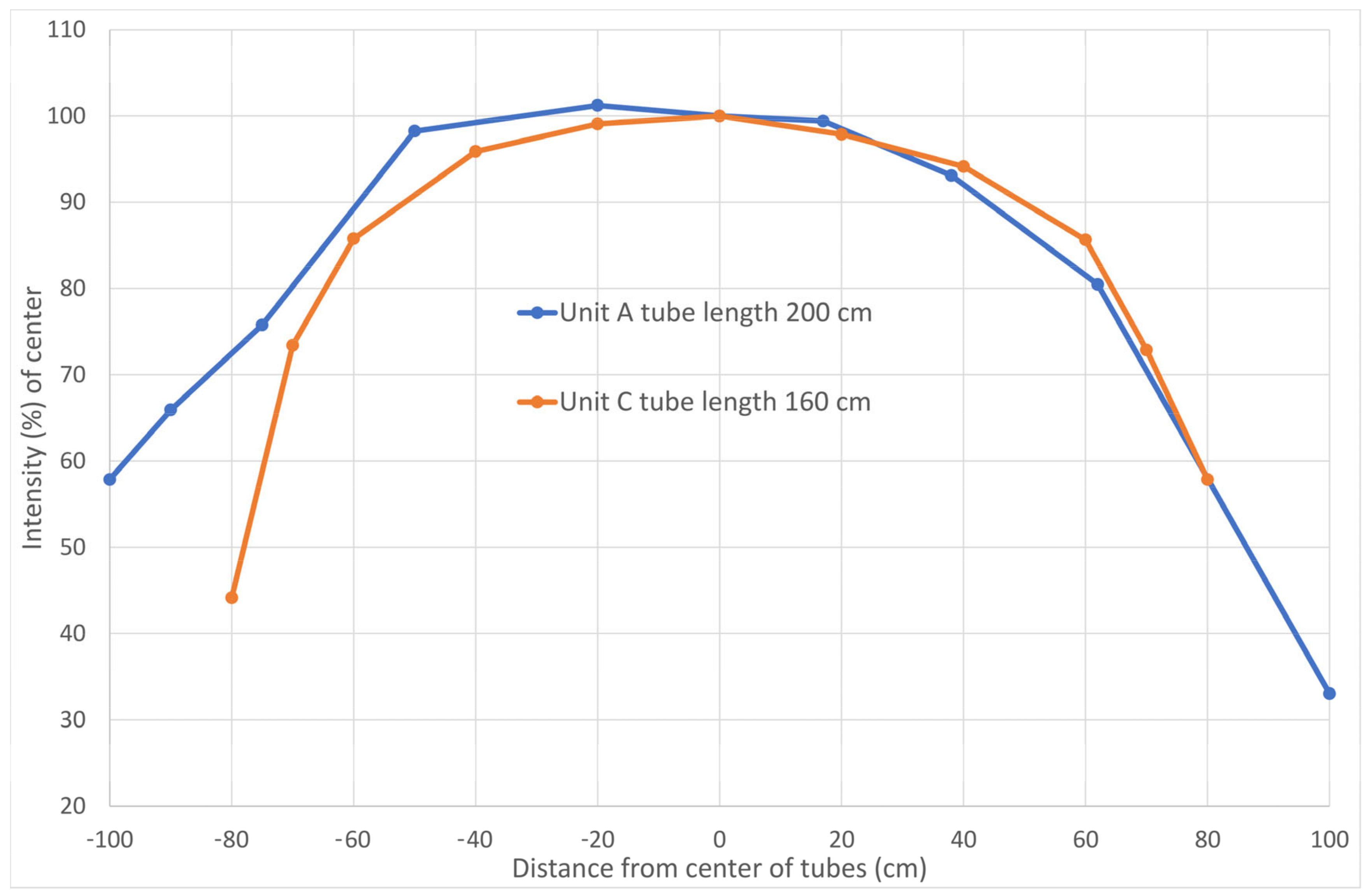
3.2. Importance of Phototherapy Unit Design
3.3. Received UV Irradiance of Calibration
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Parrish, J.A.; Fitzpatrick, T.B.; Tanenbaum, L.; Pathak, M.A. Photochemotherapy of psoriasis with oral methoxsalen and longwave ultraviolet light. N. Engl. J. Med. 1974, 291, 1207–1211. [Google Scholar] [CrossRef]
- Myers, E.; Kheradmand, S.; Miller, R. An update on narrowband ultraviolet B therapy for the treatment of skin diseases. Cureus 2021, 13, E19182. [Google Scholar] [CrossRef]
- Musters, A.H.; Mashayekhi, S.; Harvey, J.; Axon, E.; Lax, S.J.; Flohr, C.; Drucker, A.M.; Gerbens, L.; Ferguson, J.; Ibbotson, S.; et al. Phototherapy for atopic eczema. Cochrane Database Syst. Rev. 2021, 10, CD013870. [Google Scholar] [CrossRef] [PubMed]
- Ibbotson, S.H.; Bilsland, D.; Cox, N.H.; Dawe, R.S.; Diffey, B.; Edwards, C.; Farr, P.M.; Ferguson, J.; Hart, G.; Hawk, J.; et al. An update and guidance on narrowband ultraviolet B phototherapy: A British Photodermatology Group Workshop report. Br. J. Dermatol. 2004, 151, 283–297. [Google Scholar] [CrossRef] [PubMed]
- Diffey, B.L.; Harrington, T.R.; Challoner, A.V.J. A comparison of the anatomical uniformity of irradiation in two different photochemotherapy units. Br. J. Dermatol. 1978, 99, 361–363. [Google Scholar] [CrossRef] [PubMed]
- Diffey, B.L.; Harrington, T.R.; Davis, A. The anatomical distribution of ultraviolet radiation in photochemotherapy. Phys. Med. Biol. 1977, 22, 1014–1016. [Google Scholar] [CrossRef] [PubMed]
- Wulf, H.C.; Lock-Andersen, J.; The Scandinavian Photodermatology Research Group. Standard erythema dose. Skin. Res. Technol. 1996, 4, 192. [Google Scholar]
- Heydenreich, J.; Wulf, H.C. Miniature personal electronic UVR dosimeter with erythema response and time-stamped readings in a wristwatch. Photochem. Photobiol. 2005, 81, 1138–1144. [Google Scholar] [CrossRef] [PubMed]
- Heydenreich, J.; Wulf, H.C. Personal electronic UVR dosimeter measurements: Specific and general uncertainties. Photochem. Photobiol. Sci. 2019, 18, 1461–1470. [Google Scholar] [CrossRef] [PubMed]
- Moseley, H. Scottish UV dosimetry guidelines, “ScUViDo”. Photodermatol. Photoimmunol. Photomed. 2001, 17, 230–233. [Google Scholar] [CrossRef] [PubMed]
- Departmental order regarding control measurement of sunbeds in solaria and regarding digital registration (in Danish): Erhvervsministeriets Bekendtgørelse om kontrolmåling af solarier i solcentre og om digital registrering. BEK nr. 657 af 12/05/2015. Erhvervs-og Vækstministeriet, Sikkerhedsstyrelsen, Jounalnummer 170-01-00008. Available online: https://www.retsinformation.dk/eli/lta/2015/657 (accessed on 11 November 2022).
- Taylor, D.K.; Anstey, A.V.; Coleman, A.J.; Diffey, B.L.; Farr, P.M.; Ferguson, J.; Ibbotson, S.; Langmack, K.; Lloyd, J.J.; McCann, P.; et al. Guidelines for dosimetry and calibration in ultraviolet radiation therapy: A report of a British Photodermatology Group workshop. Br. J. Dermatol. 2002, 146, 755–763. [Google Scholar] [CrossRef] [PubMed]
- Cameron, H.; Yule, S.; Moseley, H.; Dawe, R.S.; Ferguson, J. Taking treatment to the patient: Development of a home TL-01 ultraviolet B phototherapy service. Br. J. Dermatol. 2002, 147, 957–965. [Google Scholar] [CrossRef] [PubMed]
- Jacob, J.; Pona, A.; Cline, A.; Feldman, S. Home UV Phototherapy. Dermatol. Clin. 2020, 38, 109–126. [Google Scholar] [CrossRef] [PubMed]
- Currie, G.D.; Evans, A.L.; Smith, D.; Martin, C.J.; McCalman, S.; Bilsland, D. An automated dosimetry system for testing whole-body ultraviolet phototherapy cabinets. Phys. Med. Biol. 2001, 46, 333–346. [Google Scholar] [CrossRef] [PubMed]
- Langmack, K.A. An insight into the contributions of self-shielding and lamp reflectors to patient exposure in phototherapy units. Phys. Med. Biol. 1998, 43, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Clarkson, D.M.; Franks, L. The use of a simulated body shape for determination of patient dosimetry within whole body ultraviolet treatment cabinets. Phys. Med. Biol. 2006, 51, N51–N58. [Google Scholar] [CrossRef] [PubMed]
- Fulljames, C.A.; Welsh, A.D. Measurement of patient dose in ultraviolet therapy using a phantom. Br. J. Dermatol. 2000, 142, 748–751. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.A.; Laube, S.; Edwards, C.; Gambles, B.; Anstey, A.V. Rate of acute adverse events for narrow-band UVB and Psoralen-UVA phototherapy. Photodermatol. Photoimmunol. Photomed. 2007, 23, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Wulf, H.C.; Heydenreich, J.; Philipsen, P.A. Variables in full-body ultraviolet B treatment of skin diseases. Photodermatol. Photoimmunol. Photomed. 2010, 26, 165–169. [Google Scholar] [CrossRef] [PubMed]
| Participant | Sex | Height cm | Weight kg | BMI |
|---|---|---|---|---|
| 1 | F | 160 | 63 | 25 |
| 2 | F | 162 | 60 | 23 |
| 3 | F | 163 | 48 | 18 |
| 4 | F | 166 | 65 | 24 |
| 5 | F | 167 | 87 | 31 |
| 6 | F | 172 | 61 | 21 |
| 7 | M | 172 | 90 | 30 |
| 8 | F | 172 | 127 | 43 |
| 9 | F | 173 | 117 | 39 |
| 10 | F | 176 | 75 | 24 |
| 11 | M | 186 | 85 | 25 |
| 12 | M | 205 | 96 | 23 |
| Mean | 9 F/3 M | 173 | 81.2 | 27.2 |
| Range | 160–205 | 48–127 | 18–43 |
| Unit | Unit | Unit | Unit | Unit | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | ||||||||||||
| Dosimeter Location | Mean | RSD | Mean RSD | Mean | RSD | Mean RSD | Mean | RSD | Mean RSD | Mean | RSD | Mean RSD | Mean | RSD | Mean RSD | |
| Head/Shoulder | H1 | 107 | 12 | 73 | 23 | 46 | 57 | 11 | 108 | 47 | 17 | |||||
| H2 | 107 | 13 | 63 | 25 | 53 | 47 | 9 | 84 | 43 | 8 | ||||||
| H3 | 95 | 14 | 52 | 29 | 62 | 32 | 29 | 99 | 53 | 45 | ||||||
| H4 | 113 | 11 | 12 | 68 | 20 | 24 | 59 | 42 | 44 | 8 | 112 | 101 | 46 | 14 | 21 | |
| S1 | 108 | 5 | 91 | 11 | 84 | 26 | 72 | 33 | 66 | 17 | ||||||
| S2 | 72 | 20 | 29 | 45 | 49 | 43 | 9 | 127 | 26 | 29 | ||||||
| S4 | 70 | 18 | 14 | 30 | 41 | 32 | 46 | 41 | 37 | 9 | 134 | 98 | 23 | 29 | 25 | |
| Trunk | C1 | 99 | 11 | 94 | 6 | 92 | 14 | 113 | 7 | 82 | 13 | |||||
| C2 | 13 | 163 | 59 | 18 | 22 | 101 | 7 | 116 | 60 | 22 | ||||||
| C3 | 100 | 7 | 100 | 5 | 100 | 8 | 100 | 13 | 100 | 7 | ||||||
| C4 | 7 | 218 | 100 | 58 | 25 | 14 | 7 | 199 | 80 | 12 | 130 | 66 | 47 | 27 | 17 | |
| B1 | 97 | 11 | 89 | 6 | 101 | 16 | 120 | 2 | 114 | 6 | ||||||
| B2 | 46 | 51 | 47 | 24 | 46 | 53 | 39 | 60 | 74 | 17 | ||||||
| B3 | 98 | 8 | 99 | 9 | 96 | 13 | 79 | 24 | 105 | 7 | ||||||
| B4 | 43 | 70 | 35 | 60 | 19 | 15 | 31 | 96 | 44 | 32 | 51 | 34 | 70 | 22 | 13 | |
| Arm | UA1 | 125 | 7 | 94 | 10 | 115 | 8 | 58 | 25 | 72 | 9 | |||||
| UA2 | 117 | 4 | 65 | 22 | 110 | 8 | 103 | 13 | 24 | 68 | ||||||
| UA3 | 89 | 25 | 65 | 11 | 96 | 23 | 78 | 35 | 73 | 27 | ||||||
| UA4 | 14 | 124 | 40 | 21 | 62 | 26 | 12 | 138 | 44 | 11 | 96 | 42 | 20 | 67 | 43 | |
| LA1 | 122 | 6 | 66 | 22 | 107 | 9 | 96 | 16 | 86 | 8 | ||||||
| LA2 | 119 | 3 | 94 | 8 | 109 | 15 | 101 | 14 | 20 | 65 | ||||||
| LA3 | 80 | 23 | 47 | 32 | 87 | 17 | 92 | 14 | 81 | 19 | ||||||
| LA4 | 18 | 50 | 21 | 26 | 25 | 22 | 13 | 118 | 40 | 22 | 76 | 30 | 56 | 33 | 31 | |
| Leg | UL1 | 125 | 5 | 88 | 10 | 114 | 4 | 131 | 3 | 107 | 5 | |||||
| UL2 | 112 | 6 | 80 | 6 | 116 | 9 | 102 | 9 | 56 | 31 | ||||||
| UL3 | 108 | 5 | 95 | 7 | 111 | 7 | 122 | 4 | 102 | 4 | ||||||
| UL4 | 25 | 47 | 16 | 12 | 92 | 29 | 15 | 114 | 34 | 57 | 48 | 16 | 57 | 37 | 19 | |
| LL1 | 106 | 11 | 69 | 16 | 105 | 7 | 126 | 5 | 93 | 9 | ||||||
| LL2 | 107 | 9 | 69 | 12 | 119 | 7 | 110 | 13 | 53 | 24 | ||||||
| LL3 | 104 | 10 | 80 | 15 | 112 | 7 | 123 | 3 | 94 | 10 | ||||||
| LL4 | 55 | 24 | 13 | 31 | 29 | 18 | 51 | 35 | 14 | 85 | 29 | 13 | 71 | 25 | 17 | |
| Mean total | 31.3 | 22.4 | 42.2 | 50.0 | 23.4 | |||||||||||
| Normalized | 1.40 | 1.00 | 1.88 | 2.23 | 1.04 | |||||||||||
| Mean | ||||||||||||||||
| (H+S values | 37.3 | 20.5 | 42.8 | 33.6 | 23.5 | |||||||||||
| excluded) | ||||||||||||||||
| Unit | Unit | Unit | Unit | Unit | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | |||||||
| Dosimeter Location | Mean | Mean Group | Mean | Mean Group | Mean | Mean Group | Mean | Mean Group | Mean | Mean Group | |
| Head/Shoulder | H1 | 81 | 68 | 35 | 8 | 43 | |||||
| H2 | 81 | 58 | 41 | 7 | 38 | ||||||
| H3 | 72 | 49 | 47 | 23 | 48 | ||||||
| H4 | 86 | 80 | 63 | 60 | 46 | 42 | 6 | 11 | 42 | 43 | |
| S1 | 82 | 85 | 65 | 57 | 60 | ||||||
| S2 | 55 | 27 | 38 | 7 | 23 | ||||||
| S4 | 53 | 63 | 28 | 47 | 35 | 46 | 7 | 24 | 21 | 35 | |
| Trunk | C1 | 75 | 87 | 71 | 89 | 74 | |||||
| C2 | 10 | 55 | 17 | 6 | 55 | ||||||
| C3 | 76 | 93 | 77 | 79 | 91 | ||||||
| C4 | 6 | 42 | 54 | 72 | 5 | 42 | 9 | 46 | 43 | 66 | |
| B1 | 73 | 83 | 78 | 94 | 104 | ||||||
| B2 | 35 | 44 | 36 | 31 | 67 | ||||||
| B3 | 74 | 92 | 74 | 62 | 95 | ||||||
| B4 | 32 | 54 | 56 | 69 | 24 | 53 | 25 | 53 | 64 | 82 | |
| Arm | UA1 | 95 | 88 | 89 | 46 | 66 | |||||
| UA2 | 88 | 60 | 85 | 81 | 22 | ||||||
| UA3 | 68 | 61 | 74 | 61 | 66 | ||||||
| UA4 | 11 | 65 | 20 | 57 | 9 | 64 | 9 | 49 | 18 | 43 | |
| LA1 | 93 | 62 | 83 | 75 | 78 | ||||||
| LA2 | 90 | 87 | 84 | 79 | 18 | ||||||
| LA3 | 61 | 44 | 67 | 73 | 73 | ||||||
| LA4 | 14 | 64 | 24 | 54 | 10 | 61 | 18 | 61 | 50 | 55 | |
| Leg | UL1 | 95 | 82 | 88 | 103 | 97 | |||||
| UL2 | 85 | 75 | 89 | 80 | 51 | ||||||
| UL3 | 82 | 88 | 86 | 96 | 92 | ||||||
| UL4 | 19 | 70 | 11 | 64 | 12 | 69 | 45 | 81 | 52 | 73 | |
| LL1 | 80 | 64 | 81 | 100 | 84 | ||||||
| LL2 | 81 | 64 | 92 | 87 | 48 | ||||||
| LL3 | 79 | 75 | 86 | 97 | 85 | ||||||
| LL4 | 42 | 71 | 29 | 58 | 39 | 74 | 66 | 87 | 64 | 70 | |
| Mean total | 64 | 61 | 57 | 52 | 59 | ||||||
| Mean | 61 | 63 | 61 | 63 | 65 | ||||||
| (H+S values excluded) | |||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wulf, H.C.; Philipsen, P.A.; Heydenreich, J. Anatomical Distribution of Ultraviolet Radiation Depends on Phototherapy Unit Design and on Personal Height and Body Mass. Int. J. Transl. Med. 2023, 3, 66-80. https://doi.org/10.3390/ijtm3010006
Wulf HC, Philipsen PA, Heydenreich J. Anatomical Distribution of Ultraviolet Radiation Depends on Phototherapy Unit Design and on Personal Height and Body Mass. International Journal of Translational Medicine. 2023; 3(1):66-80. https://doi.org/10.3390/ijtm3010006
Chicago/Turabian StyleWulf, Hans Christian, Peter A. Philipsen, and Jakob Heydenreich. 2023. "Anatomical Distribution of Ultraviolet Radiation Depends on Phototherapy Unit Design and on Personal Height and Body Mass" International Journal of Translational Medicine 3, no. 1: 66-80. https://doi.org/10.3390/ijtm3010006
APA StyleWulf, H. C., Philipsen, P. A., & Heydenreich, J. (2023). Anatomical Distribution of Ultraviolet Radiation Depends on Phototherapy Unit Design and on Personal Height and Body Mass. International Journal of Translational Medicine, 3(1), 66-80. https://doi.org/10.3390/ijtm3010006






