Association between Peer Victimization (PV) in Childhood/Adolescence and Personality Disorders among Adult Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Procedure
2.3. Instruments
2.4. Statistical Analysis
3. Results
3.1. Sociodemographic Characteristics of Patients
3.2. Axis I Disorders
3.3. Structured Clinical Interview of DSM IV (R) Axis II Personality Disorders Questionnaire (SCID II-Q)
3.4. Self-Esteem and Social Support
4. Discussion
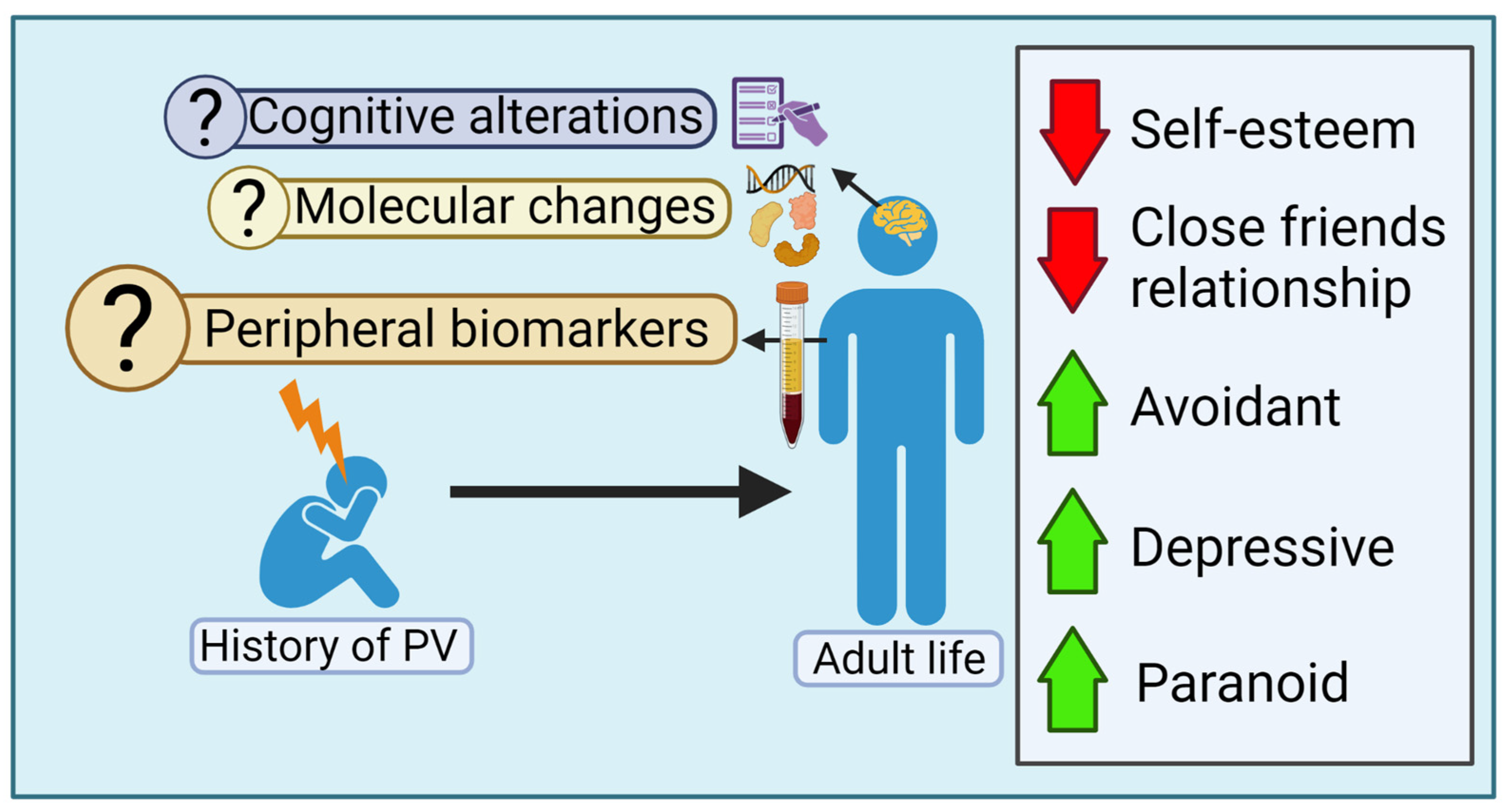
4.1. The Impact of PV in the Long-Term Personality Dysfunction
4.2. Peer Victimization: Toxic Stress, Allostatic Load and Epigenetics
4.3. Psychological Processes That Link PV and Dysfunctional Personality Traits
4.4. Limitations and Future Perspective
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Menesini, E.; Salmivalli, C. Bullying in schools: The state of knowledge and effective interventions. Psychol. Health Med. 2017, 22 (Suppl. S1), 240–253. [Google Scholar] [CrossRef] [PubMed]
- Hymel, S.; Swerer, S.M. Four decades of research on school bullying. Am. Psychol. 2015, 70, 293–299. [Google Scholar] [CrossRef]
- Olweus, D. Victimization by Peers: Antecedents and Long-Term Outcomes. In Social Withdrawal, Inhibition and Shyness in Childhood; Rubin, K.H., Aserdorf, J.B., Eds.; Earlbaum: Hilldale, NJ, USA, 1993; pp. 315–341. [Google Scholar]
- Nansel, T.R.; Craig, W.; Overpeck, M.D.; Saluja, G.; Ruan, J. Cross-national consistency in the relationships between bullying behaviors and psychosocial adjustment. Arch. Pedriatr. Adolesc. Med. 2004, 158, 730–736. [Google Scholar] [CrossRef]
- Currie, C.; Zanotti, C.; Morgan, A.; Currie, D.; de Looze, M.; Roberts, C.; Samdal, O.; Smith, O.R.; Barnekow, V. Social Determinants of Health and Well-Being among Young People. Health Behaviour in School-Aged Children (HCSC) Study: International Report from the 2009/2010 Survey; WHO Regional Office for Europe: Copenhagen, Denmark, 2012; (Health Policy for Children and Adolescents, No. 6); Available online: https://www.euro.who.int/__data/assets/pdf_file/0007/167281/E96444_part1.pdf (accessed on 18 December 2022).
- Luxemberg, H.; Limber, S.P.; Olweus, D. Bullying in U.S. Schools: 2019 Status Report; Hazelden Publishing: Center City, MN, USA, 2019; Available online: https://olweus.sites.clemson.edu/documents/Status%20Report_2019.pdf (accessed on 18 December 2022).
- Smith, P.K.; Brain, P. Bullying in schools: Lessons from two decades of research. Aggress. Behav. 2000, 26, 1–9. [Google Scholar] [CrossRef]
- Arsaneault, L.; Bowes, L.; Shakoor, S. Bullying victimization in youths and mental health problems: ‘Much ado about nothing’? Psychol. Med. 2010, 40, 717–729. [Google Scholar] [CrossRef] [PubMed]
- Hawker, D.S.L.; Boulton, M.J. Twenty years’ research on peer victimization and psychosocial maladjustment: A meta-analytic review of cross-sectional studies. J. Child Psychol. Psychiatry Allied Discip. 2000, 41, 441–455. Available online: https://pubmed.ncbi.nlm.nih.gov/10836674/ (accessed on 18 December 2022). [CrossRef]
- Arana, A.A.; Boyd, E.Q.; Guarneri-White, M. The impact of social and physical peer victimization on systemic inflammation in adolescence. Merril Palmer Q. 2018, 64, 12–40. Available online: https://www.muse.jhu.edu/article/705184 (accessed on 18 December 2022). [CrossRef]
- Sourander, A.; Jensen, P.; Ronning, J.A.; Niemela, S.; Helenius, H.; Sillamäki, L.; Kumpulainen, K.; Piha, J.; Tamminen, T.; Moilanen, I.; et al. What is the early adulthood outcome of boys who bully or are bullied in childhood? The finnish “from a boy to a man” study. Pediatrics 2007, 120, 397–404. [Google Scholar] [CrossRef]
- Takizawa, R.; Maughan, B.; Arsenault, L. Adult health outcomes of childhood bullying victimization: Evidence from a five-decade longitudinal british birth cohort. Am. J. Psychiatry 2014, 171, 777–784. [Google Scholar] [CrossRef]
- Klomek, A.B.; Sourander, A.; Elonheimo, H. Bullying by peers in childhood and effects on psychopathology, suicidality and criminality in adulthood. Lancet Psychiatry 2015, 2, 930–941. [Google Scholar] [CrossRef]
- McDougall, P.; Vaillancourt, T. Long-term adult outcomes of peer victimization in childhood and adolescence. Am. Psychol. 2015, 70, 300–310. [Google Scholar] [CrossRef] [PubMed]
- Moore, S.E.; Norman, R.E.; Suetani, S.; Thomas, H.J.; Sly, P.D.; Scott, J.G. Consequences of bullying victimization in childhood and adolescence: A systematic review and meta-analysis. World J. Psychiatry 2017, 7, 60–76. [Google Scholar] [CrossRef] [PubMed]
- Copeland, W.; Wolke, D.; Angold, A.; Costello, J. Adult psychiatric outcomes of bullying and being bullied by peers in childhood and adolescence. JAMA Psychiatry 2013, 70, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Lereya, S.T.; Copeland, W.E.; Costello, E.J.; Wolke, D. Adult mental health consequences of peer bullying and maltreatment in childhood: Two cohorts in two countries. Lancet Psychiatry 2015, 2, 524–531. [Google Scholar] [CrossRef] [PubMed]
- Cicchetti, D.; Rogosch, F.A. Equifinality and multifinality in developmental psychopathology. Dev. Psychopathol. 1996, 8, 597–600. [Google Scholar] [CrossRef]
- Vaillancourt, T.; Sanderson, C.; Arnold, P.; McDougall, P. The Neurobiology of Peer Victimization: Longitudinal Links to Health, Genetic Risk, and Epigenetic Mechanisms. In Handbook of Bullying Prevention: A Life Course Perspective; Bradshaw, C., Ed.; NASW Press: Cary, NC, USA, 2017; pp. 35–47. [Google Scholar]
- Caspi, A.; McClay, J.; Moffitt, T.E.; Mill, J.; Martin, J.; Craig, I.W.; Taylor, A.; Poulton, R. Role of genotype in the cycle of violence in maltreated children. Science 2002, 297, 851–854. [Google Scholar] [CrossRef]
- Hodges, E.V.E.; Boivin, M.; Vitaro, F.; Bukowski, W.M. The power of friendship: Protection against an escalating cycle of peer victimization. Dev. Psychol. 1999, 35, 94–101. [Google Scholar] [CrossRef]
- Fitzpatrick, S.; Bussey, K. The role of perceived friendship self-efficacy as a protective factor against the negative effects of social victimization. Soc. Dev. 2014, 23, 41–60. [Google Scholar] [CrossRef]
- Clauss, J.A.; Blackford, J.U. Behavioral inhibition and risk for development social anxiety disorder: A meta-analytic study. J. Am. Acad. Child Adolesc. Psychiatry 2012, 51, 1066–1075. [Google Scholar] [CrossRef]
- Caouette, J.D.; Guyer, A.E. Gaining insight into adolescent vulnerability for social anxiety from developmental cognitive neuroscience. Dev. Cogn. Neurosci. 2014, 8, 65–76. [Google Scholar] [CrossRef]
- Wolke, D.; Lereya, S.T. Long term effects of bullying. Arch. Dis. Child. 2015, 100, 879–885. [Google Scholar] [CrossRef] [PubMed]
- Kasen, S.; Johnson, J.G.; Chen, H.; Crawford, T.N. School Climate and Change in Personality Disorder Symptom Trajectories Related to Bullying: A Prospective Study. In Bullying in North American Schools; Espalage, D.L., Swearer, S.M., Eds.; Routledge: New York, NY, USA, 2010. [Google Scholar]
- Sansone, R.A.; Lam, C.; Wiederman, M.W. Being bullied in childhood: Correlations with borderline personality in adulthood. Compr. Psychiatry 2010, 51, 458–461. [Google Scholar] [CrossRef] [PubMed]
- Erazo, M.B.; Krygsman, A.L.; Vallancourt, T. The cumulative effects of bullying victimization in childhood and adolescence on borderline personality disorder symptoms in emerging adulthood. Int. J. Bullying Prev. 2022. [Google Scholar] [CrossRef]
- Antila, H.; Arola, R.; Hakko, H.; Riala, K.; Riipinen, P.; Kantjärvi, L. Bullying involvement in relation to personality disorders: A prospective follow-up of 508 inpatient adolescents. Eur. Child Adolesc. Psychiatry 2017, 26, 779–789. [Google Scholar] [CrossRef]
- Millon, T. Trastornos de la Personalidad: Más Allá del DSM IV; Masson: Barcelona, Spain, 1998. [Google Scholar]
- Young, J. Cognitive Therapy for Personality Disorders: A Schema-Focused Approach; Professional Resource Press: Sarasota, FL, USA, 1994. [Google Scholar]
- Sweerer, S.M.; Hymel, S. Understanding the psychology of bullying: Moving toward a social-ecological diathesis stress model. Am. Psychol. 2015, 70, 344–353. [Google Scholar] [CrossRef]
- Guroglu, B.; Veenstra, R. Neural underpinnings of peer experiences and interactions: A review of social neuroscience research. Merril Palmer Q. 2021, 67, 416–456. [Google Scholar] [CrossRef]
- Chen, Z.; Williams, K.D.; Fitness, J.; Newton, N.C. When hurt will not heal. Exploring the capacity to relive social and physical pain. Psychol. Sci. 2008, 19, 789–795. [Google Scholar] [CrossRef]
- Lupien, S.J.; Juster, R.P.; Raymond, C.; Marín, M.F. The effects of chronic stress on the human brain: From neurotoxicity, to vulnerability, to opportunity. Front. Neuroendocrinol. 2018, 49, 91–105. [Google Scholar] [CrossRef]
- First, M.B.; Gibbon, M.; Spitzer, R.L.; Williams, J.B.; Benjamin, L.S. Entrevista Clínica Estructurada Para Los Trastornos de la Personalidad del eje II del DSM-IV (SCID-II); Masson: Barcelona, Spain, 1999. [Google Scholar]
- First, M.B.; Gibbon, M.; Spitzer, R.L.; Williams, J.B.; Benjamin, L.S. SCID-II Personality Questionnaire; American Psychiatric Press: Washington, DC, USA, 1997. [Google Scholar]
- Campo-Arias, A.; Díaz-Martínez, L.A.; Barros-Bermúdez, J.A. Consistencia interna del cuestionario autoadministado de la Entrevista Clínica Estructurada para Trastornos del Eje II del DSM IV. Rev. Colomb. Psiquiat. 2008, 37, 378–384. Available online: http://www.redalyc.org/articulo.oa?id=80611205008 (accessed on 11 December 2022).
- Baumeister, R.; Leary, M.R. The need to belong: Desire for interpersonal attachments as a fundamental human motivation. Psychol. Bull. 1995, 117, 497–529. Available online: https://pubmed.ncbi.nlm.nih.gov/7777651/ (accessed on 18 December 2022). [CrossRef]
- Graham, S.; Junoven, J. Self-blame and peer victimization in middle school: An attibutional analysis. Dev. Psychol. 1998, 34, 587–599. [Google Scholar] [CrossRef] [PubMed]
- Negi, R. Cognitive processes of victims of bullying. Int. J. Bullying Prev. 2021, 3, 1–13. [Google Scholar] [CrossRef]
- Calderero, M.; Salazar, I.C.; Caballo, V.E. Una revisión de las relaciones entre el acoso escolar y la ansiedad social. Behav. Psychol. 2011, 19, 393–419. Available online: https://www.behavioralpsycho.com/wp-content/uploads/2019/08/08.Calderero_19-2oa.pdf (accessed on 18 December 2022).
- Keil, V.; Price, J.M. Social information-processing patterns of maltreated children in two social domains. J. Appl. Dev. Psychol. 2009, 30, 43–52. [Google Scholar] [CrossRef]
- Ziv, Y.; Leibovich, I.; Shechtman, Z. Bullying victimization in early adolescence: Relations to social information processing patterns. Aggress. Behav. 2013, 39, 482–492. [Google Scholar] [CrossRef] [PubMed]
- Butler, J.C.; Doherty, M.S.; Potter, R.M. Social antecedents and consequences of interpersonal rejection sensitivity. Personal. Individ. Differ. 2007, 43, 1376–1385. [Google Scholar] [CrossRef]
- Schäfer, M.; Korno, S.; Smith, P.K.; Hunter, S.C.; Mora-Merchán, A.; Singer, M.; van der Meulen, K. Lonely in the crowd: Recollections of bullying. Br. J. Dev. Psychol. 2004, 22, 379–394. [Google Scholar] [CrossRef]
- Levy, S.R.; Ayduk, O.; Downey, G. The Role of Rejection Sensitivity in People’s Relationships with Significant Others and Valued Social Groups. In Interpersonal Rejection; Leary, M., Ed.; Oxford University Press: Oxford, UK, 2001; pp. 251–289. [Google Scholar]
- Slavisch, G.M.; O’Donovan, A.; Epel, E.; Kennedy, M. Black sheep get the blues: A psychobiological model of social rejection and depression. Neurosci. Biobehav. Rev. 2010, 35, 39–45. [Google Scholar] [CrossRef]
- Muñoz-Prieto, M.M. Incidencia del Acoso Escolar en Alumnos de 4° y 6° de Educación Primaria en Colegios de la Ciudad de Vigo. Ph.D. Thesis, Universidad de Salamanca, Salamanca, Spain, 2009. [Google Scholar]
- Troop-Gordon, W.; Rudolph, K.D.; Sugimura, N.; Little, T.D. Peer victimization in middle childhood impedes adaptive responses to stress: A pathway to depressive symptoms. J. Clin. Child Adolesc. Psychol. 2014, 44, 432–445. [Google Scholar] [CrossRef]
- Contreras, A.; Valiente, C.; Vázquez, C.; Trucharte, A.; Peinado, V.; Varese, F.; Bentall, R. The network structure of paranoia dimensions and its mental health correlates in the general population: The core role of loneliness. Schizophr. Res. 2022, 246, 65–73. [Google Scholar] [CrossRef]
- Xu, Y.M.; Pu, S.S.; Li, Y.; Zhong, B.L. Possible Avoidant Personality Disorder Magnifies the Association Between Bullying Victimization and Depressive Symptoms Among Chinese University Freshmen. Front. Psychiatry 2022, 13, 822185. [Google Scholar] [CrossRef]
- Idsoe, T.; Vallancourt, T.; Dyregrov, A.; Hagen, K.A.; Ogden, T.; Naerde, A. Bullying victimization and trauma. Front. Psychiatry 2021, 11, 480353. [Google Scholar] [CrossRef] [PubMed]
- Slavich, G.M. Social Safety Theory: A biologically based evolutionary perspective on life stress, health and behavior. Annu. Rev. Clin. Psychol. 2020, 16, 265–295. [Google Scholar] [CrossRef] [PubMed]
- Zárate-Garza, P.P.; Biggs, B.K.; Croarkin, P.; Morath, B.; Leffler, J.; Cuéllar-Barboza, A.; Tye, S. How well do we understand the long-term health implications of childhood bullying? Harv. Rev. Psychiatry 2017, 25, 89–95. [Google Scholar] [CrossRef]
- Eisenberger, N.I.; Lieberman, M.D.; Williams, K.D. Does rejection hurt? An fMRI study of social exclusion. Science 2003, 302, 290–292. [Google Scholar] [CrossRef] [PubMed]
- Rudolph, K.D.; Miernicki, M.E.; Troop-Gordon, W.; Davis, M.; Telzer, E.H. Adding insult to injury: Neural sensitivity to social exclusion is associated with internalizing symptoms in chronically peer victimized girls. Soc. Cogn. Neurosci. 2016, 11, 829–842. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Teicher, M.H. Scars that won’t heal: The neurobiology of child abuse. Sci. Am. 2002, 286, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Shonkoff, J.P.; Boyce, T.; McEwen, B.S. Neuroscience, molecular biology and the childhood roots of health disparities: Building a new framework for health promotion and disease prevention. JAMA 2009, 301, 2252–2259. [Google Scholar] [CrossRef]
- Teicher, M.H.; Samson, J.A.; Anderson, C.M.; Ohashi, K. The effects of childhood maltreatment on brain structure, function and connectivity. Nat. Rev. Neurosci. 2016, 17, 152–666. [Google Scholar] [CrossRef]
- Copeland, W.E.; Wolke, D.; Lereya, S.T.; Shanahan, L.; Worthman, C.; Costello, E.J. Childhood bullying involvement predicts low grade systemic inflammation into adulthood. Proc. Natl. Acad. Sci. USA 2014, 111, 7570–7575. [Google Scholar] [CrossRef] [PubMed]
- Ke, T.; De Simoni, S.; Barker, E.; Smith, P. The association between peer-victimization and structural and functional brain outcomes: A systematic review. JCCP Adv. 2022, 2, e12081. [Google Scholar] [CrossRef]
- Swartz, J.R.; Carranza, A.F.; Knodt, A.R. Amygdala activity to angry and fearful faces relates to bullying and victimization in adolescents. Soc. Cogn. Affect. Neurosci. 2019, 14, 1027–1035. [Google Scholar] [CrossRef] [PubMed]
- McIver, T.; Bosma, R.L.; Sandre, A.; Goegan, S.; Klassen, J.; Chiarella, J.; Booij, K.; Craig, W. Peer victimization is associated with neural response to social exclusion. Merril Palmer Q. 2018, 64, 135–161. [Google Scholar] [CrossRef]
- González-Pardo, H.; Pérez-Álvarez, M. Epigenetics and its implications for Psychology. Psicothema 2013, 25, 3–12. [Google Scholar] [PubMed]
- Delgado-Morales, R.; Agis-Balboa, R.C. Epigenetic mechanisms during ageing and neurogenesis as novel therapeutic avenues in human brain disorders. Clin. Epigenet. 2017, 9, 67. [Google Scholar] [CrossRef] [PubMed]
- Spuch, C.; Agis-Balboa, R.C. Epigenética en neurociencias. Span. Soc. Biochem. Mol. Biol. SEBB Mag. 2014, 174, 18–21. [Google Scholar]
- Weaber, C.G.; Cervoni, C.; Champagne, F.A.; D’Alessio, A.C.; Sharma, S.; Seckl, J.R.; Dymov, S.; Szyf, M.; Meaney, M.J. Epigenetic programming by maternal behavior. Nat. Neurosci. 2004, 7, 847–854. [Google Scholar] [CrossRef]
- Mulder, R.; Walton, E.; Neumann, A.; Houtepen, L.C.; Felix, J.; Bakermans-Kranenburg, M.J.; Suderman, M.; Tiemeier, H.; van Ijzendoornm, M.; Relton, C.; et al. Epigenomics of being bullied: Changes in DNA following bullying exposure. Epigenetics 2020, 15, 750–764. [Google Scholar] [CrossRef]
- Ouellet-Morin, I.; Wong, C.C.Y.; Danese, A.; Pariante, C.M.; Papadopoulos, A.S.; Mill, L.; Arsenault, L. Increased serotonin transporter gene (SERT) DNA methylation is associated with bullying victimization and blunted cortisol response to stress in childhood: A longitudinal study of discordant monozygotic twins. Psychol. Med. 2013, 43, 1813–1823. [Google Scholar] [CrossRef]
- Efstahopoulos, P.; Anderson, F.; Melas, P.A.; Yang, L.L.; Villaescusa, J.C.; Ruegg, J.; Ekstrom, T.J.; Forsell, Y.; Galanti, M.R.; Lavebratt, C. NR3C1 hypermethylation in depressed and bullied adolescents. Transl. Psychiatry 2018, 8, 121. [Google Scholar] [CrossRef]
- Marzi, S.J.; Sujden, K.; Arsenault, L.; Belsky, D.W.; Burrage, J.; Corcoran, D.L.; Danese, A.; Fisher, H.L.; Hannon, E.; Moffitt, T.E.; et al. Analysis of DNA methylation in young people: Limited evidence for an association between victimization stress and epigenetic variation in blood. Am. J. Psych. 2018, 175, 517–529. [Google Scholar] [CrossRef] [PubMed]
- Cacioppo, S.; Cacioppo, J. Decoding the invisible forces of social connection. Front. Integr. Neurosci. 2012, 6, 51. [Google Scholar] [CrossRef] [PubMed]
- Coan, J.; Sbarra, D.A. Social baseline theory: The social regulation of risk and effort. Curr. Opin. Psychol. 2015, 1, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Ttofi, M.M.; Bowes, L.; Farrington, D.P.; Lösel, P. Protective factors interrumping the continuity from school bullying to later internalizing and externalizing problems: A systematic review of prospective longitudinal studies. J. Sch. Violence 2014, 13, 5–38. [Google Scholar] [CrossRef]
- Middlesbrooks, J.S.; Audage, C.A. The Effects of Childhood Stress on Health across the Lifespan; Centers for Disease Control and Prevention, National Center for Injury Prevention and Control: Atlanta, GA, USA, 2008. Available online: https://stacks.cdc.gov/view/cdc/6978 (accessed on 18 December 2022).
- Ttofi, M.M.; Farrington, D.P. Effectiveness of school-based programs to reduce bullying: A systematic and meta-analytic review. J. Exp. Criminol. 2011, 7, 27–56. [Google Scholar] [CrossRef]
- Fraguas, D.; Díaz-Caneja, C.; Ayora, M.; Durán-Cutlla, M.; Abregú-Crespo, R.; Ezquiaga-Bravo, I.; Martín-Babarro, J.; Arango, C. Assessment of school anti-bullying interventions: A meta-analysis of randomized controlled trials. JAMA Pediatr. 2021, 175, 44–55. [Google Scholar] [CrossRef]
- McEwen, B.S.; Eiland, L.; Hunter, R.G.; Miller, M.M. Stress and anxiety: Structural plasticity and epigenetic regulation as a consequence of stress. Neuropharmacology 2012, 62, 3–12. [Google Scholar] [CrossRef]
- Sildberg, J.L.; Copeland, W.; Linker, J.; Moore, A.; Roberson-Nay, R.; York, T.P. Psychiatric outcomes of bullying victimization: A study of discordant monozygotic twins. Psychol. Med. 2016, 46, 1875–1883. [Google Scholar] [CrossRef]
- Brewin, C.R.; Andrews, B.; Gotlib, I.H. Psychopathology and early experience: A reappraisal of retrospective reports. Psychol. Bull. 1993, 113, 82–89. [Google Scholar] [CrossRef]
- Sánchez, F.C.; Romero, M.F.; Zaragoza, J.N.; Ruiz-Cabello, A.L.; Frantzisko, O.R.; Maldonado, A.L. Prevalence and patterns of traditional bullying victimization and cyber-teasing among college population in Spain. BMC Public Health 2016, 16, 176. [Google Scholar] [CrossRef]
- Masillo, A.; Valmaggia, L.R.; Saba, R.; Brandizzi, M.; Cascio, N.; Telesfro, L.; Venturini, P.; Izzo, A.; Mattioli, M.T.; D’Alerma, M.; et al. Interpersonal sensitivity, bullying victimization and paranoid ideation among help-seeking adolescents and young adults. Early Interv. Psychiatry 2019, 13, 57–63. [Google Scholar] [CrossRef] [PubMed]
| Sociodemographic | Patients with History of PV N = 28 | Patients without History of PV N = 418 | p-Value |
|---|---|---|---|
| Gender (female/male) | 20/8 | 323/95 | ns |
| Age (years) | 28.2 ± 7.3 | 33.7 ± 8.3 | <0.001 |
| Marital Status N (%) | |||
| Married | 8 (28.6) | 146 (34.9) | ns |
| Single | 20 (71.4) | 221 (52.9) | ns |
| Divorced | 0 (0) | 45 (10.8) | - |
| Widow/er | 0 (0) | 6 (1.4) | - |
| Academic formation N (%) | |||
| Obligatory secondary education | 14 (50) | 185 (44.3) | ns |
| High School | 12 (42.9) | 154 (36.8) | ns |
| University Studies | 2 (7.1) | 79 (18.9) | ns |
| Axis I Disorders | Patients with History of PV N = 28 | Patients without History of PV N = 418 | p-Value |
|---|---|---|---|
| Anxiety disorders | 25 | 37.4 | ns |
| Depressive disorders | 50 | 38.6 | ns |
| Adjustment disorders | 3.6 | 20.6 | <0.005 |
| Somatoform disorders | 3.6 | 6.5 | ns |
| Obsessive-Compulsive | 17.9 | 4.5 | <0.005 |
| Eating disorder | 7.1 | 2.2 | ns |
| Post-traumatic Stress | 0 | 1.9 | ns |
| Psychotic symptoms | 0 | 1.2 | ns |
| Bipolar disorder | 0 | 1 | ns |
| SCID II-Q Personality Scales | Patients with History of PV N = 28 | Patients without History of PV N = 418 | p-Value |
|---|---|---|---|
| Avoidant (0–7) | 5.03 ± 1.97 | 3.19 ± 2.21 | <0.001 |
| Dependent (0–8) | 3.39 ± 1.37 | 2.76 ± 1.94 | ns |
| Obsessive (0–9) | 4.07 ± 1.78 | 3.85 ± 1.87 | ns |
| Depressive (0–8) | 5.60 ± 1.91 | 4.05 ± 2.42 | <0.001 |
| Paranoid (0–8) | 3.82 ± 1.92 | 2.59 ± 2.17 | <0.005 |
| Schizotypal (0–11) | 2.68 ± 1.65 | 2.50 ± 2.16 | ns |
| Schizoid (0–6) | 3.00 ± 1.54 | 2.69 ± 1.54 | ns |
| Histrionic (0–7) | 1.14 ± 1.53 | 0.80 ± 1.15 | ns |
| Narcissistic (0–16) | 2.93 ± 2.70 | 2.54 ± 2.34 | ns |
| Borderline (0–14) | 6.40 ± 2.95 | 4.92 ± 3.60 | <0.050 |
| Frequency (%) | Patients with History of PV N = 28 | Patients without History of PV N = 418 | p-Value |
|---|---|---|---|
| Avoidant | 60.7 | 12.2 | <0.001 |
| Dependent | 3.6 | 4.3 | ns |
| Obsessive | 7.1 | 6 | ns |
| Depressive | 28.5 | 5.2 | <0.001 |
| Paranoid | 17.9 | 5 | <0.005 |
| Schizotypal | 3.6 | 0.5 | ns |
| Schizoid | 3.6 | 0.5 | ns |
| Histrionic | 3.6 | 1.2 | ns |
| Narcissistic | 0 | 0.9 | ns |
| Borderline | 17.9 | 8.9 | ns |
| Median (IQR) | Patients with History of PV N = 28 | Patients without History of PV N = 418 | p-Value |
|---|---|---|---|
| Self-esteem (0–4) | 2 (1) | 3 (1) | <0.001 |
| Self-assessment of general mood (1–10) | 3.5 (3) | 4 (3) | ns |
| Self-assessment of social relationships (1–10) | 4 (4) | 5 (3) | <0.05 |
| Self-assessment of daily work or school (1–10) | 4 (4.75) | 5 (5) | ns |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernández-Martínez, R.; Fernández-Pereira, C.; Pérez-Rodríguez, D.; Salgado-Barreira, A.; García, C.V.; Teso-Cuesta, S.; Prieto-González, J.M.; Olivares Díez, J.M.; Agís-Balboa, R.C. Association between Peer Victimization (PV) in Childhood/Adolescence and Personality Disorders among Adult Patients. Int. J. Transl. Med. 2023, 3, 12-26. https://doi.org/10.3390/ijtm3010002
Fernández-Martínez R, Fernández-Pereira C, Pérez-Rodríguez D, Salgado-Barreira A, García CV, Teso-Cuesta S, Prieto-González JM, Olivares Díez JM, Agís-Balboa RC. Association between Peer Victimization (PV) in Childhood/Adolescence and Personality Disorders among Adult Patients. International Journal of Translational Medicine. 2023; 3(1):12-26. https://doi.org/10.3390/ijtm3010002
Chicago/Turabian StyleFernández-Martínez, Rafael, Carlos Fernández-Pereira, Daniel Pérez-Rodríguez, Angel Salgado-Barreira, Cesar Veiga García, Sara Teso-Cuesta, Jose María Prieto-González, José Manuel Olivares Díez, and Roberto Carlos Agís-Balboa. 2023. "Association between Peer Victimization (PV) in Childhood/Adolescence and Personality Disorders among Adult Patients" International Journal of Translational Medicine 3, no. 1: 12-26. https://doi.org/10.3390/ijtm3010002
APA StyleFernández-Martínez, R., Fernández-Pereira, C., Pérez-Rodríguez, D., Salgado-Barreira, A., García, C. V., Teso-Cuesta, S., Prieto-González, J. M., Olivares Díez, J. M., & Agís-Balboa, R. C. (2023). Association between Peer Victimization (PV) in Childhood/Adolescence and Personality Disorders among Adult Patients. International Journal of Translational Medicine, 3(1), 12-26. https://doi.org/10.3390/ijtm3010002






