Rib Fractures: A Review of Presenting Factors, Associated Injuries and Outcomes at a Level 1 Trauma Facility
Abstract
1. Introduction
2. Materials and Methods
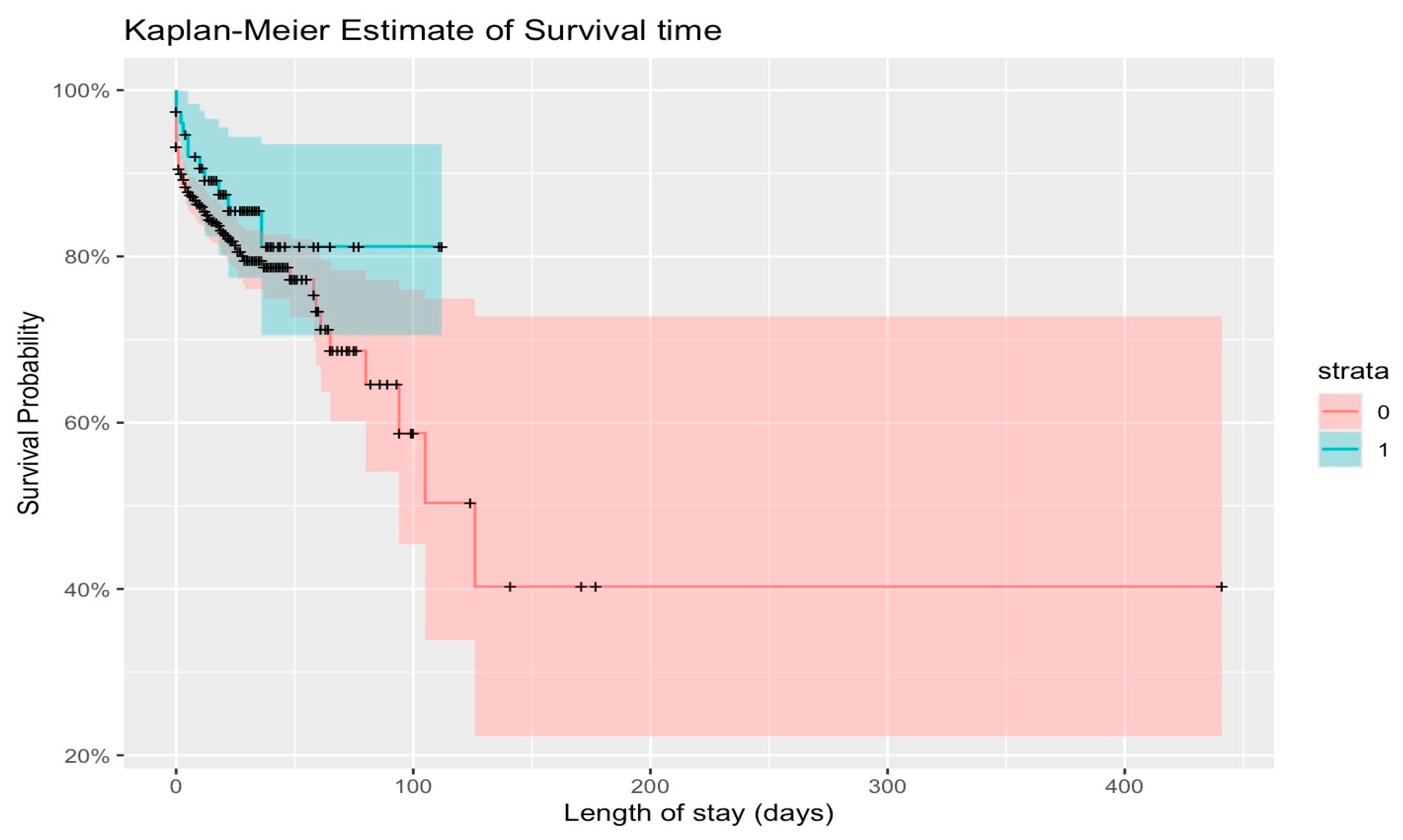
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Witt, C.E.; Bulger, E.M. Comprehensive approach to the management of the patient with multiple rib fractures: A review and introduction of a bundled rib fracture management protocol. Trauma Surg. Acute Care Open 2017, 2, e000064. [Google Scholar] [CrossRef]
- Ziegler, D.W.; Agarwal, N.N. The morbidity and mortality of rib fractures. J. Trauma 1994, 37, 975–979. [Google Scholar] [CrossRef]
- Flagel, B.T.; Luchette, F.A.; Reed, R.L.; Esposito, T.J.; Davis, K.A.; Santaniello, J.M.; Gamelli, R.L. Half-a-dozen ribs: The break point for mortality. Surgery 2005, 138, 717–723. [Google Scholar] [CrossRef]
- Tanaka, H.; Yukioka, T.; Yamaguti, Y.; Shimizu, S.; Goto, H.; Matsuda, H.; Shimazaki, S. Surgical stabilization or internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J. Trauma 2002, 52, 727–732. [Google Scholar] [CrossRef]
- Dehghan, N.; De Mestral, C.; McKee, M.D.; Schemitsch, E.H.; Nathens, A. Flail chest injuries: A review of outcomes and treatment practices from National Trauma Data Bank. J. Trauma Acute Care Surg. 2014, 76, 462–468. [Google Scholar] [CrossRef]
- Bulger, E.; Arneson, M.A.; Mock, C.N.; Jurkovic, G.J. Rib fractures in the elderly. J. Trauma 2000, 48, 1040–1046, discussion 1046–1047. [Google Scholar] [CrossRef] [PubMed]
- Fabricant, L.; Ham, B.; Mullins, R.; Mayberry, J. Prolonged pain and disability are common after rib fractures. Am. J. Surg. 2013, 205, 511–515. [Google Scholar] [CrossRef] [PubMed]
- Gordy, S.; Fabricant, L.; Ham, B.; Mullins, R.; Mayberry, J. The contribution of rib fractures to chronic pain and disability. Am. J. Surg. 2014, 207, 659–662, discussion 662–663. [Google Scholar] [CrossRef]
- Harrington, D.T.; Philips, B.; Machan, J.; Zacharias, N.; Velmahos, G.C.; Rosenblatt, M.S.; Winston, E.; Patterson, L.; Desjardins, S.; Winchell, R.; et al. Factors associated with survival following blunt chest trauma in older patients: Results from a large regional trauma cooperative. Arch. Surg. 2010, 145, 432–437. [Google Scholar] [CrossRef] [PubMed]
- Pressley, C.M.; Fry, W.R.; Philp, A.S.; Berry, S.D.; Smith, R.S. Predicting outcome of patients with chest wall injury. Am. J. Surg. 2012, 204, 910–913. [Google Scholar] [CrossRef]
- Leinicke, J.A.; Elmore, L.; Freeman, B.D.; Colditz, G.A. Operative management of rib fractures in the setting of flail chest: A systematic review and meta-analysis. Ann. Surg. 2013, 258, 914–921. [Google Scholar] [CrossRef]
- Richardson, J.D.; Franklin, G.A.; Heffley, S.; Seligson, D. Operative fixation of chest wall fractures: An underused procedure? Am. Surg. 2007, 73, 591–597. [Google Scholar] [CrossRef]
- Slobogean, G.P.; MacPherson, C.A.; Pelletier, A.; Hameed, S.M. Surgical fixation vs nonoperative management of flail chest: A meta-analysis. J. Am. Coll. Surg. 2003, 216, 302–311. [Google Scholar] [CrossRef]
- Roser, M.; Rohenkohl, B.; Arriagada, P.; Hasell, J.; Ritchie, H.; Ortiz-Ospina, E. World Bank Income Groups-Economic Growth. 2023. Available online: https://ourworldindata.org/economic-growth (accessed on 28 August 2025).
- Schulte, K.; Whitaker, D.; Attia, R. In patients with acute flail chest does surgical rib fixation improve outcomes in terms of morbidity and mortality? Interact. Cardiovasc. Thorac. Surg. 2016, 23, 314–319. [Google Scholar] [CrossRef]
- De Jong, M.B.; Kokke, M.C.; Hietbrink, F.; Leenen, L.P. Surgical management of rib fractures: Strategies and literature review. Scand. J. Surg. 2014, 103, 120–125. [Google Scholar] [CrossRef]
- De Moya, M.; Nirula, R.; Biffl, W. Rib fixation: Who, what, when? Trauma Surg. Acute Care Open 2017, 2, e000059. [Google Scholar] [CrossRef]
- Pettiford, B.L.; Luketich, J.D.; Landreneau, R.J. The management of flail chest. Thorac. Surg. Clin. 2007, 17, 25–33. [Google Scholar] [CrossRef]
- Marasco, S.; Cooper, J.; Pick, A.; Kossmann, T. Pilot study of operative fixation of fractured ribs in patients with flail chest. ANZ J. Surg. 2009, 79, 804–808. [Google Scholar] [CrossRef] [PubMed]
- Monzon, B.I.; Fingleson, L.M.; Moeng, M.S. Surgical rib fixation as an alternative method of treatment for multiple rib fractures: An audit of results compared with traditional medical management. S. Afr. J. Surg. 2021, 59, 86–89. [Google Scholar] [CrossRef]
- Hardcastle, T.C.; Steyn, E.; Boffard, K.; Goosen, J.; Toubkin, M.; Loubser, A.; Allard, D.; Moeng, S.; Muckart, D.; Brysiewicz, P.; et al. Guideline for the assessment of trauma centres for South Africa. S. Afr. J. Surg. 2011, 101, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Moore, J. Chest Trauma: Current Recommendations for Rib Fractures, Pneumothorax, and Other Injuries. Curr. Anesthesiol. Rep. 2020, 10, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Summer, A.; Boston, R. STATA: A Statistical Analysis System for Examining Biomedical Data. In Mathematical Modeling in Nutrition and the Health Sciences; Novotny, J.A., Green, M.H., Boston, R.C., Eds.; Advances in Experimental Medicine and Biology; Springer: Boston, MA, USA, 2023; Volume 537, pp. 353–369. [Google Scholar] [CrossRef]
- Billé, A.; Okiror, L.; Campbell, A.; Simons, J.; Routledge, T. Evaluation of long-term results and quality of life in patients who underwent rib fixation with titanium devices after trauma. Gen. Thorac. Cardiovasc. Surg. 2013, 61, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Hemati, K.; Gray, A.T.; Agrawal, A. Comprehensive Review of the Non-operative Management of Traumatic Rib Fractures. Curr. Anesthesiol. Rep. 2024, 14, 567–575. [Google Scholar] [CrossRef]
- Doben, A.R.; Eriksson, E.A.; Denlinger, C.E.; Leon, S.M.; Couillard, D.J.; Fakhry, S.M.; Minshall, C.T. Surgical rib fixation for flail chest deformity improves liberation from mechanical ventilation. J. Crit. Care 2014, 29, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Tamas, F. Surgical management of chest wall trauma. Thoracic. Surg. Clin. 2010, 20, 755–766. [Google Scholar]
- Galvagno, S.M.; Smith, C.; Varon, A.; Hasenboehler, E.; Sultan, S.; Shaefer, G. EAST Guidelines. Thoracic Trauma, Blunt, Pain Management. J. Trauma 2016, 81, 936–951. [Google Scholar] [CrossRef]
- Franssen, A.; Daemen, J.; Daemen, J.H.T.; Luyten, J.A.; Meesters, B.; Pijnenburg, A.M.; Reisinger, K.W.; van Vugt, R.; Hulsewé, K.W.E.; Vissers, Y.L.J.; et al. Treatment of traumatic rib fractures: An overview of current evidence and future perspectives. J. Thorac. Dis. 2024, 16, 5399–5408. [Google Scholar] [CrossRef]
- Boffard, K.; White, J.O. Definitive Surgical Trauma Care, 6th ed.; CRC Press: Abingdon, UK, 2024; pp. 116–125. [Google Scholar]
- Davoodabadi, A.; Mosavibioki, N.; Mashayekhil, M.; Gilasi, H.; Kashi, E.A.; Haghpanah, B. Correlation of rib fracture patterns with abdominal solid organ injury: A retrospective observational cohort study. Chin. J. Traumatol. 2021, 25, 45–48. [Google Scholar] [CrossRef]
- Peek, J.; Reinier, B.; Hietbrink, F.; De Jong, M.B.; Heng, M.; Beeres, F.J.; IJpma, F.F.; Leenen, L.P.; Groenwold, R.H.H.; Houwert, R.M. Epidemiology and outcome of rib fractures: A nationwide study in the Netherlands. Eur. J. Trauma Emerg. Surg. 2022, 48, 265–271. [Google Scholar] [CrossRef]
- Rapsang, A.; Shyam, D. Scoring Systems of Severity in Patients with Multiple Trauma. Cir. Esp. J. 2015, 93, 213–221. [Google Scholar] [CrossRef]

| Features | Subtypes | n (Percentage) |
|---|---|---|
| Incidence of Rib fractures | Total 7750 | 940 (12%) |
| Age | 45 (34–55) | |
| Gender | Male | 737 (78%) |
| Female | 203 (22%) | |
| Ethnicity | White | 423 (45%) |
| African | 420 (45%) | |
| Indian | 49 (5%) | |
| Others | 25 (3%) | |
| Unknown | 23 (2%) | |
| Mechanism of injury | Blunt | 899 (96%) |
| Penetrating | 41 (4%) | |
| Rib Fractures | <2 | 169 (18%) |
| 2–3 | 146 (16%) | |
| >3 | 625 (66%) | |
| [Clinical Flail Segment] | 44 (5%) | |
| Systolic Blood Pressure median [IQR] | 126 (109–144) | |
| Pulse median [IQR] | 91 (79–108) | |
| ISS median [IQR] | 17 (10–29) | |
| NISS median [IQR] | 22 (14–34) | |
| Rib fixation | 76 (8%) | |
| LOS (in days) median [IQR] | 14 (6–25) | |
| Discharged | 781 (83%) | |
| Died | 159 (17%) | |
| 30-day mortality | 148 (93%) |
| Associated Injuries | Subtypes | Percentage | Total |
|---|---|---|---|
| Chest | Mild—Other associated fractures (sternum, scapula) | 106 (27%) | 396 (42.1%) |
| Moderate—Associated Cardiac, lung contusions | 221 (56%) | ||
| Severe—Major Contusions and fractures, or combined other injuries (aortic, diaphragm rupture) | 69 (17%) | ||
| Head | Mild—Facial fractures, concussion | 95 (31%) | 306 (32.55%) |
| Moderate—Above plus minus TBI isolated bleed/BOS fracture | 108 (35%) | ||
| Severe—Above plus TBI multiple bleeds, cerebral edema, DAI | 103 (34%) | ||
| Spine | Mild—Isolated C, L or T-spine isolated | 112 (42%) | 269 (28.6%) |
| Moderate—Multiple C, L or T spine | 87 (32%) | ||
| Severe—C, L and T spine, or associated injury | 70 (26%) | ||
| Abdomen | Mild—1 organ injured | 105 (32%) | 330 (35.1%) |
| Moderate—2/> organs injured, Isolated pelvic fracture | 139 (42%) | ||
| Severe—3/> organs injured, or abdominal injury with associated pelvic fracture | 86 (26%) | ||
| Extremities | Mild—1 fracture | 199 (57%) | 351 (37.3%) |
| Moderate—2–3 fractures | 93 (26%) | ||
| Severe—>3 fractures | 59 (17%) |
| Variables | Subtypes | Alive n = (%) or Median (Q1–Q3) | Dead n = (%) or Median (Q1–Q3) | p-Value |
|---|---|---|---|---|
| Rib fractures | 1 | 150 (89%) | 19 (11%) | <0.001 |
| 2–3 | 127 (87%) | 19 (13%) | ||
| >3 | 476 (82%) | 105 (18%) | ||
| Flail segment | 28 (64%) | 16 (36%) | ||
| Age | <65 years | 661 (86%) | 110 (14%) | <0.0001 |
| >65 years | 120 (71%) | 49 (29%) | ||
| Head, neck, C-spine | Mild | 86 (91%) | 9 (9%) | <0.001 |
| Moderate | 80 (74%) | 28 (26%) | ||
| Severe | 44 (43%) | 59 (57%) | ||
| Chest | Mild | 92 (87%) | 14 (13%) | 0.027 |
| Moderate | 163 (74%) | 58 (26%) | ||
| Severe | 52 (75%) | 17 (25%) | ||
| Abdomen | Mild | 83 (79%) | 22 (21%) | 0.001 |
| Moderate | 106 (76%) | 33 (24%) | ||
| Severe | 48 (56%) | 38 (44%) | ||
| Extremity | Mild | 164 (82%) | 35 (18%) | 0.006 |
| Moderate | 72 (77%) | 21 (23%) | ||
| Severe | 37 (63%) | 22 (37%) | ||
| Systolic BP (mmHg) | 129 (115–145) | 103 (68–132) | <0.001 | |
| Pulse | 90 (78–104) | 107 (83–124) | <0.001 | |
| ISS | 18 (10) | 35 (13) | <0.001 | |
| NiSS | 23 (13) | 45 (17) | <0.001 | |
| Length of Stay(days) | 16 (9–27) | 1 (0–9) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Laney, E.; Makhadi, S.; Nweke, E.E.; Elebo, N.; Moeng, M.S. Rib Fractures: A Review of Presenting Factors, Associated Injuries and Outcomes at a Level 1 Trauma Facility. Trauma Care 2025, 5, 25. https://doi.org/10.3390/traumacare5040025
Laney E, Makhadi S, Nweke EE, Elebo N, Moeng MS. Rib Fractures: A Review of Presenting Factors, Associated Injuries and Outcomes at a Level 1 Trauma Facility. Trauma Care. 2025; 5(4):25. https://doi.org/10.3390/traumacare5040025
Chicago/Turabian StyleLaney, Estelle, Shumani Makhadi, Ekene Emmanuel Nweke, Nnenna Elebo, and Maeyane Stephens Moeng. 2025. "Rib Fractures: A Review of Presenting Factors, Associated Injuries and Outcomes at a Level 1 Trauma Facility" Trauma Care 5, no. 4: 25. https://doi.org/10.3390/traumacare5040025
APA StyleLaney, E., Makhadi, S., Nweke, E. E., Elebo, N., & Moeng, M. S. (2025). Rib Fractures: A Review of Presenting Factors, Associated Injuries and Outcomes at a Level 1 Trauma Facility. Trauma Care, 5(4), 25. https://doi.org/10.3390/traumacare5040025





