Evaluation of a Standardized Severity Grading System for Blunt Thoracic Aortic Injury in the Endovascular Era: A Retrospective Review from a Level I Trauma Center
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Image Acquisition
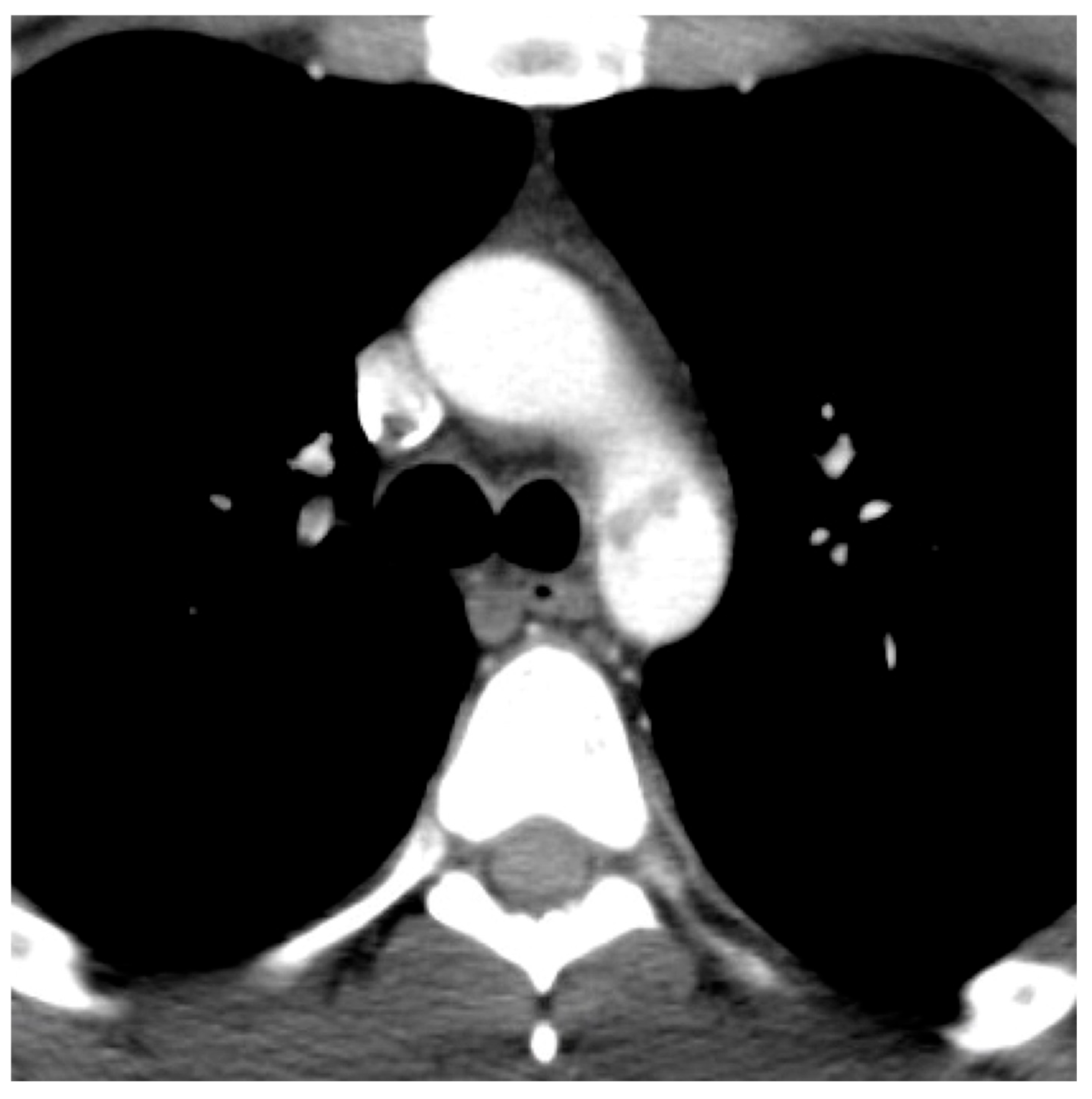
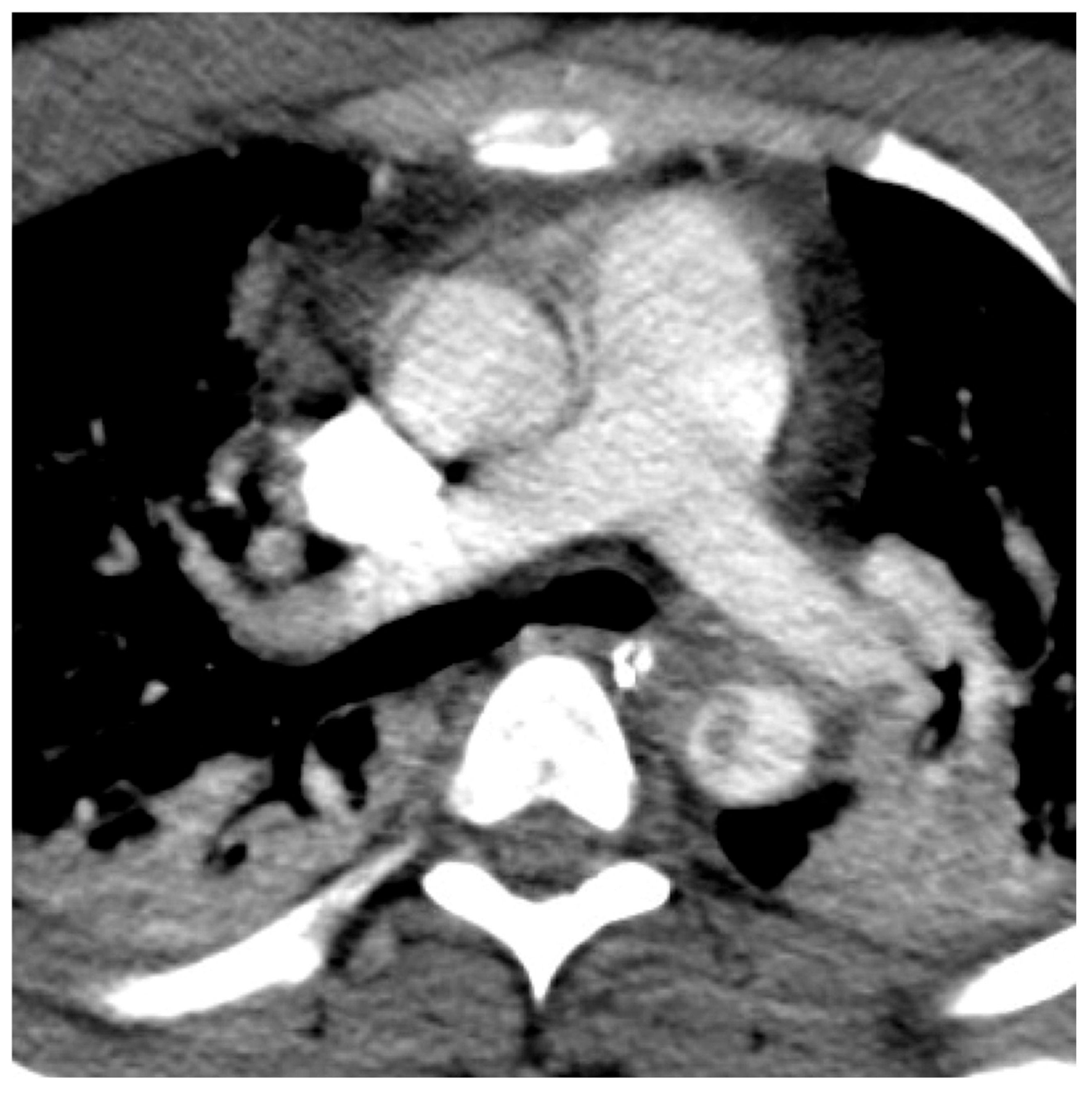
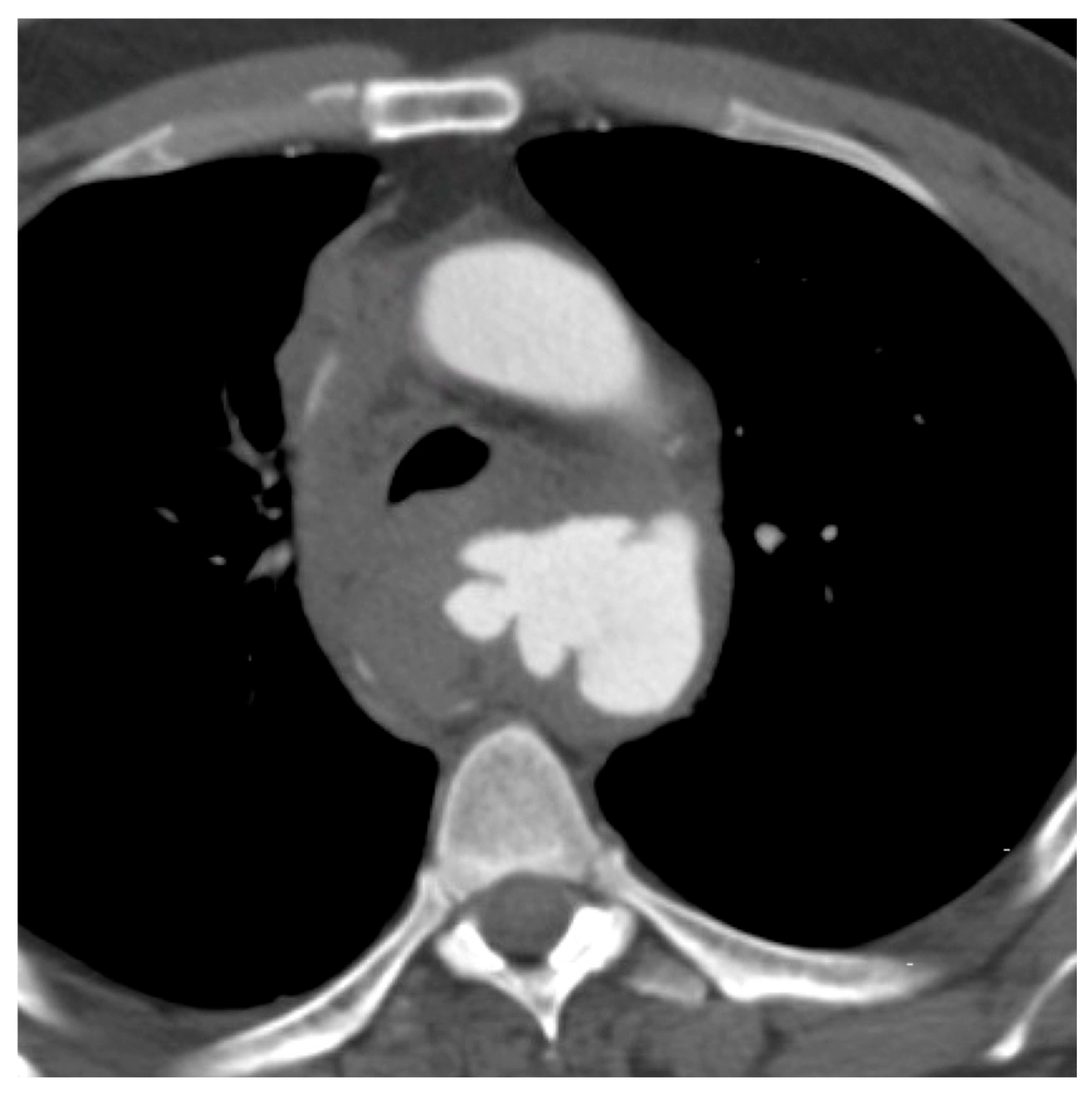
2.3. Image Interpretation
2.4. Analysis and Reporting
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brown, S.R.; Still, S.A.; Eudailey, K.W.; Beck, A.W.; Gunn, A.J. Acute traumatic injury of the aorta: Presentation, diagnosis, and treatment. Ann. Transl. Med. 2021, 9, 1193. [Google Scholar] [CrossRef]
- Steenburg, S.D.; Ravenel, J.G. Acute traumatic thoracic aortic injuries: Experience with 64-MDCT. Am. J. Roentgenol. 2008, 191, 1564–1569. [Google Scholar] [CrossRef]
- Steenburg, S.D.; Ravenel, J.G.; Ikonomidis, J.S.; Schönholz, C.; Reeves, S. Acute traumatic aortic injury: Imaging evaluation and management. Radiology 2008, 248, 748–762. [Google Scholar] [CrossRef]
- Arthurs, Z.M.; Starnes, B.W.; Sohn, V.Y.; Singh, N.; Martin, M.J.; Andersen, C.A. Functional and survival outcomes in traumatic blunt thoracic aortic injuries: An analysis of the National Trauma Databank. J. Vasc. Surg. 2009, 49, 988–994. [Google Scholar] [CrossRef]
- Parmley, L.F.; Mattingly, T.W.; Manion, W.C.; Jahnke, E.J., Jr. Nonpenetrating traumatic injury of the aorta. Circulation 1958, 17, 1086–1101. [Google Scholar] [CrossRef] [PubMed]
- Demehri, S.; Rybicki, F.J.; Desjardins, B.; Fan, C.-M.; Flamm, S.D.; Francois, C.J.; Gerhard-Herman, M.D.; Kalva, S.P.; Kim, H.S.; Mansour, M.A.; et al. ACR Appropriateness Criteria(®) blunt chest trauma--suspected aortic injury. Emerg. Radiol. 2012, 19, 287–292. [Google Scholar] [CrossRef]
- Monga, A.; Patil, S.B.; Cherian, M.; Poyyamoli, S.; Mehta, P. Thoracic Trauma: Aortic Injuries. Semin. Interv. Radiol. 2021, 38, 84–95. [Google Scholar] [CrossRef] [PubMed]
- Shackford, S.R.; Dunne, C.E.; Karmy-Jones, R.; Long, W.; Teso, D.; Schreiber, M.A.; Watson, J.; Watson, C.; McIntyre, R.C.; Ferrigno, L.; et al. The evolution of care improves outcome in blunt thoracic aortic injury: A Western Trauma Association multicenter study. J. Trauma. Acute Care Surg. 2017, 83, 1006–1013. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.A.; Matsumura, J.S.; Mitchell, R.S.; Farber, M.A.; Greenberg, R.K.; Azizzadeh, A.; Murad, M.H.; Fairman, R.M. Endovascular repair of traumatic thoracic aortic injury: Clinical practice guidelines of the Society for Vascular Surgery. J. Vasc. Surg. 2011, 53, 187–192. [Google Scholar] [CrossRef]
- Elkbuli, A.; Dowd, B.; Spano, P.J.; Smith, Z.; Flores, R.; McKenney, M.; Boneva, D. Thoracic Endovascular Aortic Repair Versus Open Repair: Analysis of the National Trauma Data Bank. J. Surg. Res. 2020, 245, 179–182. [Google Scholar] [CrossRef]
- Mirvis, S.E.; Shanmuganathan, K.; Miller, B.H.; White, C.S.; Turney, S.Z. Traumatic aortic injury: Diagnosis with contrast-enhanced thoracic CT--five-year experience at a major trauma center. Radiology 1996, 200, 413–422. [Google Scholar] [CrossRef] [PubMed]
- Melton, S.M.; Kerby, J.D.; McGiffin, D.; McGwin, G.; Smith, J.K.; Oser, R.F.; Cross, J.M.; Windham, S.T.; Moran, S.G.; Hsia, J.; et al. The evolution of chest computed tomography for the definitive diagnosis of blunt aortic injury: A single-center experience. J. Trauma 2004, 56, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Jacob-Brassard, J.; Salata, K.; Kayssi, A.; Hussain, M.A.; Forbes, T.L.; Al-Omran, M.; de Mestral, C. A systematic review of nonoperative management in blunt thoracic aortic injury. J. Vasc. Surg. 2019, 70, 1675–1681.e6. [Google Scholar] [CrossRef]
- Reddy, K.N.; Matatov, T.; Doucet, L.D.; Heldmann, M.; Zhao, C.X.; Zhang, W.W. Grading system modification and management of blunt aortic injury. Chin. Med. J. 2013, 126, 442–445. [Google Scholar] [CrossRef] [PubMed]
- Madigan, M.C.; Lewis, A.J.; Liang, N.L.; Handzel, R.; Hager, E.; Makaroun, M.S.; Chaer, R.A.; Eslami, M.H. Outcomes of Operative and Non-Operative Management in Blunt Thoracic Aortic Injury. J. Vasc. Surg. 2022, 76, 239–247. [Google Scholar] [CrossRef]
- Forman, M.J.; Mirvis, S.E.; Hollander, D.S. Blunt thoracic aortic injuries: CT characterisation and treatment outcomes of minor injury. Eur. Radiol. 2013, 23, 2988–2995. [Google Scholar] [CrossRef]
- Lamarche, Y.; Berger, F.H.; Nicolaou, S.; Bilawich, A.-M.; Louis, L.; Inacio, J.R.; Janusz, M.T.; Evans, D. Vancouver simplified grading system with computed tomographic angiography for blunt aortic injury. J. Thorac. Cardiovasc. Surg. 2012, 144, 347–354.e1. [Google Scholar] [CrossRef]
- Azizzadeh, A.; Keyhani, K.; Miller, C.C., III; Coogan, S.M.; Safi, H.J.; Estrera, A.L. Blunt traumatic aortic injury: Initial experience with endovascular repair. J. Vasc. Surg. 2009, 49, 1403–1408. [Google Scholar] [CrossRef]
- Quiroga, E.; Starnes, B.W.; Tran, N.T.; Singh, N. Implementation and results of a practical grading system for blunt thoracic aortic injury. J. Vasc. Surg. 2019, 70, 1082–1088. [Google Scholar] [CrossRef]
- Khoynezhad, A.; Azizzadeh, A.; Donayre, C.E.; Matsumoto, A.; Velazquez, O.; White, R. Results of a multicenter, prospective trial of thoracic endovascular aortic repair for blunt thoracic aortic injury (RESCUE trial). J. Vasc. Surg. 2013, 57, 899–905.e1. [Google Scholar] [CrossRef]
- Grigorian, A.; Spencer, D.; Donayre, C.; Nahmias, J.; Schubl, S.; Gabriel, V.; Barrios, C. National Trends of Thoracic Endovascular Aortic Repair Versus Open Repair in Blunt Thoracic Aortic Injury. Ann. Vasc. Surg. 2018, 52, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Demetriades, D.; Velmahos, G.C.; Scalea, T.M.; Jurkovich, G.J.; Karmy-Jones, R.; Teixeira, P.G.; Hemmila, M.R.; O’COnnor, J.V.; McKenney, M.O.; Moore, F.O.; et al. Operative repair or endovascular stent graft in blunt traumatic thoracic aortic injuries: Results of an American Association for the Surgery of Trauma Multicenter Study. J. Trauma 2008, 64, 561–570. [Google Scholar] [CrossRef] [PubMed]
- Scalea, T.M.; Feliciano, D.V.; DuBose, J.J.; Ottochian, M.; O’Connor, J.V.; Morrison, J.J. Blunt Thoracic Aortic Injury: Endovascular Repair Is Now the Standard. J. Am. Coll. Surg. 2019, 228, 605–610. [Google Scholar] [CrossRef]
- Ultee, K.H.; Soden, P.A.; Chien, V.; Bensley, R.P.; Zettervall, S.L.; Verhagen, H.J.; Schermerhorn, M.L. National trends in utilization and outcome of thoracic endovascular aortic repair for traumatic thoracic aortic injuries. J. Vasc. Surg. 2016, 63, 1232–1239.e1. [Google Scholar] [CrossRef]
- Mohapatra, A.; Liang, N.L.; Makaroun, M.S.; Schermerhorn, M.L.; Farber, A.; Eslami, M.H. Risk factors for mortality after endovascular repair for blunt thoracic aortic injury. J. Vasc. Surg. 2020, 71, 768–773. [Google Scholar] [CrossRef]
- Arbabi, C.N.; DuBose, J.; Charlton-Ouw, K.; Starnes, B.W.; Saqib, N.; Quiroga, E.; Miller, C.; Azizzadeh, A.; Afifi, R.; McNutt, M.; et al. Outcomes and practice patterns of medical management of blunt thoracic aortic injury from the Aortic Trauma Foundation global registry. J. Vasc. Surg. 2022, 75, 625–631. [Google Scholar] [CrossRef]
- DuBose, J.J.; Azizzadeh, A.; Estrera, A.L.; Safi, H.J. Contemporary management of blunt aortic trauma. J. Cardiovasc. Surg. 2015, 56, 751–762. [Google Scholar]
- R: A Language and Environment for Statistical Computing; Version 4.2.0; R Foundation for Statistical Computing: Vienna, Austria, 2020.
- Aladham, F.; Sundaram, B.M.; Williams, D.M.; Quint, L.E. Traumatic aortic injury: Computerized tomographic findings at presentation and after conservative therapy. J. Comput. Assist. Tomogr. 2010, 34, 388–394. [Google Scholar] [CrossRef]
- Kapoor, H.; Lee, J.T.; Orr, N.T.; Nisiewicz, M.J.; Pawley, B.K.; Zagurovskaya, M. Minimal Aortic Injury: Mechanisms, Imaging Manifestations, Natural History, and Management. Radiographics 2020, 40, 1834–1847. [Google Scholar] [CrossRef] [PubMed]

| Variable | n = 38 a |
|---|---|
| Age, in years | 46 (24, 58) |
| Sex | |
| Male | 32 (84%) |
| Female | 6 (16%) |
| Mechanism of injury | |
| Motor vehicle collision | 20 (53%) |
| Motorcycle collision | 10 (26%) |
| Pedestrian struck | 6 (16%) |
| Fall | 2 (5%) |
| Concomitant injuries * | |
| Major head and neck (AIS 3) | 11 (29%) |
| Major face (AIS 3) | 0 (0%) |
| Major chest (AIS 3) | 37 (97%) |
| Major abdomen (AIS 3) | 13 (34%) |
| Major extremities and/or pelvis (AIS 3) | 23 (61%) |
| Major external (AIS 3) | 1 (3%) |
| ISS | 34 (29, 40) |
| TAI Severity Grade | |
| 1 (intimal tear) | 4 (11%) |
| 2 (focal dissection/intramural hematoma) | 10 (26%) |
| 3 (pseudoaneurysm) | 22 (58%) |
| 4 (rupture) | 2 (5%) |
| Location of TAI | |
| Aortic root | 0 (0%) |
| Aortic arch | 2 (5%) |
| Aortic isthmus | 29 (76%) |
| Descending thoracic aorta | 7 (18%) |
| Intervention | |
| No repair b | 18 (47%) |
| Operative repair | 20 (53%) |
| Hospital mortality | 6 (16%) |
| Hospital length of stay, in days | 18 (9, 28) |
| Variable | Grade 1; n = 4 a | Grade 2; n = 10 | Grade 3; n = 22 | Grade 4; n = 2 |
|---|---|---|---|---|
| Age, in years | 48 (14) | 43 (19) | 47 (22) | 48 (19) |
| Sex | ||||
| Male | 4 (100%) | 7 (70%) | 19 (86%) | 2 (100%) |
| Female | 0 (0%) | 3 (30%) | 3 (14%) | 0 (0%) |
| Mechanism of injury | ||||
| Motor vehicle collision | 0 (0%) | 7 (70%) | 13 (59%) | 0 (0%) |
| Motorcycle collision | 2 (50%) | 3 (30%) | 4 (18%) | 1 (50%) |
| Pedestrian struck | 1 (25%) | 0 (0%) | 4 (18%) | 1 (50%) |
| Fall | 1 (25%) | 0 (0%) | 1 (5%) | 0 (0%) |
| Concomitant injuries * | ||||
| Major head and neck (AIS 3) | 0 (0%) | 2 (20%) | 8 (36%) | 1 (50%) |
| Major face (AIS 3) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Major chest (AIS 3) | 3 (75%) | 10 (100%) | 22 (100%) | 2 (100%) |
| Major abdomen (AIS 3) | 4 (100%) | 3 (30%) | 6 (27%) | 0 (0%) |
| Major extremities and/or pelvis (AIS 3) | 3 (75%) | 6 (60%) | 14 (64%) | 0 (0%) |
| Major external (AIS 3) | 1 (25%) | 0 (0%) | 0 (0%) | 0 (0%) |
| ISS | 36 (6) | 33 (5) | 38 (12) | 44 (15) |
| Location of TAI | ||||
| Aortic root | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Aortic arch | 0 (0%) | 0 (0%) | 2 (9%) | 0 (0%) |
| Aortic isthmus | 3 (75%) | 8 (80%) | 16 (73%) | 2 (100%) |
| Descending thoracic aorta | 1 (25%) | 2 (20%) | 4 (18%) | 0 (0%) |
| Intervention | ||||
| No repair b | 4 (100%) | 8 (80%) | 4 (18%) | 2 (100%) |
| Operative repair | 0 (0%) | 2 (20%) | 18 (82%) | 0 (0%) |
| Hospital mortality | 1 (25%) | 1 (10%) | 3 (14%) | 1 (50%) |
| Hospital length of stay, in days | 30 (35) | 17 (12) | 20 (12) | 18 (25) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scott, E.M.; Chen, B.Y.; Sobieh, A.; Dorfman, J.D.; Lo, H.S. Evaluation of a Standardized Severity Grading System for Blunt Thoracic Aortic Injury in the Endovascular Era: A Retrospective Review from a Level I Trauma Center. Trauma Care 2025, 5, 22. https://doi.org/10.3390/traumacare5030022
Scott EM, Chen BY, Sobieh A, Dorfman JD, Lo HS. Evaluation of a Standardized Severity Grading System for Blunt Thoracic Aortic Injury in the Endovascular Era: A Retrospective Review from a Level I Trauma Center. Trauma Care. 2025; 5(3):22. https://doi.org/10.3390/traumacare5030022
Chicago/Turabian StyleScott, Erin M., Byron Y. Chen, Ahmed Sobieh, Jon D. Dorfman, and Hao S. Lo. 2025. "Evaluation of a Standardized Severity Grading System for Blunt Thoracic Aortic Injury in the Endovascular Era: A Retrospective Review from a Level I Trauma Center" Trauma Care 5, no. 3: 22. https://doi.org/10.3390/traumacare5030022
APA StyleScott, E. M., Chen, B. Y., Sobieh, A., Dorfman, J. D., & Lo, H. S. (2025). Evaluation of a Standardized Severity Grading System for Blunt Thoracic Aortic Injury in the Endovascular Era: A Retrospective Review from a Level I Trauma Center. Trauma Care, 5(3), 22. https://doi.org/10.3390/traumacare5030022





